Journal Description
Diseases
Diseases
is an international, peer-reviewed, open access, multidisciplinary journal which focuses on the latest and outstanding research on diseases and conditions published monthly online by MDPI. The first issue is released in 2013.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, ESCI (Web of Science), PubMed, PMC, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q2 (Medicine, Research and Experimental)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.4 days after submission; acceptance to publication is undertaken in 2.7 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
- Sections: published in 8 topical sections.
Impact Factor:
2.9 (2023)
Latest Articles
Efficacy and Safety of Adding Ribavirin to Sofosbuvir-Based Direct-Acting Antivirals (DAAs) in Re-Treating Non-Genotype 1 Hepatitis C—A Systematic Review and Meta-Analysis
Diseases 2025, 13(5), 138; https://doi.org/10.3390/diseases13050138 - 29 Apr 2025
Abstract
Background: There is still debate whether ribavirin should be added to direct-acting antivirals (DAAs) for the management of treatment-experienced individuals with non-genotype-1 hepatitis C. This study compared the efficacy and safety of adding ribavirin to sofosbuvir-based combinations compared to sofosbuvir-based regimens alone in
[...] Read more.
Background: There is still debate whether ribavirin should be added to direct-acting antivirals (DAAs) for the management of treatment-experienced individuals with non-genotype-1 hepatitis C. This study compared the efficacy and safety of adding ribavirin to sofosbuvir-based combinations compared to sofosbuvir-based regimens alone in treating non-genotype 1 hepatitis C virus (HCV) in individuals who have been previously treated. Methods: We searched Cochrane CENTRAL, PubMed, SCOPUS, CINAHL and preprint databases from inception to September 2023 for randomized controlled trials (RCTs) that compared sofosbuvir-based regimens with ribavirin to sofosbuvir-based regimens alone in previously treated individuals with non-genotype 1 HCV infection. Data extraction and quality of study assessments were performed by two independent authors, and synthesis was performed using bias-adjusted models, heterogeneity using I2, and publication bias using funnel plots. Results: Eight RCTs compared sofosbuvir-based combinations with and without ribavirin were included. Overall, the addition of ribavirin to sofosbuvir, compared to sofosbuvir alone, did not show a benefit in achieving sustained virological response (SVR) (OR 0.91, 95% CI 0.26–3.17, I2 = 70.0%) with moderate certainty in Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) evidence. In subgroup analysis, there was no benefit of adding ribavirin to sofosbuvir in individuals with non-genotype 1 HCV. The additional ribavirin was associated with increased adverse events (OR 2.03, 95% CI 1.58–2.6, I2 = 8.0%) and treatment discontinuation (OR 1.81, 95% CI 0.78–4.28, I2 = 0.0%). Conclusions: The moderate certainty evidence suggests that adding ribavirin to sofosbuvir-based regimens may not confer benefit in achieving SVR in previously treated individuals with non-genotype 1 HCV but increases the odds of adverse events and treatment discontinuation. More evidence is needed on the effect of additional ribavirin in achieving SVR in individuals with decompensated cirrhosis. Registration: The protocol is registered on the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42022368868).
Full article
(This article belongs to the Special Issue Viral Hepatitis: Diagnosis, Treatment and Management)
►
Show Figures
Open AccessArticle
Unmasking the Hidden Morbidity of Ocular Diseases in Primary Care Through a Collaboration with Specialists in Remote Areas: A Cross-Sectional Study from Rural Crete, Greece
by
Konstantinos Chliveros, Manolis Linardakis, Ioanna Tsiligianni, Miltiadis Tsilimbaris, Ioannis Pallikaris and Christos Lionis
Diseases 2025, 13(5), 137; https://doi.org/10.3390/diseases13050137 - 29 Apr 2025
Abstract
►▼
Show Figures
Background: Ocular disorders are not frequently addressed in primary care, which is more visible in remote rural settings. The aim of the study was to assess the prevalence and pattern of eye diseases in a remote rural population of Crete and to
[...] Read more.
Background: Ocular disorders are not frequently addressed in primary care, which is more visible in remote rural settings. The aim of the study was to assess the prevalence and pattern of eye diseases in a remote rural population of Crete and to explore whether they represent a hidden morbidity. Materials and Methods: A community-based, cross-sectional study based on data collected through a comprehensive clinical investigation conducted by a mobile ophthalmological unit. Permanent inhabitants, aged over 40 years, living in one remote rural community located on the highest mountain of Crete, were invited to participate. The prevalence of eye diseases was measured during the comprehensive ophthalmological examination. Patients’ medical records were used to assess hidden morbidity. The National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25) was applied to measure self-reported vision-targeted health status. Results: A total of 239 individuals agreed to participate; 54.9% were females (n = 151), with a mean ageof 66.13 years (±14.56). The most common diagnoses were refractory errors (59%), cataract (21.7%), glaucoma (11.7%), maculopathy (8.8%), and dry eyes (8.8%). A previously undiagnosed eye disorder was detected in 34.3% (n = 82). Total scores of NEI VFQ-25 measured quality of life were highand significantly lower in Known Cases of eye diseases compared to patients with New or Without diagnosis (76.6 vs. 84.1 and 84.6, respectively, p = 0.009). Conclusions: Our study highlighted the need for increased awareness of primary care in rural areas concerning eye disorders. Local policies should focus on implementing public health interventions and encouraging close cooperation with specialists to overcome accessibility issues.
Full article
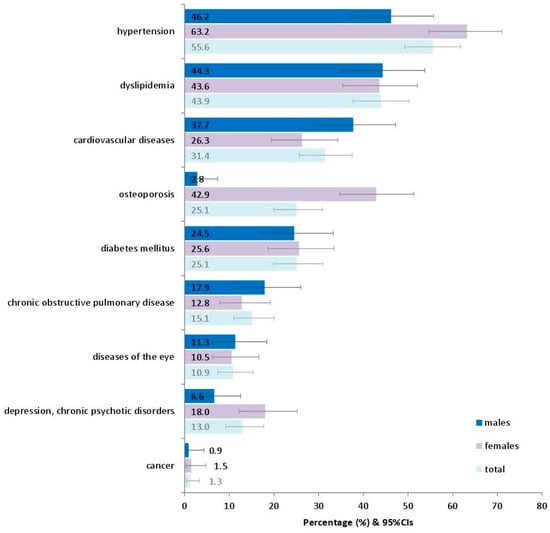
Figure 1
Open AccessSystematic Review
Cardiac Repair and Clinical Outcomes of Stem Cell Therapy in Heart Failure: A Systematic Review and Meta-Analysis
by
Salman Muslem, Mariam AlTurani, Muhammad Bilal Maqsood and Maryam Al Qaseer
Diseases 2025, 13(5), 136; https://doi.org/10.3390/diseases13050136 - 29 Apr 2025
Abstract
Background: While heart failure with reduced ejection fraction (HFrEF) remains a major global health burden, mesenchymal stem cell (MSC) therapy has emerged as a promising intervention designed to improve cardiac function and reduce morbidity among patients unresponsive to conventional treatments. MSC therapy has
[...] Read more.
Background: While heart failure with reduced ejection fraction (HFrEF) remains a major global health burden, mesenchymal stem cell (MSC) therapy has emerged as a promising intervention designed to improve cardiac function and reduce morbidity among patients unresponsive to conventional treatments. MSC therapy has shown promise by targeting left ventricular pressure and improving wall thickness, contributing to reductions in HF-related morbidity and mortality rates. This systematic review and meta-analysis bridges a gap in current research through a focused examination of the most recent clinical trials to cohesively assess MSC therapy in HFrEF patients. Methods: We conducted a systematic review and meta-analysis of clinical trials published from 2018 onwards, which were obtained from multiple databases such as PUBMED, Scopus, EBSCO Medline, EBSCO CINAHL Science Direct, and the Cochrane Library. This review investigates the efficacy and safety outcomes of MSC therapy in patients above 18 years of age with a known diagnosis of heart failure with a reduced ejection fraction (HFrEF). The primary outcome was the change in the left ventricular ejection fraction (LVEF). Secondary outcomes encompassed several efficacy outcomes, such as Global Circumferential strain (GCS), the 6-Minute Walk Test (6MWT), Quality of Life (QoL), and major adverse cardiac events (MACE). A PRISMA flow diagram was constructed to illustrate the identification, screening, eligibility, and inclusion of studies at each stage of the review process. Results: A total of 330 studies were initially identified, but only 12 met the inclusion criteria. MSC therapy resulted in a small, non-significant improvement in LVEF (Hedges’ g = 0.096, p = 0.18) with low heterogeneity (I² = 0.5%). Only QoL showed significant improvement (Hedges’ g = −0.518, p = 0.01). No significant changes in other efficacy outcomes were observed. The therapy was not associated with an increased risk of MACE. Conclusion: While MSC therapy was safe and improved QoL for HFrEF patients, it did not significantly improve LVEF or other efficacy outcomes. Further large-scale, standardized trials are required to better understand the potential role of MSCs in heart failure (HF) therapy.
Full article
(This article belongs to the Section Cardiology)
►▼
Show Figures
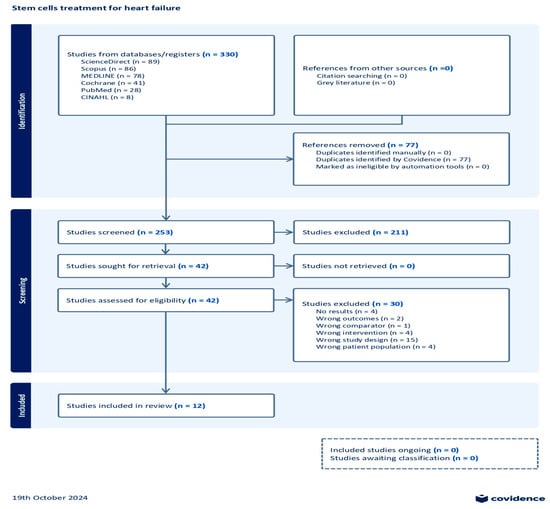
Figure 1
Open AccessArticle
Minimally Invasive Versus Full Sternotomy Approaches in Mitral Valve Surgery for Infective Endocarditis: A Retrospective Comparative Analysis
by
Elisa Mikus, Mariafrancesca Fiorentino, Diego Sangiorgi, Antonino Costantino, Simone Calvi, Elena Tenti, Elena Tremoli, Alberto Tripodi and Carlo Savini
Diseases 2025, 13(5), 135; https://doi.org/10.3390/diseases13050135 - 28 Apr 2025
Abstract
►▼
Show Figures
Background: This study evaluates the outcomes of isolated mitral valve surgery for infective endocarditis performed via conventional full sternotomy or minimally invasive right minithoracotomy. While minimally invasive surgery (MIS) is well-established for elective mitral procedures, its role in infective endocarditis remains less explored
[...] Read more.
Background: This study evaluates the outcomes of isolated mitral valve surgery for infective endocarditis performed via conventional full sternotomy or minimally invasive right minithoracotomy. While minimally invasive surgery (MIS) is well-established for elective mitral procedures, its role in infective endocarditis remains less explored due to the complexity of the disease. Methods: A retrospective analysis of 134 patients who underwent isolated mitral valve surgery for infective endocarditis between January 2010 and March 2024 was conducted. Patients were divided into two groups based on the surgical approach: full sternotomy (n = 94) and MIS via right minithoracotomy (n = 40). Variables analyzed included preoperative characteristics, intraoperative details, and postoperative outcomes, such as mortality, complications, and hospital stay duration. Given significant baseline differences, inverse probability weighting was applied for comparability. Results: Mitral valve replacement was performed in 77% of cases. After adjustment, the MIS group demonstrated shorter intensive care unit stays (p = 0.018), with no significant differences in in-hospital mortality (p = 0.145) or total hospitalization length (p = 0.151). Conclusions: Minimally invasive mitral valve surgery is a safe and effective alternative to sternotomy in infective endocarditis, offering comparable outcomes with shorter ICU stays. Further research is needed to refine patient selection and validate these findings.
Full article
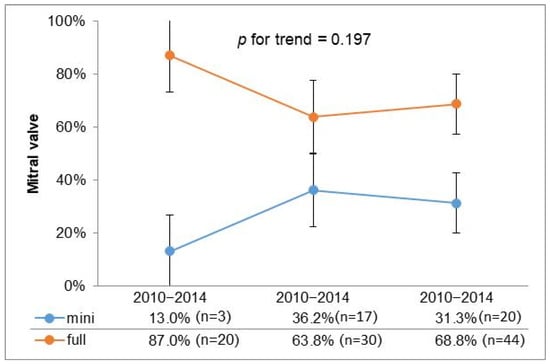
Figure 1
Open AccessReview
Sarcopenia in Rheumatic Diseases: A Hidden Issue of Concern
by
Eleni C. Pardali, Markos Klonizakis, Dimitrios G. Goulis, Sousana K. Papadopoulou, Christos Cholevas, Constantinos Giaginis, Christina Tsigalou, Dimitrios P. Bogdanos and Maria G. Grammatikopoulou
Diseases 2025, 13(5), 134; https://doi.org/10.3390/diseases13050134 - 26 Apr 2025
Abstract
►▼
Show Figures
Sarcopenia is characterized by a loss of muscle mass and function, with significant implications for the physical performance of the affected people. Although commonly associated with aging, disease-related sarcopenia is of great clinical importance, particularly as it impacts disease progression and outcomes. Individuals
[...] Read more.
Sarcopenia is characterized by a loss of muscle mass and function, with significant implications for the physical performance of the affected people. Although commonly associated with aging, disease-related sarcopenia is of great clinical importance, particularly as it impacts disease progression and outcomes. Individuals with rheumatic diseases (RDs), including rheumatoid arthritis, systemic sclerosis, spondyloarthritides, systemic lupus erythematosus, fibromyalgia, myositis, or vasculitis, exhibit a high prevalence of sarcopenia, which exacerbates their clinical symptoms and contributes to poorer disease outcomes. Chronic inflammation influences muscle tissue degradation, causing a decline in physical performance. Apart from the apparent clinical manifestations, patients with RDs also use pharmacological treatments that negatively impact muscle mass further, increasing the risk of sarcopenia. Nutrition (diet and dietary supplements) and exercise interventions have been recommended as protective measures for sarcopenia as they may mitigate its adverse events. The present narrative review seeks to explore the methods used to assess sarcopenia in patients with RDs, its prevalence among them, and the challenges faced by the affected individuals, while critically assessing the appropriateness and limitations of current sarcopenia assessment tools in the context of RDs.
Full article
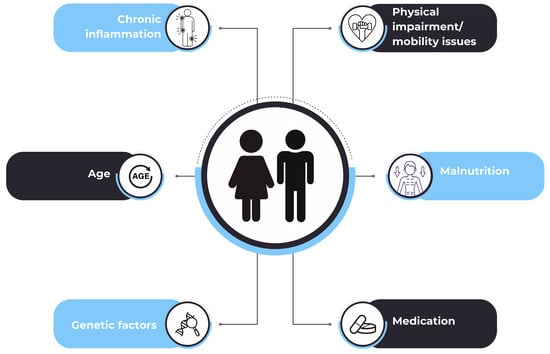
Figure 1
Open AccessCase Report
Clinical Heterogeneity of Early-Onset Autoimmune Gastritis: From the Evidence to a Pediatric Tailored Algorithm
by
Ivan Taietti, Martina Votto, Riccardo Castagnoli, Mirko Bertozzi, Maria De Filippo, Antonio Di Sabatino, Ombretta Luinetti, Alessandro Raffaele, Alessandro Vanoli, Marco Vincenzo Lenti, Gian Luigi Marseglia and Amelia Licari
Diseases 2025, 13(5), 133; https://doi.org/10.3390/diseases13050133 - 25 Apr 2025
Abstract
►▼
Show Figures
Autoimmune gastritis (AIG) is an uncommon and often underestimated condition in children, characterized by chronic stomach inflammation leading to the destruction of oxyntic glands with subsequent atrophic and metaplastic changes. This condition is associated with hypo-/achlorhydria, impairing iron and vitamin B12 absorption. The
[...] Read more.
Autoimmune gastritis (AIG) is an uncommon and often underestimated condition in children, characterized by chronic stomach inflammation leading to the destruction of oxyntic glands with subsequent atrophic and metaplastic changes. This condition is associated with hypo-/achlorhydria, impairing iron and vitamin B12 absorption. The pathogenesis involves the activation of helper type 1 CD4+/CD25-T-cells against parietal cells. Clinical manifestations in children are not specific and include abdominal pain, bloating, nausea, vomiting, and iron deficiency anemia (IDA). The disease is also linked to an increased risk of pernicious anemia, intestinal-type gastric cancer, and type I neuroendocrine tumors. AIG is often diagnosed through the presence of autoantibodies in the serum, such as parietal cell (APCA) and intrinsic factor (IF) antibodies. However, therapeutic recommendations for pediatric AIG are currently lacking. We aim to present two clinical cases of pediatric-onset AIG, highlighting the heterogeneous clinical manifestations and the challenges in diagnosis with the support of an updated literature review. A 9-year-old girl presented with refractory IDA, initial hypogammaglobulinemia, and a 12-year-old boy was initially diagnosed with eosinophilic esophagitis. Both cases underline the importance of considering AIG in children with chronic gastrointestinal symptoms and gastric atrophy. Diagnostic workup, including endoscopy and serological tests, is crucial for accurate identification. A better understanding of this condition is imperative for timely intervention and regular monitoring, given the potential long-term complications, including the risk of malignancy. These cases contribute to expanding the clinical spectrum of pediatric AIG and highlight the necessity for comprehensive evaluation and management in affected children.
Full article

Figure 1
Open AccessArticle
Beneficial Effects of White Grape Pomace in Experimental Dexamethasone-Induced Hypertension
by
Raluca Maria Pop, Paul-Mihai Boarescu, Corina Ioana Bocsan, Mădălina Luciana Gherman, Veronica Sanda Chedea, Elena-Mihaela Jianu, Ștefan Horia Roșian, Ioana Boarescu, Floricuța Ranga, Maria Doinița Muntean, Maria Comșa, Sebastian Armean, Ana Uifălean, Alina Elena Pârvu and Anca Dana Buzoianu
Diseases 2025, 13(5), 132; https://doi.org/10.3390/diseases13050132 - 24 Apr 2025
Abstract
►▼
Show Figures
Background: Grape pomace (GP), a by-product of winemaking, is a rich source of bioactive polyphenols known for their antioxidant and anti-inflammatory properties. While the cardiovascular benefits of red grape pomace have received significant scientific attention, the therapeutic potential of white grape pomace remains
[...] Read more.
Background: Grape pomace (GP), a by-product of winemaking, is a rich source of bioactive polyphenols known for their antioxidant and anti-inflammatory properties. While the cardiovascular benefits of red grape pomace have received significant scientific attention, the therapeutic potential of white grape pomace remains largely unexplored, particularly in glucocorticoid-induced hypertension. Given the rising prevalence of hypertension and the oxidative-inflammatory mechanisms underlying its progression, this study investigates the effects of white GP on blood pressure regulation, oxidative stress, and pro-inflammatory cytokine expression in an experimental model of dexamethasone (DEXA)-induced hypertension (HTN). By focusing on white GP, this research addresses a significant gap in current knowledge and proposes a novel, sustainable approach to managing hypertension through valorising winemaking by-products. Methods: The first concentration used, GP1, was 795 mg polyphenols/kg bw, while the second concentration, GP2, was 397.5 mg polyphenols/kg bw. Results: White GP polyphenols extract in the DEXA_GP1 group had reduced systolic and diastolic blood pressure. The extract with a higher content of polyphenols (GP1) prevented the elevation of serum levels of total oxidative stress (TOS), malondialdehyde (MDA), and oxidative stress index (OSI), while the extract with a lower content of polyphenols (GP2) slightly reduced serum levels of MDA. Both concentrations of GP increased serum levels of NO and Total Thiols, significantly higher (p < 0.05) than in the group treated with lisinopril. The serum levels of tumour necrosis factor-alpha (TNF-α) increased in all groups where HTN was induced. Both doses of GP extract prevented the elevation of TNF-α. Heart tissue levels of the studied cytokines (TNF-α, interleukin (IL)-1β, and IL-6 were not influenced (p > 0.05) by either the HTN induction or the treatment administered. Conclusions: These findings suggest that grape pomace may serve as a promising nutraceutical intervention for hypertension management, particularly in conditions associated with oxidative stress.
Full article

Figure 1
Open AccessArticle
Desmocollin-3 and Bladder Cancer
by
Chandreshwar P. Shukla, Nayan K. Jain, Michael A. O’Donnell, Kapil V. Vachhani, Rashmi Patel, Janki Patel, Rajiv Modi, Arpit Dheeraj, Jee Min Lee, Annah Rolig, Sanjay V. Malhotra and Bakulesh Khamar
Diseases 2025, 13(5), 131; https://doi.org/10.3390/diseases13050131 - 23 Apr 2025
Abstract
►▼
Show Figures
Background: Desmocollin3, a transmembrane protein, is expressed in the basal/suprabasal layer of normal stratified epithelium. DSC3 gene expression is described in muscle-invasive bladder cancer (MIBC). DSC3-protein-expressing recurrent non-muscle-invasive bladder cancer (NMIBC) had a durable response to CADI-03, a DSC3-specific active immunotherapy. Methods: We
[...] Read more.
Background: Desmocollin3, a transmembrane protein, is expressed in the basal/suprabasal layer of normal stratified epithelium. DSC3 gene expression is described in muscle-invasive bladder cancer (MIBC). DSC3-protein-expressing recurrent non-muscle-invasive bladder cancer (NMIBC) had a durable response to CADI-03, a DSC3-specific active immunotherapy. Methods: We evaluated DSC3 protein expression and its correlation with tumor-infiltrating immune cells in bladder cancer. DSC3 gene expression and its correlation with 208 immune encoding genes, treatment outcome, and survival were evaluated using the “ARRAYEXPRESS” and “TCGA” datasets. Immune genes were grouped as tumor-controlling immune genes (TCIGs) and tumor-promoting immune genes (TPIGs) as per their functions. Results & conclusions: NMIBC had higher DSC3 expression compared to MIBC. More immune genes were correlated with DSC3 in MIBC (21) compared to NMIBC (11). Amongst the TCIGs, six in NMIBC and one in MIBC had a negative correlation while two in NMIBC and nine in MIBC had a positive correlation with DSC3. Amongst the TPIGs, nine in NMIBC and five in MIBC had a negative correlation. Seven TPIGs had a positive correlation with DSC3 in MIBC and none in NMIBC. Of the T cell exhaustion markers, none were correlated with DSC3 in MIBC. Among NMIBC, CTLA4 and TIGIT were the only markers of exhaustion that demonstrated a negative correlation with DSC3. DSC3 expression was also higher in p53 mutant compared to wild p53, non-papillary MIBC compared to papillary MIBC, and in basal, squamous molecular subtype compared to luminal MIBC. MIBC with lower DSC3 expression had better outcomes (response, survival) compared to those with higher DSC3 expression.
Full article
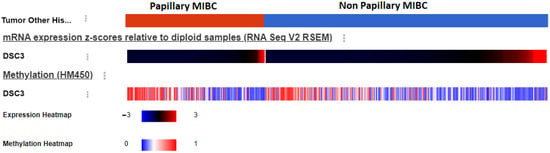
Figure 1
Open AccessArticle
Prevalence of Chronic Obstructive Pulmonary Disease and Asthma in the Community of Pathumthani, Thailand
by
Narongkorn Saiphoklang, Pitchayapa Ruchiwit, Apichart Kanitsap, Pichaya Tantiyavarong, Pasitpon Vatcharavongvan, Srimuang Palungrit, Kanyada Leelasittikul, Apiwat Pugongchai and Orapan Poachanukoon
Diseases 2025, 13(5), 130; https://doi.org/10.3390/diseases13050130 - 23 Apr 2025
Abstract
►▼
Show Figures
Background: Airway diseases, particularly asthma and chronic obstructive pulmonary disease (COPD), pose significant respiratory problems. The prevalence and risk factors of these diseases among community dwellers vary geographically and because of underdiagnosis. This study aims to determine the prevalence and factors associated
[...] Read more.
Background: Airway diseases, particularly asthma and chronic obstructive pulmonary disease (COPD), pose significant respiratory problems. The prevalence and risk factors of these diseases among community dwellers vary geographically and because of underdiagnosis. This study aims to determine the prevalence and factors associated with these diseases in a provincial-metropolitan area in Thailand. Methods: A cross-sectional study was conducted between April 2023 and November 2023 on individuals aged 18 years or older residing in Pathumthani, Thailand. Data on demographics, pre-existing diseases, respiratory symptoms, and pulmonary functions assessed by spirometry, including forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and bronchodilator responsiveness (BDR), were collected. COPD was defined as having respiratory symptoms, a risk factor, and post-bronchodilator FEV1/FVC < 70%. Asthma was defined as having respiratory symptoms and a positive bronchodilator responsiveness. Results: A total of 1014 subjects (71.7% female) were included, with a mean age of 56.6 years. The smoking history was 10.4% (13.4 pack-years). Common symptoms included cough (18.4%), sputum production (14.5%), and dyspnea (10.0%). COPD was found in 8.3%, while asthma was found in 10.3%. Logistic regression analysis indicated that these diseases were significantly associated with older age (odds ratio [OR] 1.023; 95% confidence interval [CI] 1.007–1.039 for every 1-year increase in age), smoking (OR 2.247; 95% CI 1.068–4.728), heart disease (OR 2.709; 95% CI 1.250–5.873), wheezing (OR 3.128; 95% CI 1.109–8.824), runny nose (OR 1.911; 95% CI 1.050–3.477), and previous treatment for dyspnea (OR 6.749, 95% CI 3.670–12.409). Conclusions: COPD and asthma were relatively prevalent in our study. Being elderly, smoking, having heart disease, and experiencing any respiratory symptoms with a history of treatment are crucial indicators for these airway diseases. Pulmonary function testing might be needed for active surveillance to detect these respiratory diseases in the community.
Full article
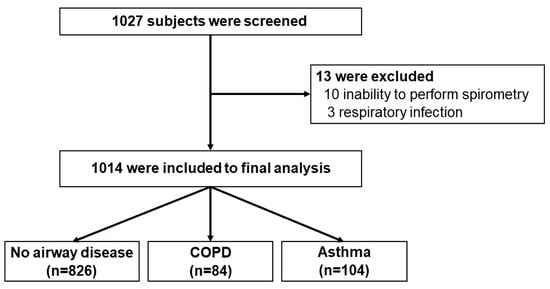
Figure 1
Open AccessReview
Current and Emerging Parenteral and Peroral Medications for Weight Loss: A Narrative Review
by
Abdullah Al Lawati, Ayman Alhabsi, Rhieya Rahul, Maria-Luisa Savino, Hamed Alwahaibi, Srijit Das and Hanan Al Lawati
Diseases 2025, 13(5), 129; https://doi.org/10.3390/diseases13050129 - 22 Apr 2025
Abstract
Obesity is a growing global health challenge, necessitating effective treatment options beyond lifestyle interventions. This narrative review explores established and emerging pharmacotherapies for weight management, including parenteral agents like Liraglutide, Semaglutide, Setmelanotide, and Tirzepatide, as well as peroral medications such as Phentermine, Phentermine/Topiramate,
[...] Read more.
Obesity is a growing global health challenge, necessitating effective treatment options beyond lifestyle interventions. This narrative review explores established and emerging pharmacotherapies for weight management, including parenteral agents like Liraglutide, Semaglutide, Setmelanotide, and Tirzepatide, as well as peroral medications such as Phentermine, Phentermine/Topiramate, Bupropion/Naltrexone, Orlistat, and Metformin. Newer treatments like Cagrilintide and Bimagrumab show promise for enhancing weight loss outcomes. Parenteral GLP-1 receptor agonists demonstrate superior efficacy compared to traditional peroral medications, with gastrointestinal side effects being the most common. Artificial intelligence presents intriguing opportunities to enhance weight loss strategies; however, its integration into clinical practice remains investigational and requires rigorous clinical validation. While current anti-obesity medications deliver significant benefits, future research must determine the efficacy, safety, and cost-effectiveness of AI-driven approaches. This includes exploring how AI can complement combination therapies and tailor personalized interventions, thereby grounding its potential benefits in robust clinical evidence. Future directions will focus on integrating AI into clinical trials to refine and personalize obesity management strategies.
Full article
(This article belongs to the Special Issue Body Composition, Energy Expenditure and Lifestyle During Obesity Management)
►▼
Show Figures
Figure 1
Open AccessArticle
Ultrasound Relationship of Plantar Fat and Predislocation Syndrome
by
Ana María Rayo Pérez, Rafael Rayo Martín, Rafael Rayo Rosado, Joao Miguel Costa Martiniano and Raquel García-de-la-Peña
Diseases 2025, 13(5), 128; https://doi.org/10.3390/diseases13050128 - 22 Apr 2025
Abstract
►▼
Show Figures
Background: Plantar fat plays a crucial role in protecting and cushioning the metatarsals. Its degeneration is a risk factor for the development of metatarsalgia and, consequently, predislocation syndrome. Objectives: To evaluate the relationship between plantar fat thickness and predislocation syndrome in an adult
[...] Read more.
Background: Plantar fat plays a crucial role in protecting and cushioning the metatarsals. Its degeneration is a risk factor for the development of metatarsalgia and, consequently, predislocation syndrome. Objectives: To evaluate the relationship between plantar fat thickness and predislocation syndrome in an adult population, and to determine a possible association between a decrease in forefoot plantar fat and the presence of symptoms. Material and Methods: A retrospective observational study was conducted, including records of patients who visited the podiatry clinic between December 2022 and December 2023. Fifty complete records were selected, divided into two groups, one healthy and one pathological, aged between 18 and 70 years. An ultrasound examination of the plantar area of the second metatarsophalangeal joint was performed to assess the thickness of the fat and plantar plate. Results: The analysis of the 50 records, divided into healthy and pathological groups, reveals significant differences in the thickness of plantar fat and the plantar plate between the two groups. Subjects with predislocation syndrome have a significantly lower plantar fat thickness (0.566 cm) compared to the healthy group (0.941 cm) and also show a greater thickness of the plantar plate (0.359 cm vs. 0.244 cm). Statistical tests confirm these differences with high significance (p < 0.001). The ROC curve shows that plantar fat thickness is a good predictor of predislocation syndrome, with an area under the curve (AUC) of 0.923, emphasizing the utility of this measure in identifying the condition. Conclusions: Preliminary studies suggest that a reduction in plantar fat increases the predisposition to develop predislocation syndrome at the level of the second metatarsophalangeal joint.
Full article
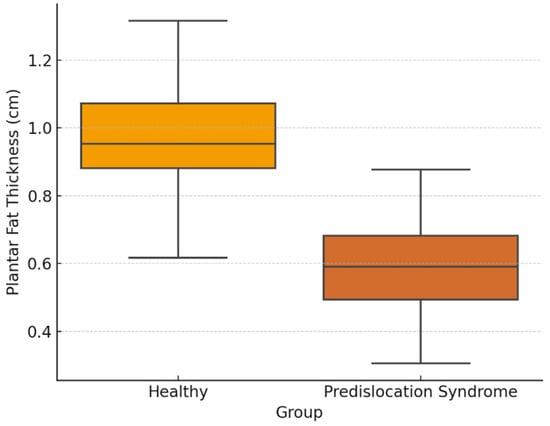
Figure 1
Open AccessSystematic Review
A Closer Look at the Dermatological Profile of GLP-1 Agonists
by
Calista Persson, Allison Eaton and Harvey N. Mayrovitz
Diseases 2025, 13(5), 127; https://doi.org/10.3390/diseases13050127 - 22 Apr 2025
Abstract
►▼
Show Figures
Background/objectives: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are widely used in treating type 2 diabetes and obesity, offering established metabolic and cardiovascular benefits. Emerging evidence suggests these agents also exert direct dermatologic effects. This systematic review categorizes these effects and explores their role in
[...] Read more.
Background/objectives: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are widely used in treating type 2 diabetes and obesity, offering established metabolic and cardiovascular benefits. Emerging evidence suggests these agents also exert direct dermatologic effects. This systematic review categorizes these effects and explores their role in inflammatory skin diseases. Methods: A comprehensive literature search was performed across EMBASE, PubMed, Web of Science, and Google Scholar for studies published from 2014 to 2025. Inclusion criteria were English-language, peer-reviewed original research involving human subjects that linked GLP-1RAs to dermatologic effects. Animal and in vitro studies were excluded. PRISMA guidelines were followed. Results: Fifty-one studies met inclusion criteria. Thirty-four reported adverse effects, including hypersensitivity, injection-site reactions, pruritus, urticaria, angioedema, and immune-mediated conditions like bullous pemphigoid. Seventeen studies described beneficial outcomes, such as improvements in psoriasis, reduced hidradenitis suppurativa flares, enhanced wound healing, anti-aging potential, and decreased inflammation. GLP-1RAs showed cytokine modulation in psoriasis, though their role in hidradenitis suppurativa remains uncertain. Cosmetic concerns, such as “Ozempic Face” due to rapid weight loss, were also noted. Conclusions: GLP-1RAs have a broad spectrum of dermatologic effects, from immunomodulatory benefits to adverse cutaneous reactions. Their impact on inflammatory skin disorders suggests a novel therapeutic avenue. However, adverse reactions and aesthetic changes warrant vigilance. Future research should focus on mechanistic studies, long-term safety, and identifying biomarkers to predict dermatologic responses, ultimately guiding personalized treatment approaches.
Full article
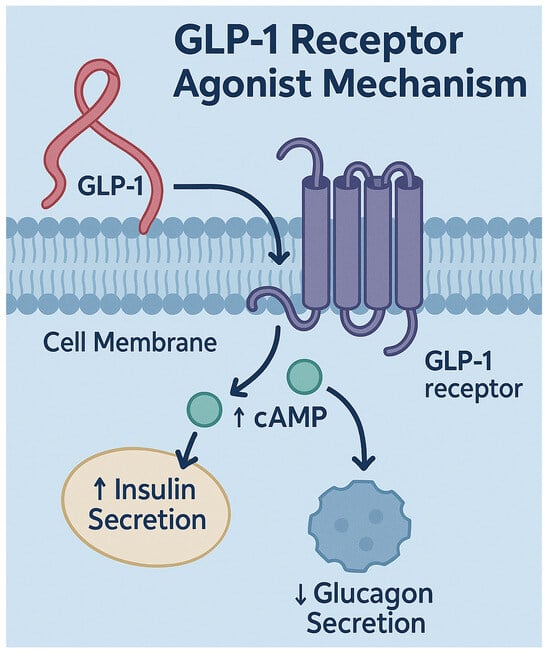
Figure 1
Open AccessArticle
Clinical Importance of B-Type Natriuretic Peptide Levels in Sinus Rhythm at 3 Months After Persistent Atrial Fibrillation Ablation
by
Jumpei Saito, Toshihiko Matsuda, Yui Koyanagi, Katsuya Yoshihiro, Yuma Gibo, Soichiro Usumoto, Wataru Igawa, Toshitaka Okabe, Naoei Isomura and Masahiko Ochiai
Diseases 2025, 13(4), 126; https://doi.org/10.3390/diseases13040126 - 21 Apr 2025
Abstract
►▼
Show Figures
Background: B-type natriuretic peptide (BNP) levels after ablation have been associated with a risk of arrhythmia recurrence (AR) after atrial fibrillation (AF) ablation. In addition, baseline BNP levels were also predictors of AR after AF ablation. However, previous studies have not been clear
[...] Read more.
Background: B-type natriuretic peptide (BNP) levels after ablation have been associated with a risk of arrhythmia recurrence (AR) after atrial fibrillation (AF) ablation. In addition, baseline BNP levels were also predictors of AR after AF ablation. However, previous studies have not been clear about whether sinus rhythm (SR) or AF was present at the time of BNP measurement. In this study, we investigated BNP levels in SR at 1,3 months after persistent AF ablation. Methods: We followed up 178 patients with persistent AF undergoing first-time arrhythmia ablation. BNP levels were measured before 1 and 3 months later after AF ablation in SR. The correlation between AR within 1 year after AF ablation and measured BNP levels was examined. Results: A total of 178 cases (81 males, mean age 69 (60, 74), mean CHA2DS2 Vasc score 2 (0, 4)) with persistent AF were included for ablation. BNP levels before AF ablation were not significantly different between AR and not AR patients. The BNP levels of AR patients were significantly elevated from 1 month to 3 months after the procedure compared with those without (−11.1 pg/mL (−53, 5.7) vs. 17.8 pg/mL (−58.3, 180.5), p < 0.0001). Elevated BNP levels in SR after AF ablation were a significant predictor of AR. Conclusions: Elevated BNP levels in SR 3 months after AF ablation compared with BNP levels 1 month after persistent AF ablation might be a significant prognostic factor in AR.
Full article
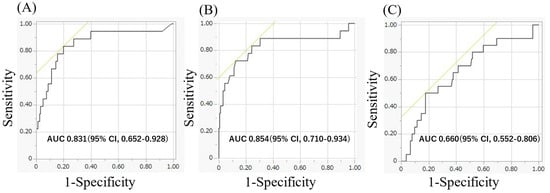
Figure 1
Open AccessCase Report
Patient with Secondary Amyloidosis Due to Crohn’s Disease on Hemodialysis Effectively Treated with Ferric Carboxymaltose Injections: A Case Report and Literature Review
by
Masayo Ueno, Fumihito Hirai, Asami Fuji, Yuko Shimomura, Keiko Uemoto, Kosuke Masutani and Takao Saito
Diseases 2025, 13(4), 125; https://doi.org/10.3390/diseases13040125 - 21 Apr 2025
Abstract
►▼
Show Figures
Background: Almost all patients undergoing dialysis develop renal anemia and receive medicines such as erythropoietin and iron preparations. However, the conventional intravenous treatment with saccharated ferric oxide (SFO) is insufficient for these patients when they have incurable and persistent iron deficiency anemia due
[...] Read more.
Background: Almost all patients undergoing dialysis develop renal anemia and receive medicines such as erythropoietin and iron preparations. However, the conventional intravenous treatment with saccharated ferric oxide (SFO) is insufficient for these patients when they have incurable and persistent iron deficiency anemia due to secondary amyloidosis. Therefore, we administered 500 mg of ferric carboxymaltose (FCM) to such a patient with Crohn’s disease. Case presentation: A 56-year-old man on maintenance hemodialysis had secondary amyloidosis due to Crohn’s disease. Additionally, he was anemic and received 40 mg of SFO weekly; however, his hemoglobin (Hb) level remained low at 7 g/dL. Therefore, 500 mg of FCM was administered bimonthly from the first to the fourth dose, and the Hb level temporarily increased compared to that after the previous SFO administration. Since bimonthly administration did not adequately maintain the Hb level, FCM was administered monthly from the 5th to 12th dose, which stabilized the Hb level at 10–12 g/dL. No side effects, such as hypophosphatemia, were observed. Conclusions: A single dose of 500 mg FCM administered once every 1–2 months stabilizes the Hb level and contributes to efficient iron utilization in patients with incurable anemia undergoing hemodialysis.
Full article
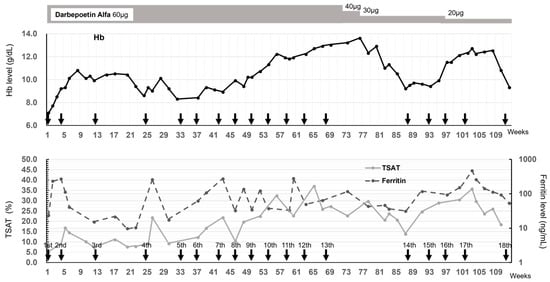
Figure 1
Open AccessSystematic Review
Rabies Vaccination and Public Health Insights in the Extended Arabian Gulf and Saudi Arabia: A Systematic Scoping Review
by
Helal F. Hetta, Khalid S. Albalawi, Amal M. Almalki, Nasser D. Albalawi, Abdulmajeed S. Albalawi, Suleiman M. Al-Atwi, Saleh E. Alatawi, Mousa J. Alharbi, MeshaL F. Albalawi, Ahmad A. Alharbi, Hassabelrasoul Elfadil, Abdullah S. Albalawi and Reem Sayad
Diseases 2025, 13(4), 124; https://doi.org/10.3390/diseases13040124 - 21 Apr 2025
Abstract
Background and Aim: This systematic scoping review examines rabies-related incidents, interventions, and post-exposure immunoprophylaxis in the Arabian Gulf region and Saudi Arabian Peninsula. Methods: A comprehensive literature search was conducted in databases including PubMed, Scopus, WoS, MedLine, and Cochrane Library up to July
[...] Read more.
Background and Aim: This systematic scoping review examines rabies-related incidents, interventions, and post-exposure immunoprophylaxis in the Arabian Gulf region and Saudi Arabian Peninsula. Methods: A comprehensive literature search was conducted in databases including PubMed, Scopus, WoS, MedLine, and Cochrane Library up to July 2024. Studies were included discussing the reported cases of rabies that received the PEP in all countries of the Arabian Gulf, their epidemiological data, the received schedules of vaccination, and their safety. The search was done by using the following terminologies: rabies vaccine, rabies human diploid cell vaccine, vaccine, Saudi Arabia, Bahrain, Iraq, Kuwait, Oman, Qatar, United Arab Emirates, Southwest Asia, Iran, West Asia, Western Asia, Persian Gulf, Arabian Gulf, Gulf of Ajam, Saudi Arabian Peninsula, and The Kingdom of Saudi Arabia. Results: The systematic scoping review included 36 studies, synthesizing findings from diverse research designs, including large-scale cross-sectional studies and case reports, spanning nearly three decades. Findings indicated that young males in urban areas are most at risk for animal bites, predominantly from domestic dogs and cats. While post-exposure prophylaxis (PEP) was generally administered within recommended timeframes, vaccination completion rates varied. Conclusions: The review highlighted gaps in public awareness about rabies risks and prevention. Vaccine safety profiles were generally favorable, with mostly mild-to-moderate side effects reported. The study underscores the need for enhanced public health education, standardized PEP protocols, and a One Health approach to rabies prevention.
Full article
(This article belongs to the Special Issue Infectious Disease Epidemiology 2024)
►▼
Show Figures

Figure 1
Open AccessArticle
Correlation of Inflammatory Biomarkers and IgG4 Antibodies with Malaria in Cameroon’s Buea Municipality Children
by
Jerome Nyhalah Dinga, Flora Ayah, Emmanuel Fondungallah Anu, Haowen Qin, Stanley Dobgima Gamua, Anthony Kukwah Tufon, Magloire Essissima Amougou and Rameshbabu Manyam
Diseases 2025, 13(4), 123; https://doi.org/10.3390/diseases13040123 - 21 Apr 2025
Abstract
►▼
Show Figures
Background: In recent decades, malaria has become a major worldwide public health problem in endemic countries, especially with children below five years. Malaria causes inflammation, and inflammatory biomarkers like α-1-glycoprotein (AGP) and C-reactive protein (CRP) are elevated in serum during malaria. This work
[...] Read more.
Background: In recent decades, malaria has become a major worldwide public health problem in endemic countries, especially with children below five years. Malaria causes inflammation, and inflammatory biomarkers like α-1-glycoprotein (AGP) and C-reactive protein (CRP) are elevated in serum during malaria. This work aimed at assessing the serum levels of AGP (chronic inflammation) and CRP (acute inflammation) biomarkers and IgG4 and their correlation with malaria in children below five years in the Buea Health District of the South West Region of Cameroon. Methods: This cross-sectional study was carried out between February and April, 2024. AGP and CRP were measured using Q-7plex Human Micronutrient Measurement Kit while IgG4 levels were measured using Enzyme-Linked Immunosorbent Assay with 80 samples. Results: Serum AGP and CRP biomarker levels were significantly higher in malaria-positive children compared to malaria-negative children (p < 0.001 and p < 0.001, respectively). IgG4 levels were high in malaria-negative children (mean OD = 0.51) compared to children infected with the malaria parasite (mean OD = 0.29), in a manner that was statistically significant (p < 0.03). Hemoglobin (Hb) had a strong negative correlation with AGP (−0.62) and CRP (−0.46), meaning that as Hb levels increased, AGP and CRP levels decreased. CRP had a strong positive correlation with both age (0.3) and AGP (0.5), suggesting that as age increased or as AGP levels rose, CRP levels tended to increase as well. Conclusions: This study revealed that malaria causes alterations in the serum levels of AGP, CRP, and IgG4 in children below the age of 5 in the Buea municipality of Cameroon. It impacts immune responses by increasing the level of inflammation biomarkers like AGP and CRP and decreasing IgG4, a marker associated with immune regulation. Thus, this study helps the understanding of the inflammatory nature of malaria and could be expanded to aid in the broader public health efforts to control and prevent malaria, reduce its complications, and improve overall health outcomes in children in the Buea municipality.
Full article
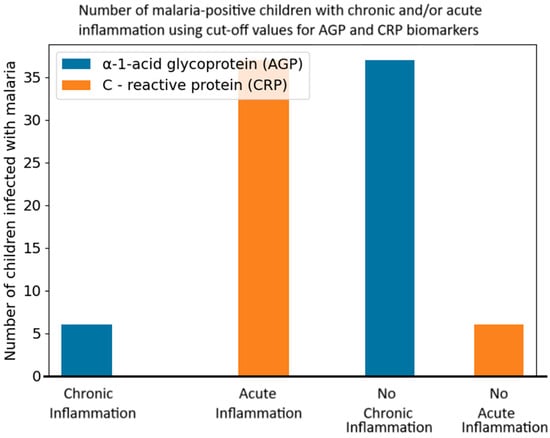
Figure 1
Open AccessArticle
Clinical Trial: Effects of Autologous Dendritic Cell Administration on Renal Hemodynamics and Inflammatory Biomarkers in Diabetic Kidney Disease
by
Endang Drajat, Aziza Ghanie Icksan, Jonny Jonny, Aditya Pratama Lokeswara, Bhimo Aji Hernowo, Elvita Rahmi Daulay and Terawan Agus Putranto
Diseases 2025, 13(4), 122; https://doi.org/10.3390/diseases13040122 - 21 Apr 2025
Abstract
Background: Diabetic kidney disease (DKD) is a significant risk factor for End-Stage Renal Disease, with a high global incidence and mortality rate. Hyperglycemia in DKD induces inflammation, contributing to glomerular hyperfiltration, fibrosis, and impaired renal function. Current therapies, including SGLT2 inhibitors, ACE inhibitors,
[...] Read more.
Background: Diabetic kidney disease (DKD) is a significant risk factor for End-Stage Renal Disease, with a high global incidence and mortality rate. Hyperglycemia in DKD induces inflammation, contributing to glomerular hyperfiltration, fibrosis, and impaired renal function. Current therapies, including SGLT2 inhibitors, ACE inhibitors, and ARBs, show limited efficacy. Autologous dendritic cells (DCs) offer potential anti-inflammatory effects by reducing cytokine activity and fibrosis biomarkers. Methods: A quasi-experimental pretest–post-test design was conducted involving 29 DKD patients. Baseline blood and urine samples were collected for MMP-9, TGF-β, and Doppler ultrasound (PSV, EDV) measurements. The subjects received subcutaneous injections of autologous DCs, and follow-up measurements were conducted four weeks after treatment. The statistical analyses included paired t-tests, Wilcoxon signed-rank tests, and linear regression. Results: After treatment, there were a significant decrease in PSV (from 47.1 ± 23.87 cm/s to 27.85 ± 20.53 cm/s, p = 0.044) and a significant increase in EDV (from 13 ± 5.32 cm/s to 15.7 ± 12.55 cm/s, p = 0.039). A strong correlation was observed between the TGF-β and MMP-9 levels (p = 0.001). Linear regression analysis showed reduced MMP-9 influence on the TGF-β after treatment, suggesting potential fibrosis reduction. Gender and UACR subgroup analyses revealed significant PSV and EDV improvements in females and the microalbuminuria group. Conclusion: Autologous dendritic cell therapy significantly improved renal hemodynamics and showed potential to reduce fibrosis by modulating TGF-β and MMP-9 levels in DKD patients, warranting further investigation.
Full article
Open AccessArticle
Exploring Self-Perceived Stress and Anxiety Throughout Pregnancy: A Longitudinal Study
by
Mar Miguel Redondo, Cristina Liebana-Presa, Javier Pérez-Rivera, Cristian Martín-Vázquez, Natalia Calvo-Ayuso and Rubén García-Fernández
Diseases 2025, 13(4), 121; https://doi.org/10.3390/diseases13040121 - 19 Apr 2025
Abstract
►▼
Show Figures
Background: Anxiety and stress are common during pregnancy and can impact the health of the pregnant woman and the newborn. There is a lack of research focused on identifying weaknesses that promote equity in the care of pregnant women. The objective of this
[...] Read more.
Background: Anxiety and stress are common during pregnancy and can impact the health of the pregnant woman and the newborn. There is a lack of research focused on identifying weaknesses that promote equity in the care of pregnant women. The objective of this study was to describe the levels of anxiety and stress during the three trimesters of pregnancy and to compare whether there are differences according to obstetric and gynecological variables. Methods: A descriptive prospective longitudinal and correlational observational study was carried out. Non-probability sampling was carried out with 176 women. The Pregnancy-Related Anxiety Questionnaire and the Perceived Stress Scale were used. Results: The prevalence of anxiety was 23.9%, 17%, and 17.6%, and mean stress scores reached 32.24, 33.02, and 49.74 in the first, second, and third trimesters, respectively. In comparison, without miscarriages, anxiety was higher during the first trimester. In multiparous women who had suffered a miscarriage, anxiety was higher in the first trimester. Conclusions: Anxiety is higher during the first trimester. Mean stress levels are higher during the third trimester compared to the other two trimesters. Care for these vulnerable pregnant women can impact society’s health system and align with the Sustainable Development Goals of Health and Well-being and Gender Equality in others.
Full article
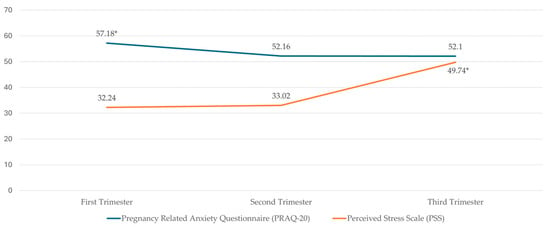
Figure 1
Open AccessArticle
Factors Influencing Physical Performance and Quality of Life in Post-COVID-19 Patients
by
Ajchamon Thammachai, Patchareeya Amput and Sirima Wongphon
Diseases 2025, 13(4), 120; https://doi.org/10.3390/diseases13040120 - 19 Apr 2025
Abstract
Background: This study aims to identify the factors related to demographic variables and physical performance associated with quality of life (QoL) in post-COVID-19 pa-tients who have recovered from mild infection and were not hospitalized. Methods: Seventy-four post-COVID-19 individuals who recovered from
[...] Read more.
Background: This study aims to identify the factors related to demographic variables and physical performance associated with quality of life (QoL) in post-COVID-19 pa-tients who have recovered from mild infection and were not hospitalized. Methods: Seventy-four post-COVID-19 individuals who recovered from mild COVID-19 infec-tion were assessed for the baseline demographic variables (age, sex, height, weight, body mass index; BMI) and clinical information (comorbidities, duration of COVID-19 infection, and exercise habits). Vital signs (heart rate, blood pressure, and oxygen sat-uration; SpO2) were measured. Physical performance was evaluated for upper- and lower-limb muscle strength, ability of balance, and cardiorespiratory performance. All participants were assessed for QoL. Results: Hand grip strength was negatively asso-ciated with gender and age while positively associated with the duration of COVID-19. Quadricep strength also showed a negative association with gender and duration of COVID-19. Age was positively associated with multiple quality of life dimensions, while emotional role limitations were negatively associated with the duration of COVID-19 and waist circumference. Mental health was negatively linked to BMI. Conclusions: This study highlights the complex impact of COVID-19 on physical per-formance and QoL, revealing that older adults often report better QoL despite reduced muscle strength, particularly in women. The findings emphasize the need for targeted rehabilitation programs addressing both physical and emotional health for vulnerable groups.
Full article
Open AccessBrief Report
Possible Significance of Neutrophil–Hemoglobin Ratio in Differentiating Progressive Supranuclear Palsy from Depression: A Pilot Study
by
Michał Markiewicz, Natalia Madetko-Alster, Dagmara Otto-Ślusarczyk, Karolina Duszyńska-Wąs, Bartosz Migda, Patryk Chunowski, Marta Struga and Piotr Alster
Diseases 2025, 13(4), 119; https://doi.org/10.3390/diseases13040119 - 18 Apr 2025
Abstract
Background: Research has associated chronic inflammation with the evolution of neurological and psychiatric disorders. Neurodegenerative diseases, including Parkinson’s Disease (PD), Alzheimer’s Disease (AD), and less common ones such as Progressive Supranuclear Palsy (PSP), are commonly linked to depression. However, the pathomechanisms and the
[...] Read more.
Background: Research has associated chronic inflammation with the evolution of neurological and psychiatric disorders. Neurodegenerative diseases, including Parkinson’s Disease (PD), Alzheimer’s Disease (AD), and less common ones such as Progressive Supranuclear Palsy (PSP), are commonly linked to depression. However, the pathomechanisms and the role of neuroinflammation in these disorders remain unclear; therefore, interest is increasing in easily accessible inflammatory morphological assessments of blood samples, such as the neutrophil-to-lymphocyte ratio (NLR), the neutrophil-to-monocyte ratio (NMR), and the neutrophil-to-hemoglobin ratio (N/HGBR). Methods: The authors analyzed 15 age-matched controls and 21 patients with PSP; the PSP group was additionally divided into 11 patients without depression (PSP) and 10 with depression (Beck Depression Inventory [BDI] ≥ 14) (PSP-D). Results: In the PSP-D group, the level of N/HGBR was significantly lower than in the controls (p = 0.01), but there were no significant differences in any other neutrophil-derived parameters or comparisons of morphological blood assessment. Patients with PSP-D exhibited a marginally significant decrease in neutrophil levels compared to the controls. Conclusions: This is the first study highlighting the possible significance of peripheral inflammatory factors in patients with PSP affected by depression. It highlights possible tendencies in the area of non-specific inflammatory markers and suggests their relation to affective disorders in PSP.
Full article
(This article belongs to the Special Issue Research Progress in Neurodegenerative Diseases)
►▼
Show Figures
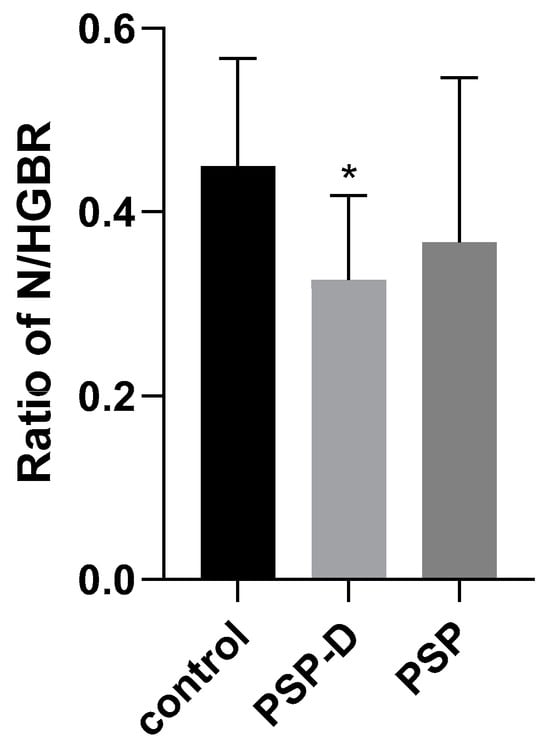
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Cancers, Current Oncology, Diagnostics, Diseases, Onco
Artificial Intelligence in Cancer Pathology and Prognosis
Topic Editors: Hamid Khayyam, Ali Hekmatnia, Rahele Kafieh, Ali JamaliDeadline: 1 May 2025
Topic in
Biomolecules, Cancers, Diseases, Neurology International, Biomedicines
Brain Cancer Stem Cells and Their Microenvironment
Topic Editors: Maria Patrizia Stoppelli, Luca Colucci-D'Amato, Francesca BianchiniDeadline: 31 December 2025
Topic in
Biomedicines, Diseases, JCM, JPM, Uro, Reports
Clinical, Translational, and Basic Research and Novel Therapy on Functional Bladder Diseases and Lower Urinary Tract Dysfunctions
Topic Editors: Hann-Chorng Kuo, Yao-Chi Chuang, Chun-Hou LiaoDeadline: 31 December 2026
Topic in
Cancers, Current Oncology, Diseases, IJMS, Cells
Cellular and Molecular Mechanisms of Obesity-Associated Cancer Development and Treatments
Topic Editors: Ming Yang, Chunye ZhangDeadline: 31 August 2027

Conferences
Special Issues
Special Issue in
Diseases
Treatment Strategies and Immune Responses in Rheumatic Diseases
Guest Editor: Rita Aguiar MouraDeadline: 30 April 2025
Special Issue in
Diseases
Feature Papers in the 'Respiratory Diseases' Section in 2024–2025
Guest Editors: Gaetano Caramori, Andrea BiancoDeadline: 1 May 2025
Special Issue in
Diseases
Targeted Therapies for Acute Leukemias
Guest Editor: Eleftheria HatzimichaelDeadline: 31 May 2025
Special Issue in
Diseases
Cancers of the Genitourinary System: Pathophysiology, Modeling, and Treatment
Guest Editors: Hisham Bahmad, Wassim Abou-KheirDeadline: 9 June 2025
Topical Collections
Topical Collection in
Diseases
Effects of Food Antioxidants on Cardiovascular Diseases and Human Cancers
Collection Editors: Esra Capanoglu, Maurizio Battino
Topical Collection in
Diseases
Lysosomal Storage Diseases
Collection Editors: José A. Sánchez-Alcázar, Luis Jiménez Jiménez










