Cross-National Systematic Review of Neonatal Mortality and Postnatal Newborn Care: Special Focus on Pakistan
Abstract
1. Introduction
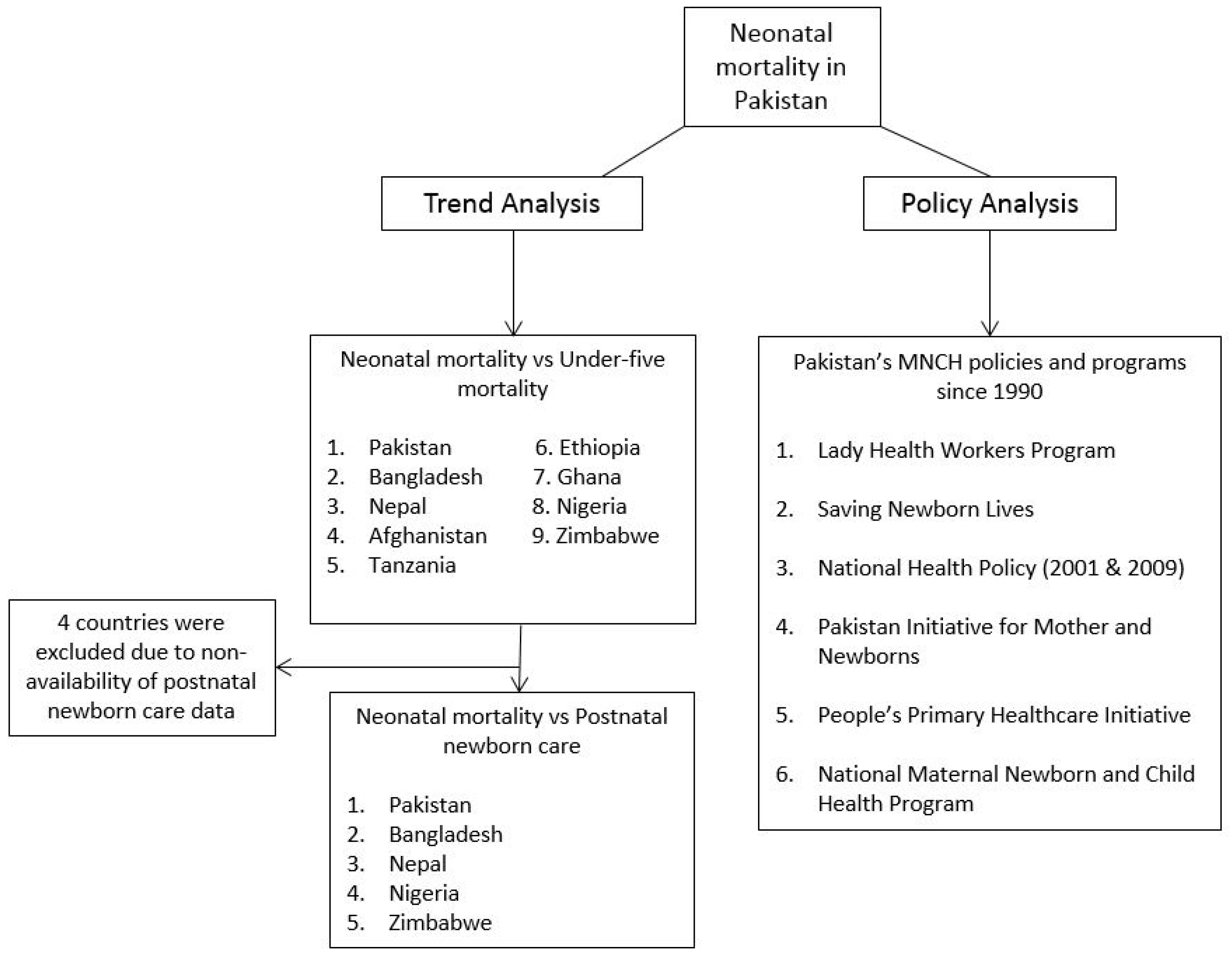
2. Materials and Methods
2.1. Data Source for Trend Analysis
2.2. Measures
2.3. Demographic and Health Surveys (DHSs)
2.4. Pakistan DHS of 2012–2013
2.5. Data Source for Policy Analysis
- any health policies or programs related to maternal, newborn, and child health that started after the year 1990, and are still in progress;
- public, private, semi-private, and non-governmental organization programs;
- implemented in more than 20 districts.
2.6. Data Analysis
3. Results and Discussion
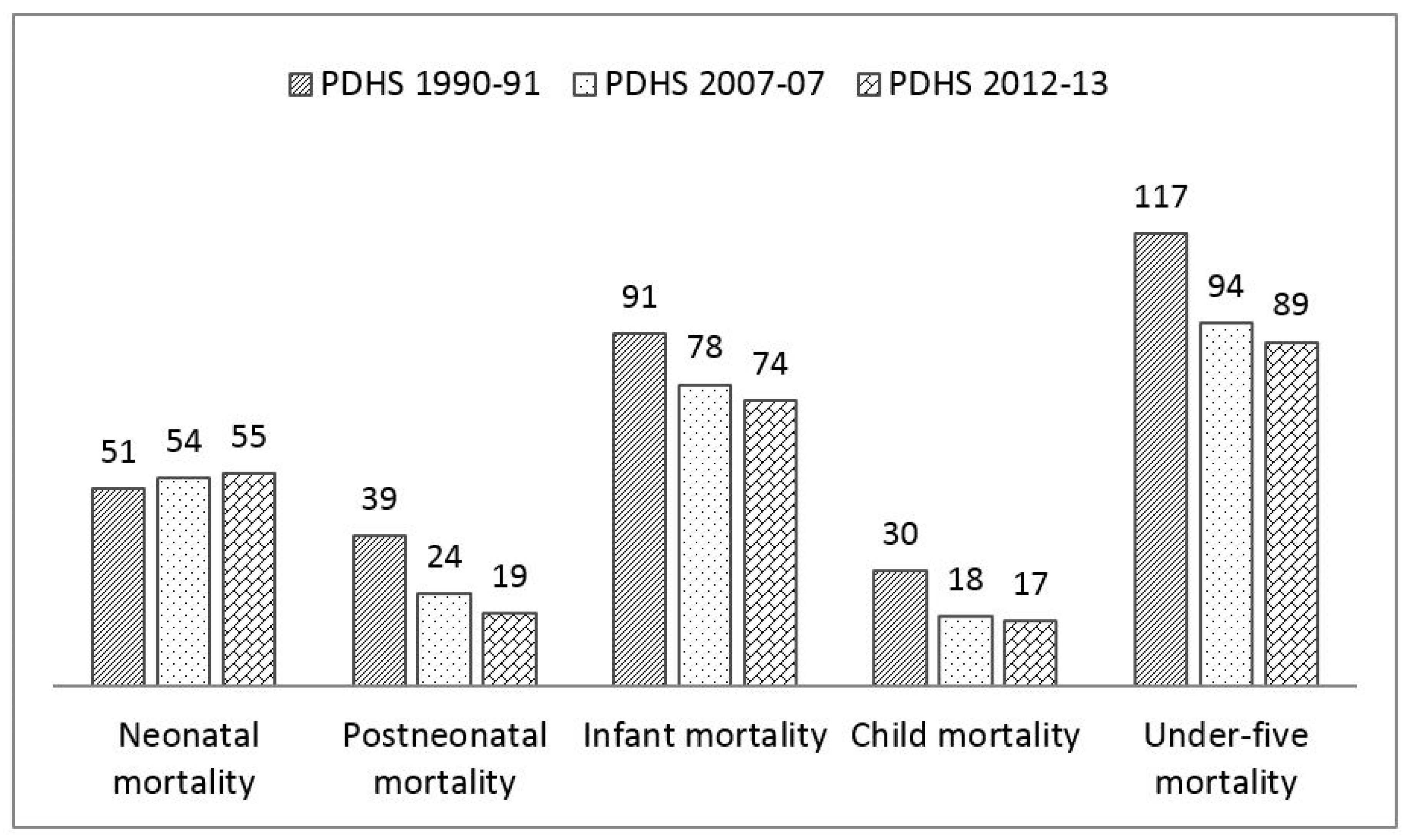
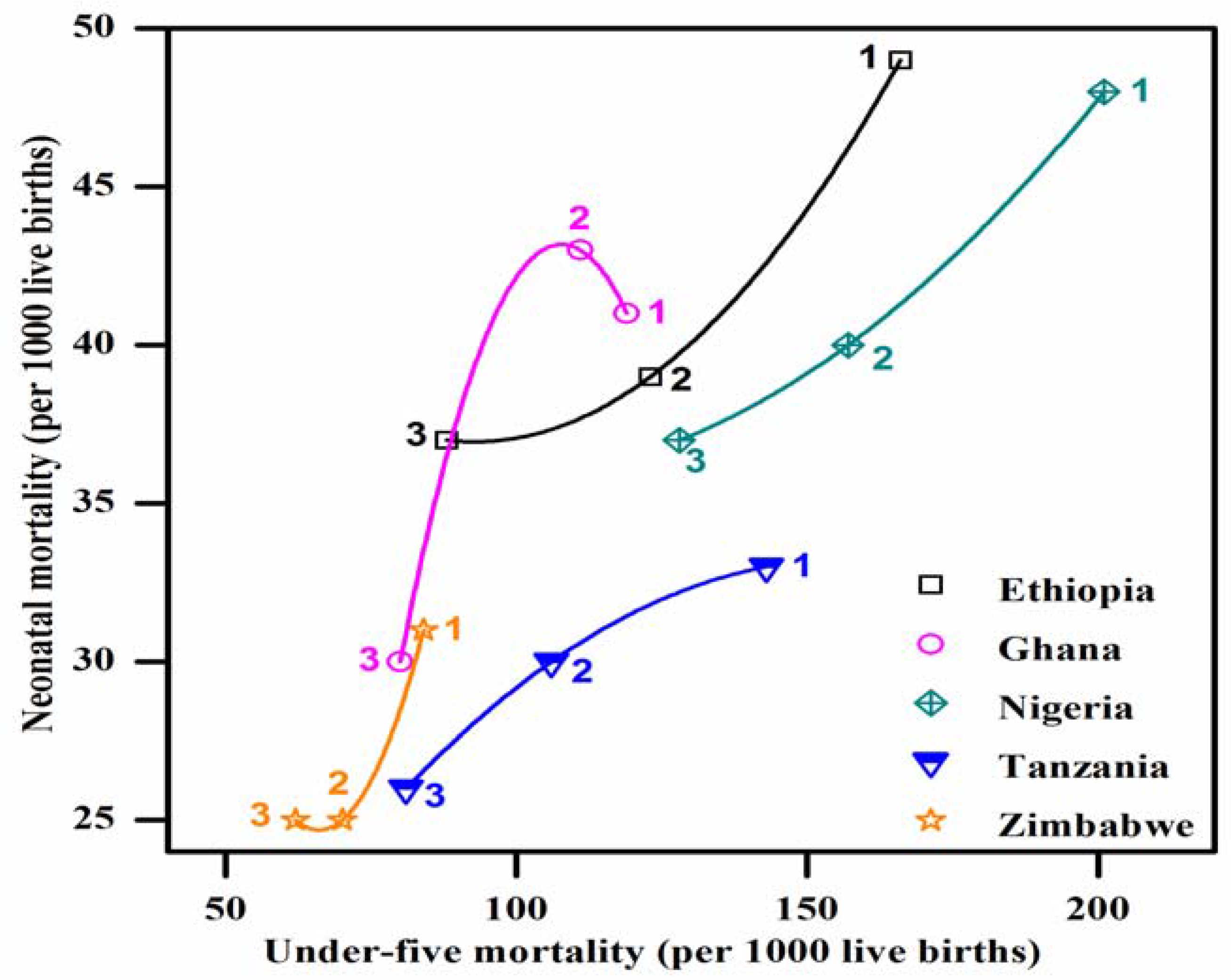
3.1. Neonatal Mortality Rate
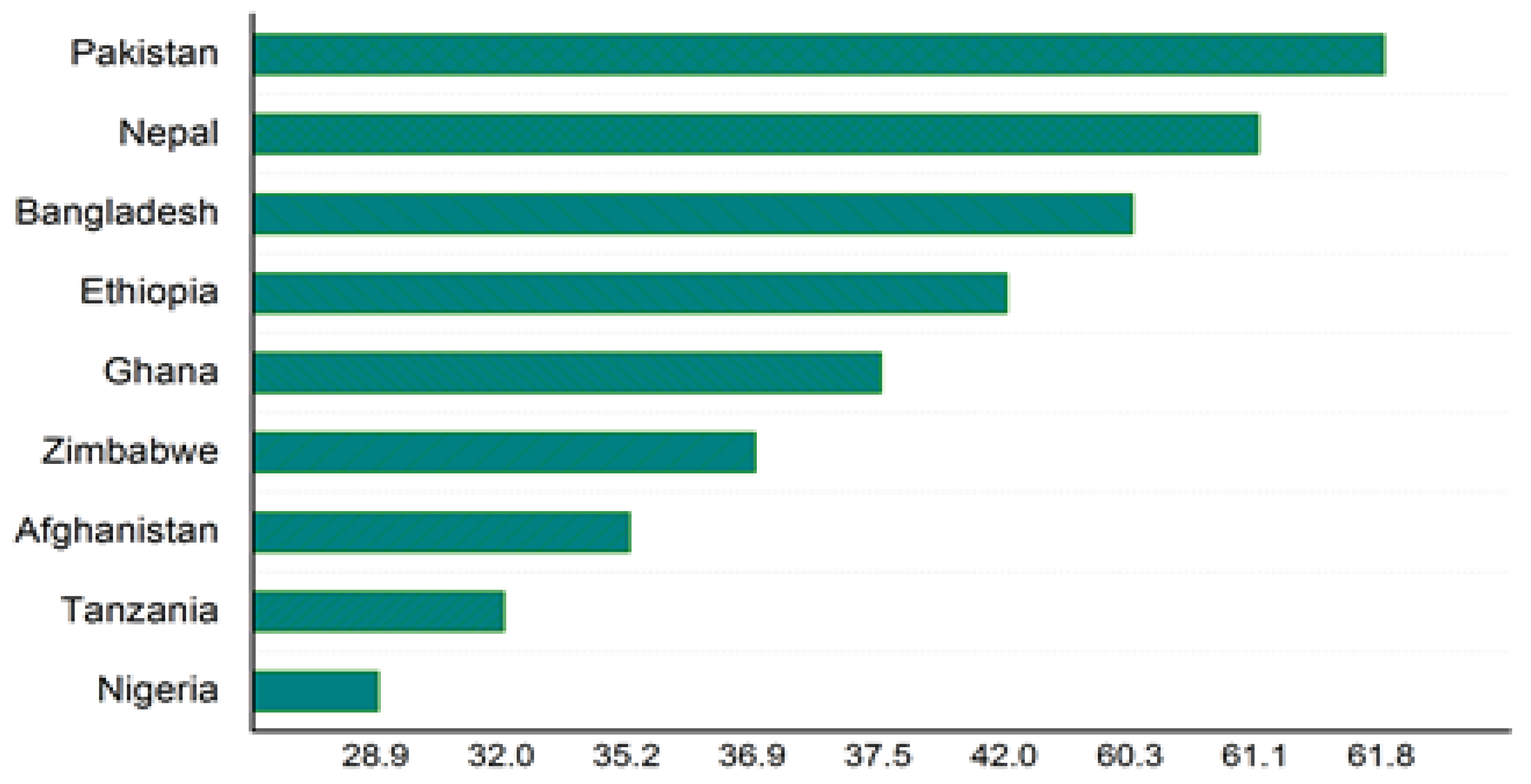
3.2. Ineffective Postnatal Care
3.3. No Nationwide Policy on Newborn Care
3.4. Limitations
4. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- United Nations. The Millennium Development Goals. Report 2013 New York. Available online: http://www.un.org/millenniumgoals/pdf/Goal_4_fs.pdf (accessed on 8 January 2015).
- United Nations. The Millennium Development Goals. Report 2014. Available online: http://www.un.org/millenniumgoals/2014%20MDG%20report/MDG%202014%20English%20web.pdf (accessed on 8 January 2015).
- World Health Organization. Global Health Observatory. Available online: http://www.who.int/gho/ child_health/mortality/neonatal_text/en/ (accessed on 8 February 2015).
- Belizán, J.M.; McClure, E.M.; Goudar, S.S.; Pasha, O.; Esamai, F.; Patel, A.; Chomba, E.; Garces, A.; Wright, L.L.; Koso-Thomas, M. Neonatal death in low-to middle-income countries: A global network study. Am. J. Perinatol. 2012, 29, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Oestergaard, M.Z.; Inoue, M.; Yoshida, S.; Mahanani, W.R.; Gore, F.M.; Cousens, S.; Lawn, J.E.; Mathers, C.D. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: A systematic analysis of progress, projections, and priorities. PLoS Med. 2011, 8, e1001080. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population Studies Islamabad, Pakistan. Pakistan Demographic and Health Survey 2012–2013; MEASURE DHS ICF International: Calverton, MD, USA, 2013. [Google Scholar]
- Pakistan Millennium Development Goals Report 2013; Planning Commission, Government of Pakistan; United Nations Development Programme: New York, NY, USA, 2013.
- Ayaz, A.; Saleem, S. Neonatal mortality and prevalence of practices for newborn care in a squatter settlement of karachi, pakistan: A cross-sectional study. PLoS ONE 2010, 5, e13783. [Google Scholar] [CrossRef] [PubMed]
- Nisar, Y.B.; Dibley, M.J. Determinants of neonatal mortality in pakistan: Secondary analysis of pakistan demographic and health survey 2006–2007. BMC Public Health 2014, 14, 663. [Google Scholar] [CrossRef] [PubMed]
- Cross-national research to help countries prepare for an aging population. Rev. Panam. Salud Pública 2001, 10, 277–283.
- World Health Organization. Who Recommendations on Postnatal Care of the Mother and Newborn; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Mazia, G.; Narayanan, I.; Warren, C.; Mahdi, M.; Chibuye, P.; Walligo, A.; Mabuza, P.; Shongwe, R.; Hainsworth, M. Integrating quality postnatal care into pmtct in Swaziland. Glob. Public Health 2009, 4, 253–270. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Monitoring Progress towards the Millennium Development Goals. Available online: http://www.mdgtrack.org/index.php?m=1&tab=c (accessed on 27 June 2015).
- Coltart, D. A Decade of Suffering in Zimbabwe: Economic Collapse and Political Repression under Robert Mugabe; CATO Institute: Washington, DC, USA, 2008. [Google Scholar]
- Ghana, Ministry of Health. Ghana National Newborn Health Strategy and Action Plan 2014–2018; Ministry of Health: Accra, Ghana, 2014.
- National Neonatal Health Strategy and Guidelines for Bangladesh, October 2009. Available online: https://extranet.who.int/nutrition/gina/sites/default/files/BGD%202009%20National%20Neonatal%20Health%20Strategy.pdf (accessed on 29 June 2015).
- Biswas, A.; Rahman, F.; Eriksson, C.; Halim, A.; Dalal, K. Facility death review of maternal and neonatal deaths in Bangladesh. PLoS ONE 2015, 10, e0141902. [Google Scholar] [CrossRef] [PubMed]
- Sitrin, D.; Guenther, T.; Murray, J.; Pilgrim, N.; Rubayet, S.; Ligowe, R.; Pun, B.; Malla, H.; Moran, A. Reaching mothers and babies with early postnatal home visits: The implementation realities of achieving high coverage in large-scale programs. PLoS ONE 2013, 8, e68930. [Google Scholar] [CrossRef] [PubMed]
- Saadat, S.; Cortez, R.; Voetberg, A.; Chowdhury, S.; Sarker, I. Achieving Mdgs 4&5: Nepal’s Progress on Maternal and Child Health; The World Bank: Washington, DC, USA, 2014. [Google Scholar]
- Pradhan, Y.; Upreti, S.R.; KC, N.P.; Ashish, K.; Khadka, N.; Syed, U.; Kinney, M.V.; Adhikari, R.K.; Shrestha, P.R.; Thapa, K. Newborn survival in Nepal: A decade of change and future implications. Health Policy Plan. 2012, 27, iii57–Iii71. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, S.; Maqsood, S.; Zakar, R.; Zakar, M.Z.; Fischer, F. Continuum of care in maternal, newborn and child health in Pakistan: Analysis of trends and determinants from 2006 to 2012. BMC Health Serv. Res. 2017, 17, 189. [Google Scholar] [CrossRef] [PubMed]
- Tinker, A.; Parker, R.; Lord, D.; Grear, K. Advancing newborn health: The saving newborn lives initiative. Glob. Public Health 2010, 5, 28–47. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Newborn Death and Illness. Millennium Development goal (mdg) 4. Available online: http://www.who.int/pmnch/media/press_materials/fs/fs_newborndealth_illness/en/ (accessed on 4 February 2015).
- Nepal Demographic and Health Survey 2011; Ministry of Health and Population (MOHP), New ERA: Kathmandu, Nepal; ICF International Inc.: Calverton, MD, USA, 2012.
- Bangladesh Demographic and Health Survey 2011; National Institute of Population Research and Training (NIPORT): Dhaka, Bangladesh; Mitra and Associates, and ICF International: Calverton, MD, USA, 2013.
- Nigeria Demographic and Health Survey 2013; National Population Commission (NPC) and ICF International: Rockville, MD, USA, 2014.
- Zimbabwe Demographic and Health Survey 2010–2011; Zimbabwe National Statistics Agency (ZIMSTAT) and ICF International: Calverton, MD, USA, 2012.
- Jehan, I.; Harris, H.; Salat, S.; Zeb, A.; Mobeen, N.; Pasha, O.; McClure, E.M.; Moore, J.; Wright, L.L.; Goldenberg, R.L. Neonatal mortality, risk factors and causes: A prospective population-based cohort study in Urban Pakistan. Bull. World Health Organ. 2009, 87, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Nesbitt, R.C.; Lohela, T.J.; Manu, A.; Vesel, L.; Okyere, E.; Edmond, K.; Owusu-Agyei, S.; Kirkwood, B.R.; Gabrysch, S. Quality along the continuum: A health facility assessment of intrapartum and postnatal care in Ghana. PLoS ONE 2013, 8, e81089. [Google Scholar] [CrossRef] [PubMed]
- Spector, J.M.; Lashoher, A.; Agrawal, P.; Lemer, C.; Dziekan, G.; Bahl, R.; Mathai, M.; Merialdi, M.; Berry, W.; Gawande, A.A. Designing the who safe childbirth checklist program to improve quality of care at childbirth. Int. J. Gynecol. Obstet. 2013, 122, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Spector, J.M.; Agrawal, P.; Kodkany, B.; Lipsitz, S.; Lashoher, A.; Dziekan, G.; Bahl, R.; Merialdi, M.; Mathai, M.; Lemer, C. Improving quality of care for maternal and newborn health: Prospective pilot study of the who safe childbirth checklist program. PLoS ONE 2012, 7, e35151. [Google Scholar] [CrossRef] [PubMed]
- Lawn, J.E.; Cousens, S.N.; Darmstadt, G.L.; Bhutta, Z.A.; Martines, J.; Paul, V.; Knippenberg, R.; Fogstad, H. 1 year after the lancet neonatal survival series—Was the call for action heard? Lancet 2006, 367, 1541–1547. [Google Scholar] [CrossRef]
- National Programme for Family Planning and Primary Health Care, 2010. Available online: http://www.pc.gov.pk/downloads/pc1-forms_vertical-health-program/National%20Program%20for%20Family%20Planning.pdf (accessed on 6 January 2015).
- Opportunities for Newborn Survival in Pakistan, Save the Children. 2009. Available online: http://www.healthynewbornnetwork.org/sites/default/files/resources/Opportunities%20for%20nb%20survival%202009_0.pdf (accessed on 4 April 2015).
- National Health Policy 2001—The Way Forward. Ministry of Health, Government of Pakistan. Available online: http://www.nacp.gov.pk/introduction/national_health_policy/NationalHealthPolicy-2001.pdf (accessed on 24 February 2015).
- Pakistan Initiative for Mothers and Newborns (Paiman). Available online: http://paiman.jsi.com/Resources/Docs/wp_2008-09.pdf (accessed on 20 January 2015).
- Mid-Term Evaluation of the National Maternal and Child Health Programme in Pakistan, 2012. Available online: http://www.trfpakistan.org/LinkClick.aspx?fileticket=0WOWUr-6vQI%3D&tabid=2618 (accessed on 28 June 2015).
- People’s Primary Health Care Initiative Sindh, Quarterly Bulletin June 2014. Available online: http://pphisindh.org/pphinew/wordpress/monthly-performance-bulletin/ (accessed on 4 April 2015).
- National Health Policy 2009—Stepping towards Better Health. Ministry of Health, Government of Pakistan. Available online: http://www.wpfpak.org/pdfs/policies/draft_health_policy_zero_draft_19_Feb_2009.pdf (accessed on 29 June 2015).
- Bhutta, Z.A.; Hafeez, A.; Rizvi, A.; Ali, N.; Khan, A.; Ahmad, F.; Bhutta, S.; Hazir, T.; Zaidi, A.; Jafarey, S.N. Reproductive, maternal, newborn, and child health in Pakistan: Challenges and opportunities. Lancet 2013, 381, 2207–2218. [Google Scholar] [CrossRef]
- Hafeez, A.; Mohamud, B.K.; Shiekh, M.R.; Shah, S.A.I.; Jooma, R. Lady health workers programme in pakistan: Challenges, achievements and the way forward. J. Pak. Med. Assoc. 2011, 61, 210. [Google Scholar] [PubMed]
- National Programme for Family Planning and Primary Health Care. Resource Document. Ministry of Health, Pakistan. Available online: https://www.advancingpartners.org/sites/default/files/cadres/policies/ national_program_for_family_planning.pdf (accessed on 6 January 2015).
- National Maternal Newborn and Child Health (Mnch) Program 2006. Available online: http://www.pc.gov.pk/downloads/pc1-forms_vertical-health-program/National%20Maternal% 20Newborn%20and%20Child%20Health%20%20Programme.pdf (accessed on 20 February 2015).
- Thacker, N.; Vashishtha, V.M.; Awunyo-Akaba, J.; Mistry, R.F. Civil society organizations, the implementing partners of the global vaccine action plan. Vaccine 2013, 31, B97–B102. [Google Scholar] [CrossRef] [PubMed]
- Pphi Sindh (People’s Primary Health Care Initiative), June Quarterly Bulletin. Resource Document. PPHI, Sindh, Pakistan. Available online: http://pphisindh.org/pphiweb/index.php/bulletin/ (accessed on 4 April 2015).
- Gonzalez, R.; Merialdi, M.; Lincetto, O.; Lauer, J.; Becerra, C.; Castro, R.; García, P.; Saugstad, O.D.; Villar, J. Reduction in neonatal mortality in Chile between 1990 and 2000. Pediatrics 2006, 117, e949–e954. [Google Scholar] [CrossRef] [PubMed]
- Lawn, J.E.; Blencowe, H.; Oza, S.; You, D.; Lee, A.C.; Waiswa, P.; Lalli, M.; Bhutta, Z.; Barros, A.J.; Christian, P. Every newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar] [CrossRef]
- Corsi, D.J.; Neuman, M.; Finlay, J.E.; Subramanian, S. Demographic and health surveys: A profile. Int. J. Epidemiol. 2012, 41, 1602–1613. [Google Scholar] [CrossRef] [PubMed]


| Data Point | Country | Survey Period | Total No. of Households Interviewed in the DHS | No. of Women Interviewed for Child Mortality | Total No. of Births for Postnatal Newborn Care |
|---|---|---|---|---|---|
| 1 | Pakistan | 1990–1991 | 3591 | 3227 | - |
| Afghanistan | 1995–1996 | - | - | - | |
| Bangladesh | 1993–1994 | 9174 | 8174 | - | |
| Nepal | 1996 | 8082 | 8429 | - | |
| Zimbabwe | 1994 | 5984 | 6128 | - | |
| Ghana | 1993–1994 | 5822 | 4562 | - | |
| Nigeria | 2003 | 7225 | 7620 | - | |
| Ethiopia | 2000 | 14,072 | 15,367 | - | |
| Tanzania | 1996 | 7969 | 8120 | - | |
| 2 | Pakistan | 2006–2007 | 92,340 | 10,023 | - |
| Afghanistan | 2006–2007 | 8278 | 8281 | - | |
| Bangladesh | 2007 | 10,400 | 10,996 | - | |
| Nepal | 2006 | 8707 | 10,793 | - | |
| Zimbabwe | 2005–2006 | 9285 | 8907 | - | |
| Ghana | 2003 | 6251 | 5691 | - | |
| Nigeria | 2008 | 34,070 | 33,385 | - | |
| Ethiopia | 2005 | 13,721 | 14,070 | - | |
| Tanzania | 2004–2005 | 9735 | 10,329 | - | |
| 3 | Pakistan | 2012–2013 | 14,000 | 13,558 | 4246 |
| Afghanistan | 2010 | 22,351 | 47,848 | - | |
| Bangladesh | 2011 | 17,141 | 17,842 | 4652 | |
| Nepal | 2011 | 10,826 | 12,674 | 2030 | |
| Zimbabwe | 2010–2011 | 9756 | 9171 | 2448 | |
| Ghana | 2008 | 11,778 | 4916 | - | |
| Nigeria | 2013 | 38,522 | 38,948 | 12,473 | |
| Ethiopia | 2010–2011 | 16,706 | 16,515 | - | |
| Tanzania | 2009–2010 | 9623 | 10,139 | - |
| Countries | Data Point 1 | Data Point 2 | Data Point 3 | Trends | Expected Year of Achieving MDG4 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Under-Five Mortality (5M) | Neonatal Mortality (NM) | 5M | NM | 5M | NM | 5M | NM | ||
| Pakistan | 117 | 51 | 94 | 54 | 89 | 55 | ↓ | ↑ | 2025 |
| Afghanistan | 80 | 25 | 72 | 25 | 71 | 25 | ↓ | no change | 2025 |
| Bangladesh | 133 | 52 | 65 | 37 | 53 | 32 | ↓ | ↓ | Achieved in 2012 |
| Nepal | 118 | 50 | 61 | 33 | 54 | 33 | ↓ | no change | Achieved in 2010 |
| Zimbabwe | 62 | 25 | 70 | 25 | 84 | 31 | ↑ | ↑ | 2025 |
| Ghana | 119 | 41 | 111 | 43 | 80 | 30 | ↓ | ↓ | 2025 |
| Nigeria | 201 | 48 | 157 | 40 | 128 | 37 | ↓ | ↓ | 2025 |
| Ethiopia | 166 | 49 | 123 | 39 | 88 | 37 | ↓ | ↓ | Achieved in 2014 |
| Tanzania | 143 | 33 | 106 | 30 | 81 | 26 | ↓ | ↓ | Achieved in 2013 |
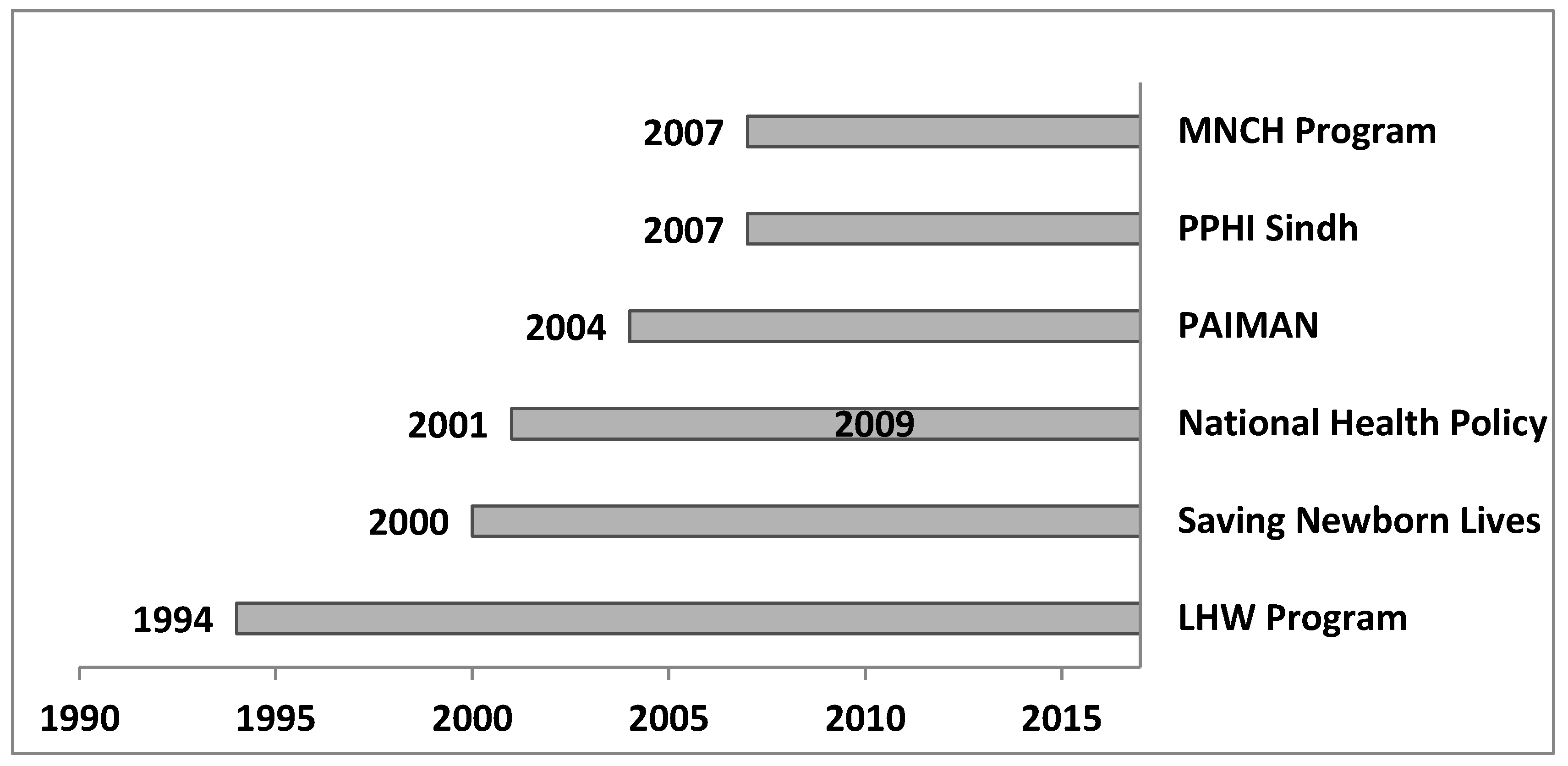
| Program | Year Started | Scale of the Program | MNCH Components |
|---|---|---|---|
| National Program for Family Planning and Health Care (LHW program) [34] | 1994 | Nationwide (rural population) |
|
| Saving Newborn Lives [35] | 2000 | Few districts (rural population) |
|
| National Health Policy 2001 [36] | 2001 | Nationwide |
|
| Pakistan Initiative for Mothers and Newborns [37] | 2004 | 24 districts |
|
| Maternal, Newborn and Child Health Program [38] | 2007 | Nationwide |
|
| People’s Primary Health Care Initiative [39] | 2007 | One province (Sindh) |
|
| National Health Policy 2009 [40] | 2009 | Nationwide |
|
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, M.; Won, Y. Cross-National Systematic Review of Neonatal Mortality and Postnatal Newborn Care: Special Focus on Pakistan. Int. J. Environ. Res. Public Health 2017, 14, 1442. https://doi.org/10.3390/ijerph14121442
Ahmed M, Won Y. Cross-National Systematic Review of Neonatal Mortality and Postnatal Newborn Care: Special Focus on Pakistan. International Journal of Environmental Research and Public Health. 2017; 14(12):1442. https://doi.org/10.3390/ijerph14121442
Chicago/Turabian StyleAhmed, Mansoor, and Youngjoon Won. 2017. "Cross-National Systematic Review of Neonatal Mortality and Postnatal Newborn Care: Special Focus on Pakistan" International Journal of Environmental Research and Public Health 14, no. 12: 1442. https://doi.org/10.3390/ijerph14121442
APA StyleAhmed, M., & Won, Y. (2017). Cross-National Systematic Review of Neonatal Mortality and Postnatal Newborn Care: Special Focus on Pakistan. International Journal of Environmental Research and Public Health, 14(12), 1442. https://doi.org/10.3390/ijerph14121442




