Inhibition of CYP2B6 by Medicinal Plant Extracts: Implication for Use of Efavirenz and Nevirapine-Based Highly Active Anti-Retroviral Therapy (HAART) in Resource-Limited Settings
Abstract
:1. Introduction
2. Results
2.1. Inhibition Screening and IC50 Determination
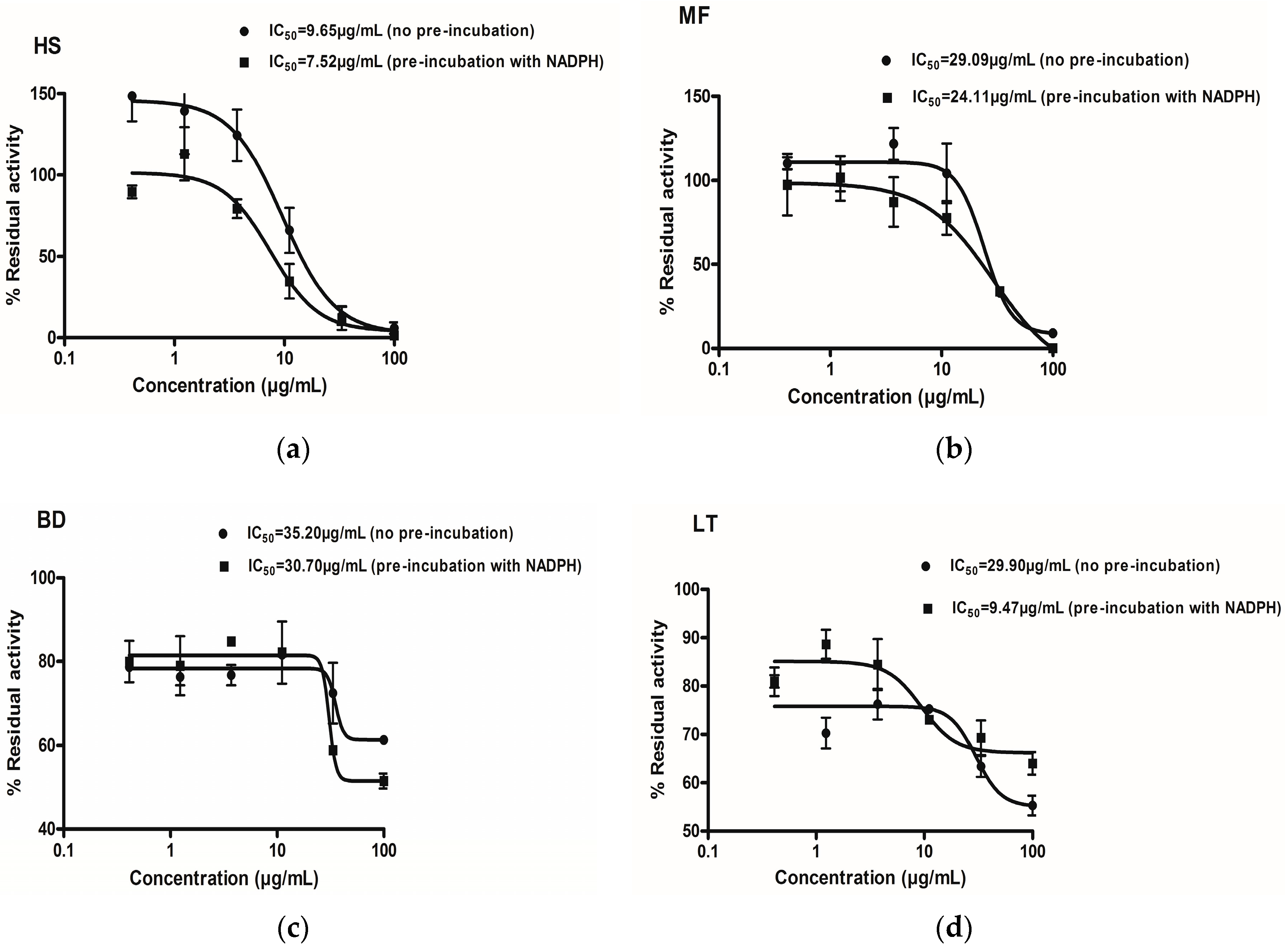
| Inhibitor | Conventional IC50 (µg/mL) (Mean ± SEM) | IC50 (no Pre-Incubation with NADPH) (µg/mL) (Mean ± SEM) | IC50 (Pre-Incubation with NADPH) (µg/mL) (Mean ± SEM) | Fold Shift (−IC50/+IC50) |
|---|---|---|---|---|
| Newbouldia laevi | 100 ± 8.71 | ND | ND | ND |
| Hyptis suaveolens | 19.09 ± 1.16 | 10.60 ± 1.32 | 7.52 ± 1.20 | 1.40 |
| Launeae taraxacifolia | 33.87 ± 1.54 | 29.90 ± 1.32 | 9.47 ± 1.41 | 3.17 |
| Boerhavia diffusa | 34.93± 1.06 | 35.20 ± 2.86 | 30.70 ± 2.02 | 1.20 |
| Myrothamnus flabellifolious | 23.66 ± 4.86 | 29.09 ± 1.74 | 24.11 ± 1.24 | 1.21 |
| Miconazole | 0.53 ± 0.14 | 0.63 ± 0.15 | 0.72 ± 0.20 | 0.88 |
2.2. Prediction of in Vivo Herb-Drug Interaction for IC50
| Herbal Extracts | % Yield | Recommended Herbal Dose (Single; mg) | Putative GIT Concentration (µg/mL) | Estimated Bioavailable Concentration (µg/mL) |
|---|---|---|---|---|
| Newbouldia laevis | 14.66 | 200 | 800 | 117.28 |
| Hyptis suaveolens | 6.51 | 400 | 1600 | 104.16 |
| Launaea taraxacifolia | 10.40 | 200 | 800 | 83.3 |
| Boerhavia diffusa | 11.24 | 200 | 800 | 89.92 |
| Myrothamnus flabellifolius | 10.80 | 200 | 800 | 86.4 |
| Herbal Extracts | Inhibitor Concentration (µg/mL) | IC50 (µg/mL) | Risk of HDI in the Gut * |
|---|---|---|---|
| Newbouldia laevis | 117.28 | 100 | Unlikely |
| Hyptis suaveolens | 104.16 | 20.33 | Likely |
| Launaea taraxacifolia | 83.20 | 33.87 | Likely |
| Boerhavia diffusa | 89.92 | 34.93 | Likely |
| Myrothamnus flabellifolius | 86.40 | 23.66 | Likely |
2.3. Time Dependent Inhibition (TDI) by IC50 Curve-Shift and Single Point NADPH Inhibition Screening Evaluation


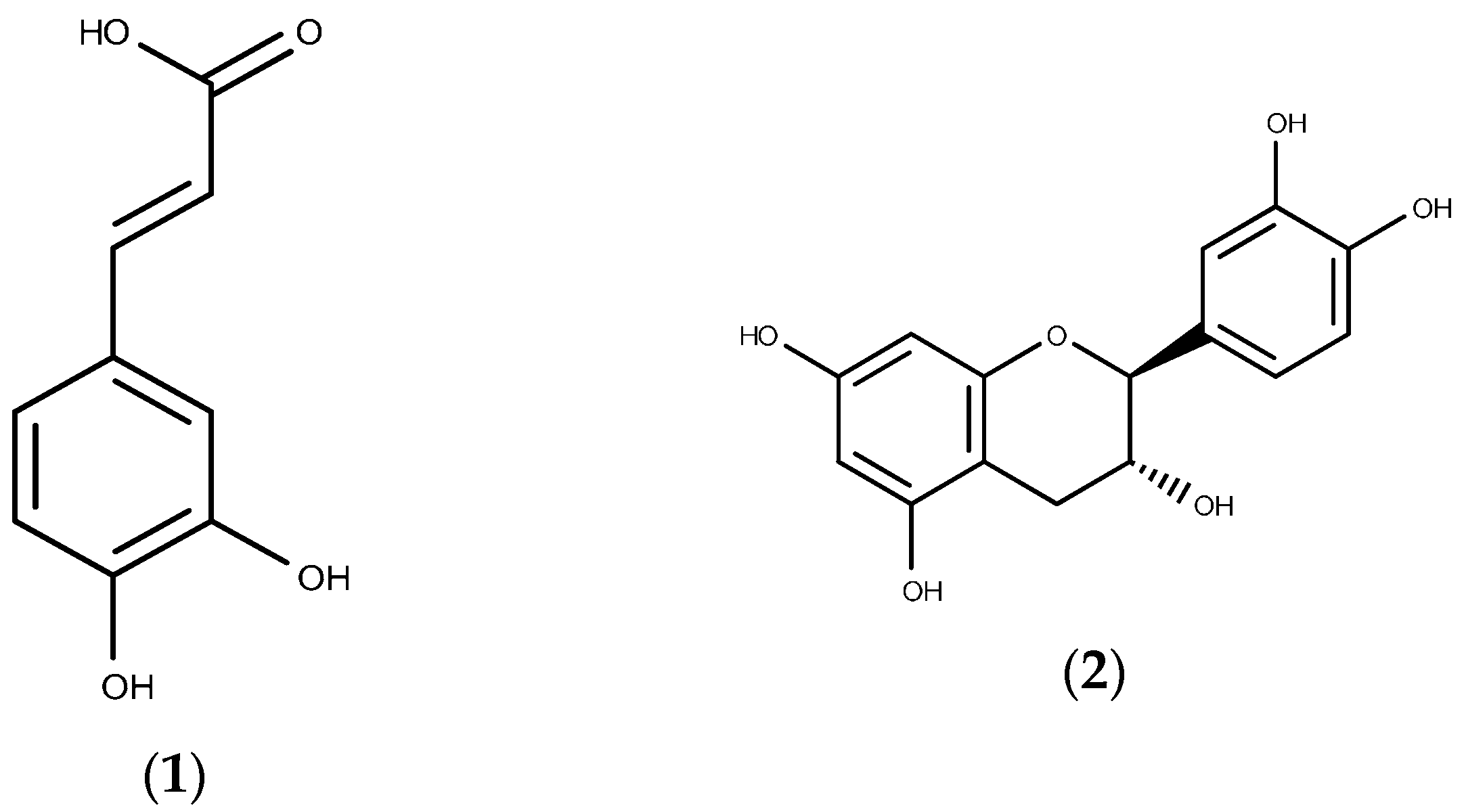
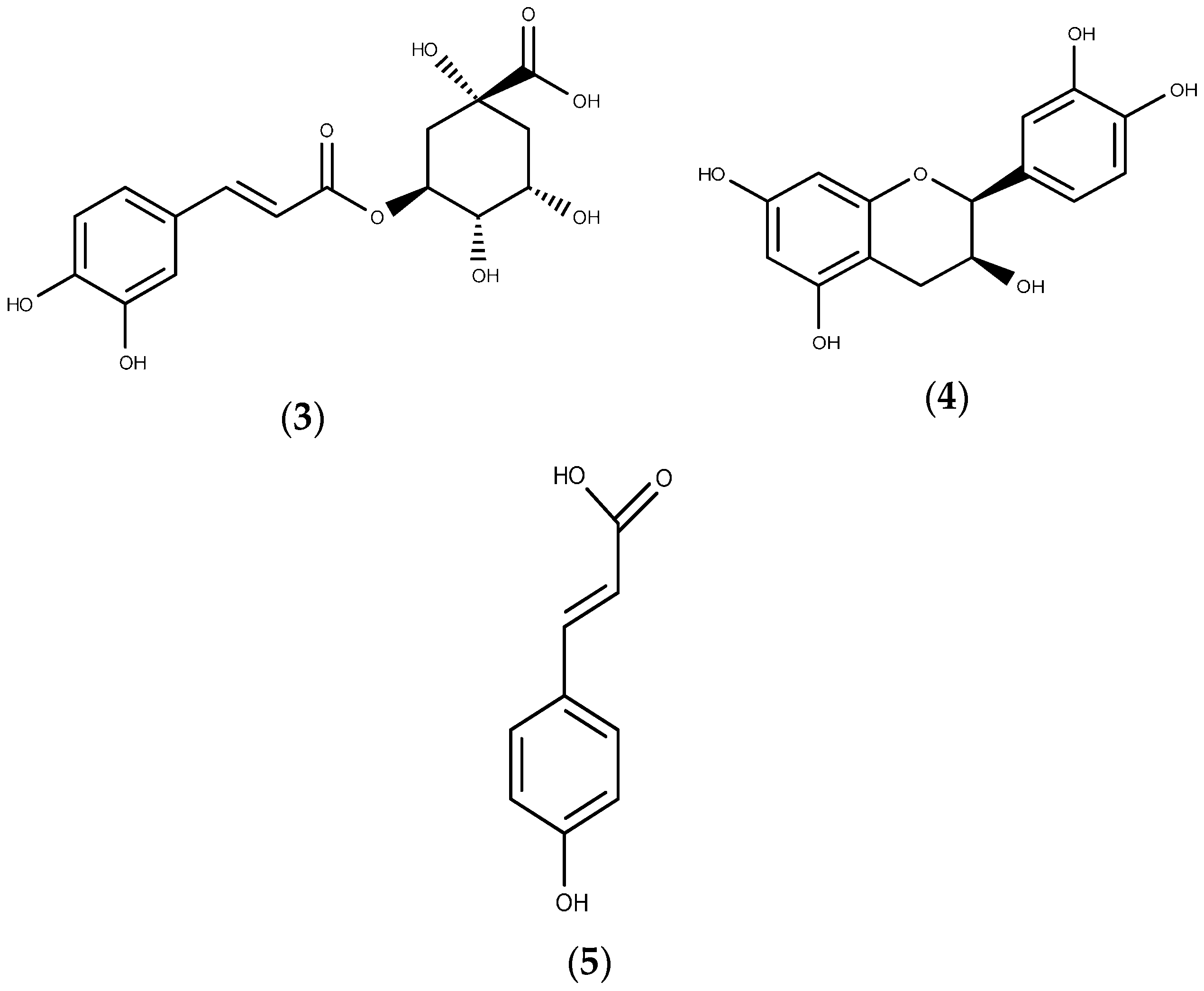
2.4. Relative Quantification of Selected Phenolic Compounds Using UPLC-MS
| Phenolic Compound | Newbouldia laevis (Mean ± SEM) | Hyptis suaveolens (Mean ± SEM) | Launaea taraxacifolia (Mean ± SEM) | Boerhavia diffusa (Mean ± SEM) | Myrothamnus flabellifolius (Mean ± SEM) |
|---|---|---|---|---|---|
| Catechin | Trace | Trace | Trace | 1.40 ± 0.03 | 27.58 ± 0.10 |
| p-Coumaric acid | 7.54 ± 0.10 | 75.25 ± 0.10 | 751.41 ± 1.30 | 13.89 ± 0.10 | 39.13 ± 0.21 |
| Caffeic acid | 10.01± 0.01 | 100.00 ± 0.97 | 998.59 ± 1.48 | 10.59 ± 0.06 | 3.98 ± 0.01 |
| Epicatechin | Trace | Trace | Trace | Trace | 170.06 ± 0.39 |
| Chlorogenic acid | 166.77 ± 0.20 | 1665.33 ± 0.87 | 1662.98 ± 2.10 | Trace | 5.84 ± 0.10 |
3. Discussion
4. Materials and Methods
4.1. Chemicals and Reagents
4.2. Plant Material
| Plant Species | Commonly Found African Countries | Purported Medicinal Value |
|---|---|---|
| Newbouldia laevis | Ghana, Togo, Nigeria, Congo | Anti-malaria, immune booster, anti-bacterial, anti-fungal |
| Hyptis suaveolens | Ghana, Togo, Nigeria, Congo, Benin, Guinea | Anti-bacterial, anti-fungal, anti-malaria, anti-cholesterol |
| Launaea taraxacifolia | Ghana, Togo, Nigeria, Congo, Benin, Guinea, Cote d’Ivoire | Anti-bacterial, anti-fungal, anti-malaria, anti-cholesterol, urinary infections, anti-diabetic |
| Boerhavia diffusa | Ghana, Togo, Nigeria, Congo, Benin, Guinea, Cote d’Ivoire, South Africa | Anti-bacterial, hepatoprotective, anti-nociceptive |
| Myrothamnus flabellifolious | Zimbabwe, Botswana, South Africa, Uganda, Egypt | Anti-viral, immune booster |
4.3. Extraction of Plant Material
4.4. Screening for Inhibition
4.5. Time-Dependent Inhibition (TDI) Assessment Using the IC50 Curve-Shift
4.6. Relative Quantification of Selected Phenolic Compounds Using UPLC-MS
4.7. Data Analysis
4.7.1. IC50 Determination
4.7.2. IC50 Curve-Shift for TDI Prediction, Point Screening and Relative Quantification of Phenolic Compound
4.7.3. Prediction of in Vivo Herb-Drug Interaction for IC50
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Basavaraj, K.H.; Navya, M.A.; Rashmi, R. Quality of life in HIV/AIDS. Indian J. Sex. Transm. Dis. 2010, 31, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Oguntibeju, O.O. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV/AIDS 2012, 4, 117–124. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antiretroviral Therapy for HIV Infection in Adults and Adolescents; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Bhatt, N.B.; Baudin, E.; Meggi, B.; da Silva, C.; Barrail-Tran, A.; Furlan, V.; Grinsztejn, B.; Bonnet, M.; Taburet, A.M.; Jani, I.V.; et al. Nevirapine or efavirenz for tuberculosis and HIV coinfected patients: Exposure and virological failure relationship. J. Antimicrob. Chemother. 2014, 70, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Rodney, P.; Ndjakani, Y.; Ceesay, F.K.; Wilson, N.O. Addressing the Impact of HIV/AIDS on Women and Children in Sub-Saharan Africa: PEPFAR, the U.S. Strategy. Afr. Today 2011, 57, 64–76. [Google Scholar] [CrossRef]
- Yimer, G.; Amogne, W.; Habtewold, A.; Makonnen, E.; Ueda, N.; Suda, A.; Worku, A.; Haefeli, W.E.; Burhenne, J.; Aderaye, G.; et al. High plasma efavirenz level and CYP2B6 *6 are associated with efavirenz-based HAART-induced liver injury in the treatment of naïve HIV patients from Ethiopia: A prospective cohort study. Pharmacogenom. J. 2012, 12, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Ward, B.A.; Gorski, J.C.; Jones, D.R.; Hall, S.D.; Flockhart, D.A.; Desta, Z. The cytochrome P450 2B6 (CYP2B6) is the main catalyst of efavirenz primary and secondary metabolism: Implication for HIV/AIDS therapy and utility of efavirenz as a substrate marker of CYP2B6 catalytic activity. J. Pharmacol. Exp. Ther. 2003, 306, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Haas, D.W.; Gebretsadik, T.; Mayo, G.; Menon, U.N.; Acosta, E.P.; Shintani, A.; Floyd, M.; Stein, C.M.; Wilkinson, G.R. Associations between CYP2B6 polymorphisms and pharmacokinetics after a single dose of nevirapine or efavirenz in African americans. J. Infect. Dis. 2009, 199, 872–880. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, K.; Gatanaga, H.; Tachikawa, N.; Teruya, K.; Kikuchi, Y.; Yoshino, M.; Kuwahara, T.; Shirasaka, T.; Kimura, S.; Oka, S. Homozygous CYP2B6 *6 (Q172H and K262R) correlates with high plasma efavirenz concentrations in HIV-1 patients treated with standard efavirenz-containing regimens. Biochem. Biophys. Res. Commun. 2004, 319, 1322–1326. [Google Scholar] [CrossRef] [PubMed]
- Mugusi, S.; Ngaimisi, E.; Janabi, M.; Minzi, O.; Bakari, M.; Riedel, K.D.; Burhenne, J.; Lindquist, L.; Mugusi, F.; Sandstrom, E.; et al. Liver enzyme abnormalities and associated risk factors in HIV patients on efavirenz-based HAART with or without tuberculosis co-infection in Tanzania. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Thomford, N.E.; Dzobo, K.; Chopera, D.; Wonkam, A.; Skelton, M.; Blackhurst, D.; Chirikure, S.; Dandara, C. Pharmacogenomics Implications of Using Herbal Medicinal Plants on African Populations in Health Transition. Pharmaceuticals 2015, 8, 637–663. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.G.; Oh, M.S. Herbal medicines for the prevention and treatment of Alzheimer’s disease. Curr. Pharm. Des. 2012, 18, 57–75. [Google Scholar] [PubMed]
- Chien, C.F.; Wu, Y.T.; Tsai, T.H. Biological analysis of herbal medicines used for the treatment of liver diseases. Biomed. Chromatogr. 2011, 25, 21–38. [Google Scholar] [CrossRef] [PubMed]
- Dhiman, R.K.; Chawla, Y.K. Herbal medicines for liver diseases. Dig. Dis. Sci. 2005, 50, 1807–1812. [Google Scholar] [CrossRef] [PubMed]
- Dahanukar, S.A.; Kulkarni, R.A.; Rege, N.N. Pharmacology of medicinal plants and natural products. Indian J. Pharmacol. 2000, 32, 81–118. [Google Scholar]
- Efferth, T.; Koch, E. Complex interactions between phytochemicals. The multi-target therapeutic concept of phytotherapy. Curr. Drug Targets 2011, 12, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.; Wightman, E. Herbal extracts and phytochemicals: Plant secondary metabolites and the enhancement of human brain function. Adv. Nutr. Int. Rev. J. 2011, 2, 32–50. [Google Scholar] [CrossRef] [PubMed]
- Koffuor, G.A.; Woode, E.; Amaning-Danquah, C. Potential Drug Interactions of a Polyherbal Antihypertensive Mixture in Ghana. Pharmacol. Sin. 2011, 2, 39–45. [Google Scholar]
- Chen, X.W.; Serag, E.S.; Sneed, K.B.; Liang, J.; Chew, H.; Pan, S.-Y.; Zhou, S.-F. Clinical herbal interactions with conventional drugs: From molecules to maladies. Curr. Med. Chem. 2011, 18, 4836–4850. [Google Scholar] [CrossRef] [PubMed]
- He, S.M.; Chan, E.; Zhou, S.F. ADME properties of herbal medicines in humans: Evidence, challenges and strategies. Curr. Pharm. Des. 2011, 17, 357–407. [Google Scholar] [CrossRef] [PubMed]
- Ingelman-Sundberg, M. Pharmacogenetics of cytochrome P450 and its applications in drug therapy: The past, present and future. Trends Pharmacol. Sci. 2004, 25, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Turpeinen, M.; Zanger, U.M. Cytochrome P450 2B6: Function, genetics, and clinical relevance. Drug Metab. Drug Interact. 2012, 27, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Mo, S.L.; Liu, Y.H.; Duan, W.; Wei, M.Q.; Kanwar, J.R.; Zhou, S.F. Substrate specificity, regulation, and polymorphism of human cytochrome P450 2B6. Curr. Drug Metab. 2009, 10, 730–753. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tompkins, L.M. CYP2B6: New insights into a historically overlooked cytochrome P450 isozyme. Curr. Drug Metab. 2008, 9, 598–610. [Google Scholar] [CrossRef] [PubMed]
- Turpeinen, M.; Raunio, H.; Pelkonen, O. The functional role of CYP2B6 in human drug metabolism: Substrates and inhibitors in vitro, in vivo and in silico. Curr. Drug Metab. 2006, 7, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Zanger, U.M.; Klein, K. Pharmacogenetics of cytochrome P450 2B6 (CYP2B6): Advances on polymorphisms, mechanisms, and clinical relevance. Front. Genet. 2013, 4, 24. [Google Scholar] [CrossRef] [PubMed]
- McGinnity, D.F.; Tucker, J.; Trigg, S.; Riley, R.J. Prediction of CYP2C9-mediated drug-drug interactions: A comparison using data from recombinant enzymes and human hepatocytes. Drug Metab. Dispos. 2005, 33, 1700–1707. [Google Scholar] [CrossRef] [PubMed]
- Abourashed, E. Bioavailability of Plant-Derived Antioxidants. Antioxidants 2013, 2, 309–325. [Google Scholar] [CrossRef] [PubMed]
- Stout, C.W.; Weinstock, J.; Homoud, M.K.; Wang, P.J.N.; Estes, A.M.; Link, M.S. Herbal medicine: Beneficial effects, side effects, and promising new research in the treatment of arrhythmias. Curr. Cardiol. Rep. 2003, 5, 395–401. [Google Scholar]
- Djuv, A.; Nilsen, O.G.; Steinsbekk, A. The co-use of conventional drugs and herbs among patients in Norwegian general practice: A cross-sectional study. BMC Complement. Altern. Med. 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Fugh-berman, A. Herb-drug interactions. Lancet 2000, 355, 134–138. [Google Scholar] [CrossRef]
- Chen, X.W.; Sneed, K.B.; Pan, S.Y.; Cao, C.; Kanwar, R.J.; Chew, H.; Zhou, S.F. Herb-drug interactions and mechanistic and clinical considerations. Curr. Drug Metab. 2012, 13, 640–651. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.M.; Strong, J.M.; Zhang, L.; Reynolds, K.S.; Nallani, S.; Temple, R.; Abraham, S.; Al Habet, S.; Baweja, R.K.; Burckart, G.J.; et al. New era in drug interaction evaluation: US Food and Drug Administration update on CYP enzymes, transporters, and the guidance process. J. Clin. Pharmacol. 2008, 48, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Bjornsson, T.D.; Callaghan, J.T.; Einolf, H.J.; Fischer, V.; Gan, L.; Grimm, S.; Kao, J.; King, S.P.; Miwa, G.; Ni, L.; et al. The conduct of in vitro and in vivo drug-drug interaction studies: A PhRMA perspective. J. Clin. Pharmacol. 2003, 43, 443–469. [Google Scholar]
- Zhang, L.; Zhang, Y.D.; Zhao, P.; Huang, S.M. Predicting drug-drug interactions: An FDA perspective. AAPS J. 2009, 11, 300–306. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Guideline on the Investigation of Drug Interactions; Committee for Human Medicinal Products (CHMP); CPMP/EWP/560/560/95/Rev; London, UK, 2015; pp. 1–59. [Google Scholar]
- Manda, V.K.; Dale, O.R.; Awortwe, C.; Ali, Z.; Khan, I.; Walker, L.; Khan, S.I. Evaluation of drug interaction potential of Labisia pumila (Kacip Fatimah) and its constituents. Front. Pharmacol. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Obach, R.S.; Walsky, R.L.; Venkatakrishnan, K. Mechanism-based inactivation of human cytochrome p450 enzymes and the prediction of drug-drug interactions. Drug Metab. Dispos. 2007, 35, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Berry, L.M.; Zhao, Z. An examination of IC50 and IC50-shift experiments in assessing time-dependent inhibition of CYP3A4, CYP2D6 and CYP2C9 in human liver microsomes. Drug Metab. Lett. 2008, 2, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Lu, C.; Balani, S.K.; Gan, L.-S. A refined cytochrome P540 IC50 shift assay for reliably identifying CYP3A time-dependent inhibitors. Drug Metab. Dispos. 2011, 39, 1054–1057. [Google Scholar] [CrossRef] [PubMed]
- Grimm, S.W.; Einolf, H.J.; Hall, S.D.; He, K.; Lim, H.K.; Ling, K.H.J.; Lu, C.; Nomeir, A.; Seibert, E.; Skordos, K.W.; et al. The conduct of in vitro studies to address time-dependent inhibition of drug-metabolizing enzymes: A perspective of the Pharmaceutical Research and Manufacturers of America. Drug Metab. Dispos. 2009, 37, 1355–1370. [Google Scholar] [CrossRef] [PubMed]
- Adinortey, M.B.; Sarfo, J.K.; Quayson, E.T.; Weremfo, A.; Adinortey, C.A. Phytochemical Screening, Proximate and Mineral Composition of Launaea taraxacifolia Leaves. Res. J. Med. Plant 2012, 6, 171–179. [Google Scholar] [CrossRef]
- Ocama, P.; Katwere, M.; Piloya, T.; Feld, J.; Opio, K.C.; Kambugu, A.; Katabira, E.; Thomas, D.; Colebunders, R.; Ronald, A. The spectrum of liver diseases in HIV infected individuals at an HIV treatment clinic in Kampala, Uganda. Afr. Health Sci. 2008, 8, 8–12. [Google Scholar] [PubMed]
- Price, J.C.; Thio, C.L. Liver disease in the HIV-infected individual. Clin. Gastroenterol. Hepatol. 2010, 8, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Husain, N.E.O.; Ahmed, M.H. Managing dyslipidemia in HIV/AIDS patients: Challenges and solutions. HIV/AIDS 2015, 7, 1–10. [Google Scholar] [PubMed]
- Lo, J. Dyslipidemia and lipid management in HIV-infected patients. Curr. Opin. Endocrinol. Diabetes Obes. 2011, 18, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Feeney, E.R.; Mallon, P.W.G. HIV and HAART-Associated Dyslipidemia. Open Cardiovasc. Med. J. 2011, 5, 49–63. [Google Scholar] [CrossRef] [PubMed]
- Da Neto, S.P.L.F.; das Neves, M.B.; Ribeiro-Rodrigues, R.; Page, K.; Miranda, A.E. Dyslipidemia and fasting glucose impairment among HIV patients three years after the first antiretroviral regimen in a Brazilian AIDS outpatient clinic. Braz. J. Infect. Dis. 2013, 17, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Estrada, V.; Portilla, J. Dyslipidemia related to antiretroviral therapy. AIDS Rev. 2011, 13, 49–56. [Google Scholar] [PubMed]
- Rastogi, H.; Jana, S. Evaluation of Inhibitory Effects of Caffeic acid and Quercetin on Human Liver Cytochrome P450 Activities. Phytother. Res. 2014, 28, 1873–1878. [Google Scholar] [CrossRef] [PubMed]
- Baer-Dubowska, W.; Szaefer, H.; Krajka-Kuzniak, V. Inhibition of murine hepatic cytochrome P450 activities by natural and synthetic phenolic compounds. Xenobiotica 1998, 28, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Huynh, H.T.; Teel, R.W. Effects of plant-derived phenols on rat liver cytochrome P450 2B1 activity. Anticancer Res. 2002, 22, 1699–1703. [Google Scholar] [PubMed]
- Nagao, T.; Komine, Y.; Soga, S.; Meguro, S.; Hase, T.; Tanaka, Y.; Tokimitsu, I. Ingestion of a tea rich in catechins leads to a reduction in body fat and malondialdehyde-modified LDL in men. Am. J. Clin. Nutr. 2005, 81, 122–129. [Google Scholar] [PubMed]
- Kannan, R.R.R.; Arumugam, R.; Thangaradjou, T.; Anantharaman, P. Phytochemical constituents, antioxidant properties and p-coumaric acid analysis in some seagrasses. Food Res. Int. 2013, 54, 1229–1236. [Google Scholar] [CrossRef]
- Farag, M.A.; Wessjohann, L.A. Metabolome classification of commercial Hypericum perforatum (St. John’s Wort) preparations via UPLC-qTOF-MS and chemometrics. Planta Med. 2012, 78, 488–496. [Google Scholar] [CrossRef] [PubMed]
- Berry, L.M.; Zhao, Z.; Lin, M.J. Dynamic Modeling of Cytochrome P450 Inhibition in vitro: Impact of Inhibitor Depletion on IC50 Shifts. Drug Metab. Dispos. 2013, 41, 1433–1441. [Google Scholar] [CrossRef] [PubMed]
- Awortwe, C.; Bouic, P.J.; Masimirembwa, C.M.; Rosenkranz, B. Inhibition of Major Drug Metabolizing CYPs by Common Herbal Medicines used by HIV/AIDS Patients in Africa—Implications for Herb-Drug Interactions. Drug Metab. Lett. 2013, 7, 83–95. [Google Scholar] [CrossRef]
- Sample Availability: Not available.
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomford, N.E.; Awortwe, C.; Dzobo, K.; Adu, F.; Chopera, D.; Wonkam, A.; Skelton, M.; Blackhurst, D.; Dandara, C. Inhibition of CYP2B6 by Medicinal Plant Extracts: Implication for Use of Efavirenz and Nevirapine-Based Highly Active Anti-Retroviral Therapy (HAART) in Resource-Limited Settings. Molecules 2016, 21, 211. https://doi.org/10.3390/molecules21020211
Thomford NE, Awortwe C, Dzobo K, Adu F, Chopera D, Wonkam A, Skelton M, Blackhurst D, Dandara C. Inhibition of CYP2B6 by Medicinal Plant Extracts: Implication for Use of Efavirenz and Nevirapine-Based Highly Active Anti-Retroviral Therapy (HAART) in Resource-Limited Settings. Molecules. 2016; 21(2):211. https://doi.org/10.3390/molecules21020211
Chicago/Turabian StyleThomford, Nicholas E., Charles Awortwe, Kevin Dzobo, Faustina Adu, Denis Chopera, Ambroise Wonkam, Michelle Skelton, Dee Blackhurst, and Collet Dandara. 2016. "Inhibition of CYP2B6 by Medicinal Plant Extracts: Implication for Use of Efavirenz and Nevirapine-Based Highly Active Anti-Retroviral Therapy (HAART) in Resource-Limited Settings" Molecules 21, no. 2: 211. https://doi.org/10.3390/molecules21020211








