Antenatal Clinic and Stop Smoking Services Staff Views on “Opt-Out” Referrals for Smoking Cessation in Pregnancy: A Framework Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
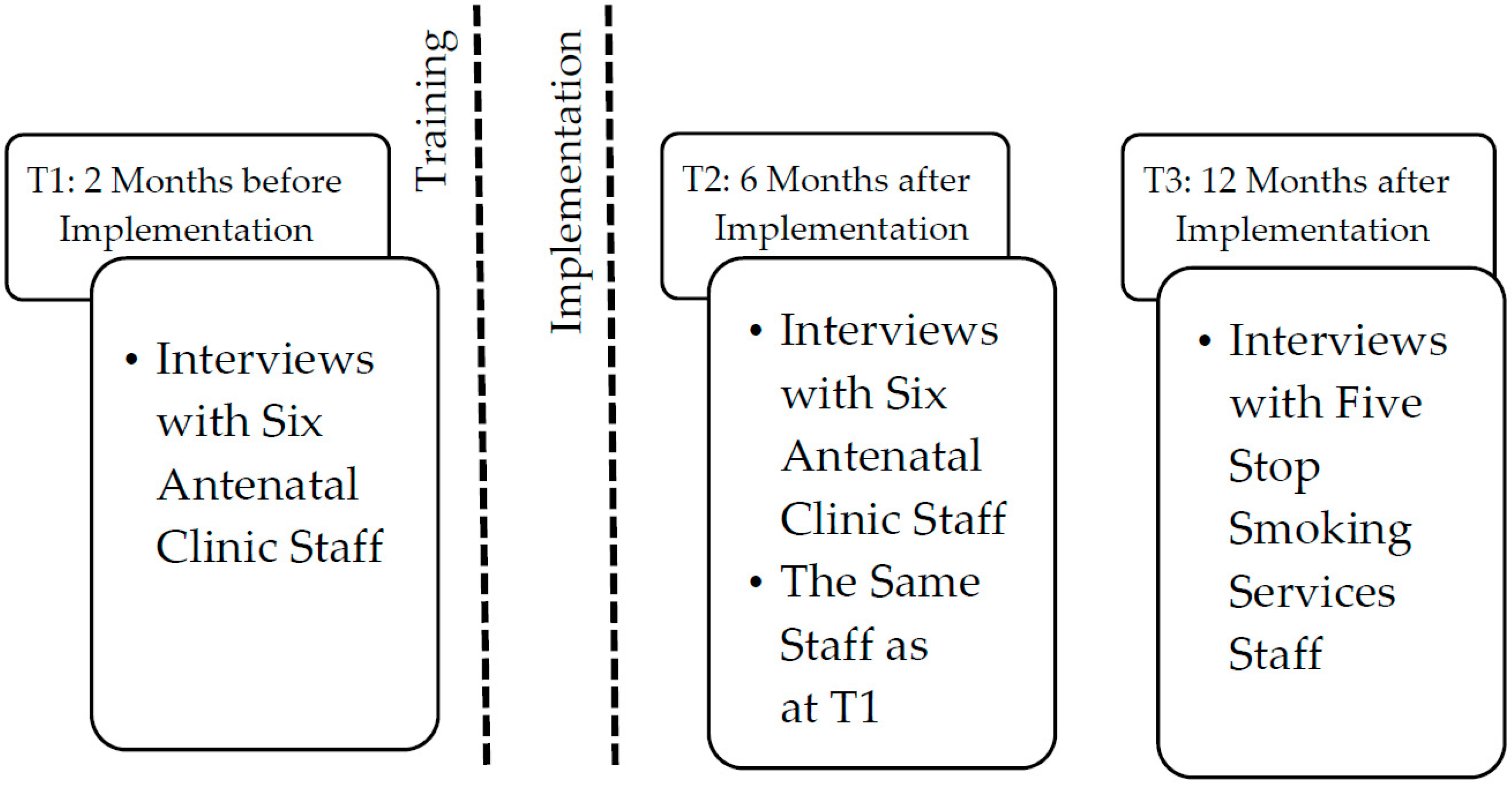
2.2. Procedure and Participants
2.3. Ethical Considerations
2.4. Analysis
3. Results
3.1. Views on Implementation of the Pathway
3.1.1. Perceived Impact on Professional Roles
“Just the fact that they keep giving us more jobs here. We get more and more jobs. We haven’t got enough time to actually do all the jobs.”(p. 5, HSW, Before)
“To begin with there was a lot more (referrals) than there is now. It gave us quite a big workload, but we’ve worked through it, there’s SOPs (standard operating procedures) on what we should do and how it’s to be done and as soon as that was put in to place it was a hell of a lot easier to do.”(p. 10, SSS, After)
“I think the difficulty was that with many of our other referrals people are choosing to refer themselves and they’re fully aware of exactly what they’re being referred in to. That was the difficulty with these women. So I guess in that sense they didn’t always get the same as that other referral, because they didn’t know why we were calling them. And that’s why sometimes it took a lot more work.”(p. 7, SSS, After)
3.1.2. Confidence in Administering the Pathway
“I think that’s how they might see it, some of them, that you’re either being patronizing or you’re accusing them of smoking when they don’t, which I’m not going to be doing either, I’m just going to be asking a question for their wellbeing, it’s not my wellbeing, it’s their we’re concerned with.”(p. 2, HSW, Before)
“I feel a bit bad because I’ll know my next question from them is ‘well why is there (high CO reading) and what does it mean and what’s going to happen’, and I’ll have to say ‘I’m sorry, look I don’t know!’”(p. 2, HSW, After)
“Yeah it’s a really difficult number (4–7 ppm), because obviously it is triggering a referral, but we just didn’t know why (…) so I tried to find some research about that, but there’s nothing out there. Nobody got back to me. I rang [the CO monitor manufacturer] as well and tried to get information from them as to why we might get false readings.”(p. 7, SSS, After)
3.1.3. Engaging the Women
“We don’t ask them, we tell them that this is a test we’re going to do. I don’t actually ask, but then when I’ve told them what test we’re going to do, I do say ‘is that alright’ and most of them just say ‘yes’ , but a few have refused.”(p. 5, HSW, After)
3.2. Impact of the “Opt-Out” Referral Pathway on the Women
3.2.1. Impact on Non-Smokers with CO Levels ≥ 4 ppm
3.2.2. Impact on Smokers Not Ready to Quit
“I suppose it’s difficult sometimes because there’s women that smoke and have had babies that are perfectly well, so it’s hard to get through to somebody that’s seen that, because they can turn round and say ‘well, my sister’s just had a baby and she smokes and her baby’s absolutely fine, so why should I stop smoking’…But I suppose some people don’t understand the complications as much, so I suppose they should have the options there, that this could happen and that could happen.”(p. 4, HSW, Before)
“I think ‘the ‘opt-out’ pathway’ is just something else that contributes to that drip, drip, drip effect…It may be that they continue to smoke for that pregnancy, but for the next pregnancy they think about it and they’ve quit. You know it’s really hard to measure…”(p. 8, SSS, After)
3.2.3. Impact on Smokers Ready to Make a Positive Change
“With the CO reading we get a lot of clients who say that they are going to face-to-face appointments because we can see the CO reading and they can see how it’s affecting them internally as well as, you know, externally really…because it kind of is a shocker I think to some people.”(p. 9, SSS, After)
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Cnattingius, S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob. Res. 2004, 6 (Suppl. S2), 125–140. [Google Scholar] [CrossRef] [PubMed]
- Shipton, D.; Tappin, D.M.; Vadiveloo, T.; Crossley, J.A.; Aitken, D.A.; Chalmers, J. Reliability of self reported smoking status by pregnant women for estimating smoking prevalence: A retrospective, cross sectional study. BMJ 2009, 339, b4347. [Google Scholar] [CrossRef] [PubMed]
- Pickett, K.E.; Rathouz, P.J.; Kasza, K.; Wakschlag, L.S.; Wright, R. Self-reported smoking, cotinine levels, and patterns of smoking in pregnancy. Paediatr. Perinat. Epidemiol. 2005, 19, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, C.; O’Mara-Eves, A.; Oliver, S.; Caird, J.R.; Perlen, S.M.; Eades, S.J.; Thomas, J. Psychosocial Interventions for Supporting Women to Stop Smoking in Pregnancy. Available online: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001055.pub4/pdf (accessed on 2 August 2016).
- Bauld, L.; Bell, K.; McCullough, L.; Richardson, L.; Greaves, L. The effectiveness of NHS smoking cessation services: A systematic review. J. Public Health (Oxf.) 2010, 32, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Fahy, S.J.; Cooper, S.; Coleman, T.; Naughton, F.; Bauld, L. Provision of smoking cessation support for pregnant women in England: Results from an online survey of NHS stop smoking services for pregnant women. BMC Health Serv. Res. 2014, 14, 107. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Quitting Smoking in Pregnancy and Following Childbirth Commissioning Guide; National Institute for Health and Care Excellence: London, UK, 2010. [Google Scholar]
- McGowan, A.; Hamilton, S.; Barnett, D.; Nsofor, M.; Proudfoot, J.; Tappin, D.M. “Breathe”: The stop smoking service for pregnant women in glasgow. Midwifery 2010, 26, e1–e13. [Google Scholar] [CrossRef] [PubMed]
- Bauld, L.; Hackshaw, L.; Ferguson, J.; Coleman, T.; Taylor, G.; Salway, R. Implementation of routine biochemical validation and an “opt out” referral pathway for smoking cessation in pregnancy. Addiction 2012, 107 (Suppl. S2), 53–60. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.A.; Cooper, S.; Fahy, S.J.; Bowker, K.; Leonardi-Bee, J.; McEwen, A.; Whitemore, R.; Coleman, T. “Opt-Out” Referrals after Identifying Pregnant Smokers Using Exhaled Air Carbon Monoxide: Impact on Engagement with Smoking Cessation Support. Available online: http://tobaccocontrol.bmj.com/content/early/2016/05/25/tobaccocontrol-2015-052662.full (accessed on 2 August 2016).
- Condliffe, L.; McEwen, A.; West, R. The attitude of maternity staff to, and smoking cessation interventions with, childbearing women in london. Midwifery 2005, 21, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, A.; Springett, J.; Karlsson, L.; Hakansson, A.; Ottosson, T. Some lessons from Swedish midwives’ experiences of approaching women smokers in antenatal care. Midwifery 2005, 21, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Randall, S. Midwives’ attitudes to smoking and smoking cessation in pregnancy. Br. J. Midwifery 2009, 17, 642–646. [Google Scholar] [CrossRef]
- Abatemarco, D.J.; Steinberg, M.B.; Delnevo, C.D. Midwives’ knowledge, perceptions, beliefs, and practice supports regarding tobacco dependence treatment. J. Midwifery Womens Health 2007, 52, 451–457. [Google Scholar] [CrossRef] [PubMed]
- The Royal College of Midwives. The Role and Responsibilities of Maternity Support Workers. Available online: https://www.rcm.org.uk/sites/default/files/MSW%20R%26R%20Guide_4.pdf (accessed on 2 August 2016).
- Stenhouse, E.; Adams, L.; Corrigan, O.; Letherby, G.; Bendall, A. Carbon Monoxide Screening in Pregnancy: An Evaluation Study of a Plymouth Pilot Intervention; Plymouth Electronic Archive and Research Library: Plymouth, UK, 2014. [Google Scholar]
- Lorencatto, F.; West, R.; Michie, S. Specifying evidence-based behavior change techniques to aid smoking cessation in pregnancy. Nicotine Tob. Res. 2012, 14, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Bennett, L.; Grant, A.; Jones, S.; Bowley, M.; Heathcote-Elliott, C.; Ford, C.; Jones, A.; Lewis, R.; Munkley, M.; Owen, C.; et al. Models for access to maternal smoking cessation support (MAMSS): A study protocol of a quasi-experiment to increase the engagement of pregnant women who smoke in nhs stop smoking services. BMC Public Health 2014, 14, 1041. [Google Scholar] [CrossRef] [PubMed]
- McEwen, A. Standard Treatment Programme: A Guide to Behavioural Support for Smoking Cessation. Available online: http://documents.tips/health-medicine/standard-treatment-programme.html (accessed on 2 August 2016).
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- Sloan, M.; Campbell, K.A.; Bowker, K.; Coleman, T.; Cooper, S.; Brafman-Price, B.; Naughton, F. Pregnant women’s experiences and views on an “opt-out” referral pathway to specialist smoking cessation support: A qualitative evaluation. Nicotine Tob. Res. 2016, 18, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Hiscock, R.; Murray, S.; Brose, L.S.; McEwen, A.; Bee, J.L.; Dobbie, F.; Bauld, L. Behavioural therapy for smoking cessation: The effectiveness of different intervention types for disadvantaged and affluent smokers. Addict. Behav. 2013, 38, 2787–2796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aveyard, P.; Lawrence, T.; Evans, O.; Cheng, K.K. The influence of in-pregnancy smoking cessation programmes on partner quitting and women’s social support mobilization: A randomized controlled trial [ISRCTN89131885]. BMC Public Health 2005, 5, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lifestyles Statistics Team; Health & Social Care Information Centre. Statistics on Women’s Smoking Status at Time of Delivery: England, Quarter 4—April 2013 to March 2014, Final Report. Available online: http://www.hscic.gov.uk/searchcatalogue?productid=14841&q=title%3a%22Statistics+on+Women%27s+Smoking+Status+at+Time+of+Delivery%22&sort=Relevance&size=10&page=1#top (accessed on 22 June 2015).
- Yar, M.; Dix, D.; Bajekal, M. Socio-demographic characteristics of the healthcare workforce in England and Wales—Results from the 2001 census. Health Stat. Q. 2006, 32, 44–56. [Google Scholar] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]

© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campbell, K.A.; Bowker, K.A.; Naughton, F.; Sloan, M.; Cooper, S.; Coleman, T. Antenatal Clinic and Stop Smoking Services Staff Views on “Opt-Out” Referrals for Smoking Cessation in Pregnancy: A Framework Analysis. Int. J. Environ. Res. Public Health 2016, 13, 1004. https://doi.org/10.3390/ijerph13101004
Campbell KA, Bowker KA, Naughton F, Sloan M, Cooper S, Coleman T. Antenatal Clinic and Stop Smoking Services Staff Views on “Opt-Out” Referrals for Smoking Cessation in Pregnancy: A Framework Analysis. International Journal of Environmental Research and Public Health. 2016; 13(10):1004. https://doi.org/10.3390/ijerph13101004
Chicago/Turabian StyleCampbell, Katarzyna Anna, Katharine Anna Bowker, Felix Naughton, Melanie Sloan, Sue Cooper, and Tim Coleman. 2016. "Antenatal Clinic and Stop Smoking Services Staff Views on “Opt-Out” Referrals for Smoking Cessation in Pregnancy: A Framework Analysis" International Journal of Environmental Research and Public Health 13, no. 10: 1004. https://doi.org/10.3390/ijerph13101004





