Crossing the Telemedicine Chasm: Have the U.S. Barriers to Widespread Adoption of Telemedicine Been Significantly Reduced? †
Abstract
:1. Introduction
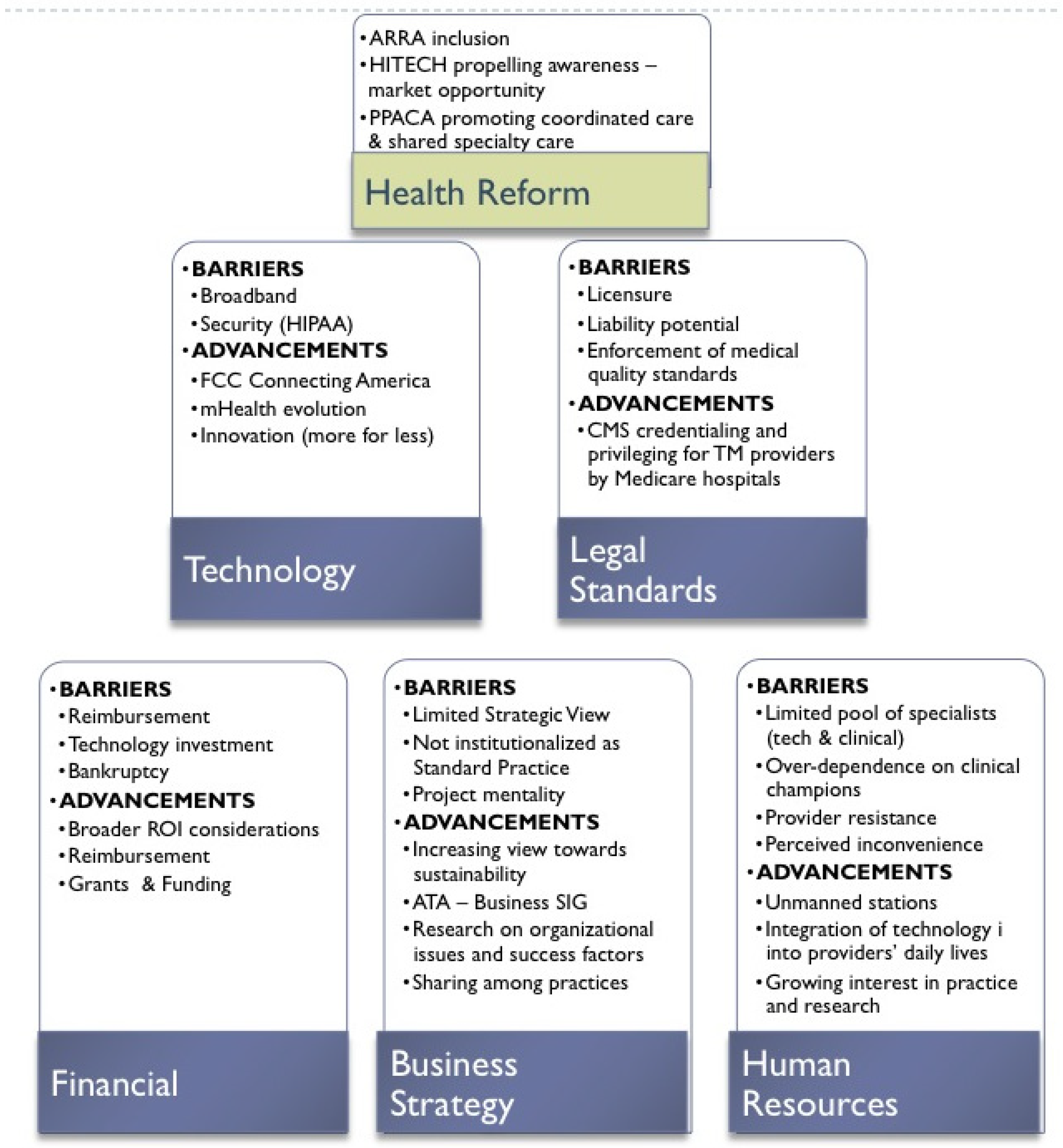
2. Health Reform and Telemedicine
2.1. Technology
2.1.1. Barriers
2.1.2. Recent Advancements
2.2. Legal
2.2.1. Barriers
2.2.2. Recent Advancements
2.3. Financial
2.3.1. Barriers
2.3.2. Recent Advancements
2.4. Business Strategy
2.4.1. Barriers
2.4.2. Recent Advancements
2.5. Human Resources
2.5.1. Barriers
2.5.2. Recent Advancements
3. Conclusions—Road to the Future
Acknowledgments
Conflicts of Interest
References
- Sood, S.; Mbarika, V.; Jugoo, S.; Dookhy, R.; Doarn, C.R.; Prakash, N.; Merrell, R.C. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed. e-Health 2007, 13, 573–590. [Google Scholar]
- Ackerman, M.J.; Filart, R.; Burgess, L.P.; Lee, I.; Poropatich, R.K. Developing next-generation telehealth tools and technologies: Patients, systems, and data perspectives. Telemed. e-Health 2010, 16, 93–95. [Google Scholar] [CrossRef]
- Norris, A.C. Essentials of Telemedicine and Telecare; John Wiley & Sons, Inc.: New York, NY, USA, 2001. [Google Scholar]
- Darkins, A.W.; Cary, M.A. Telemedicine and Telehealth: Principles, Policies, Performance, and Pitfalls; Springer Publishing Company, Inc.: New York, NY, USA, 2000. [Google Scholar]
- Rashid, L. Bashshur compelling issues in telemedicine. Telemed. e-Health 2013, 19, 330–332. [Google Scholar] [CrossRef]
- Buntin, M.B.; Jain, S.H.; Blumenthal, D. Health information technology: Laying the infrastructure for national health reform. Health Aff. 2010, 29, 1214–1219. [Google Scholar]
- Fisher, E.S. Building a medical neighborhood for the medical home. N. Engl. J. Med. 2008, 359, 1202–1205. [Google Scholar]
- American Telemedicine Association. Comment Letter to Dr. Donald M. Berwick, Administrator of the Centers for Medicare & Medicaid Services, on Accountable Care Organization Proposed Regulations; Centers for Medicare & Medicaid Services: Washington, DC, USA, 2011; pp. 1–6. [Google Scholar]
- Bashshur, R.L.; Shannon, G.W.; Krupinski, E.A.; Grigsby, J.; Kvedar, J.C.; Weinstein, R.S.; Sanders, J.H.; Rheuban, K.S.; Nesbitt, T.S.; Alverson, D.C.; et al. National telemedicine initiatives: Essential to healthcare reform. Telemed. e-Health 2009, 15, 600–610. [Google Scholar] [CrossRef]
- Bates, D.W.; Bitton, A. The future of health information technology in the patient-centered medical home. Health Aff. 2010, 29, 614–621. [Google Scholar] [CrossRef]
- Lorenzo Moreno, P.D.; Deborah Peikes, P.D.; Amy Krilla, M.S.W. Necessary But Not Sufficient: The HITECH Act and Health Information Technology’s Potential to Build Medical Homes (Prepared by Mathematica Policy Research under Contract No. HHSA290200900019I TO2); AHRQ Publication No. 10-0080-EF; Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services: Rockville, MD, USA, June 2010. [Google Scholar]
- Stark, R.; Shear, J. Federal Patient Centered Medical Home (PCMH) Collaborative: Catalouge of Federal PCMH Activities as of October 2012; PCMH: Rockville, MD, USA, 2012; pp. 1–6. [Google Scholar]
- Bresnick, J. UCLA Awarded Grant to Study Telemedicine, Behavioral Health. Available online: http://ehrintelligence.com/2013/06/12/ucla-awarded-grant-to-study-telemedicine-behavioral-health/ (accessed on 19 July 2013).
- Koch, S. Home telehealth—Current state and future trends. Int. J. Med. Inform. 2006, 75, 565–576. [Google Scholar] [CrossRef]
- American Telemedicine Association. Telemedicine in the Patient Protection and Affordable Care Act; American Telemedicine Association: Washington, DC, USA, 2010. [Google Scholar]
- Alverson, D.C.; Shannon, S.; Sullivan, E.; Prill, A.; Effertz, G.; Helitzer, D.; Beffort, S.; Preston, A. Telehealth in the trenches: Reporting back from the frontlines in Rural America. Telemed. e-Health 2004, 10, S-95–S-109. [Google Scholar]
- OECD Broadband Statistics Update. Available online: http://www.oecd.org/sti/broadband/broadband-statistics-update.htm (accessed on 6 June 2012).
- Zickuhr, K. Pew Research Center’s Internet & American Life Project; Pew Research Center: Washington, DC, USA, 2013. [Google Scholar]
- Federal Communication Commission. Connecting America: The National Broadband Plan; The National Broadband Plan: Washington, DC, USA, 2010; p. 145.
- Bennett, R.; Stewart, L.A.; Atkinson, R.D. The Whole Picture: Where America’s Broadband Networks Really Stand; The Information Technology & Innovation Foundation: Washington, DC, USA, 2013. [Google Scholar]
- Greenfield, A. Everywhere: The Dawning Age of Ubiquitous Computing, 1st ed.; New Riders: Berkeley, CA, USA, 2006. [Google Scholar]
- Agoulmine, N. Efficient and cost-effective communications in ubiquitous healthcare: Wireless sensors, devices and solutions. IEEE Xplore 2012, 50, 90–91. [Google Scholar]
- Avancha, S.; Baxi, A.; Kotz, D. Privacy in mobile technology for personal healthcare. ACM Comput. Surv. 2012, 45, 1–54. [Google Scholar] [CrossRef]
- Kim, J. 12 Telemedicine Innovations That Will Shape Healthcare’s Future. Available online: http://www.cio.com/slideshow/detail/101906 (accessed on 5 November 2013).
- Lisetti, C.; Yasavur, U.; Leon, C.D.; Amini, R.; Rishe, N.; Visser, U. Building an On-Demand Avatar-Based Health Intervention for Behavior Change. In Proceedings of the 25th Florida Artificial Intelligence Research Society—FLAIRS Conference, Marco Island, FL, USA, 23–25 May 2012.
- Jacobson, P.D.; Selvin, E. Licensing telemedicine: The need for a national system. Telemed e-Health 2000, 6, 429–439. [Google Scholar] [CrossRef]
- Center for Telehealth & e-Health Law. Available online: www.ctel.org/about-2/our-mission/# (accessed on 8 July 2013).
- American Telemedicine Association Telemedicine Defined. Available online: http://www.americantelemed.org/i4a/pages/index.cfm?pageid=3333 (accessed on 12 July 2013).
- Rowthorn, V.; Hoffmann, D. Legal Impediments to the difussion of telemedicine. J. Health Care Law Policy 2011, 14, 1–54. [Google Scholar]
- Sao, D.; Amar, G.; Gantz, D. Chapter 20: Legal and Regulatory Barriers to Telemedicine in the United States: Public and Private Approaches toward Health Care Reform. In The Globalization of Health Care: Legal and Ethical Issues; Cohen, I.G., Ed.; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Delaware Regulations Title 24: Professional Regulation; State of Delaware General Assembly: Washington, DC, USA, 2012.
- Centers for Medicare & Medicaid Services. Available online: http://www.cms.gov/Regulations-and-Guidelines/Legislation/CFCsAndCoPs/index.html (accessed on 8 July 2013).
- Federation of State Medical Boards. Telemedicine Overview: Board-by-Board Approach. Available online: www.fsmb.org/pdf/grpol_telemedicine_licensure.pdf (accessed on 5 November 2013).
- Field, M.J. Telemedicine: A Guide to Assessing Telecommunications in Health Care; The National Academy Press: Washington, DC, USA, 1996. [Google Scholar]
- Resnick, H.E.; Alwan, N. Use of health information technology in home health and hospice agencies: United States. JAMIA 2007, 17, 389–395. [Google Scholar]
- Menachemi, N.; Burke, D.E.; Ayers, D.J. Factors affecting the adoption of telemedicine—A multiple adopter perspective. J. Med. Syst. 2004, 28, 617–632. [Google Scholar]
- Telemedicine. Available online: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Delivery-Systems/Telemedicine.html (accessed on 12 July 2013).
- American Medical Association Telehealth Services. Available online: http://www.americantelemed.org/docs/default-source/policy/cms-medicare-telehealth-services-fact-sheet.pdf?sfvrsn=6 (accessed on 5 November 2013).
- Medicare Program; Revisions to Payment Policies under the Physician Fee Schedule, Clinical Laboratory Fee Schedule & Other Revisions to Part B for CY 2014; Medicare Program: Washington, DC, USA, 2013; pp. 43281–43532.
- Ackerman, K. Virginia Bill Mandates Telemedicine Coverage—Barrier Remain. Available online: http://www.ihealthbeat.org/insight/2010/virginia-bill-mandates-coverage-of-telemedicine-barriers-remain (accessed on 5 November 2013).
- Linkous, J. CEO: 7 Market Trends Shaping the Future of Telemedicine. Available online: http://www.americantelemed.org/news-landing/2013/01/08/ata-ceo-7-market-trends-shaping-the-future-of-telemedicine (accessed on 22 July 2013).
- Moehr, J.R.; Schaafsma, J.; Anglin, C.; Pantazi, S.V.; Grimm, N.A.; Anglin, S. Success factors for telehealth—A case study. Int. J. Med. Inform. 2006, 75, 755–763. [Google Scholar]
- LeRouge, C.; Tulu, B.; Forducey, P. The business of telemedicine: Strategy primer. Telemed. e-Health 2010, 16, 898–909. [Google Scholar]
- Gaur, P. The Future of mHealth. Available online: http://blogs.jpost.com/content/future-mhealth-pramod-gaur-vice-president-telehealth-unitedhealth-group (accessed on 12 July 2013).
- Pruitt, S. The office for the advancement of telehealth. Telemed. e-Health 2013, 19, 346–348. [Google Scholar]
- Ajith, N.T.; Lakshman, R.; Shankar, S. Multimodal interactive kiosk system for diabetes education and diagnosis in Rural India. Int. J. Comput. Appl. 2010, 1, 1–4. [Google Scholar]
- Cain, C.; Haque, S. Organizational Workflow and Its Impact on Work Quality. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Whitten, P.S.; Mackert, M.S. Addressing telehealth’s foremost barrier: Provider as initial gatekeeper. Int. J. Technol. Assess. Health Care 2005, 21, 517–521. [Google Scholar]
- Harnett, B.M.; Doarn, C.R.; Rosen, J.; Hannaford, B.; Broderick, T.J. Evaluation of unmanned airborne vehicles and mobile robotic telesurgery in an extreme environment. Telemed. e-Health 2008, 14, 539–544. [Google Scholar]
- Agha, Z.; Schapira, R.; Laud, P.; McNutt, G.; Roter, D. Patient satisfaction with physician–patient communication during telemedicine. Telemed. e-Health 2009, 15, 830–839. [Google Scholar]
- Mair, F.; Whitten, P. Systematic review of studies of patient satisfaction with telemedicine. Br. Med. J. 2000, 320, 1517–1520. [Google Scholar]
- Doarn, C.R.; Merrell, R.C. What a legacy—Did they realize what they might start? Telemed. e-Health 2013, 19, 501. [Google Scholar]
- Gupta, A.; Sao, D. The constitutionality of current legal barriers to telemedicine in the United States: Analysis and future directions of its relationship to national and international health care reform. Health Matrix 2012, 21, 385–442. [Google Scholar]
- Raoin, K. Datamonitor: Homecare Telehealth Expected to Grow Despite Current Barriers to Adoption. Available online: http://it.tmcnet.com/news/2007/08/30/2897900.htm (accessed on 12 July 2013).
- Bashshur, R.L.; Shannon, G.W. The Transformation of Telemedicine. In History of Telemedicine; Mary Ann Liebert, Inc.: New Rochelle, NY, USA, 2009; pp. 317–353. [Google Scholar]
- Gawande, A. Big Med: Restaurant Chains Have Managed to Combine Quality Control, Cost Control, and Innovation. Can Hospitals? Available online: http://www.newyorker.com/reporting/2012/08/13/120813fa_fact_gawande (accessed on 5 November 2013).
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
LeRouge, C.; Garfield, M.J. Crossing the Telemedicine Chasm: Have the U.S. Barriers to Widespread Adoption of Telemedicine Been Significantly Reduced? . Int. J. Environ. Res. Public Health 2013, 10, 6472-6484. https://doi.org/10.3390/ijerph10126472
LeRouge C, Garfield MJ. Crossing the Telemedicine Chasm: Have the U.S. Barriers to Widespread Adoption of Telemedicine Been Significantly Reduced? . International Journal of Environmental Research and Public Health. 2013; 10(12):6472-6484. https://doi.org/10.3390/ijerph10126472
Chicago/Turabian StyleLeRouge, Cynthia, and Monica J. Garfield. 2013. "Crossing the Telemedicine Chasm: Have the U.S. Barriers to Widespread Adoption of Telemedicine Been Significantly Reduced? " International Journal of Environmental Research and Public Health 10, no. 12: 6472-6484. https://doi.org/10.3390/ijerph10126472
APA StyleLeRouge, C., & Garfield, M. J. (2013). Crossing the Telemedicine Chasm: Have the U.S. Barriers to Widespread Adoption of Telemedicine Been Significantly Reduced? . International Journal of Environmental Research and Public Health, 10(12), 6472-6484. https://doi.org/10.3390/ijerph10126472



