Important Variables When Screening for Students at Suicidal Risk: Findings from the French Cohort of the SEYLE Study
Abstract
:1. Introduction
2. Material and Method
2.1. The SEYLE Study
- (1)
- “Question Persuade and Refer” (QPR) gatekeeper program [11], a training of the adults working in the school;
- (2)
- a mental health awareness program designed for students called the “Youth Aware of Mental Health” (YAM) program [12];
- (3)
- a two-stage health professional screening of at risk students “ProfScreen” [13]; and
- (4)
- a minimal information program considered as the control group “Information”.
2.2. Self-Report Questionnaire Screening
2.2.1. The SEYLE Questionnaire
2.2.2. ProfScreen: At Risk Students
| Scales | Cut Offs |
|---|---|
| Depression (BDI) | ≥superior or equal to 14 (Mild depression) |
| Anxiety (SAS) | ≥superior or equal to 45 (Mild anxiety) |
| Suicidal ideations/behaviors (PSS) + question about previous suicide attempt | any suicidal thought or attempts in the last two weeks a life-time history of suicide attempt |
| Non-suicidal self-injury (Shortened version of DSHI) | a life-time history of two or more incidents of intentional self-injury |
| Eating behavior (BMI) | BMI < 16,5 |
| Sensation seeking and delinquent behaviors | three or more positive answers out of six |
| Tobacco * | ≥2 cigarettes per day (France: ≥7) |
| Alcohol | student has/had: an alcoholic drink at least twice a week and/or drinks at least three alcohol units per occurrence and/or got drunk at least three times (lifetime) and/or at least three hangovers (lifetime) |
| Illegal drugs | illegal drug used three times or more during lifetime |
| Excessive use of media | Over five hours per day in front of a screen |
| Loneliness/Social relationships problems | Student feels lonely most of the time in the past 12 months |
| Bullying | ≥5 incidents (chosen out of 15) in the past 12 months |
| Truancy | Student missed class 3 times or more in the past two weeks (in France: ≥ 2 because the school year started a week before the program started and we considered necessary to modify this cut off in order to avoid a bias) |
2.3. Emergency Cases
2.4. Interviews and Referrals
2.5. Statistical Procedures
3. Results
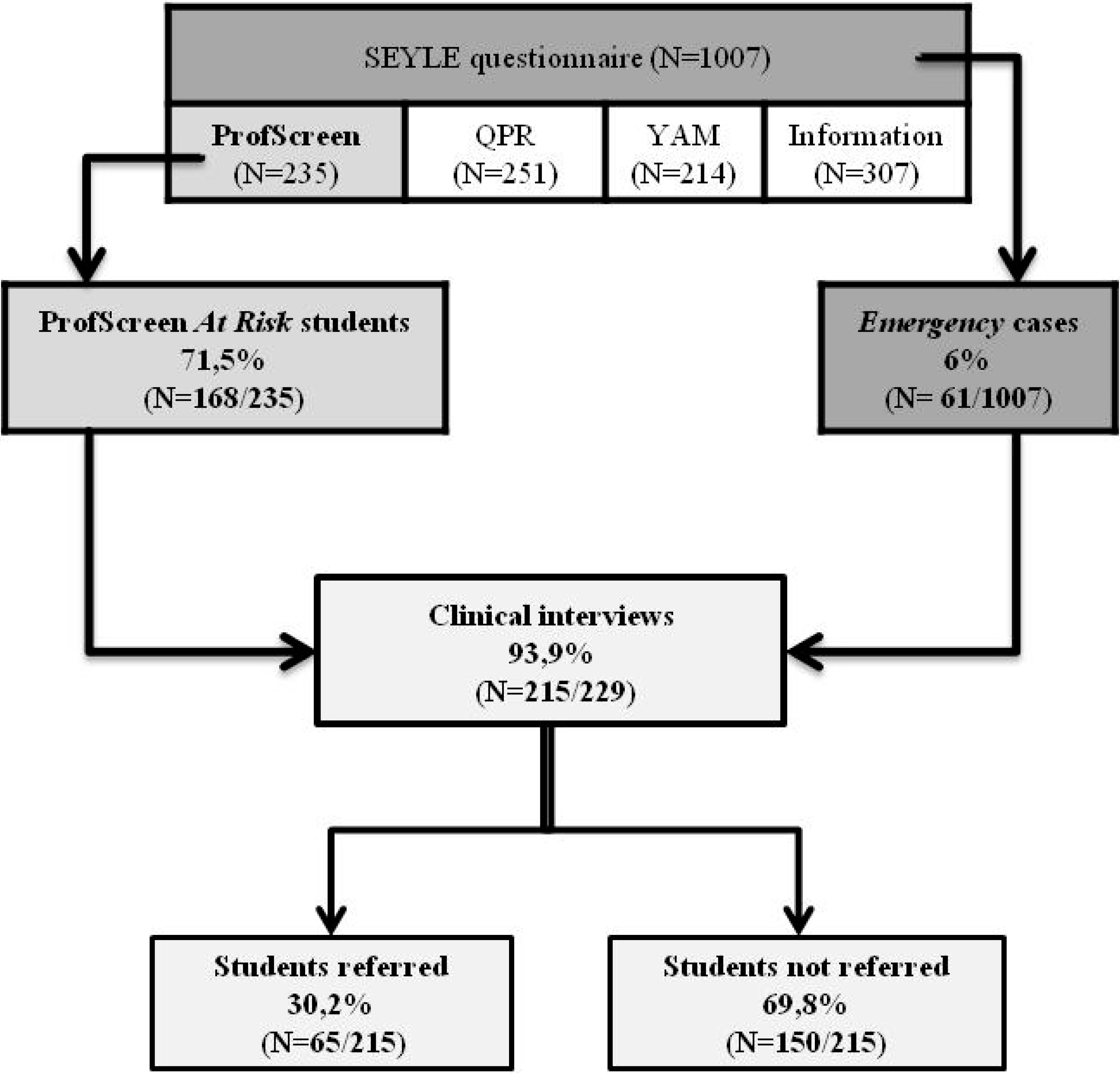
3.1. Referrals
| Total Sample | ProfScreen | Emergency Cases | ||
|---|---|---|---|---|
| N = 235 | N = 1007 | |||
| N | % | N * | % | |
| Students screened positive | 168 | 71,5 | 61 | 6 |
| Students referred for treatment | 38 | 16,2 | 27 | 2,7 |
3.2. Psychopathology
| Scales | At risk Students (N = 168) | Referred Students (N = 38) | p Value * | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Alcohol | 84 | 50,0 | 20 | 52,6 | NS |
| Depression | 61 | 36,3 | 28 | 73,7 | <0.001 |
| NSSI | 59 | 35,1 | 19 | 50,0 | 0.0525 |
| Bullying | 44 | 26,2 | 13 | 34,2 | NS |
| Suicidal behaviours | 36 | 21,4 | 17 | 44,7 | <0.001 |
| Truancy | 27 | 16,1 | 6 | 15,8 | NS |
| Anxiety | 26 | 15,5 | 13 | 34,2 | <0.001 |
| Illegal drugs | 21 | 12,5 | 6 | 15,8 | NS |
| Tobacco | 19 | 11,3 | 4 | 10,5 | NS |
| Social relationships | 16 | 9,5 | 9 | 23,7 | <0.01 |
| Eating habits | 12 | 7,1 | 1 | 2,6 | NS |
| Media exposure | 11 | 6,5 | 4 | 10,5 | NS |
| Sensation seeking | 1 | 0,6 | 0 | 0,0 | NS |
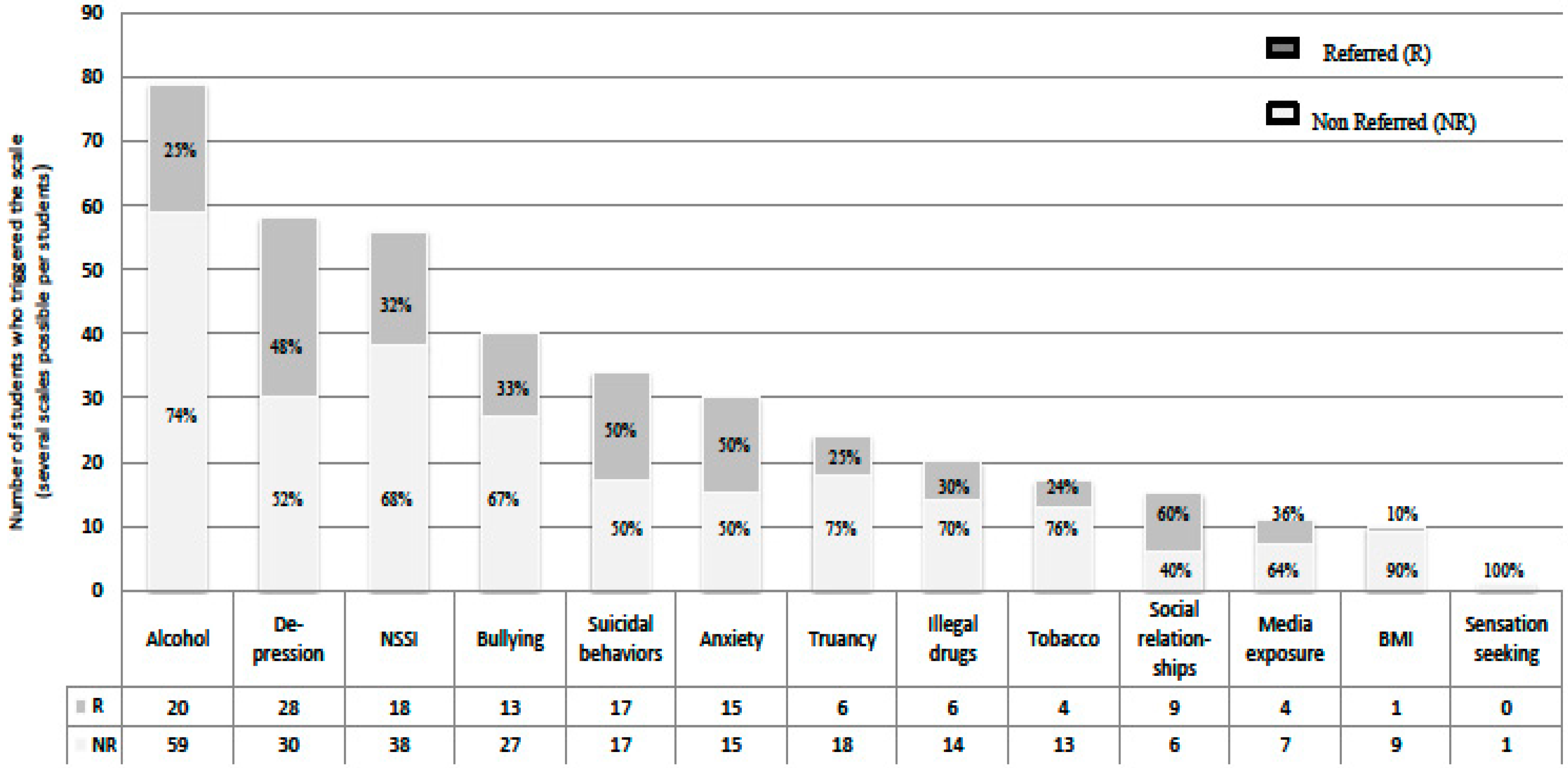
3.3. Scales and Referrals
| Scales | OR in Bivariate Regression [CI: 95%] | OR in Multivariate Regression [CI: 95%] |
|---|---|---|
| Beck Depression Inventory BDI-II | 1.15 ** [1.09–1.22] | 1.13 ** [1.07–1.20] |
| Zung Self-Assessment Anxiety Scale SAS | 1.11 ** [1.06–1.17] | NS |
| Non Suicidal Self Injury NSSI | 3.10 ** [1.38–6.95] | 2.85 * [1.03–7.90] |
| Alcohol consumption | 2.89 ** [1.35–6.22] | 2.80 * [1.05–7.43] |
3.4. Reasons for Referrals
| ProfScreen + Emergencies (baseline) | n = 63 ** | |
|---|---|---|
| n | % | |
| Depressive symptom | 32 | 50,8 |
| Suicidal behaviours | 25 | 39,7 |
| Anxiety | 24 | 38,1 |
| Negative life events | 22 | 34,9 |
| Non-Suicidal Self-Injury | 12 | 19,0 |
| Irritability | 10 | 15,9 |
| Family conflicts | 10 | 15,9 |
| Eating disorder | 6 | 9,5 |
| Alcohol | 6 | 9,5 |
| Low self esteem | 5 | 7,9 |
| Impulsivity | 4 | 6,3 |
| Tobacco | 4 | 6,3 |
| Sleep Disorder | 4 | 6,3 |
| Drugs | 3 | 4,8 |
| Risk behaviours | 3 | 4,8 |
| Social relationships (isolation) | 3 | 4,8 |
| Behaviour disorder | 2 | 3,2 |
| Bullying | 2 | 3,2 |
| Domestic violence | 2 | 3,2 |
| Sexual harrassement | 2 | 3,2 |
| Parentification | 1 | 1,6 |
| Phobia | 1 | 1,6 |
4. Discussion
4.1. False Positive Cases are Functionally Impaired
4.2. Risk Behavior and Psychopathology
4.3. Reasons to Refer
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Preventing suicide: A global imperative. Available online: http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/ (accessed 16 December 2014).
- Wasserman, D.; cheng, Q.; Jiang, G.-X. Global suicide rates among young people aged 15–19. World Psychiat. 2005, 4, 114–120. [Google Scholar]
- Suicide a leading cause of death among young adults in high-income countries. Available online: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/mental-health/news/news/2014/09/suicide-a-leading-cause-of-death-among-young-adults-in-high-income-countries (accessed 16 January 2015).
- Lonnqvist, J. Major psychiatric disorders in suicide and suicide attempters. In Oxford Textbook of Suicidology and Suicide Prevention; Wasserman, D., Wasserman, C., Eds.; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Bertolote, J.M.; Fleischmann, A.; De Leo, D.; Wasserman, D. Suicide and mental disorders: Do we know enough? Br. J. Psychiatry J. Ment. Sci. 2003, 183, 382–383. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of dsm-iv disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Paus, T.; Keshavan, M.; Giedd, J.N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Morabia, A.; Zhang, F. History of medical screening: From concepts to action. Postgrad. Med. J. 2004, 80, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Raffle, A.E.; Gray, J.A.M. Screening; Oxford University Press: Oxford, UK, 2007. [Google Scholar]
- Wasserman, D.; Carli, V.; Wasserman, C.; Apter, A.; Balazs, J.; Bobes, J.; Bracale, R.; Brunner, R.; Bursztein-Lipsicas, C.; Corcoran, P.; et al. Saving and empowering young lives in Europe (SEYLE): A randomized controlled trial. BMC Public Health 2010. [Google Scholar] [CrossRef] [PubMed]
- QPR Institute. Available online: http://www.qprinstitute.com/ (accessed 5 January 2014).
- Youth Aware of Mental Health. Available online: http://www.y-a-m.org/ (accessed 13 January 2015).
- Kaess, M.; Brunner, R.; Parzer, P.; Carli, V.; Apter, A.; Balazs, J.A.; Bobes, J.; Coman, H.G.; Cosman, D.; Cotter, P.; et al. Risk-behaviour screening for identifying adolescents with mental health problems in Europe. Eur. Child Adolesc. Psychiatry 2014, 23, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Carli, V.; Wasserman, C.; Wasserman, D.; Sarchiapone, M.; Apter, A.; Balazs, J.; Bobes, J.; Brunner, R.; Corcoran, P.; Cosman, D.; et al. The saving and empowering young lives in Europe (SEYLE) randomized controlled trial (RCT): Methodological issues and participant characteristics. BMC Public Health 2013. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.N.; Eckert, T.L.; DuPaul, G.J.; White, G.P. Adolescent suicide prevention: acceptability of school-based programs among secondary school principals. Suicide Life. Threat. Behav. 1999, 29, 72–85. [Google Scholar] [PubMed]
- Eckert, T.L.; Miller, D.N.; DuPaul, G.J.; Riley-Tillman, T.C. Adolescent suicide prevention: School psychologists’ acceptability of school-based programs. Sch. Psychol. Rev. 2003, 32, 57–76. [Google Scholar]
- Husky, M.M.; Kaplan, A.; McGuire, L.; Flynn, L.; Chrostowski, C.; Olfson, M. Identifying adolescents at risk through voluntary school-based mental health screening. J. Adolesc. 2011, 34, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.S.; Greenberg, T.; Velting, D.M.; Shaffer, D. Youth suicide risk and preventive interventions: A review of the past 10 years. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 386–405. [Google Scholar] [CrossRef] [PubMed]
- Leon, A.C.; Portera, L.; Olfson, M.; Weissman, M.M.; Kathol, R.G.; Farber, L.; Sheehan, D.V.; Pleil, A.M. False positive results: A challenge for psychiatric screening in primary care. Am. J. Psychiatry 1997, 154, 1462–1464. [Google Scholar] [PubMed]
- Laukkanen, E.; Hintikka, J.J.; Kylmä, J.; Kekkonen, V.; Marttunen, M. A brief intervention is sufficient for many adolescents seeking help from low threshold adolescent psychiatric services. BMC Health Serv. Res. 2010. [Google Scholar] [CrossRef] [PubMed]
- Lewinsohn, P.; Rohde, P.; Seeley, J. Adolescent suicidal ideation and attempts: Prevalence, risk factors, and clinical implications. Clin. Psychol. Sci. Pract. 1996, 3, 25–46. [Google Scholar] [CrossRef]
- Carli, V.; Hoven, C.W.; Wasserman, C.; Chiesa, F.; Guffanti, G.; Sarchiapone, M.; Apter, A.; Balazs, J.; Brunner, R.; Corcoran, P.; et al. A newly identified group of adolescents at “invisible” risk for psychopathology and suicidal behavior: Findings from the SEYLE study. World Psychiat. 2014, 13, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Oquendo, M.A.; Perez-Rodriguez, M.M.; Poh, E.; Sullivan, G.; Burke, A.K.; Sublette, M.E.; Mann, J.J.; Galfalvy, H. Life events: A complex role in the timing of suicidal behavior among depressed patients. Mol. Psychiatry 2014, 19, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Mathew, A.; Nanoo, S. Psychosocial stressors and patterns of coping in adolescent suicide attempters. Indian J. Psychol. Med. 2013, 35, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.-P.; Tubiana, A.; Cohen, R. Screening Adolescents : Helping to Unblock Psychiatric Services; 23rd Congress of the European Psychiatric Association: Vienna, Austria, 2015. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kahn, J.-P.; Tubiana, A.; Cohen, R.F.; Carli, V.; Wasserman, C.; Hoven, C.; Sarchiapone, M.; Wasserman, D. Important Variables When Screening for Students at Suicidal Risk: Findings from the French Cohort of the SEYLE Study. Int. J. Environ. Res. Public Health 2015, 12, 12277-12290. https://doi.org/10.3390/ijerph121012277
Kahn J-P, Tubiana A, Cohen RF, Carli V, Wasserman C, Hoven C, Sarchiapone M, Wasserman D. Important Variables When Screening for Students at Suicidal Risk: Findings from the French Cohort of the SEYLE Study. International Journal of Environmental Research and Public Health. 2015; 12(10):12277-12290. https://doi.org/10.3390/ijerph121012277
Chicago/Turabian StyleKahn, Jean-Pierre, Alexandra Tubiana, Renaud F. Cohen, Vladimir Carli, Camilla Wasserman, Christina Hoven, Marco Sarchiapone, and Danuta Wasserman. 2015. "Important Variables When Screening for Students at Suicidal Risk: Findings from the French Cohort of the SEYLE Study" International Journal of Environmental Research and Public Health 12, no. 10: 12277-12290. https://doi.org/10.3390/ijerph121012277





