Participatory Research to Design a Novel Telehealth System to Support the Night-Time Needs of People with Dementia: NOCTURNAL
Abstract
:1. Introduction
2. Methodology
- Gathering user requirements using a user centred design approach.
- System development and integration.
- Data analysis and decision support.
- Trial evaluation, analysis and validation.
- A referral was sent from HSC to FOLD, a project partner.
- An email was sent to the Lead on user engagement (SM) and copied to the PI.
- SM would then contact all those on the referral to set up an initial face to face visit. This initial visit would last no more than 30 min, during which time project would be discussed in detail with potential participants and carers or invited significant other of their choice. The concept of NOCTURNAL and requirement from each participant will be clearly explained and SM would regularly check the understanding of those in attendance during the meeting. A participant information sheet for each person attending was provided. The issue of consent to participate and also how to withdraw from the project outlined. The consent to participate form was ‘walked’ through, and left with those present to reflect upon. A date for a follow-up visit was agreed for one week’s time to discuss the project and seek consent to participate.
- The second meeting one week later would also last no more than 30 min and was led by SM. She recapped on the project and sought views on consent to participate. If consent was forthcoming SM would begin the process of starting to gather user information. Based on semi-structure interviews with a phenomenological approach SM would probe on the participants lived experience for example:
- Describe a good night at home
- Tell me what helps you feel safe at home during the hours of darkness?
- How do you feel at night?
- Do you feel satisfied with your night-time routine?
- What do you understand by technology?
- When you think about technology how does it make you feel?
- What challenges do you think that using technology would present to you?
- Can you see any benefits of using technology?
- Promoting independence
- Maintaining dignity
- Maximising social inclusion
- Managing risk
- Providing stimulation
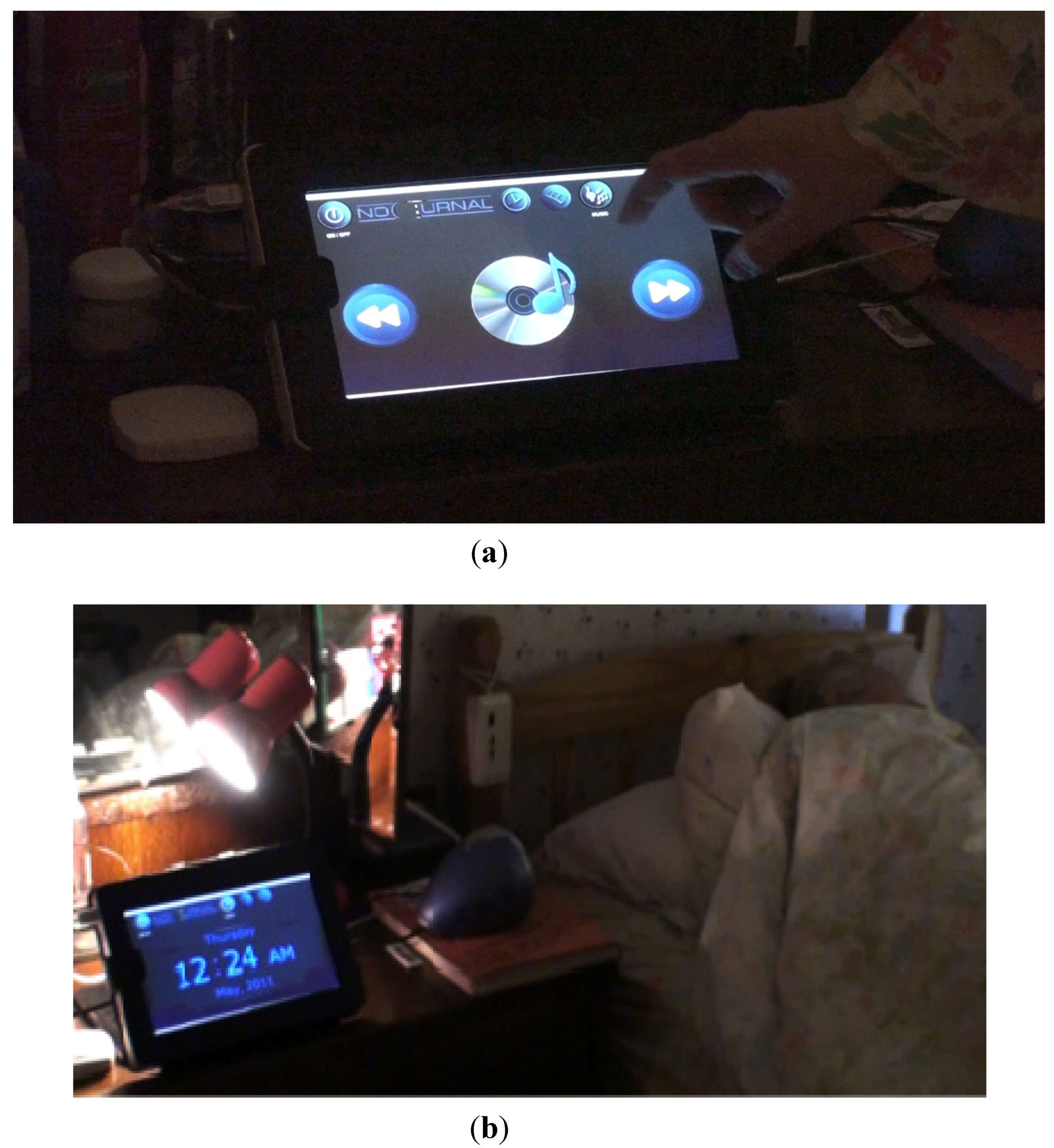
- Phase one: this was validation and evaluation of first stage prototype of NOCTURNAL. At this stage the key aim was to test the stability of the system as we moved from the lab to the home and integrated from home to FOLD. During this stage prototype one was be set up in participants home to test stability, usability and integration with FOLD.
- Phase two: Evaluation of second stage prototype of NOCTURNAL. The key functionality to be tested was the implementation of music and the possibly light linked to respond to sensor data.
- Phase three: Evaluation of stable NOCTURNAL system and full integration into the FOLD Telecare system.
- Has this NOCTURNAL technology the potential to be developed into the smart home platform to offer therapeutic intervention to people living at home with dementia?
- Can people with dementia and their carers be directly involved in researc
3. Ethical Governance
4. Findings
4.1. User Specific Findings
4.1.1. Participant Recruitment
- ○
- This was a time intensive phase of the project.
- ○
- Recruitment was very slow and regular contact with HSC staff was essential to remind them about our work.
- ○
- A high number of participants were referred to the project team who were not suitable candidates.
4.1.2. User Acceptance of Technology Installation
- Promoting independence
- Maintaining dignity
- Maximising social inclusion
- Managing risk
- Providing stimulation
4.1.3. Carers Concerns
4.1.4. A Short Case Scenario
4.2. Technical Platform
- Home networks, providing either wired and wireless connectivity with specialist protocols such as X10 used to supplement standard 802.x and z-wave networks;

4.2.1. Examples of Service Application
4.2.2. Visualisation of Ambient Assisted Living Service Data
- (1)
- Bed occupancy:
- If (the bed sensor is “in” AND NOT (“out” in less than 1 min)) AND (no other PIR activated), then the bed entry is valid;
- If (the bed sensor is “out”AND NOT(“in” in less than a minute)) AND (other PIR activated), then the bed out is valid;
- (2)
- Sleep epoch: If the interval between each sleep epoch is less than 2 min, then merge the two epochs
- (1)
- Daily sleep pattern which displays a client’s daily sleep—wake cycles;
- (2)
- Weekly sleep pattern which includes:
- Client’s daily sleep pattern over past seven days. This section enables convenient visual comparison of sleep patterns and detection of unusual days;
- Summary and trend of seven days of daily sleep-wake episodes; and
- Summary and trend of seven days daily amount of sleep time.
- (3)
- Monthly sleep pattern, which includes:
- Summary and trend of four weeks of daily sleep-wake episodes; and
- Summary and trend of four weeks daily amount of sleep time.
5. Discussion
6. Conclusions
Acknowledgments
Conflicts of Interest
References
- Alzheimer’s Association. Alzheimer’s Disease Facts and Figures, Alzheimer’s & Dementia. 2012. Available online: http://www.alz.org/downloads/facts_figures_2012.pdf (accessed on 3 December 2013).
- Holland, A.J.; Hon, J.; Huppert, F.A.; Stevens, F. Incidence and course of dementia in people with down’s syndrome: Findings from a population-based study. J. Intellect. Disabil. Res. 2000, 44, 138–146. [Google Scholar]
- Alzheimer’s Society. Dementia 2012: A National Challenge. 2012. Available online: http://www.alzheimers.org.uk/site/scripts/download_info.php?fileID=1389 (accessed on 29 October 2013).
- World Health Organsiation. Dementia: Factsheet No 362. Available online: http://www.who.int/mediacentre/factsheets/fs362/en/ (accessed on 11 April 2013).
- Dementia UK. About Dementia Factsheet 362, 2011. Available online: http://www.dementiauk.org/information-support/about-dementia/#1 (accessed on 29 October 2013).
- Alzheimer’s Society. What is Alzheimer’s Disease? Available online: http://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=100 (accessed on 29 October 2013).
- Alzheimer’s Disease International. Early symptoms. 2012. Available online: http://www.alz.co.uk/info/early-symptoms (accessed on 29 October 2013).
- Alzheimer’s Association. The Economic Burden of Dementia and Associated Research Funding in the United Kingdom, 2012. Available online: http://www.dementia2010.org (accessed on 29 October 2013).
- Volicer, L.; Harper, D.G.; Manning, B.C.; Goldstein, R.; Satlin, A. Sundowning and circadian rhythms in Alzheimer’s disease. Amer. J. Psychiat. 2001, 158, 704–711. [Google Scholar] [CrossRef]
- Kim, P.; Louis, C.; Muralee, S.; Tampi, R.R. Sundowning syndrome in the older patient. Clin. Geriatr. 2005, 13, 32–36. [Google Scholar]
- Dewing, J. Sundowning in older people with dementia: Evidence base, nursing assessment and interventions. Nurs. Older People 2003, 15, 24–31. [Google Scholar] [CrossRef]
- Kerr, D.; Wilkinson, H.; Cunningham, C. Supporting Older People in Care Homes at Night. 2008. Available online: http://www.jrf.org.uk/publications/supporting-older-people-care-homes-night (accessed on 19 March 2013).
- Somnia Project. Optimising Quality of Sleep among Older People in the Community and Care Homes: An Integrated Approach, 2010. Available online: http://www.somnia.surrey.ac.uk/bp.html (accessed on 29 October 2013).
- Orpwood, R.; Adlam, T.; Evans, N.; Chadd, J.; Self, D. Evaluation of an assisted-living smart home for someone with dementia. J. Assist. Technol. 2008, 2, 13–21. [Google Scholar]
- Woods, B.; Aguirre, E.; Spector, A.E.; Orrell, M. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Peng, W.; Wang, Y.; Zhang, Y.; Liang, C.M. Acupuncture for vascular dementia. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef]
- Woods, B.; Spector, A.E.; Jones, C.A.; Orrell, M.; Davies, S.P. Reminiscence therapy for dementia. Cochrane Database Syst. Rev. 2005. [Google Scholar] [CrossRef]
- Vink, A.C.; Bruinsma, M.S.; Scholten, R.J.P.M. Music therapy for people with dementia. Cochrane Database Syst. Rev. 2003. [Google Scholar] [CrossRef]
- Alzheimer’s Society. National Dementia Strategies. Available online: http://alzheimers.org.uk/ndstrategies (accessed on 19 March 2013).
- National Institute for Health and Care Excellence. Care Pathway for Dementia, 2012. Available online: http://pathways.nice.org.uk/pathways/dementia (accessed on 29 October 2013).
- Fleming, R.; Shima, S. A Review of the Empirical Studies on the Effectiveness of Assistive Technology in the Care of People with Dementia. 2010. Available online: http://www.dementia.unsw.edu.au/images/dcrc/output-files/144-review_of_the_empirical_studies_on_the_effectiveness_of_assistive_technology_in_the_care_of_people_with_dementia.pdf (accessed on 19 March 2013).
- Carswell, W.; Mccullagh, P.J.; Augusto, J.C.; Martin, S.; Mulvenna, M.D.; Zheng, H.; Wang, H.Y.; Wallace, J.G.; Mcsorley, K.; Taylor, B.; et al. A review of the role of assistive technology for people with dementia in the hours of darkness. Technol. Health Care 2009, 17, 281–304. [Google Scholar]
- Kujala, S. User involvement: A review of the benefits and challenges. Behav. Inform. Technol. 2003, 22, 1–16. [Google Scholar] [CrossRef]
- Finaly, L. Phenomenology for Therapists; Wiley-Blackwell: Oxford, England, 2011. [Google Scholar]
- Nyard, L. How can we get access to the experience of people with dementia. Scand. J. Occup. Ther. 2006, 13, 101–112. [Google Scholar] [CrossRef]
- Powell, J.; Chiu, T.; Eysenbach, G. A systematic review of networked technologies supporting carers of people with dementia. J. Telemed. Telecare 2008, 14, 154–156. [Google Scholar] [CrossRef]
- Martin, S.; Kelly, G.; Kernohan, W.G.; Mccreight, B.; Nugent, C. Smart home technologies for health and social care support. Cochrane Database Syst. Rev. 2008. [Google Scholar] [CrossRef]
- Mulvenna, M.; Bergvall-Kareborn, B.; Galbraith, B.; Wallace, J.; Martin, S. Living Labs are Innovation Catalysts. In Innovation through Knowledge Transfer; Howlett, R.J., Ed.; Springer: Heidelberg, Germany, 2010; pp. 253–264. [Google Scholar]
- Mulvenna, M.; Wallace, J.; Moore, G.; Martin, S.; Galbraith, B.; Haaker, T.; Moelaert, F.; Jansson, M.; Bergvall-Kareborn, B.; Castellot Ricardo, L.; et al. Towards sustainable business models from healthcare technology research. Int. J. Comput. Health Care 2010, 1, 20–34. [Google Scholar] [CrossRef]
- Translating Research and Innovation Lab (TRAIL). Available online: http://trail.ulster.ac.uk/ (accessed on 19 March 2013).
- Higgins, P. Involving people with dementia in research. Nurs. Times 2013, 109, 20–23. [Google Scholar]
- Kitson, T. Exploring the ethics of dementia research: A response to Berghmans and TerMuelen: A psychosocial perspective. Int. J. Geriatr. Psychiat. 1995, 10, 655–657. [Google Scholar] [CrossRef]
- Medical Research Council. MRC Ethics Guide: Medical Research Involving Adults Who Cannot Consent; MRC: London, UK, 2007; Available online: http://www.mrc.ac.uk/Utilities/Documentrecord/index.htm?d=MRC004446 (accessed on 8 August 2013).
- Allen, K. Communication and Consultation. In Exploring Ways for Staff to Involve People with Dementia in Developing Services; The Policy Press: Bristol, UK, 2001. [Google Scholar]
- Dewing, J. Participatory research. A method for process consent with persons who have dementia. Dementia 2007, 6, 11–25. [Google Scholar] [CrossRef]
- Bowes, A. Ethical implications of lifestyle monitoring data in ageing research. Inf. Commun. Soc. 2012, 15, 5–22. [Google Scholar] [CrossRef]
- Fold Telecare. Available online: http://www.foldgroup.co.uk/pages/27/telecare (accessed on 19 March 2013).
- Praxis Care. Available online: http://www.praxisprovides.com/care-scheme/st-pauls-court-dementia-care (accessed on 19 March 2013).
- Mccullagh, P.J.; Carswell, W.; Mulvenna, M.; Augusto, J.C.; Zheng, H.; Jeffers, P. Nocturnal Sensing and Intervention for Assisted Living of People with Dementia. Healthcare Sensor Networks; CRC Press Taylor & Francis Group: Boca Raton, FL, USA, 2012; pp. 283–303. [Google Scholar]
- Wang, H.Y.; Zheng, H.; Augusto, J.C.; Martin, S.; Mulvenna, M.; Carswell, W.; Wallace, J.; Jeffers, P.; Taylor, B.; Mcsorley, K. Monitoring and Analysis of Sleep Pattern for People with Early Dementia. In Proceedings of the 2010 IEEE International Conference on Bioinformatics and Biomedicine Workshops (BIBMW), Hong Kong, China, 18–21 December 2010; pp. 405–410.
- Nikamalfard, H.H.; Zheng, H.Y.; Wang, H.Y.; Jeffers, P.; Mulvenna, M.; Mccullag, P.J.; Martin, S.; Wallace, J.; Augusto, J.C.; Carswell, W.; et al. Knowledge Discovery from Activity Monitoring to Support Independent Living of People with Early Dementia. In Proceedings of the IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI 2012) in conjunction with the 8th International Symposium on Medical Devices and Biosensors and the 7th International Symposium on Biomedical and Health Engineering, Hong Kong and Shenzhen, China, 2–7 January 2012; pp. 910–913.
- Zheng, H.; Wang, H.Y.; Nikamalfard, H.; Mulvenna, M.; Mccullagh, P.J.; Martin, S.; Wallace, J.; Jeffers, P. PAViS: Pattern analysis and visualization system for sleep monitoring in ambient assisted living. Int. J. Comput. Health Care 2012, 4, 320–332. [Google Scholar]
- Clarke, Z.; Langley, J.; Judge, S.; Hawley, M.; Hosking, I.; Heron, N. User Involvement in the Early Development of Assistive Technology Devices. In Everyday Technology for Independence and Care—AAATE 2011; IOS Press: Amsterdam, The Netherlands, 2011; pp. 362–373. [Google Scholar]
- Martin, S.; Cunningham, C.; Nugent, C. Ethical considerations for integrating technology into community based service models for adults with dementia. Alzheimer’s Care Today 2007, 8, 251–259. [Google Scholar]
- Martin, S.; Bengtsson, J.E.; Dröes, R.M. Assistive Technologies and Issues Relating to Privacy, Ethics and Security. In Supporting People with Dementia Using Pervasive Health Technologies; Mulvenna, M.D., Nugent, C.D., Eds.; Advanced Information and Knowledge Processing Series; Springer: Heidelberg, Germany, 2010; pp. 63–78. [Google Scholar]
- Green, L. Ethics and community-based participatory research: Commentary on Minkler. Health Educ. Behav. 2004, 31, 1–4. [Google Scholar]
- Minkler, M. Ethical challenges for the “outside” researcher in community-based participatory research. Health Educ. Behav. 2004, 6, 684–697. [Google Scholar] [CrossRef]
- Scherer, M.J. Living in the State of Stuck: How Technology Impacts the Lives of People with Disabilities, 3rd ed.; Brookline Books: Cambridge, MA, USA, 2000. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Martin, S.; Augusto, J.C.; McCullagh, P.; Carswell, W.; Zheng, H.; Wang, H.; Wallace, J.; Mulvenna, M. Participatory Research to Design a Novel Telehealth System to Support the Night-Time Needs of People with Dementia: NOCTURNAL. Int. J. Environ. Res. Public Health 2013, 10, 6764-6782. https://doi.org/10.3390/ijerph10126764
Martin S, Augusto JC, McCullagh P, Carswell W, Zheng H, Wang H, Wallace J, Mulvenna M. Participatory Research to Design a Novel Telehealth System to Support the Night-Time Needs of People with Dementia: NOCTURNAL. International Journal of Environmental Research and Public Health. 2013; 10(12):6764-6782. https://doi.org/10.3390/ijerph10126764
Chicago/Turabian StyleMartin, Suzanne, Juan Carlos Augusto, Paul McCullagh, William Carswell, Huiru Zheng, Haiying Wang, Jonathan Wallace, and Maurice Mulvenna. 2013. "Participatory Research to Design a Novel Telehealth System to Support the Night-Time Needs of People with Dementia: NOCTURNAL" International Journal of Environmental Research and Public Health 10, no. 12: 6764-6782. https://doi.org/10.3390/ijerph10126764








