Tobacco Control Progress in Low and Middle Income Countries in Comparison to High Income Countries
Abstract
:1. Introduction
2. Materials and Methods
- Tax: In accordance with WHO recommendations [16], national tax values of ≥70% of retail prices were considered as 100% legislated policy. PS was calculated based on tax values scaled to this maximum value. Tax values are based on excise taxes, import duties, value-added taxes (VAT) and other taxes as applicable for the price of the most sold brand. When two non-equal tax values were presented per country and year (i.e., China and Vietnam), averages of the two values were used.
- Ban on advertising: PS were calculated as percentages of applying the following categories of bans on direct advertising: national TV and radio, international TV and radio, local magazines and newspapers, international magazines and newspapers, billboard and outdoor advertising, point of sale and internet. For example, in 2008, Bangladesh had direct advertising bans on national TV/radio, local magazines/newspapers and billboard/outdoor advertising, and was assigned a PS of 43% (3/7). In addition, 2014 data included an additional category: fines for violations of bans on direct advertising.
- Ban on promotion and sponsorship: PS were based on the following categories of bans on promotion and sponsorship: free distribution by mail or through other means, promotional discounts, non-tobacco products identified with tobacco brand names, brand name of non-tobacco products used for tobacco product, appearance of tobacco products in TV and/or films, sponsored events and product placement (not included for 2007). Furthermore, 2014 data included an eighth category: fines for violations of bans on promotion and sponsorship.
- Smoke-free environments: PS were defined as percentages of the number of the following public places with smoke-free legislation: healthcare facilities, educational facilities (excluding universities), universities, government facilities, indoor offices, restaurants, pubs and bars, public transportation (not included for 2007), and all other indoor public places.
- Availability of cessation support (Support for treatment of tobacco dependence): PS were calculated based upon the availability of tobacco dependence support methods. 2007 policy data included three methods of support: a toll-free quit line, nicotine replacement therapy (NRT), and the pharmaceutical smoking cessation aid Bupropion. In addition, 2008 and 2010 data included the pharmaceutical Varenicline, whereas 2012 and 2014 presented data solely on toll-free quit lines and NRT.
- Regulation on packaging: The WHO FCTC recommends tobacco packages to carry health warnings that cover ≥50% of the display area [1]. Packaging covered with ≥50% of health warnings were regarded as having 100% legislated policy and thus were assigned a PS of 100%.
- Existence of Government Objectives on Tobacco Control: PS was defined as a binary indicator (0% or 100%), indicating whether or not national governments have objectives on tobacco control in place.
3. Results
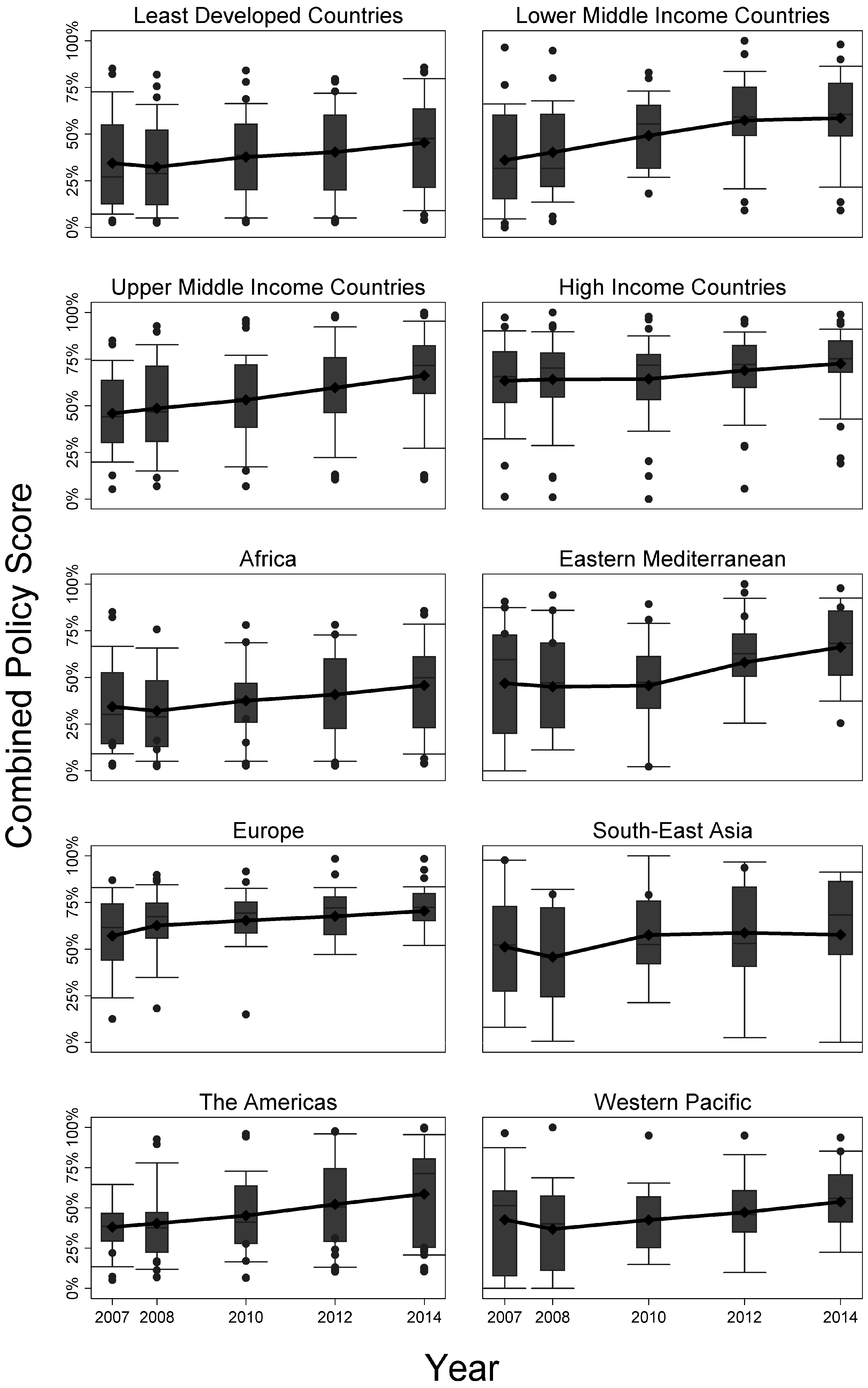
3.1. Trends of Tobacco Control Policy
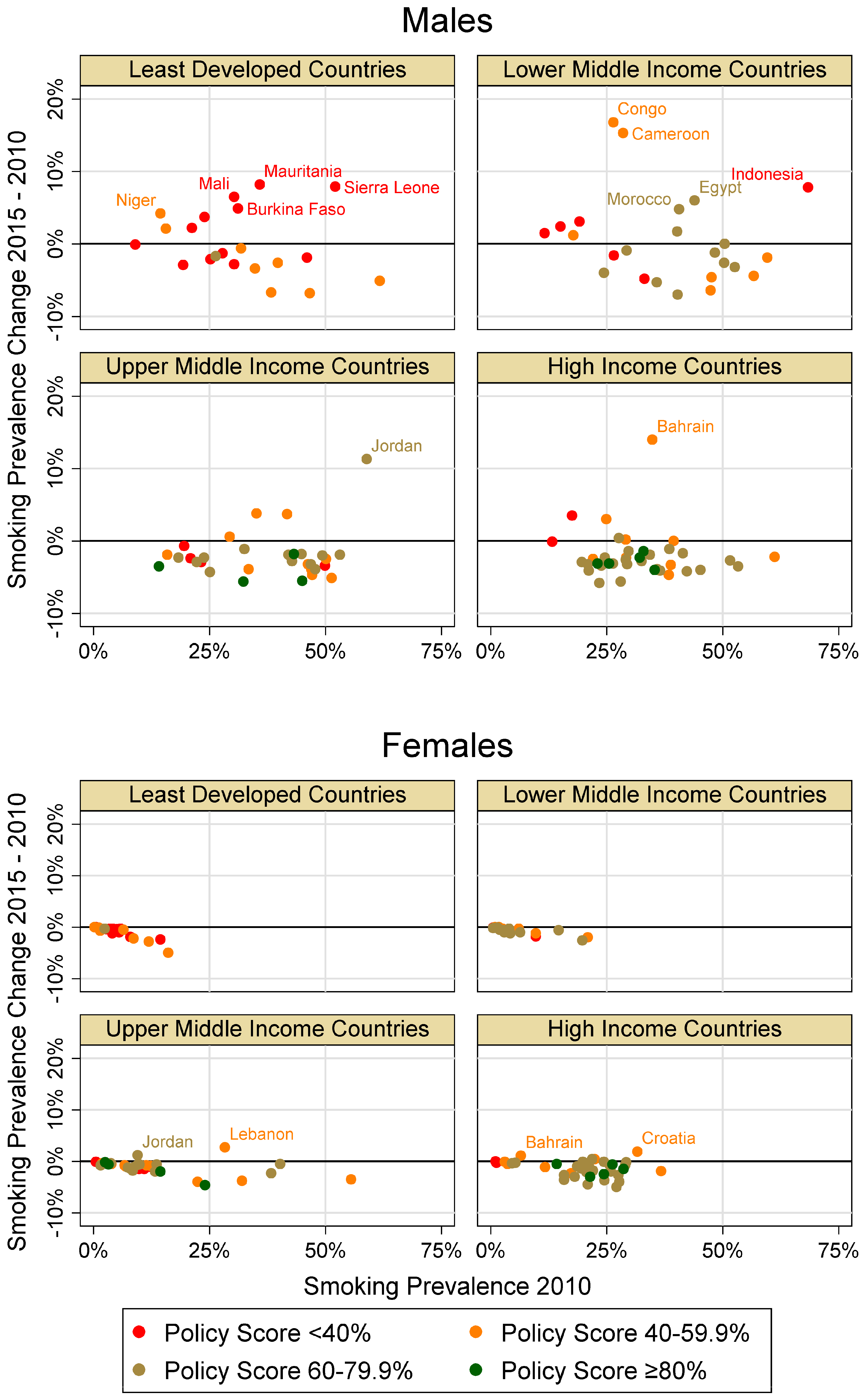
3.2. Association between Tobacco Control Policy and Change in Smoking Prevalence
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| 2007 | 2008 | 2010 | 2012 | 2014 | p-Value for Temporal Trend | |
|---|---|---|---|---|---|---|
| Region, n (# with combined PS) | 181 (142) | 194 (177) | 194 (170) | 194 (181) | 195 (185) | |
| -Africa | 46 (41) | 46 (46) | 46 (42) | 46 (44) | 47 (45) | |
| -Eastern Mediterranean | 22 (15) | 22 (21) | 22 (21) | 22 (22) | 22 (20) | |
| -Europe | 51 (39) | 53 (45) | 53 (43) | 53 (47) | 53 (51) | |
| -South-East Asia | 11 (8) | 11 (8) | 11 (8) | 11 (9) | 11 (10) | |
| -The Americas | 35 (27) | 35 (34) | 35 (33) | 35 (33) | 35 (33) | |
| -Western Pacific | 16 (12) | 27 (23) | 27 (23) | 27 (26) | 27 (26) | |
| Tax, mean% (range) | 59 (3–100) | 66 (3–100) | 68 (3–100) | 68 (4–100) | 70 (0–100) | 0.002 |
| By Region | ||||||
| -Africa | 46 (3–100) | 50 (10–100) | 51 (16–100) | 50 (12–100) | 52 (12–100) | 0.407 |
| -Eastern Mediterranean | 59 (3–97) | 54 (3–100) | 56 (3–100) | 54 (4–100) | 57 (4–100) | 0.988 |
| -Europe | 72 (11–99) | 85 (28–100) | 87 (29–100) | 88 (27–100) | 89 (25–100) | 0.001 |
| -South-East Asia | 76 (31–100) | 68 (35–100) | 70 (36–100) | 74 (43–100) | 72 (0–100) | 0.977 |
| -The Americas | 51 (3–100) | 64 (22–100) | 66 (20–100) | 67 (23–100) | 67 (23–100) | 0.036 |
| -Western Pacific | 62 (13–100) | 72 (17–100) | 72 (20–100) | 71 (21–100) | 74 (4–100) | 0.329 |
| Advertising, mean% (range) | 36 (0–100) | 39 (0–100) | 41 (0–100) | 57 (0–100) | 62 (0–100) | <0.001 |
| By Region | ||||||
| -Africa | 37 | 33 | 34 | 45 | 52 | 0.011 |
| -Eastern Mediterranean | 55 | 56 | 56 | 75 | 78 | 0.004 |
| -Europe | 41 (0–71) | 49 | 50 | 69 | 74 | <0.001 |
| -South-East Asia | 49 | 49 | 53 | 62 | 66 | 0.193 |
| -The Americas | 9 (0–86) | 16 | 22 | 37 | 43 | <0.001 |
| -Western Pacific | 45 | 41 | 44 | 60 | 66 | 0.001 |
| Promotion, mean% (range) | 35 (0–100) | 41 (0–100) | 39 (0–100) | 41 (0–100) | 45 (0–100) | 0.021 |
| By Region | ||||||
| -Africa | 29 | 30 | 29 | 30 | 36 | 0.454 |
| -Eastern Mediterranean | 58 | 61 | 66 | 66 | 66 | 0.398 |
| -Europe | 42 | 51 | 45 | 47 | 50 | 0.500 |
| -South-East Asia | 55 | 56 | 64 | 53 | 53 | 0.862 |
| -The Americas | 10 | 20 | 19 | 27 | 35 | 0.002 |
| -Western Pacific | 42 (0–83) | 43 | 36 (0–86) | 43 | 45 | 0.650 |
| Smoke free area, mean% (range ) | 36 (0–100) | 28 (0–100) | 35 (0–100) | 40 (0–100) | 43 (0–100) | <0.001 |
| By Region | ||||||
| -Africa | 36 | 21 | 25 | 27 | 30 | 0.998 |
| -Eastern Mediterranean | 47 | 44 | 38 (0–89) | 48 | 50 | 0.619 |
| -Europe | 41 | 31 | 39 | 40 | 43 | 0.276 |
| -South-East Asia | 45 | 36 | 54 (11–89) | 56 (11–89) | 58 (11–89) | 0.109 |
| -The Americas | 19 | 25 | 36 | 45 | 52 | <0.001 |
| -Western Pacific | 34 | 22 | 30 | 41 | 45 | 0.020 |
| Packaging, mean% (range) | 34 (0–100) | 38 (0–100) | 45 (0–100) | 53 (0–100) | 60 (0–100) | <0.001 |
| By Region | ||||||
| -Africa | 18 | 19 | 25 | 34 | 46 | <0.001 |
| -Eastern Mediterranean | 36 | 31 | 32 | 59 | 64 | 0.002 |
| -Europe | 44 (0–80) | 57 | 67 | 65 | 67 | 0.000 |
| -South-East Asia | 34 | 24 | 26 | 49 | 53 | 0.084 |
| -The Americas | 32 | 37 | 42 | 52 | 58 | 0.006 |
| -Western Pacific | 46 | 47 | 57 | 59 | 68 | 0.023 |
| Cessation, mean% (range) | 51 (0–100) | 48 (0–100) | 54 (0–100) | 53 (0–100) | 52 (0–100) | 0.445 |
| By Region | ||||||
| -Africa | 30 | 24 | 33 | 28 | 29 | 0.785 |
| -Eastern Mediterranean | 33 (0–67) | 47 (0–75) | 43 | 55 | 50 | 0.045 |
| -Europe | 76 | 73 | 75 | 76 | 71 | 0.641 |
| -South-East Asia | 27 (0–67) | 23 (0–75) | 30 (0–75) | 27 | 32 | 0.636 |
| -The Americas | 62 | 59 | 66 | 59 | 63 | 0.928 |
| -Western Pacific | 53 | 40 | 50 | 48 | 46 | 0.921 |
| Governmental Objectives on Tobacco Control, mean% (range) | 57 (0–100) | 69 (0–100) | 73 (0–100) | 77 (0–100) | 89 (0–100) | <0.001 |
| By Region | ||||||
| -Africa | 37 | 48 | 57 | 63 | 76 | <0.001 |
| -Eastern Mediterranean | 73 | 77 | 82 | 82 | 91 | 0.127 |
| -Europe | 59 | 77 | 82 | 83 | 94 | <0.001 |
| -South-East Asia | 73 | 82 | 82 | 91 | 100 | 0.062 |
| -The Americas | 54 | 57 | 60 | 66 | 83 | 0.009 |
| -Western Pacific | 80 | 93 | 93 | 93 | 100 | 0.057 |
| Policy score, mean% (range) | 47 (3–91) | 48 (2–94) | 52 (3–96) | 56 (3–98) | 61 (4–100) | <0.001 |
| By Region | ||||||
| -Africa | 34 (3–85) | 32 (2–84) | 38 (3–78) | 41 (3–88) | 46 (4–88) | 0.003 |
| -Eastern Mediterranean | 55 (15–85) | 54 (5–87) | 54 (5–84) | 63 (12–92) | 68 (32–90) | 0.009 |
| -Europe | 57 (13–87) | 63 (18–90) | 65 (15–92) | 68 (19–98) | 71 (21–98) | <0.001 |
| -South-East Asia | 57 (27–89) | 53 (21–78) | 61 (36–91) | 62 (23–88) | 61 (19–88) | 0.402 |
| -The Americas | 38 (5–71) | 40 (7–93) | 45 (6–96) | 52 (10–98) | 59 (11–100) | <0.001 |
| -Western Pacific | 56 (21–91) | 53 (18–94) | 56 (31–90) | 59 (25–90) | 64 (36–89) | 0.026 |
References
- World Health Organization. WHO Framework Convention on Tobacco Control; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- World Health Organization. WHO Global Report: Mortality Attributable to Tobacco; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. Tobacco: Fact Sheet No. 339. 2015. Available online: http://www.who.int/mediacentre/factsheets/fs339/en/ (accessed on 3 September 2015).
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. 2009. Available online: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf (accessed on 1 December 2015).
- Brathwaite, R.; Addo, J.; Smeeth, L.; Lock, K. A systematic review of tobacco smoking prevalence and description of tobacco control strategies in Sub-Saharan African Countries; 2007 to 2014. PLoS ONE 2015, 10, e0132401. [Google Scholar] [CrossRef] [PubMed]
- Mendez, D.; Alshanqeety, O.; Warner, K.E. The potential impact of smoking control policies on future global smoking trends. Tob. Control 2013, 22, 46–51. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2008—The MPOWER Package. 2008. Available online: http://www.who.int/tobacco/mpower/2008/en/ (accessed on 21 July 2015).
- Leischow, S.J.; Ayo-Yusuf, O.; Backinger, C.L. Converging research needs across framework convention on tobacco control articles: Making research relevant to global tobacco control practice and policy. Nicotine Tob. Res. 2013, 15, 761–766. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Parties to the WHO Framework Convention on Tobacco Control. 2015. Available online: http://www.who.int/fctc/signatories_parties/en/ (accessed on 29 July 2015).
- Gilmore, A.B.; Fooks, G.; Drope, J.; Bialous, S.A.; Jackson, R.R. Exposing and addressing tobacco industry conduct in low-income and middle-income countries. Lancet 2015, 385, 1029–1043. [Google Scholar] [CrossRef]
- Levy, D.T.; Ellis, J.A.; Mays, D.; Huang, A.-T. Smoking-related deaths averted due to three years of policy progress. Bull. World Health Organ. 2013, 91, 509–518. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2009—Implementing Smoke-Free Environments. 2009. Available online: http://www.who.int/tobacco/mpower/2009/en/ (accessed on 21 July 2015).
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2011—Warning about the Dangers of Tobacco. 2011. Available online: http://www.who.int/tobacco/global_report/2011/en/ (accessed on 21 July 2015).
- World Health Organization. WHO Report on the Global Tobacco Epidemic 2013—Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. 2013. Available online: http://www.who.int/tobacco/global_report/2013/en/ (accessed on 21 July 2015).
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2015—Raising Taxes on Tobacco. 2015. Available online: http://www.who.int/tobacco/global_report/2015/en/ (accessed on 21 July 2015).
- World Health Organization. WHO Technical Manual on Tobacco Tax Administration. 2010. Available online: http://www.who.int/tobacco/publications/tax_administration/en/ (accessed on 20 October 2015).
- Dubray, J.; Schwartz, R.; Chaiton, M.; O’Connor, S. The effect of MPOWER on smoking prevalence. Tob. Control 2014. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Co-Operation and Development. DAC List of ODA Recipients. 2015. Available online: http://www.oecd.org/dac/stats/documentupload/DAC%20List%20of%20ODA%20Recipients%202014%20final.pdf (accessed on 20 June 2015).
- World Health Organization. WHO Regions. Available online: http://www.who.int/about/regions/en/ (accessed on 21 July 2015).
- World Health Organization. Global Health Observatory Data Repository. Available online: http://apps.who.int/gho/data/node.main.65?lang=en (accessed on 8 August 2015).
- Bilano, V.; Gilmour, S.; Moffiet, T.; d’Espaignet, E.T.; Stevens, G.A.; Commar, A.; Tuyl, F.; Hudson, I.; Shibuya, K. Global trends and projections for tobacco use, 1990–2025: An analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. Lancet 2015, 385, 966–976. [Google Scholar] [CrossRef]
- The Lancet. What Will It Take to Create a Tobacco-Free World? Elsevier: Amsterdam, The Netherlands, 2015; p. 915. [Google Scholar]
- Bump, J.B.; Reich, M.R. Political economy analysis for tobacco control in low- and middle-income countries. Health Policy Plan. 2013, 28, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Nagler, R.H.; Viswanath, K. Implementation and research priorities for FCTC Articles 13 and 16: Tobacco advertising, promotion, and sponsorship and sales to and by minors. Nicotine Tob. Res. 2013, 15, 832–846. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Gender, Women, and the Tobacco Epidemic. 2010. Available online: http://www.who.int/tobacco/publications/gender/en_tfi_gender_women_marketing_tobacco_women.pdf (accessed on 3 September 2015).
- Heydari, G.; Talischi, F.; Masjedi, M.R.; Alguomani, H.; Joossens, L.; Ghafari, M. Comparison of tobacco control policies in the Eastern Mediterranean countries based on Tobacco Control Scale scores. East. Mediterr. Health J. 2012, 18, 803–810. [Google Scholar] [PubMed]
- Heydari, G.; Ebn Ahmady, A.; Lando, H.A.; Shadmehr, M.B.; Fadaizadeh, L. The second study on WHO MPOWER tobacco control scores in Eastern Mediterranean Countries based on the 2013 report: Improvements over two years. Arch. Iran. Med. 2014, 17, 621–625. [Google Scholar] [PubMed]
- Blecher, E. The impact of tobacco advertising bans on consumption in developing countries. J. Health Econ. 2008, 27, 930–942. [Google Scholar] [CrossRef] [PubMed]
- Savell, E.; Gilmore, A.; Sims, M.; Mony, P.K.; Koon, T.; Yusoff, K.; Lear, S.A.; Seron, P.; Ismail, N.; Calik, K.B.T.; et al. The environmental profile of a community’s health: A cross-sectional study on tobacco marketing in 16 countries. Bull. World Health Organ. 2015, 93, 851G–861G. [Google Scholar] [CrossRef] [PubMed]
- Blecher, E.H.; van Walbeek, C.P. An international analysis of cigarette affordability. Tob. Control 2004, 13, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Chaloupka, F.J.; Straif, K.; Leon, M.E.; Working Group; International Agency for Research on Cancer. Effectiveness of tax and price policies in tobacco control. Tob. Control 2011, 20, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Hitchman, S.C.; Fong, G.T. Gender empowerment and female-to-male smoking prevalence ratios. Bull. World Health Organ. 2011, 89, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Pampel, F.C. Global patterns and determinants of sex differences in smoking. Int. J. Comp. Sociol. 2006, 47, 466–487. [Google Scholar] [CrossRef] [PubMed]
| 2007 | 2008 | 2010 | 2012 | 2014 | p-Value for Temporal Trend | |
|---|---|---|---|---|---|---|
| Income Category, n (# with combined PS) | 181 (142) | 194 (177) | 194 (170) | 194 (181) | 195 (185) | |
| -Least Developed Countries | 47 (36) | 51 (42) | 51 (41) | 51 (47) | 52 (47) | |
| -Lower Middle Income Countries | 32 (28) | 34 (33) | 34 (32) | 34 (33) | 34 (33) | |
| -Upper Middle Income Countries | 53 (38) | 57 (56) | 57 (51) | 57 (54) | 57 (55) | |
| -High Income Countries | 49 (40) | 52 (46) | 52 (46) | 52 (47) | 52 (50) | |
| Tax, mean% (range) | 59 (3–100) | 66 (3–100) | 68 (3–100) | 68 (4–100) | 70 (0–100) | 0.002 |
| By Income Category | ||||||
| -Least Developed Countries | 47 (3–100) | 49 (10–100) | 49 (5–100) | 48 (4–100) | 49 (0–100) | 0.875 |
| -Lower Middle Income Countries | 49 (11–90) | 57 (22–100) | 60 (22–100) | 61 (23–100) | 65 (23–100) | 0.011 |
| -Upper Middle Income Countries | 59 (3–100) | 69 (3–100) | 72 (3–100) | 74 (4–100) | 76 (7–100) | 0.003 |
| -High Income Countries | 76 (14–99) | 85 (26–100) | 85 (20–100) | 84 (29–100) | 85 (28–100) | 0.164 |
| Advertising, mean% (range) | 36 (0–100) | 39 (0–100) | 41 (0–100) | 57 (0–100) | 62 (0–100) | 0.000 |
| By Income Category | ||||||
| -Least Developed Countries | 33 | 34 | 36 | 48 | 52 | 0.002 |
| -Lower Middle Income Countries | 32 | 35 | 41 | 55 | 60 | <0.001 |
| -Upper Middle Income Countries | 37 | 40 | 41 | 61 | 69 | <0.001 |
| -High Income Countries | 41 (0–71) | 45 (0–86) | 47 | 62 | 66 | <0.001 |
| Promotion, mean% (range) | 35 (0–100) | 41 (0–100) | 39 (0–100) | 41 (0–100) | 45 (0–100) | 0.021 |
| By Income Category | ||||||
| -Least Developed Countries | 32 | 35 | 33 | 33 | 38 | 0.632 |
| -Lower Middle Income Countries | 27 | 31 | 38 | 40 | 44 | 0.028 |
| -Upper Middle Income Countries | 31 | 43 | 38 | 48 | 52 | 0.006 |
| -High Income Countries | 48 | 50 | 45 | 43 | 45 | 0.400 |
| Smoke free area, mean% (range ) | 36 (0–100) | 28 (0–100) | 35 (0–100) | 40 (0–100) | 43 (0–100) | <0.001 |
| By Income Category | ||||||
| -Least Developed Countries | 36 | 23 | 25 | 25 | 31 | 0.830 |
| -Lower Middle Income Countries | 30 (0–88) | 30 | 41 | 50 | 50 | <0.001 |
| -Upper Middle Income Countries | 30 | 30 | 40 | 49 | 55 | <0.001 |
| -High Income Countries | 45 | 29 | 34 | 37 | 39 | 0.986 |
| Packaging, mean% (range) | 34 (0–100) | 38 (0–100) | 45 (0–100) | 53 (0–100) | 59 (0–100) | <0.001 |
| By Income Category | ||||||
| -Least Developed Countries | 21 | 19 | 27 | 33 | 42 | <0.001 |
| -Lower Middle Income Countries | 33 | 37 | 42 | 54 | 60 | 0.001 |
| -Upper Middle Income Countries | 32 | 42 | 49 | 56 | 64 | <0.001 |
| -High Income Countries | 48 | 54 | 59 | 69 | 70 | <0.001 |
| Cessation, mean% (range) | 51 (0–100) | 48 (0–100) | 54 (0–100) | 53 (0–100) | 52 (0–100) | 0.445 |
| By Income Category | ||||||
| -Least Developed Countries | 20 | 16 | 23 | 23 | 23 | 0.291 |
| -Lower Middle Income Countries | 48 | 46 | 54 | 51 | 46 | 0.944 |
| -Upper Middle Income Countries | 53 | 49 | 55 | 53 | 57 | 0.332 |
| -High Income Countries | 81 | 82 | 82 | 83 | 78 | 0.585 |
| Governmental Objectives on Tobacco Control, mean% (range) | 57 (0–100) | 69 (0–100) | 73 (0–100) | 77 (0–100) | 89 (0–100) | <0.001 |
| By Income Category | ||||||
| -Least Developed Countries | 38 | 53 | 59 | 67 | 78 | <0.001 |
| -Lower Middle Income Countries | 68 | 76 | 85 | 88 | 91 | 0.007 |
| -Upper Middle Income Countries | 53 | 70 | 75 | 73 | 88 | <0.001 |
| -High Income Countries | 72 | 79 | 79 | 83 | 98 | 0.001 |
| Combined policy score, mean% (range) | 47 (3–91) | 48 (2–94) | 52 (3–96) | 56 (3–98) | 61 (4–100) | <0.001 |
| By Income Category | ||||||
| -Least Developed Countries | 34 (3–85) | 32 (2–82) | 38 (3–84) | 40 (3–80) | 45 (4–86) | 0.006 |
| -Lower Middle Income Countries | 42 (14–89) | 45 (16–87) | 52 (28–78) | 58 (21–92) | 59 (21–90) | <0.001 |
| -Upper Middle Income Countries | 46 (5–85) | 49 (7–93) | 53 (7–96) | 60 (10–98) | 66 (11–100) | <0.001 |
| -High Income Countries | 62 (7–91) | 62 (7–94) | 63 (6–92) | 67 (11–90) | 70 (23–93) | 0.012 |
| Model 1 | Model 2 (with Interaction Term) | |||||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | |||||
| β | p-Value | β | p-Value | β | p-Value | β | p-Value | |
| PS 2010 | −0.037 | 0.013 | −0.007 | 0.077 | −0.027 | 0.111 | −0.006 | 0.181 |
| Income category | 0.072 | 0.424 | 0.027 | 0.970 | ||||
| LDCs | 1.468 | −0.441 | 6.136 | −0.208 | ||||
| LMICs | 2.561 | −0.002 | 4.443 | −0.254 | ||||
| UMICs | 0.295 | −0.011 | −0.470 | 0.114 | ||||
| HICs | ref | ref | ref | ref | ||||
| Income category × PS 2010 | - | - | 0.004 | 0.132 | ||||
| LDCs | −0.123 | −0.007 | ||||||
| LMICs | −0.035 | 0.004 | ||||||
| UMICs | 0.010 | −0.002 | ||||||
| HICs | ref | ref | ||||||
| Smoking Prev 2010 | 0.001 | 0.013 | −0.053 | <0.001 | −0.130 | 0.663 | −0.055 | <0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, C.L.; Becher, H.; Winkler, V. Tobacco Control Progress in Low and Middle Income Countries in Comparison to High Income Countries. Int. J. Environ. Res. Public Health 2016, 13, 1039. https://doi.org/10.3390/ijerph13101039
Anderson CL, Becher H, Winkler V. Tobacco Control Progress in Low and Middle Income Countries in Comparison to High Income Countries. International Journal of Environmental Research and Public Health. 2016; 13(10):1039. https://doi.org/10.3390/ijerph13101039
Chicago/Turabian StyleAnderson, Carrie L., Heiko Becher, and Volker Winkler. 2016. "Tobacco Control Progress in Low and Middle Income Countries in Comparison to High Income Countries" International Journal of Environmental Research and Public Health 13, no. 10: 1039. https://doi.org/10.3390/ijerph13101039
APA StyleAnderson, C. L., Becher, H., & Winkler, V. (2016). Tobacco Control Progress in Low and Middle Income Countries in Comparison to High Income Countries. International Journal of Environmental Research and Public Health, 13(10), 1039. https://doi.org/10.3390/ijerph13101039






