Mercury Exposure and Heart Diseases
Abstract
:1. Introduction
2. Materials and Methods
3. Chemical Forms and Toxicity of Mercury
4. Cardiovascular Effect of Mercury
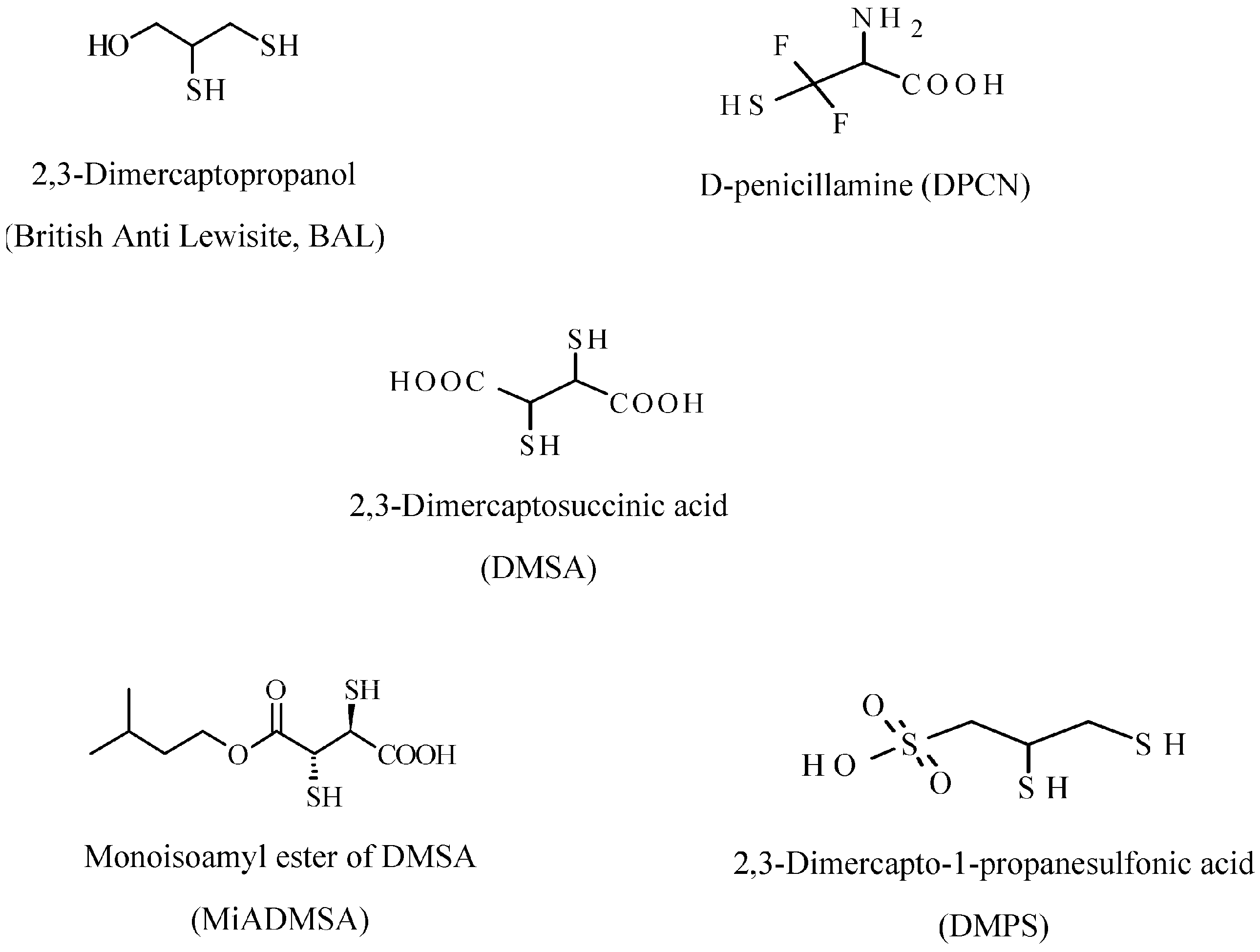
5. Mercury Chelating Agents
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Bergdahl, I.A.; Schütz, A.; Ahlqwist, M.; Bengtsson, C.; Lapidus, L.; Lissner, L.; Hulten, B. Methylmercury and inorganic mercury in serum-correlation to fish consumption and dental amalgam in a cohort of women born in 1922. Environ. Res. 1998, 77, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Swain, E.B.; Jakus, P.M.; Rice, G.; Lupi, F.; Maxson, P.A.; Pacyna, J.M.; Penn, A.; Spiegel, S.J.; Veiga, M.M. Socioeconomic consequences of mercury use and pollution. Ambio 2007, 36, 45–61. [Google Scholar] [CrossRef]
- Geelhard, G. The record of an early mercurial cure in the history of syphilis with a case history of a 29 year old white male Renaissance genius. Aust. N. Z. J. Surg. 1978, 48, 589–594. [Google Scholar] [CrossRef]
- Zhao, H.L.; Zhu, X.; Sui, Y. The short-lived Chinese emperors. J. Am. Geriatr. Soc. 2006, 54, 1295–1296. [Google Scholar] [CrossRef] [PubMed]
- Tsubaki, T.; Irukajama, K. Minamata Disease. Methylmercury poisoning in Minamata and Niigata, Japan. In Minamata Disease. Methylmercury Poisoning in Minamata and Niigata, Japan; Tsubaki, T., Irukajama, K., Eds.; Kodansha: Tokyo, Japan, 1997; p. 317. [Google Scholar]
- Carocci, A.; Rovito, N.; Sinicropi, M.S.; Genchi, G. Mercury toxicity and neurodegenerative effects. Rev. Environ. Contam. Toxicol. 2014, 229, 1–18. [Google Scholar] [PubMed]
- Bakir, F.; Damluji, S.F.; Amin-Zaki, L.; Murtadha, M.; Khalidi, A.; Al-Rawi, N.Y.; Tikriti, S.; Dahahir, H.I.; Clarkson, T.W.; Smith, J.C.; et al. Methylmercury poisoning in Iraq. Science 1973, 181, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Guzzi, G.; la Porta, C.A. Molecular mechanism triggered by mercury. Toxicology 2008, 244, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Compeau, G.C.; Bartha, R. Sulfate-reducing bacteria: Principal methylators of mercury in anoxic estuarine sediment. Appl. Environ. Microbiol. 1985, 50, 498–502. [Google Scholar] [PubMed]
- Morel, F.M.M.; Kraepiel, A.M.I.; Amyot, M. The chemical cycle and bioaccumulation of mercury. Annu. Rev. Ecol. Syst. 1998, 29, 543–566. [Google Scholar] [CrossRef]
- Carocci, A.; Catalano, A.; Lauria, G.; Sinicropi, M.S.; Genchi, G. A review on mercury toxicity in foods. In Food Toxicology; CRC Press: Boca Raton, FL, USA, 2016; Volume 16, pp. 315–326. [Google Scholar]
- Gribble, M.O.; Cheng, A.; Berger, R.D.; Rosman, L.; Guallar, E. Mercury Exposure and Heart Rate Variability: A Systematic Review. Curr. Environ. Health Rep. 2015, 2, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Roman, H.A.; Walsh, T.L.; Coull, B.A.; Dewailly, É.; Guallar, E.; Hattis, D.; Mariën, K.; Schwartz, J.; Stern, A.H.; Virtanen, J.K.; et al. Evaluation of the cardiovascular effects of methylmercury exposures: Current evidence supports development of a dose-response function for regulatory benefits analysis. Environ. Health Perspect. 2011, 119, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Exposure to Mercury: A Major Public Health Concern, Preventing Disease through Healthy Environment; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Sinicropi, M.S.; Caruso, A.; Capasso, A.; Palladino, C.; Panno, A.; Saturnino, C. Heavy metals: Toxicity and carcinogenicity. Pharmacologyonline 2010, 2, 329–333. [Google Scholar]
- Carocci, A.; Catalano, A.; Lauria, G.; Sinicropi, M.S.; Genchi, G. Lead toxicity, antioxidant defense and environment. Rev. Environ. Contam. Toxicol. 2016, 238, 45–67. [Google Scholar] [PubMed]
- Sinicropi, M.S.; Amantea, D.; Caruso, A.; Saturnino, C. Chemical and biological properties of toxic metals and use of chelating agents for the pharmacological treatment of metal poisoning. Arch. Toxicol. 2010, 84, 501–520. [Google Scholar] [CrossRef] [PubMed]
- Bernhoft, R.A. Mercury toxicity and treatment: A review of the literature. J. Environ. Public Health 2012. [Google Scholar] [CrossRef] [PubMed]
- Pirrone, N.; Mahaffey, K.R. Dynamics of Mercury Pollution on Regional and Global Scales: Atmospheric Processes and Human Exposures around the World; Springer: New York, NY, USA, 2005; p. 748. [Google Scholar]
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Mercury, ATSDR, Public Health Service; US Department of Health and Human Services: Washington, DC, USA, 1999.
- Davidson, P.W.; Myers, G.J.; Weiss, B.; Shamlaye, C.F.; Cox, C. Prenatal methyl mercury exposure from fish consumption and child development: A review of evidence and perspectives from the Seychelles Child Development Study. Neurotoxicology 2006, 27, 1106–1109. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, S.; Bullock, R.; Ebinghaus, R.; Engstrom, D.; Feng, X.; Fitzgerald, W.; Pirrone, N.; Prestbo, E.; Seigneur, C. A synthesis of progress and uncertainties in attributing the sources of mercury in deposition. Ambio 2007, 36, 19–32. [Google Scholar] [CrossRef]
- Pirrone, N.; Cinnirella, S.; Feng, X.; Finkelman, R.B.; Friedli, H.R.; Leaner, J. Global mercury emissions to the atmosphere from anthropogenic and natural sources. Atmos. Chem. Phys. 2010, 10, 5951–5964. [Google Scholar] [CrossRef]
- Biester, H.; Müller, G.; Schöler, H.F. Binding and mobility of mercury in soils contaminated by emissions from chlor-alkali plants. Sci. Total Environ. 2002, 284, 191–193. [Google Scholar] [CrossRef]
- Novoa-Munoz, J.C.; Pontevedra-Pombal, X.; Martinez-Cortizas, A.; Garcia-Rodeja Gayoso, E. Mercury accumulation in upland acid forest ecosystems nearby a coal fired power-plant in Southwest Europe (Galicia, NW Spain). Sci. Total Environ. 2008, 394, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Ballatori, N.; Clarkson, T.W. Biliary secretion of glutathione and of glutathione-metal complexes. Fundam. Appl. Toxicol. 1985, 5, 816–831. [Google Scholar] [CrossRef]
- Ullrich, S.M.; Tanton, T.W.; Abdrashitova, S.A. Mercury in the aquatic environment: A review of factors affecting methylation. Crit. Rev. Environ. Sci. Technol. 2001, 31, 241–293. [Google Scholar] [CrossRef]
- Fitzgerald, W.F.; Lamborg, C.H.; Hammerschmidt, C.R. Marine biogeochemical cycling of mercury. Chem. Rev. 2007, 107, 641–662. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, T.W.; Vyas, J.B.; Ballatori, N. Mechanisms of mercury disposition in the body. Am. J. Ind. Med. 2007, 50, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, T.W.; Magos, L. The toxicology of mercury and its chemical compounds. Crit. Rev. Toxicol. 2006, 36, 609–662. [Google Scholar] [CrossRef] [PubMed]
- Dabeka, R.; McKenzie, A.D.; Forsyth, D.S.; Conacher, H.B. Survey of total mercury in some edible fish and shellfish species collected in Canada in 2002. Food Addit. Contam. 2004, 21, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Tacon, A.G.J.; Metian, M. Fish matters: Importance of aquatic foods in human nutrition and global food supply. Rev. Fish. Sci. 2013, 21, 22–38. [Google Scholar] [CrossRef]
- Guzzi, G.; Grandi, M.; Cattaneo, C.; Calza, S.; Minoia, C.; Ronchi, A.; Gatti, A.; Severi, G. Dental amalgam and mercury levels in autopsy tissues: Food for thought. Am. J. Forensic Med. Pathol. 2006, 27, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Bertilsson, L.; Neujahr, H.Y. Methylation of mercury compounds by methylcobalamin. Biochemistry 1971, 10, 2805–2808. [Google Scholar] [PubMed]
- International Programme on Chemical Safety (IPCS). Methylmercury. Environmental Health Criteria 101; World Health Organization: Geneva, Switzerland, 1990. [Google Scholar]
- Salonen, J.T.; Seppänen, K.; Nyyssönen, K.; Korpela, H.; Kauhanen, J.; Kantola, M.; Tuomilehto, J.; Esterbauer, H.; Tatzber, F.; Salonen, R. Intake of mercury from fish, lipid peroxidation, and the risk of myocardial infarction and coronary, cardiovascular, and any death in eastern Finnish men. Circulation 1995, 91, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Magos, L.; Webb, M.; Clarkson, T.W. The interactions of selenium with cadmium and mercury. Crit. Rev. Toxicol. 1980, 8, 1–42. [Google Scholar] [CrossRef] [PubMed]
- Salonen, J.T.; Seppänen, K.; Lakka, T.A.; Salonen, R.; Kaplan, G.A. Mercury accumulation and accelerated progression of carotid atherosclerosis: A population based prospective 4-year follow-up study in men in eastern Finland. Atherosclerosis 2000, 148, 265–273. [Google Scholar] [CrossRef]
- Guallar, E.; Sanz-Gallardo, M.I.; van’t Veer, P.; Bode, P.; Aro, A.; Gómez-Aracena, J.; Kark, J.D.; Riemersma, R.A.; Martín-Moreno, J.M.; Kok, F.J. Mercury, fish oils, and the risk of myocardial infarction. N. Engl. J. Med. 2002, 347, 1747–1754. [Google Scholar] [CrossRef] [PubMed]
- Yoshizawa, K.; Rimm, E.B.; Morris, J.S.; Spate, V.L.; Hsieh, C.C.; Spiegelman, D.; Stampfer, M.J.; Willett, W.C. Mercury and the risk of coronary heart disease in men. N. Engl. J. Med. 2002, 347, 1755–1760. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, T.W.; Magos, L.; Myers, G.J. The toxicology of mercury—Current exposures and clinical manifestations. N. Engl. J. Med. 2003, 349, 1731–1737. [Google Scholar] [CrossRef] [PubMed]
- Shenker, B.J.; Guo, T.L.; Shapiro, I.M. Low-level methylmercury exposure causes human T-cells to undergo apoptosis: Evidence of mitochondrial dysfunction. Environ. Res. 1998, 77, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Ganther, H.E.; Sunde, M.L. Effect of tuna fish and selenium on the toxicity of methylmercury: A progress report. J. Food Sci. 1974, 39, 1–5. [Google Scholar] [CrossRef]
- Stoewsand, G.S.; Bache, C.A.; Lisk, D.J. Dietary selenium protection of methylmercury intoxication of Japanese quail. Bull. Environ. Contam. Toxicol. 1974, 11, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Sumino, K.; Yamamoto, R.; Kitamura, S.A. Role of selenium against methylmercury toxicity. Nature 1977, 268, 73–74. [Google Scholar] [CrossRef] [PubMed]
- Seppänen, K.; Kantola, M.; Laatikainen, R.; Nyyssönen, K.; Valkonen, V.P.; Kaarlöpp, V.; Salonen, J.T. Effect of supplementation with organic selenium on mercury status as measured by mercury in pubic hair. J. Trace Elem. Med. Biol. 2000, 14, 84–89. [Google Scholar] [CrossRef]
- Su, J.Y.; Chen, W.J. The effects of methylmercury on isolated cardiac tissues. Am. J. Pathol. 1979, 95, 753–764. [Google Scholar] [PubMed]
- Halbach, S.; Schonsteiner, G.; Vierling, W. The action of organic mercury compounds on the function of isolated mammalian heart muscle. Eur. J. Pharmacol. 1989, 167, 255–264. [Google Scholar] [CrossRef]
- Massaroni, L.; Oliveira, E.M.; Stefanon, I.; Vassallo, D.V. Effects of mercury on the mechanical and electrical activity of the Langendorff-perfused rat heart. Braz. J. Med. Biol. Res. 1992, 25, 861–864. [Google Scholar] [PubMed]
- Oliveira, E.M.; Vassallo, D.V.; Sarkis, J.J.F.; Mill, J.G. Mercury effects on the contractile activity of isolated heart muscle. Toxicol. Appl. Pharmacol. 1994, 128, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Rodgers, D.A.; Duhart, H.M.; Ali, S.F. Mercuric chloride-induced reactive oxygen species and its effect on antioxidant enzymes in different regions of rat brain. J. Environ. Sci. Health B 1997, 32, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C. Role of Mercury Toxicity in Hypertension, Cardiovascular Disease, and Stroke. J. Clin. Hyperten. 2011, 13, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Fillion, M.; Mergler, D.; Sousa Passos, C.J.; Larribe, F.; Lemire, M.; Guimarães, J.R.D. A preliminary study of mercury exposure and blood pressure in the Brazilian Amazon. Environ. Health 2006, 5, 29. [Google Scholar] [CrossRef] [PubMed]
- Valera, B.; Dewailly, E.; Poirier, P. Cardiac autonomic activity and blood pressure among Nunavik Inuit adults exposed to environmental mercury: A cross-sectional study. Environ. Health 2008, 7, 29. [Google Scholar] [CrossRef] [PubMed]
- Valera, B.; Dewailly, E.; Poirier, P. Environmental mercury exposure and blood pressure among Nunavik Inuit adults. Hypertension 2009, 54, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Valera, B.; Dewailly, E.; Poirier, P. Impact of mercury exposure on blood pressure and cardiac autonomic activity among Cree adults (James Bay, Quebec, Canada). Environ. Res. 2011, 111, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Valera, B.; Muckle, G.; Poirier, P.; Jacobson, S.W.; Jacobson, J.L.; Dewailly, E. Cardiac autonomic activity and blood pressure among Inuit children exposed to mercury. Neurotoxicology 2012, 33, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Valera, B.; Dewailly, E.; Poirier, P. Association between methylmercury and cardiovascular risk factors in a native population of Quebec (Canada): A retrospective evaluation. Environ. Res. 2013, 120, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Thurston, S.W.; Bovet, P.; Myers, G.; Davidson, P.W.; Georger, L.A.; Shamlaye, C.; Clarkson, T.W. Does prenatal methylmercury exposure from fish consumption affect blood pressure in childhood? Neurotoxicology 2007, 28, 924–930. [Google Scholar] [CrossRef] [PubMed]
- Grandjean, P.; Murata, K.; Budtz-Jorgensen, E.; Weihe, P. Cardiac autonomic activity in methylmercury neurotoxicity: 14-Year follow-up of a Faroese birth cohort. J. Pediatr. 2004, 144, 169–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bastos, W.R.; Gomes, J.P.O.; Oliveira, R.C.; Almeida, R.; Nascimento, E.L.; Bernardi, J.V.E.; Drude de Lacerda, L.; da Silveira, E.G.; Pfeiffer, W.C. Mercury in the environment and riverside population in the Madeira River Basin, Amazon, Brazil. Sci. Total Environ. 2006, 368, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C. The role of mercury and cadmium heavy metals in vascular disease, hypertension, coronary heart disease, and myocardial infarction. Altern. Ther. Health Med. 2007, 13, S128–S133. [Google Scholar] [PubMed]
- Virtanen, J.K.; Voutilainen, S.; Rissanen, T.H.; Mursu, J.; Tuomainen, T.P.; Korhonen, M.J.; Valkonen, V.P.; Seppänen, K.; Laukkanen, J.A.; Salonen, J.T. Mercury, fish oils, and risk of acute coronary events and cardiovascular disease, coronary heart disease, and all-cause mortality in men in Eastern Finland. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.M.; Lund, B.O.; Woods, J.S. Reactivity of Hg(II) with superoxide: Evidence for the catalytic dismutation of superoxide by Hg(II). J. Biochem. Toxicol. 1991, 6, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Park, S.T.; Lim, K.T.; Chung, Y.T.; Kim, S.U. Methylmercury-induced neurotoxicity in cerebral neuron culture is blocked by antioxidants and NMDA receptor antagonists. Neurotoxicology 1996, 17, 37–45. [Google Scholar] [PubMed]
- Clarkson, T.W. The toxicology of mercury. Crit. Rev. Clin. Lab. Sci. 1997, 34, 369–403. [Google Scholar] [CrossRef] [PubMed]
- Magos, L. Physiology and toxicology of mercury. Met. Ions Biol. Syst. 1997, 34, 321–370. [Google Scholar] [PubMed]
- Ehara, S.; Ueda, M.; Naruko, T.; Haze, K.; Itoh, A.; Otsuka, M.; Komatsu, R.; Matsuo, T.; Itabe, H.; Takano, T. Elevated levels of oxidized low density lipoprotein show a positive relationship with the severity of acute coronary syndromes. Circulation 2001, 103, 1955–1960. [Google Scholar] [CrossRef] [PubMed]
- Kobal, A.B.; Horvat, M.; Prezelj, M.; Briski, A.S.; Krsnik, M.; Dizdarevic, T.; Mazej, D.; Falnoga, I.; Stibilj, V.; Arneric, N.; et al. The impact of long-term past exposure to elemental mercury on antioxidative capacity and lipid peroxidation in mercury miners. J. Trace Elem. Med. Biol. 2004, 17, 261–274. [Google Scholar] [CrossRef]
- Cuvin-Aralar, M.L.; Furness, R.W. Mercury and selenium interaction: A review. Ecotoxicol. Environ. Saf. 1991, 21, 348–364. [Google Scholar] [CrossRef]
- Farina, M.; Aschner, M.; Rocha, J.B.T. Oxidative stress in MeHg-induced neurotoxicity. Toxicol. Appl. Pharmacol. 2011, 256, 405–417. [Google Scholar] [CrossRef] [PubMed]
- Magos, L.; Clarkson, T.W. Overview of the clinical toxicity of mercury. Ann. Clin. Biochem. 2006, 43, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Valko, M.; Rhodes, C.J.; Moncol, J.; Izakovic, M.; Mazur, M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem. Biol. Interact. 2006, 160, 1–40. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.H.; Huang, Y.L.; Huang, S.F. Lipid peroxidation of rats administered with methyl mercuric chloride. Biol. Trace Elem. Res. 1996, 54, 33–41. [Google Scholar] [CrossRef] [PubMed]
- InSug, O.; Datar, S.; Koch, C.J.; Shapiro, I.M.; Shenker, B.J. Mercuric compounds inhibit human monocyte function by inducing apoptosis: Evidence for formation of reactive oxygen species, development of mitochondrial membrane permeability transition and loss of reductive reserve. Toxicology 1997, 124, 211–224. [Google Scholar] [CrossRef]
- Gonzalvo, M.C.; Gil, F.; Hernandez, A.F.; Villanueva, E.; Pla, A. Inhibition of paraoxonase activity in human liver microsomes by exposure to EDTA, metals and mercurials. Chem. Biol. Interact. 1997, 105, 169–179. [Google Scholar] [CrossRef]
- Salonen, J.T.; Malin, R.; Tuomainen, T.P.; Nyyssönen, K.; Lakka, T.A.; Lehtimäki, T. Polymorphism in high density lipoprotein paraoxonase gene and risk of acute myocardial infarction in men: Prospective nested case-control study. BMJ 1999, 319, 487–488. [Google Scholar] [CrossRef] [PubMed]
- Kulka, M. A review of paraoxonase 1 properties and diagnostic applications. Pol. J. Vet. Sci. 2016, 19, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Mallat, Z.; Lambeau, G.; Tedgui, A. Lipoprotein-associated and secreted phospholipases A2 in cardiovascular disease: Roles as biological effectors and biomarkers. Circulation 2010, 122, 2183–2200. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C. The role of mercury in cardiovascular disease. J. Cardiovasc. Dis. Diagn. 2014, 2, 1–8. [Google Scholar] [CrossRef]
- Salonen, J.T.; Alfthan, G.; Huttunen, J.K.; Pikkarainen, J.; Puska, P. Association between cardiovascular death and myocardial infarction and serum selenium in a matched-pair longitudinal study. Lancet 1982, 24, 175–179. [Google Scholar] [CrossRef]
- Salonen, J.T.; Ylä-Herttuala, S.; Yamamoto, R.; Butler, S.; Korpela, H.; Salonen, R.; Nyyssönen, K.; Palinski, W.; Witztum, J.L. Autoantibody against oxidized LDL and progression of carotid atherosclerosis. Lancet 1992, 339, 883–887. [Google Scholar] [CrossRef]
- Levander, O.A. A global view of human selenium nutrition. Annu. Rev. Nutr. 1987, 7, 227–250. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.M.; Arthur, J.R. Selenium, selenoproteins and human health: A review. Public Health Nutr. 2001, 4, 593–599. [Google Scholar] [CrossRef] [PubMed]
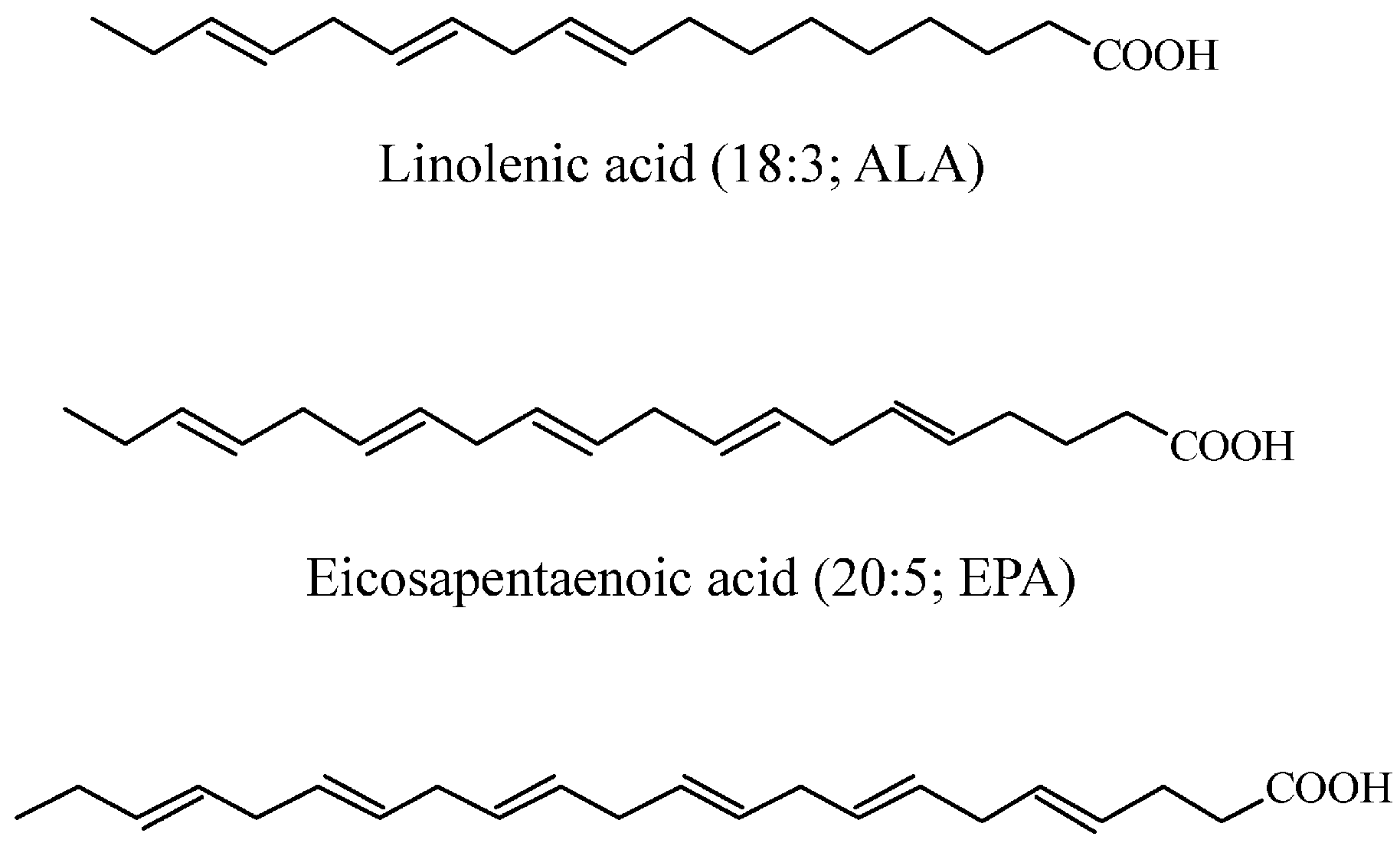
- Clandinin, M.T.; Cheema, S.; Field, C.J.; Garg, M.L.; Venkatraman, J.; Clandinin, T.R. Dietary fat: Exogenous determination of membrane structure and cell function. FASEB J. 1991, 5, 2761–2769. [Google Scholar] [PubMed]
- Vanden Heuvel, J.P. Diet, fatty acids, and regulation of genes important for heart disease. Curr. Atheroscler. Rep. 2004, 6, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Rimm, E.B. Fish intake, contaminants, and human health: Evaluating the risks and the benefits. JAMA 2006, 296, 1885–1899. [Google Scholar] [CrossRef] [PubMed]
- Furieri, L.B.; Fioresi, M.; Junior, R.F.R.; Bartolomé, M.V.; Fernandes, A.A.; Cachofeiro, V.; Lahera, V.; Salaices, M.; Stefanon, I.; Vassallo, D.V. Exposure to low mercury concentration in vivo impairs myocardial contractile function. Toxicol. Appl. Pharmacol. 2011, 255, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.M.; Egeland, G.M. Fish consumption, mercury exposure, and heart diseases. Nutr. Rev. 2004, 62, 68–72. [Google Scholar] [PubMed]
- Mozaffarian, D.; Shi, P.L.; Morris, J.S.; Spiegelman, D.; Grandjean, P.; Siscovick, D.S.; Willett, W.C.; Rimm, E.B. Mercury exposure and risk of cardiovascular disease in two U.S. cohorts. N. Engl. J. Med. 2011, 364, 1116–1125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flora, S.J.; Pachauri, V. Chelation in metal intoxication. Int. J. Environ. Res. Public Health 2010, 7, 2745–2788. [Google Scholar] [CrossRef] [PubMed]
- Ford, M.D.; Delaney, K.A.; Ling, L.J.; Erickson, T. Clinical Toxicology; W.B. Saunders Company: Philadelphia, PA, USA, 2001. [Google Scholar]


© 2017 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Genchi, G.; Sinicropi, M.S.; Carocci, A.; Lauria, G.; Catalano, A. Mercury Exposure and Heart Diseases. Int. J. Environ. Res. Public Health 2017, 14, 74. https://doi.org/10.3390/ijerph14010074
Genchi G, Sinicropi MS, Carocci A, Lauria G, Catalano A. Mercury Exposure and Heart Diseases. International Journal of Environmental Research and Public Health. 2017; 14(1):74. https://doi.org/10.3390/ijerph14010074
Chicago/Turabian StyleGenchi, Giuseppe, Maria Stefania Sinicropi, Alessia Carocci, Graziantonio Lauria, and Alessia Catalano. 2017. "Mercury Exposure and Heart Diseases" International Journal of Environmental Research and Public Health 14, no. 1: 74. https://doi.org/10.3390/ijerph14010074







