An Assessment of the Food and Nutrition Security Status of Weaned 7–12 Months Old Children in Rural and Peri-Urban Communities of Gauteng and Limpopo Provinces, South Africa
Abstract
:1. Introduction
2. Methodology
2.1. Research Technique and Sampling Technique
2.2. Description of Study Areas and Gaining Entry to the Communities
2.3. Data Collection Procedure
2.3.1. Survey
Section 1: Demographic Data
Section 2: Food Security Assessment
Section 3: Nutritional Status Assessment
2.3.2. Focus Group Discussions
2.4. Data Analysis
2.5. Ethical Approval
3. Results
3.1. Demographic Profile of Caregivers and Their Children
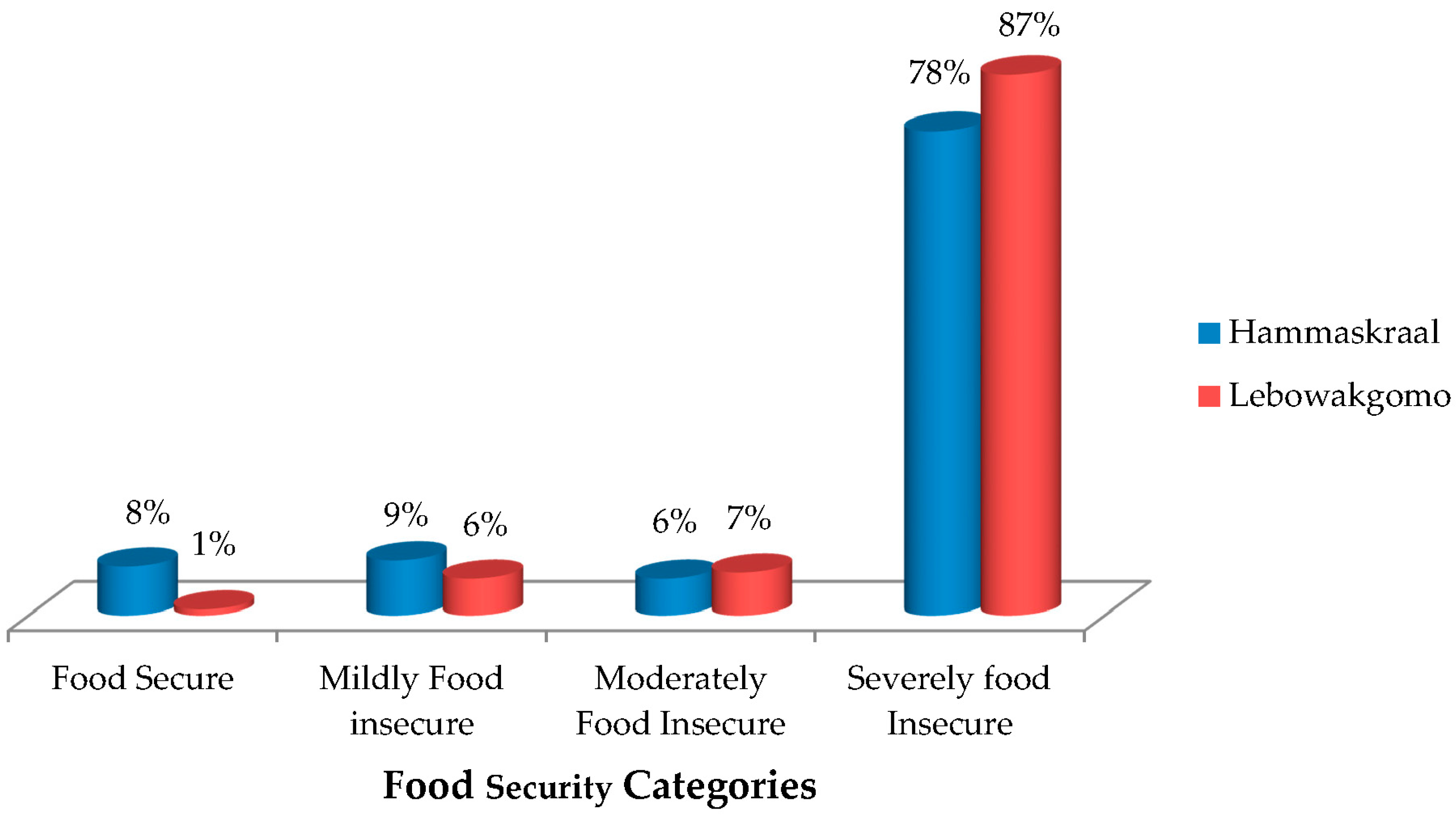
3.2. Children’s Food Insecurity Access-Related Conditions, Domains and Prevalence
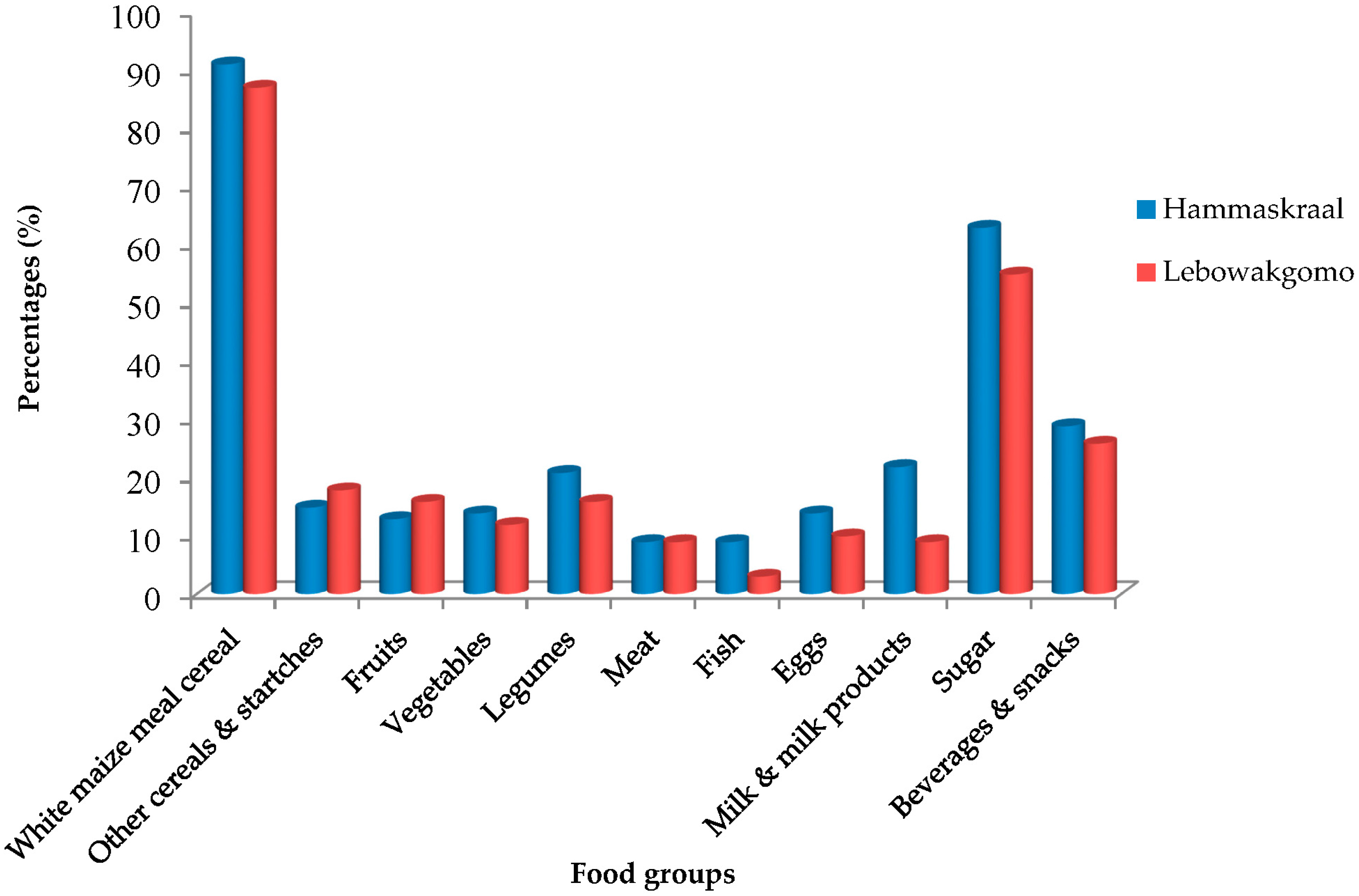
3.3. Food Consumption Frequency, Individual Diet Diversity Score (IDDS), and Weight-for-Age (WAZ) as Measures of Nutritional Quality of Children’s Diet and Nutritional Status of the Children
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Food and Agricultural Organization (FAO). The State of Food Insecurity in the World 2008; Food and Agricultural Organization: Rome, Italy, 2008. [Google Scholar]
- United Nations Children’s Fund (UNICEF). A UNICEF Policy Review: Strategy for Improved Nutrition of Children and Women in Developing Countries; United Nations Children’s Fund: New York, NY, USA, 1990. [Google Scholar]
- Aggarwal, A.; Verma, S.; Faridi, M.M.A. Complementary feeding-reasons for inappropriateness of timing, quantity and consistency. Indian J. Pediatr. 2008, 75, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Kuriyan, R.; Kupad, A.V. Complementary feeding patterns in India. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 799–805. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Complementary Feeding. Available online: http://www.who.int/nutrition/topics/complementary_feeding/en/ (accessed on 30 August 2017).
- The Constitution of the Republic of South Africa. Chapter 2: The Bill of Rights. Available online: http://www.sahistory.org.za/archive/chapter-2-bill-rights (accessed on 30 August 2017).
- Tshabalala, Z.P. An Assessment of the Impact of Food Access on Children on the Nutrition Supplementation Programme to Combat Protein-Energy Malnutrition. Master’s Thesis, University of KwaZulu-Natal, Pietermaritzburg, South Africa, 2014. [Google Scholar]
- World Health Organization (WHO). Global Database on Child Growth and Malnutrtion. Available online: http://www.who.int/nutgrowthdb/en/ (accessed on 30 August 2017).
- Lutter, C.K.; Duelmans, B.M.E.G.; De Onis, M.; Kothari, M.T.; Ruel, M.T.; Arimond, M.; Deltchler, M.; Blossener, M.; Borghi, E. Undernutrition, poor feeding practices & low coverage of key nutrition intervention. Pediatrics 2011, 126, 1418–1427. [Google Scholar]
- United Nations Children’s Fund. Key Facts and Figures on Nutrition. Available online: https://www.unicef.org/media/files/UNICEF_Key_facts_and_figures_on_Nutrition.docx (accessed on 30 August 2017).
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. South African National Health and Nutrition Examination Survey (SANHANES-1), 2014 Edition ed; HSRC Press: Cape Town, South Africa, 2014. [Google Scholar]
- Department of Health (DoH); United Nations Childre’s Fund (UNICEF). A Reflection of the South African Maize Meal and Wheat Flour Fortification Programme (2004 to 2007). Available online: https://www.unicef.org/southafrica/resources_7988.html (accessed on 30 August 2017).
- Willey, B.A.; Cameron, N.; Norris, S.A.; Pettifor, J.M.; Griffiths, P.L. Socio-economic predictors of stunting in preschool children—A population-based study from Johannesburg and Soweto. S. Afr. Med. J. 2009, 99, 450–456. [Google Scholar] [PubMed]
- Symington, E.A.; Gericke, G.J.; Nel, J.H.; Labadarios, D. The relationship between stunting and overweight among children from South Africa: Secondary analysis of the National Food Consumption Survey—Fortification Baseline I. S. Afr. Med. J. 2015, 106, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Mushaphi, L.F.; Mbhenyane, X.G.; Khoza, L.B.; Amey, A.K. Infant-feeding practices of mothers and the nutritional status of infants in the Vhembe District of Limpopo Province. S. Afr. J. Clin. Nutr. 2008, 21, 36–41. [Google Scholar] [CrossRef]
- Motadi, S.A.; Mbhenyane, X.G.; Mbhatsani, H.V.; Mabapa, N.S.; Mamabolo, R.L. Prevalence of iron and zinc deficiencies among preschool children ages 3 to 5 y in Vhembe district, Limpopo province, South Africa. Nutrition 2015, 31, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Teddlie, C.; Tashokkori, A. Foundations of Mixed Methods Research: Integrating Quantitative and Qualitative Approaches in the Social and Behavioural Sciences; Sage: London, UK, 2009. [Google Scholar]
- Cochran, W. Sampling Techniques; Wiley: Hoboken, NJ, USA, 2007. [Google Scholar]
- Teddlie, C.; Yu, F. Mixed methods sampling: A typology with example. J. Mixed Methods Res. 2007, 1, 77–100. [Google Scholar] [CrossRef]
- IDP. Region 2: Regional Integrated Development Plan 2014–2016; City of Tshwane Metropolitan Municipality: Pretoria, South Africa, 2014. [Google Scholar]
- IDP. Lepelle-Nkumpi Municipality: 2015–2016 Integrated Development Plan; Lepelle-Nkumpi Municipality: Polokwane, South Africa, 2015. [Google Scholar]
- Coates, J.; Anne, S.; Paula, B. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide; Academy for Educational Development: Washington, DC, USA, 2007. [Google Scholar]
- Faber, M.; Benade, A.J.S. Breastfeeding, complementary feeding and nutritional status of 6–12-month-old infants in rural KwaZulu-Natal. S. Afr. J. Clin. Nutr. 2007, 20, 16–24. [Google Scholar]
- Chingondole, S.M. Investigation of the Socio-Economic Impact of Morbidity and Mortality on Women’s Household Behaviours among Community Garden Clubs in Maphephetheni, KwaZulu-Natal. Ph.D. Thesis, University of KwaZulu-Natal, Pietermaritzburg, South Africa, 2006. [Google Scholar]
- Kruger, R.; Gericke, G.J. A qualitative exploration of rural feeding and weaning practices, knowledge and attitudes on nutrition. Public Health Nutr. 2003, 6, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Goosen, C.; McLachlan, M.H.; Schubl, C. Infant feeding practices during the first 6 months of life in a low-income area of the Western Cape Province. S. Afr. J. Clin. Health 2014, 8, 50–54. [Google Scholar] [CrossRef]
- Raboy, V. The ABCs of low-phytate crops. Nat. Biotechnol. 2007, 25, 874–875. [Google Scholar] [CrossRef] [PubMed]
- Duvenage, S.S.; Schönfeldt, H.C. Impact of South African fortification legislation on product formulation for low-income households. J. Food Comp. Anal. 2007, 20, 688–695. [Google Scholar] [CrossRef]
- Van-Duyn, M.A.; Pivonka, E. Overview of the health benefits of fruit and vegetable consumption for the dietetics professional: Selected literature. J. Am. Diet. Assoc. 2000, 100, 1511–1521. [Google Scholar] [CrossRef]
- Child Health Study Group. Infant feeding recommendation. Chin. J. Pediatr. 2009, 47, 504–507. [Google Scholar]
- World Health Organization (WHO). Global Strategy for Infant and Young Child Feeding; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Pan American Health Organization (PAHO); World Health Organization (WHO). Guiding Principles for Complementary Feeding of the Breastfed Child; PAHO and WHO: Washington, DC, USA, 2003. [Google Scholar]
| Variables | Hammanskraal | Lebowakgomo |
|---|---|---|
| Age of Children | ||
| 7–8 months | 50.0 | 75.5 |
| 9–10 months | 30.2 | 15.1 |
| 11–12 months | 19.8 | 9.4 |
| Gender of children | ||
| Female | 58.5 | 47.2 |
| Male | 41.5 | 52.8 |
| Age of mothers | ||
| 17–25 years | 66 | 19.8 |
| 26–35 years | 26.4 | 73.6 |
| 36–45 years | 4.7 | 6.6 |
| 46–55 years | 2.8 | 0 |
| Marital status | ||
| Single | 88.7 | 90.6 |
| Married | 11.3 | 6.6 |
| Widowed | 0 | 2.8 |
| Divorced | 0 | 0 |
| Level of education | ||
| No formal education | 3.8 | 26.4 |
| Primary | 8.5 | 21.7 |
| Secondary | 78.3 | 45.4 |
| Tertiary | 9.4 | 6.6 |
| Employment status | ||
| Employed full time | 0.9 | 2.8 |
| Employed part-time | 7.5 | 4.7 |
| Unemployed | 91.5 | 92.5 |
| Household income per month | ||
| Below R800 | 78.3 | 81.1 |
| R801–R1500 | 14.2 | 15.1 |
| R1501–R3500 | 3.8 | 1.9 |
| Above R3500 | 3.8 | 1.9 |
| Vegetable garden | ||
| Yes | 2.8 | 57.5 |
| No | 97.2 | 42.5 |
| Fruit production | ||
| Yes | 31.1 | 63.2 |
| No | 68.9 | 36.8 |
| Livestock | ||
| Yes | 3.8 | 48.5 |
| No | 96.2 | 51.5 |
| Nutrition education | ||
| Radio | 5.7 | 7.1 |
| TV | 10.4 | 2.9 |
| Public health facilities | 47.2 | 65.7 |
| Adult in household | 8.5 | 22.9 |
| None | 28.2 | 1.4 |
| Food Items | Most Days | Once a Week | Seldom | Never |
|---|---|---|---|---|
| Cereals/Starches | ||||
| Bread | 23.6 a (5.7) b | 7.5 (2.8) | 10.4 (6.6) | 57.5 (84.9) |
| Maize meal porridge-Soft | 86.8 (88.7) | 4.7 (4.7) | 3.8 (4.7) | 3.8 (1.9) |
| Maize meal porridge-Stiff | 25.5 (25.5) | 8.5 (11.3) | 17.9 (21.7) | 47.2 (41.5) |
| Maize meal porridge-Fermented | 17.0 (29.2) | 10.4 (12.3) | 9.4 (17.9) | 62.3 (40.6) |
| Cooked porridge other than maize meal | 34.0 (45.3) | 10.4 (8.5) | 5.7 (10.4) | 49.1 (35.8) |
| Infant Cereal | 29.2 (4.7) | 11.3 (0) | 7.5 (6.6) | 50.9 (88.7) |
| Rice | 14.2 (0) | 16 (0) | 3.8 (0) | 65.1(0) |
| Potato | 41.5 (13.2) | 17.9 (41.5) | 6.6 (8.5) | 33 (36.8) |
| Dairy products | ||||
| Fresh milk | 16 (0) | 8.5 (0) | 8.5 (3.8) | 66 (96.2) |
| Milk powder | 32.1 (15.1) | 11.3 (8.5) | 5.7 (11.3) | 50 (65.1) |
| Yoghurt | 26.4 (0) | 11.3 (0) | 19.8 (15.1) | 41.5 (84.9) |
| Animal foods | ||||
| Red Meat | 1.9 (6.6) | 11.3 (0) | 1.9 (2.8) | 84 (90.6) |
| Chicken | 11.3 (2.8) | 6.6 (0) | 0.9 (3.8) | 80.2 (93.4) |
| Fish | 8.5 (0) | 7.5 (0.9) | 6.6 (6.6) | 76.4 (92.5) |
| Eggs | 21.7 (11.3) | 2.8 (7.5) | 9.4 (0.9) | 65.1 (80.2) |
| Legumes | ||||
| Beans | 1.9 (8.5) | 8.5 ( 6.6) | 8.5 (17.0) | 80.2 (67.9) |
| Peanut butter | 41.5 (17.0) | 10.4 (1.9) | 10.4 (13.3) | 36.8 (68.9) |
| Vegetables | ||||
| Butternut | 21.7 (11.3) | 15.1 (6.6) | 16 (16.0) | 46.2 (66.0) |
| Carrots | 17 (3.8) | 9.4 (2.8) | 6.6 (6.6) | 66.0 (86.8) |
| Dark-green leafy vegetables | 6.6 (27.4) | 7.5 (9.4) | 5.7 (16.0) | 79.2 (47.2) |
| Cabbage | 8.5 (12.3) | 12.3 (5.7) | 2.8 (7.5) | 75.5 (74.5) |
| Tomato | 16 (31.1) | 2.8 (9.4) | 2.8 (10.4) | 77.4 (62.3) |
| Fruits | ||||
| Apple | 12.3 (6.6) | 8.5 (0) | 6.6 (13.2) | 71.7 (80.2) |
| Banana | 16.0 (31.1) | 4.7 (9.4) | 12.3 (17.9) | 66 (41.5) |
| Orange | 17.9 (22.6) | 9.4 (10.4) | 9.4 (12.3) | 62.3 (54.7) |
| Miscellaneous | ||||
| Sugar | 54.7 (39.6) | 18.9 (17.9) | 6.6 (10.4) | 18.9 (32.1) |
| Biscuits | 24.5 (16) | 11.3 (12.3) | 22.6 (18.9) | 40.6 (52.8) |
| Sweets | 20.8 (22.6) | 12.3 (11.3) | 21.7 (16.0) | 44.3 (50.0) |
| Savoury snacks | 13.2 (14.2) | 21.7 (16.0) | 19.8 (14.2) | 45.3 (55.7) |
| Carbonated drinks | 11.3 (0.9) | 10.4 (0) | 16.0 (22.6) | 61.3 (76.4) |
| Concentrated Juice | 67.9 (58.0) | 12.3 (12.3) | 5.7 (10.4) | 13.2 (22.6) |
| Tea | 67 (54.7) | 5.7 (6.6) | 7.5 (14.2) | 18.9 (24.5) |
| Coffee | 3.8 (0.9) | 1.9 (1.9) | 1.9 (97.2) | 91.5 (97.2) |
| Age Groups (Months) | n | Severely Underweight (<−3SD)% | Underweight (<−2SD)% | WAZ (SD) |
|---|---|---|---|---|
| 7–8 | 53 a; 80 b | 13.2; 22.5 | 34.0; 38.8 | −1.04 (1.81); −1.12 (2.32) |
| 9–10 | 32; 16 | 31.3; 31.6 | 34.4; 43.8 | −0.95 (2.35); −1.99 (2.09) |
| 11–12 | 21; 10 | 9.5; 20.0 | 19.0; 30.0 | −0.95 (1.14); −1.09 (1.99) |
| 7–12 | 106; 106 | 17.9; 23.6 | 31.1; 38.7 | −0.99 (1.9); −1.25 (2.26) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ntila, S.; Siwela, M.; Kolanisi, U.; Abdelgadir, H.; Ndhlala, A. An Assessment of the Food and Nutrition Security Status of Weaned 7–12 Months Old Children in Rural and Peri-Urban Communities of Gauteng and Limpopo Provinces, South Africa. Int. J. Environ. Res. Public Health 2017, 14, 1004. https://doi.org/10.3390/ijerph14091004
Ntila S, Siwela M, Kolanisi U, Abdelgadir H, Ndhlala A. An Assessment of the Food and Nutrition Security Status of Weaned 7–12 Months Old Children in Rural and Peri-Urban Communities of Gauteng and Limpopo Provinces, South Africa. International Journal of Environmental Research and Public Health. 2017; 14(9):1004. https://doi.org/10.3390/ijerph14091004
Chicago/Turabian StyleNtila, Sithandiwe, Muthulisi Siwela, Unathi Kolanisi, Hafiz Abdelgadir, and Ashwell Ndhlala. 2017. "An Assessment of the Food and Nutrition Security Status of Weaned 7–12 Months Old Children in Rural and Peri-Urban Communities of Gauteng and Limpopo Provinces, South Africa" International Journal of Environmental Research and Public Health 14, no. 9: 1004. https://doi.org/10.3390/ijerph14091004
APA StyleNtila, S., Siwela, M., Kolanisi, U., Abdelgadir, H., & Ndhlala, A. (2017). An Assessment of the Food and Nutrition Security Status of Weaned 7–12 Months Old Children in Rural and Peri-Urban Communities of Gauteng and Limpopo Provinces, South Africa. International Journal of Environmental Research and Public Health, 14(9), 1004. https://doi.org/10.3390/ijerph14091004





