1. Introduction
According to World Health Organization (WHO), approximately 830 women die, every day, from preventable causes related to pregnancy and childbirth [
1]. The ratio of maternal mortality is high in poor and rural areas, and almost 99% of maternal deaths take place in developing countries. The major causes that account for nearly 75% of all maternal deaths are [
1]:
Pre existing conditions (28%)
Severe bleeding (27%)
Pre-eclampsia and eclampsia (14%)
Infections (11%)
Obstetric labor and others (9%)
Unsafe abortion (8%)
The number of maternal deaths has declined by 44% worldwide since 1990. However, from 1990 to 2015, the decrease was only 2.3% per year, which was well below the annual decline of 5.5% required to achieve millennium development goal 5 (MDGs5) [
1,
2].
Most of the maternal deaths can be avoided since the health-care solutions to prevent and manage complications of pregnancy are widely known [
1,
3]. During pregnancy, childbirth and weeks after childbirth, all women need support and timely access to skilled nursing care. However, factors that prevent women from receiving care during pregnancy and childbirth are poverty, delays, lack of information and awareness, lack of adequate healthcare services and skilled health professionals, home deliveries and cultural practices [
1]. The delays include (i) delay at home in identifying an emergency situation and making a decision to go to a healthcare center, (ii) delay on the way in reaching the healthcare center and (iii) delay in the healthcare center in receiving effective healthcare interventions [
4]. Technologies including computers, smartphones, communication systems and eHealth applications can play an important role in minimizing these factors and can contribute to a significant reduction in maternal mortality around the world [
5].
The number of mobile phones in the world was 97 per 100 people at the end of 2014 [
6] and exceeded the world population in 2016, and among those, more than 50% are smartphones [
7]. Similarly, the number of Internet user worldwide is increasing day by day and was three billion in 2015 [
6,
8]. Mobile phones are increasingly used by more women, where some of them are from the poorest and most remote areas of the world [
9]. Mobile and wireless technologies can provide exciting low-cost highly-reachable healthcare services such as managing chronic diseases, empowering elders and pregnant women, reminding people to take medicines at the proper time, facilitating health services to remote areas, generating customized health information and improving the outcomes of health and medical systems [
10]. The improved organization of medical data, advanced data security techniques and the standardization of Internet protocols is increasingly making it possible for health professionals in different locations to reach, connect and understand each other easily. In addition, it also offers significant opportunities for improving the data analysis and replacing the traditional paper-based healthcare system where developing a national or regional overview of patient statistics is extremely difficult.
With the rapid growth in communication and information technologies (ICT), the field of eHealth has now emerged in many forms, and its potentials have been experimented on and discussed globally. eHealth is frequently becoming an essential part of people’s everyday lives and has the ability to improve the delivery and cost of healthcare and the quality of the patient experience [
11]. It enables the exchange of clinical information, physiological signals, medical imagery and laboratory results and has the capacity to revolutionize healthcare systems by delivering life-saving information even in the most remote and low-resource settings [
12]. With the development of communication technologies and eHealth applications, it is now reasonable to expect that in coming years, everyone living on our Earth will, from any location and at any time, be able to access the World Wide Web and will benefit from cost-effective, automated and personalized healthcare [
13,
14]. Improvement in data speeds, miniaturization of computers and smart devices with higher levels of reliability and security, decreasing costs and increasingly user-friendly features are becoming the main reasons for adopting eHealth solutions in our daily lives [
15]. However, the usefulness of eHealth applications does not lie in the underlying technology itself, but in the ability to develop effective networks among health professionals and patients and increase awareness in the field of health.
Different types of networks, such as family networks, social networks and professional networks, are playing an important role in our daily lives. Social networks include our friends, those we meet in our classroom, people we like to spend time with and those we engage with on social media. Similarly, our family network includes all of our family and extended family members. Lastly, our professional network includes colleagues, co-workers and customers. In the healthcare system, face-to-face meetings are always the most useful and important contact. However, a professional network of patients and health professionals can be vital to both sides. Smartphone-based devices in combination with Internet connectivity have the potential to create a network of healthcare providers and patients in order to reduce their communication gap. Such a network can create remarkable and unprecedented opportunities for improving maternal and child health outcomes by facilitating interactions and information sharing between health professionals and patients [
16].
Besides improving the interaction and communication links, such a network can be used to increase the awareness and education of patients on health issues. Generally, less than 10% of mothers know about the development of the fetuses they were carrying [
17]. Not only that, the pregnant mothers do not know what are the good and bad things they should do and avoid during pregnancy. There should be a way to help expectant mothers be aware of their pregnancy development. They should be able to access pregnancy-related customized information and useful tips regarding each stage of their pregnancy at their fingertips and should be connected to healthcare providers whenever and where ever they want. Communication technologies and smartphone devices can be used as a fast and efficient way to push customized and timely information to every possible pregnant woman regardless of her location. This will not only help in information sharing between pregnant women and maternity homes, but will also improve decision making and reduce delays.
Based on the discussions in the previous paragraphs, this work aims at proposing and designing a network model, the Pregnancy Care Network (PCN), which aim to strengthen communication links between healthcare providers and pregnant women and increase education, awareness and quality of nursing care during pregnancy. The goal is to educate mothers, monitor pregnancy, prevent pregnancy complications and improve maternal health. The PCN, a computer and smartphone-based application will not only help pregnant women know about their maternal health and pregnancy-related complications but will also connect them to maternal healthcare providers. Besides, it enables maternal health reporting by allowing health professionals to collect real-time data about pregnant women and their status in a region, for effective care, follow-ups and policy-making.
Overall, PCN will help develop a communication and alert system, monitor pregnancies, increase antenatal care visits and the number of facility deliveries through automated reminders, develop an overview of women’s statistics and sharing pregnant women’s real-time data between institutions for an effective referral. Moreover, PCN can contribute to the reduction of delay associated with transport to the referral facility and delay associated with timely intervention when the mother reaches the referral facility.
2. Background
Before the arrival of smartphones, Personal Digital Assistants (PDAs) were experimented on with electronic health tools. These tools were designed to improve health monitoring, management, education and decision-making and offered a significant advantage over paper-based data collection [
18]. Blaya et al. [
19] showed that PDAs, used for collecting tuberculosis data over a large geographical area in Peru, were more efficient and reliable than paper-based data collection.
After the arrival of PDAs, systems facilitating electronic medical record keeping, storage and communication systems for medical data, laboratory information systems that automate testing and reporting and early disease warning were introduced. These systems collect data from patients and healthcare facilities to create community-wide views of disease trends and clinical activities [
20]. In addition, systems facilitating care at remote areas were implemented to use a Short Message Service (SMS) for reminders, monitoring, health education and asynchronous communication.
For instance, a mobile phone-based system [
4] was implemented in Rwanda to monitor the information on pregnancy and newborns. An SMS-based project was developed to trace the number of pregnancies and their related complications in the community through instant messaging. The project enabled community health workers to send timely notification of emergencies by sending an SMS to healthcare centers and emergency and ambulances services. The system helped women by reducing the delays in getting effective and on-time healthcare interventions. The system also served as a remote data entry point for pregnant women and their health statistics and as a unique interface to provide real-time data to healthcare providers.
Similarly, a cluster-randomized, controlled trial [
21] evaluated the effect of a mobile phone intervention on perinatal mortality in a low resource setting in Zanzibar. Two thousand five hundred and fifty pregnant women, where 1311 women were in the intervention group and 1239 in the control group, from 24 primary healthcare centers in six districts were included in the study and followed until 42 days after delivery. The intervention was based on a text message sent from mobile phones. Mobile phone applications were shown to improve the health of the newborn and were suggested to be considered by policymakers in low resource settings.
Besides SMS-based messaging systems, eHealth applications were also developed for improving maternal health outcomes. PotM, a mobile health application [
22,
23], was developed to assist health professionals in the management of pre-eclampsia. PotM was a decision-based model that integrated the risk prediction of adverse maternal outcomes associated with pre-eclampsia with the recommendations of WHO for the management of pre-eclampsia. PotM combines two previously successful innovations of the miniPIERS (mini pre-eclampsia integrated estimate of risk score) risk assessment model [
24] and the phone oximeter into an mHealth app. The application guides and trains health professionals with systematic and standardized procedures of antenatal assessment, including measurement of blood pressure, dipstick proteinuria and symptoms.
There are a plenty of pregnancy-related applications on the World Wide Web and the Microsoft, Google Play and Apple stores. However, none of them utilize mobile and wireless technologies to provide pregnant women the opportunity to enhance their pregnancy-related knowledge, prevent and control the complications of pregnancy, nor connect them to nurses and other healthcare providers by establishing a reliable communication and alert system. The aim of this design is to educate women, monitor pregnancy and connect pregnant women with nurses and other health professionals.
3. Methodology
3.1. Pregnancy Care Network (PCN) Overview
This section discusses the main features of the PCN and presents the theoretical design of PCN in details. The prevalent functionality of the PCN is to equip nurses, healthcare providers and expectant mothers with a mobile and computer-based application, which will help them manage their pregnancy-related knowledge and needs. PCN will store, query and retrieve pregnancy-related information and women’s health records including their clinical data. Health records and clinical data of women will reside on a remote server, uploaded/stored by healthcare providers and pregnant women themselves through a web user interface and PCN client application. Pregnancy-related information (for education and awareness purpose) will be stored locally on the smartphones or computers where the application is installed in order to be used without an Internet connection. PCN will allow users to browse medical content (such as symptoms, preventions, guidance in case of danger signs and unknown conditions), as well as upload and modify clinical data and laboratory results. In addition, it will enable fast and reliable communication between nurses, healthcare providers and pregnant women.
The network is designed keeping in mind both low- and high-resource settings, making it equally applicable in all scenarios. In low-resource settings where there is no Internet connectivity, PCN will use SMS and the local mobile operator for emergency communication. In the presence of Internet connectivity, PCN will have access to the latest data from the central server and will facilitate audio and video communication between pregnant women and healthcare providers. Synchronization of the women’s data with the central server will take place when Internet connectivity becomes available.
The primary users of PCN will be pregnant women, nurses and other health professionals who are responsible for delivering healthcare to pregnant women in the community healthcare centers or in a hospital setting. The education level of these users can vary significantly, so the use of PCN and its interface are intended to be kept as simple as possible while still being completely comprehensive at all levels of intended use.
PCN will offer an interface to healthcare providers for registration of new pregnancies at the community or hospital level. Registered pregnancies will be effectively monitored up to the time of delivery and postpartum. At each level (in the community or hospital), selected staff in charge of maternal and child health will be responsible for motivating community members to attend antenatal care and provide support and referral to the healthcare centers particularly in the case of emergency situations. After the registration of new pregnancies in the system, women download and install the application on their smartphone or PC, start getting customized information about their pregnancy and report all danger signs to the respective authorities through the facility provided in PCN.
For a normal pregnancy (when no danger signs are reported), the PCN will send automated notification and reminders at specific dates for clinical appointments (medical check-ups and follow-up visits), the development of the fetus, delivery date, etc., through the application and by SMS. In the case of danger signs, an emergency alert system can be activated by women, which provides immediate communication with the respective healthcare provider, advising on immediate action. Ambulance requests can automatically be routed to the nearest available ambulance service to ensure that the women/newborns are transferred in a timely manner to emergency obstetric and neonatal care.
3.2. System Architecture
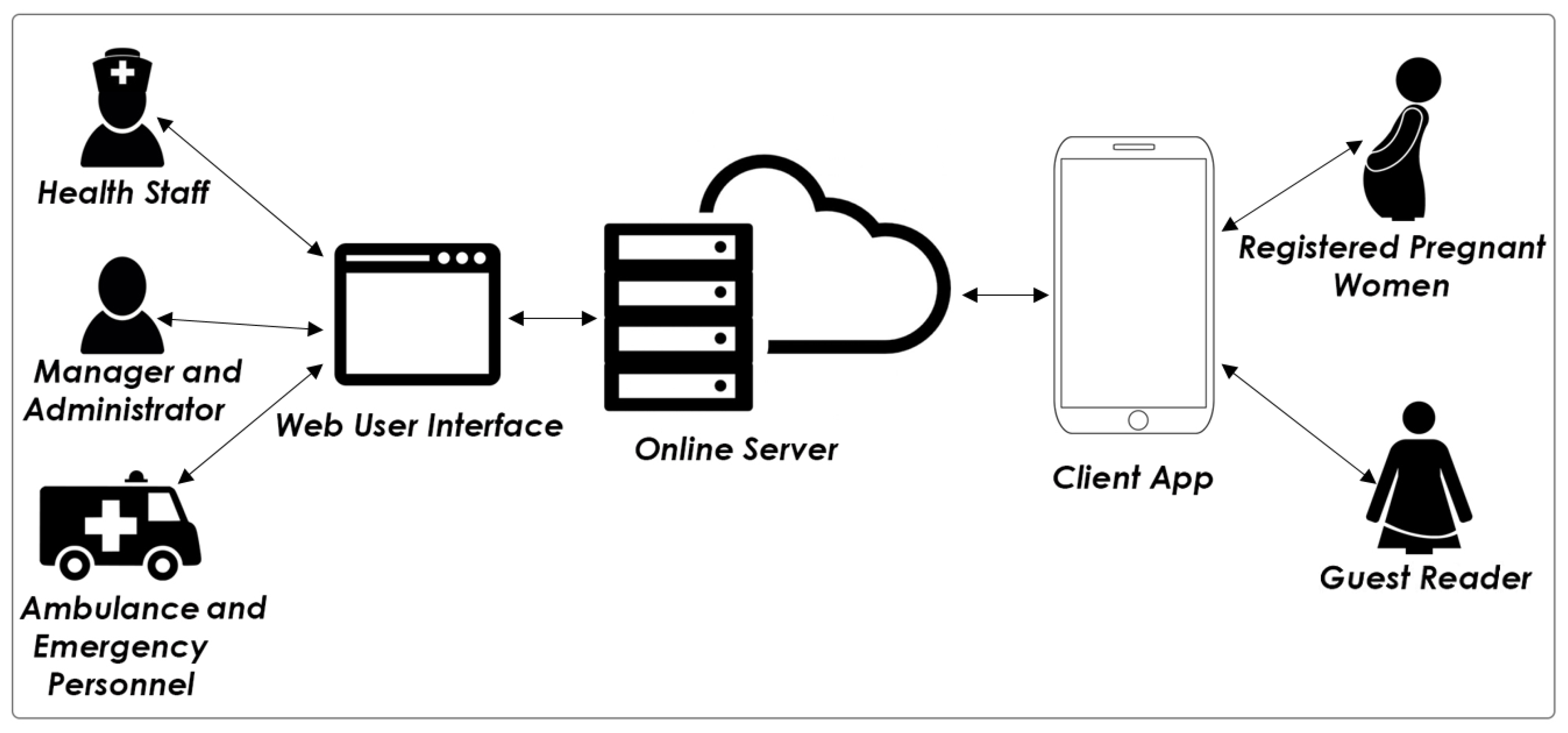
Figure 1 illustrates the design and proposed system architecture of PCN. The main components of the PCN are the online server, web user interface and the client app. Two interfaces, a web client and a standalone application, will allow the user to communicate and interact directly with the online server and will allow the management and storage of women’s health records. The web client (web user interface) will be used by the health staff, health supervisors and emergency team, while the standalone application (client application) will be used by pregnant women and general interested readers. The online server manages the physical infrastructure, such as the storage of files and women’s health records, and is also responsible for performing maintenance operations, such as backing up data, etc.
The main database at the central server is comprised of women’s health records and will be dedicated to collecting, storing, processing and making available health information important to the delivery of quality care to pregnant women during pregnancy and after childbirth. The clinical data consist of longitudinal records of a woman’s care provided at different times in different healthcare facilities. Women’s health records include demographic data, medical history, laboratory results, immunization history, radiology reports, drug allergies, etc.
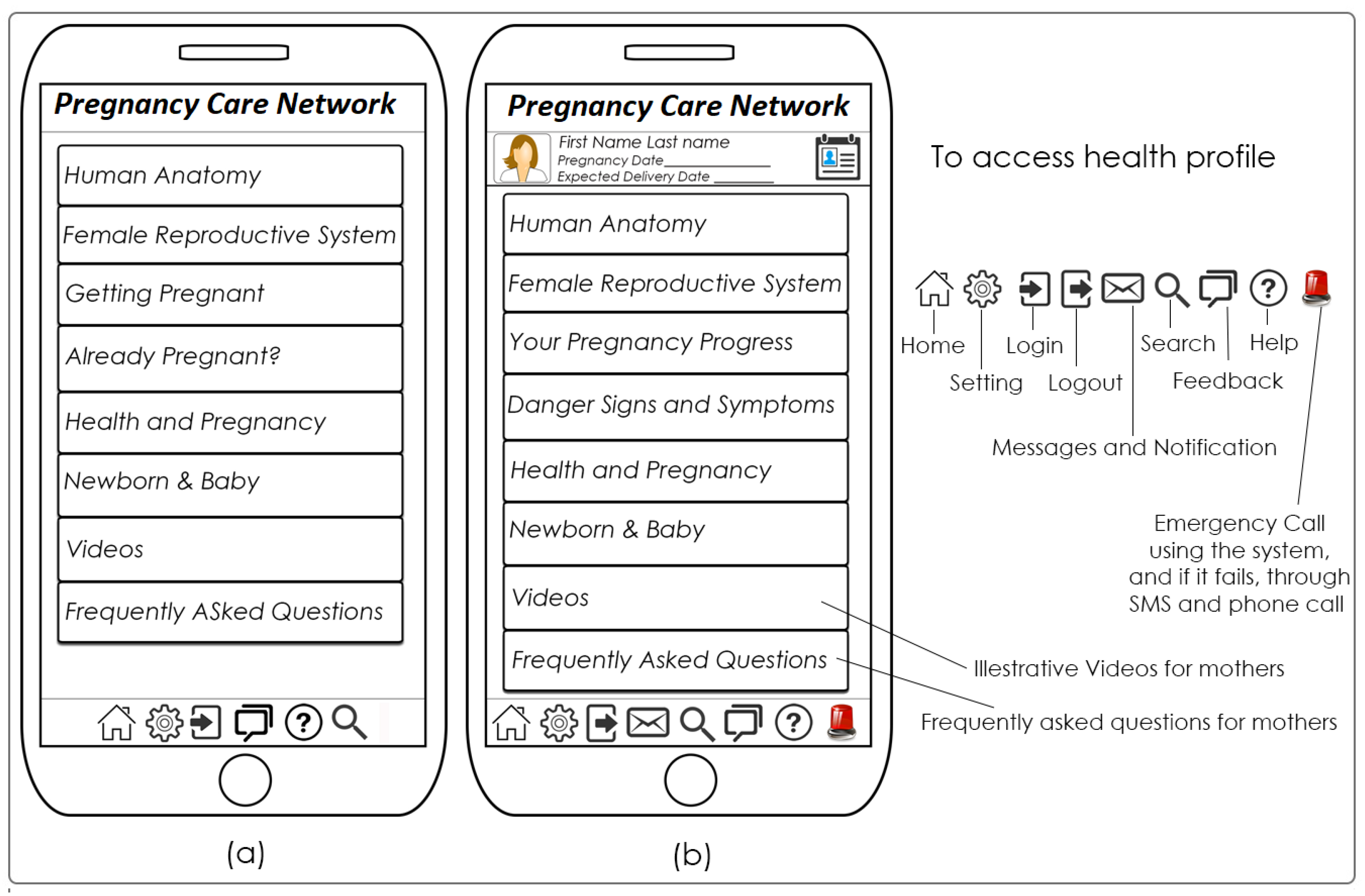
Similarly, in the client app, pregnancy-related information will be organized by time (month), by signs and symptoms and by disease name with the search facility, as well, as shown in
Figure 2. The locally-maintained medical content will include information about the female anatomy and reproductive system, health issues related to pregnancy, danger signs and precautionary measures in the form of videos, pictures and text and Internet links.
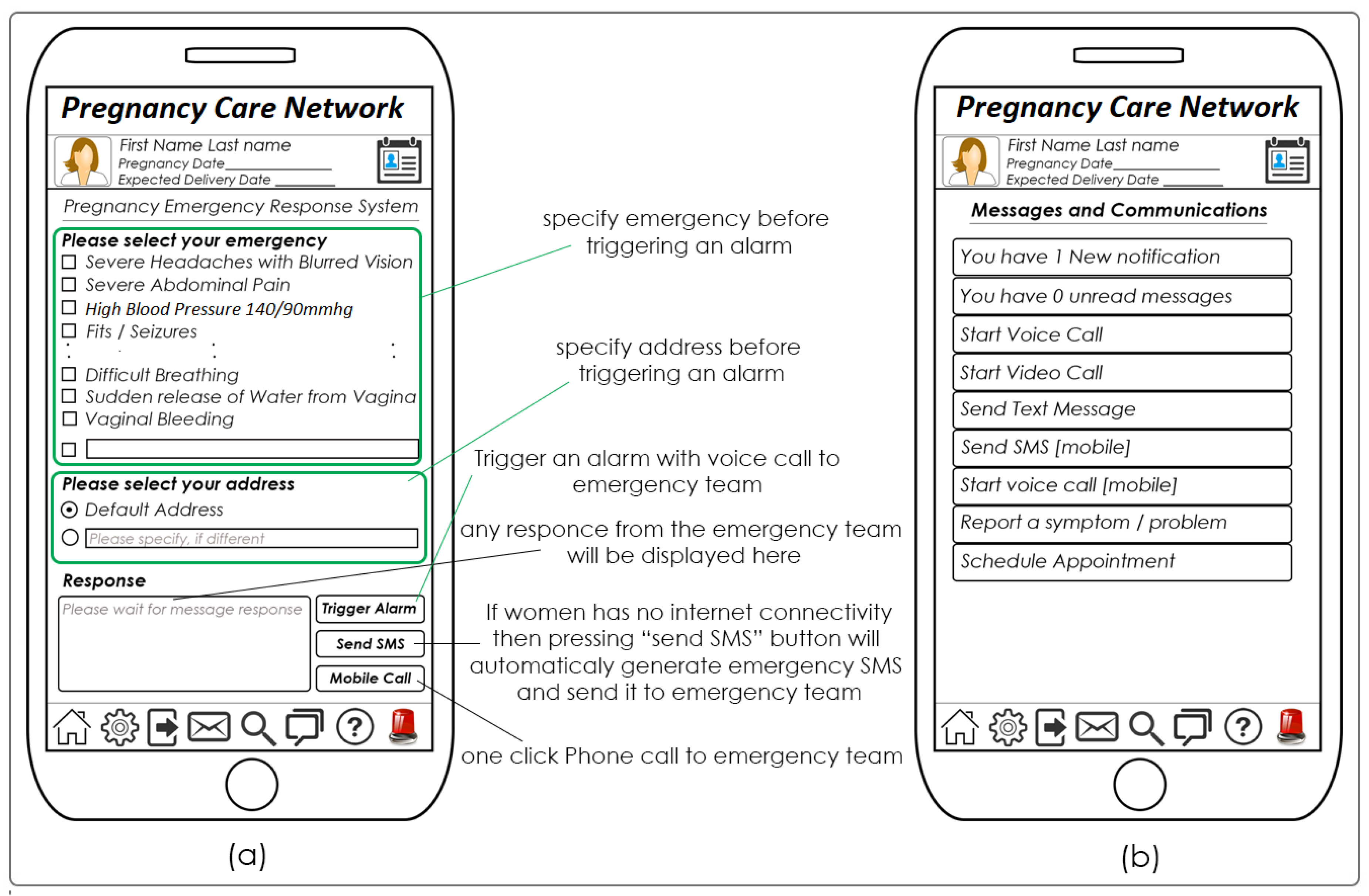
In addition to getting customized information, the client application can also be used by pregnant women (if needed) to communicate with nurses and other health professionals. This communication can be real time (with video, audio and text chat facility) or can be asynchronous where the sender and receiver reply whenever they are available. In the case of non-availability of Internet coverage, pregnant women can send an important message via SMS. All she has to do is to press a button, and the application will compose necessary content for the SMS and will send it to the web user interface and the pre-defined mobile number of the respective health professionals. There is also a one-click emergency call option where the emergency team can be contacted via the client application both through the Internet and the local mobile operator.
Similarly, the web user interface allows nurses and other health professionals to register pregnancy, manage and maintain women’s health records, interact and communicate with women, send messages and reminders and schedule appointments.
The complete system of PCN consists of a client application running on the user’s smartphone, a central database containing all demographic and clinical data of women on an online server and a web user interface that allows health professionals and supervisors to enter, retrieve and analyze health data of expectant mothers as shown in
Figure 3.
The client application will be freely available for download where everyone, regardless of pregnancy status, will be able to install and use it. The central database along with the web user interface will be installed on a secure online server. Access to the web user interface can then be distributed and granted with the permissions/guidelines of the competent health authorities/government health officials.
3.3. System Development
The methodology used for planning, creating, testing and deploying an information system or software is called the application development life-cycle. It is a process of splitting the software development work into different phases with the aim to better plan and manage the whole task. The iterative and incremental development [
25] methodology was used for the development of PCN. With this methodology, the system is developed through repeated cycles (hence iterative) and in smaller portions at a time (hence incremental). This allows the software developer to take advantage of what was learned during the development of earlier parts or versions of the system. The development is started with a basic implementation of the system, and then, iteratively, new features and functionalities are added and design modifications are made, as needed.
It must be noted that during this work, the first two phases (requirements and design) of the development process of PCN have been focused on and completed. The others phases are in the pipeline and are intended to be completed, as well.
The development of PCN involves a process consisting of the following steps [
25].
Requirements: This phase consists of gathering information about the target population, determining the needs or conditions to meet, deciding the content and knowledge to be delivered, the tasks and function to be completed and analyzing available technologies feasible for development and implementation.
Design: The design phase consists of planning, creating specifications, conceptualizing and framing the material and production of content, preparing the storyboard, layout design and user interface.
Develop: The third phase involves the creation of the activities that will be implemented. It consists of developing and programming the navigation structure, user interface, settings, images, content and animations.
Test: Testing ensures that the materials achieved the desired goals and basic functionality. It is used to verify whether the component meets the requirements decided earlier, responds correctly to all kinds of inputs, performs its functions in an acceptable manner, is sufficiently usable, can be installed and used in its intended environments and achieves the general result its end users require.
Debug: Debugging is the process of identifying and removing errors that prevent correct operation of the system.
Deployment: This stage consist of the installation of systems files on a central server and making available the client application through different mobile platforms.
Evaluate and maintain: This phase involves review, evaluation and modification of a component after deployment to correct faults, add features, improve the performance or other attributes.
3.4. Technology and Tools
During the design and development of PCN, free software will be preferred whenever possible.
Visual Studio Community 2015 Edition, which is a free and rich integrated development environment for creating desktop, web and mobile applications, is used. It contains a workspace and an extensible plug-in system for customizing the environment. Visual Studio Community 2015 Edition comes with Xamarin, which is a tool used to write native Android, iOS and Windows applications with native user interfaces and share code across multiple platforms. For the development of the client app, Visual Studio together with the C# programming language and Xamarin are preferred used.
For the server-side application and web user interface, ASP.net and the C# programming language will be preferred. The SQL Server database is intended to be used for storing and managing demographic and health records of expectant mothers. For the production of two-dimensional graphics and manipulating and retouching photos, Microsoft Paint and Adobe Photoshop CS6 are suitable. In addition, tools like JavaScript, XML, AJAX, Web 2.0, Web-services and JSON will also be incorporated during the development of PCN.
Programming files of PCN will be installed on a central server, and the client application will be made available for free download on different mobile platforms (Windows, Android and iOS), where anyone will be able to download it and use it.
3.5. User Interface
The web user interface and client application will be equally used from any computing device such as smartphones, tablets and desktops. Both interfaces will be responsive (adjusted automatically according to the device screen size); however, the web user interface is optimized for large screens, as it is intended to be used by health professionals mostly in their offices. Contents such as women’s records will reside remotely on an online server, and contents such as information for women’s education will reside locally in the client application; however, access to all information will be presented to the user as the resources are located locally in the device. Women’s clinical data management, information regarding women’s status and related biosignals can be displayed and managed through the system’s interface (web user interface and client application). Pregnancy-related information (for educating women) is stored locally in the client application so that it can be used without any active connection to the Internet. However, connectivity to health professionals will require an active Internet connection or a mobile operator connection.
3.5.1. Client Application
PCN will support the ability to input, view and edit the pregnant women’s history and medical information. The application will also allow viewing of past evaluations and prescribed medications. All entries are stored with timestamps to assure data consistency. The expected delivery date is calculated from available data such as ultrasound measurements, last menstrual period or fundal height.
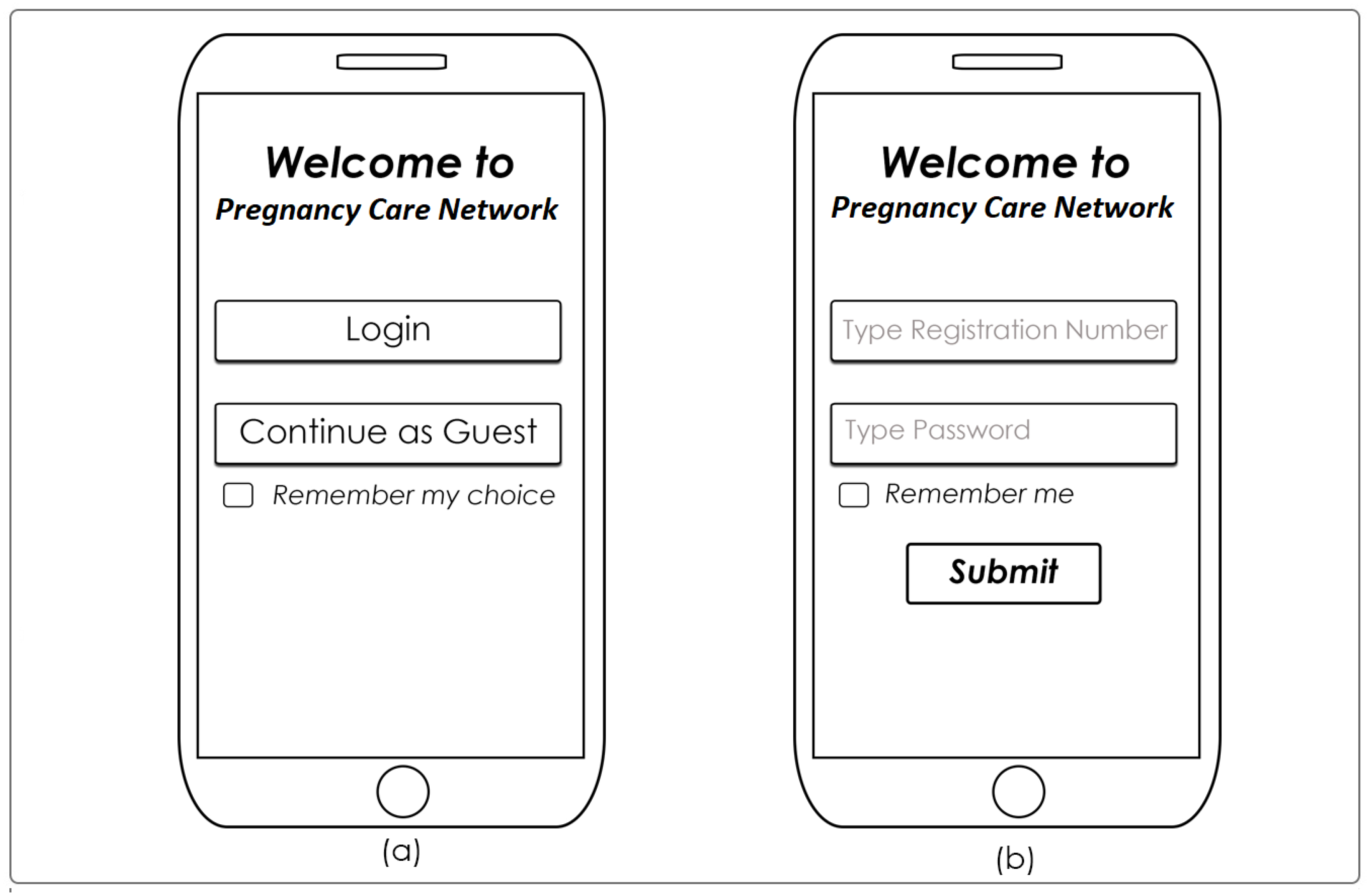
The first screen of the client application is shown in
Figure 4a, where the user has an option to use the application as a guest user or as a registered pregnant women. As a guest user, only pregnancy-related information is available for display.
Figure 4b shows the login screen for registered pregnant women. Similarly,
Figure 5a shows the front screen for the guest user when they enter the client application, and
Figure 5b shows the front screen for registered users where pregnancy-related information, as well as clinical data, are available.
The application will display pregnancy-related information divided into different sections. The application will educate women about female anatomy and pregnancy-related diseases and provide help and guidance regarding prevention, control, signs and symptoms of each stage and complication of pregnancy and delivery. It will provide interactive information based on text, images, videos and Internet links and will keep women informed and connected anytime, anywhere.
Figure 6 is self-explanatory and shows options for communication with health staff and the emergency team. The system supports a bi-directional flow of information. A registered health professional can create and send a customized message to particular women. In the same way, registered women can create and send customized messages to health professionals and emergency teams. Each party will be notified if it receives a message, and the sender will be notified when his/her message is read. If a high priority message is not signaled read in a particular amount of time, it is assumed that the receiver is offline, and an SMS will be sent as an alternative method. In case the Internet is not available, the client application will automatically send the communication message through the local mobile operator at that location. For each registered pregnancy, the PCN will send notifications and reminders, one from the health professionals and one from the system itself (it will be automatic, based on the time and characteristics of women). In the case of danger signs (hemorrhage or unknown serious conditions) during pregnancy, the system can be used to send emergency requests to the nearest ambulance service manager for immediate intervention. The emergency message can be automatically generated with a click and will include the reported emergency sign, the name, address and contact details of women (see
Figure 6). A communication will be established or a message will be sent back to the women indicating the immediate action to be taken to manage the emergency till the arrival of the pending ambulance.
It must be noted that users can access information in a non-linear way, without any specific order to navigate the PCN, leaving the user free to establish the construction of knowledge.
3.5.2. Web User Interface
A password-protected web user interface, developed for nurses and other health professionals, gives access to women’s demographic and clinical data and enables tracking the history of individual women. The web user interface provides access to individual and aggregated reports on registered pregnancies and their complications, emergencies, deliveries, facility visits, maternal mortality and other characteristics.
Data can be viewed and filtered by a specific community, age, complication or other characteristics. Users (health professionals) working at each level will be assigned an account, authorizing him/her to view and possibly change data only at his/her respective level and role in the healthcare system.
3.6. Functionalities
Women will be registered in the system at their first pregnancy. Primary healthcare centers, maternity homes and hospitals, which have administrative access to the system, can register pregnancy of women when it is confirmed. All details of women are inserted into the system including name, date of birth, contact details, any medical conditions, etc. Each time a woman gets pregnant, her pregnancy has to be registered in the PCN system. If a woman is already in the system and this is the second or third time she becomes pregnant, then only her pregnancy is registered, and other registration details are updated (if required). At first registration, each woman will be allocated a unique username (or registration number) and a temporary password, which she can change later.
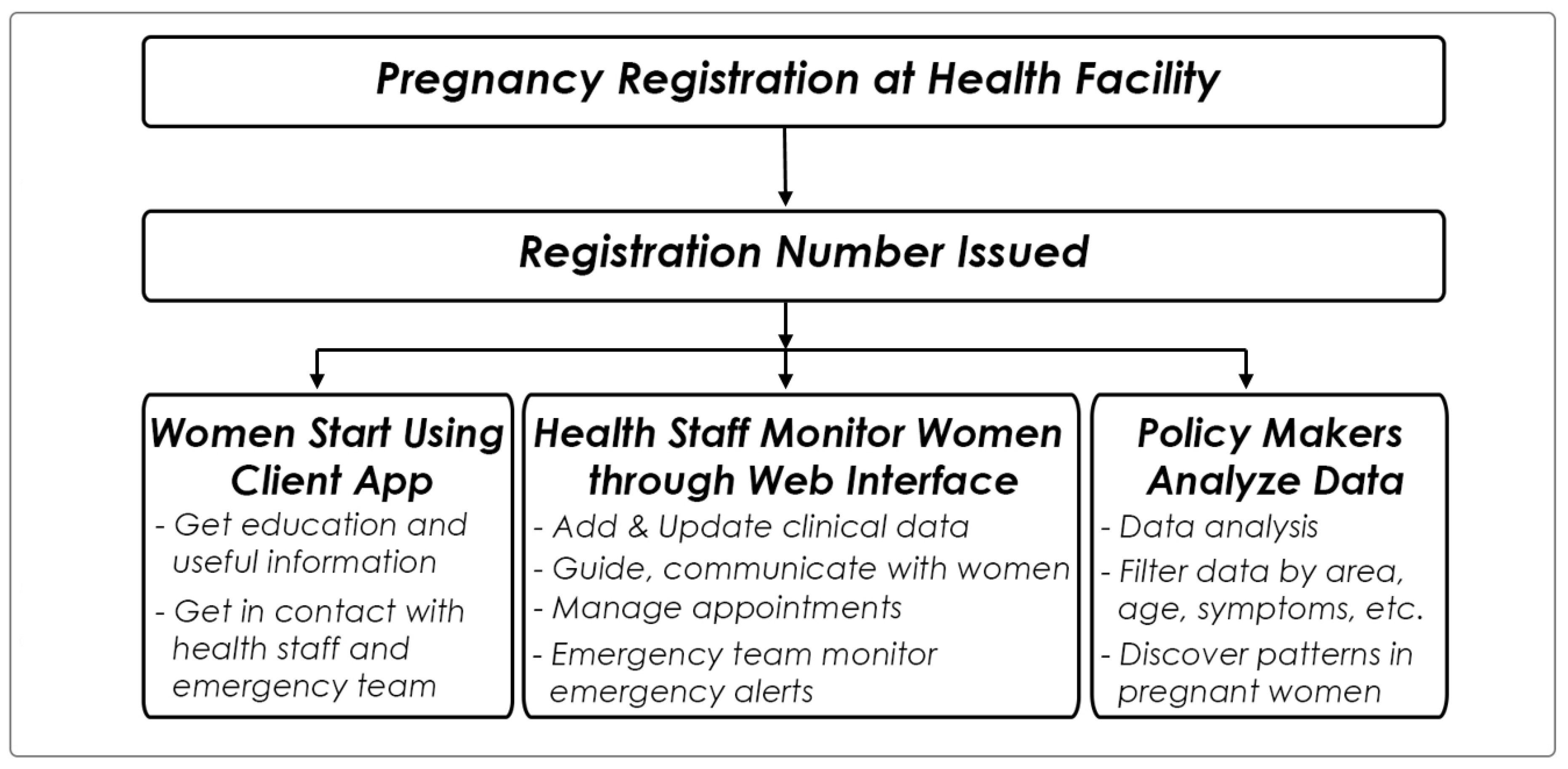
Figure 7 represents the information and workflow in the PCN system.
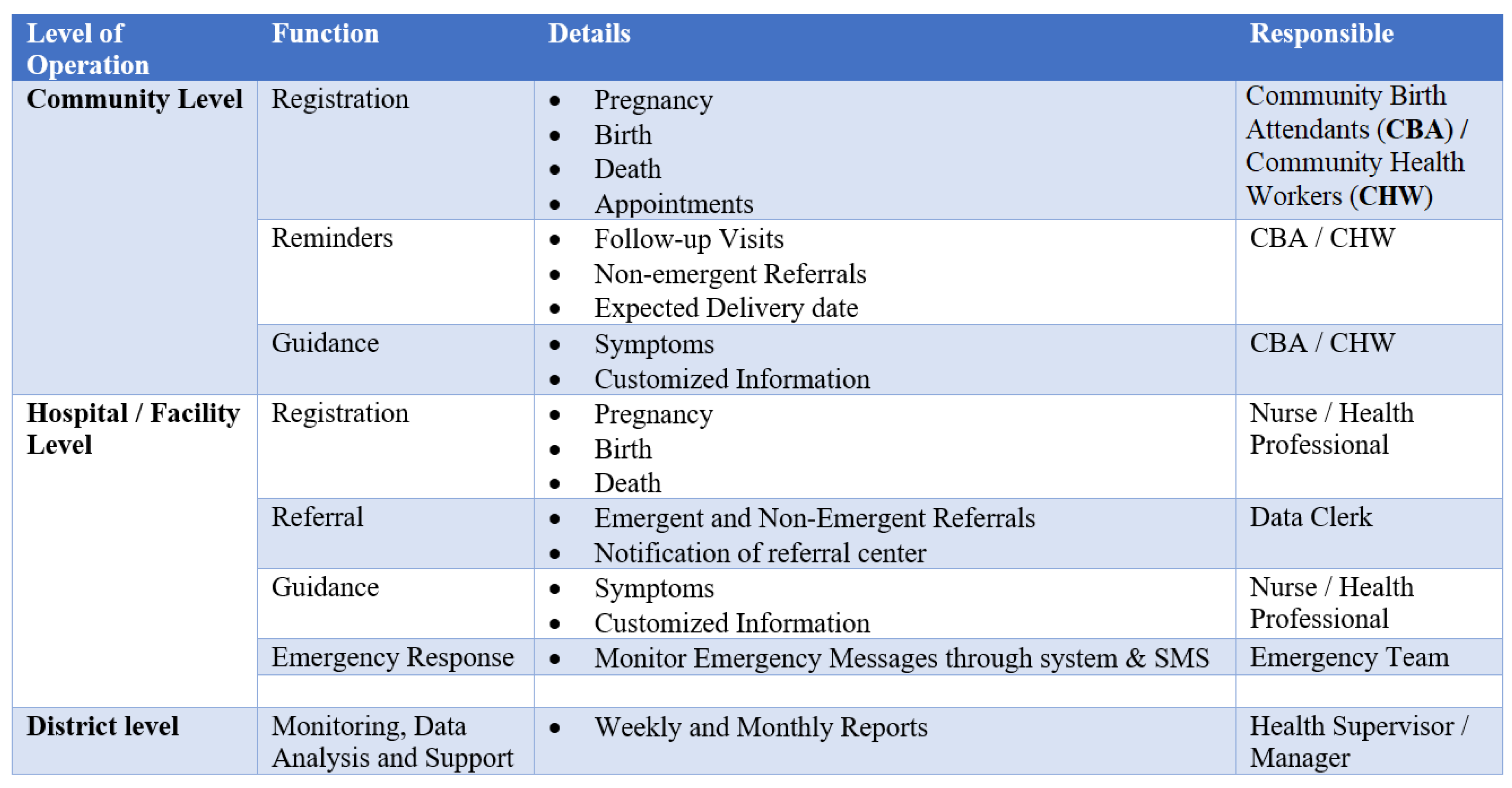
Each time pregnant women have some complication and visit a maternity home, their profile will be updated with the latest medical tests, treatment, etc. After registration, women will start using the client application (using smartphones, tablets or PCs). At each stage of pregnancy, women will get useful information and guidance about the respective complications in pregnancy. Pregnant women and nurses can use PCN to communicate with each other. Real-time communication can be done in case both parties are online at the same time; otherwise, a message will be left, which can be accessed when the user becomes online. Detailed functions of the system are presented in
Figure 8.
Primary healthcare centers and health authorities can get statistics of pregnant women in a certain region or area, which helps them in important decisions regarding women’s health and maternal mortality. PCN automatically reminds pregnant woman about each visit, follow-up visit, expected and delivery date, possible complication, nearest emergency and referral centers.
A feedback option is available for possible suggestions, improvements and complaints about the system from potential users. PCN will support the following tasks through its client application and web interface.
3.6.1. Using Client Application
Educate women.
Immediate access to women’s data (only available to registered users).
Longitudinal collection of health information of women (only available to registered users).
Connect with health staff and emergency service (only available to registered users).
Feedback to the system.
3.6.2. Using Web User Interface (Authorized Users)
Register pregnancies.
Search for the existing pregnancies.
Add and update clinical data.
Provide guidance, make appointments and referrals.
Set reminders.
Analyze data and monitor pregnancies.
Feedback to the system.
3.7. Security, Privacy and Confidentiality of Women’s Information
In the client app, the privacy of each registered pregnant women will be taken into account by using passwords for login. Access to an online database and clinical data is granted only to authorized users to protect and maintain women’s health information. On the web user, interface access can be granted by policies and job titles. Different policies can be generated for different types of staff according to their role in the health system. Each policy will define who can access and what type of activities are permitted. For instance, health staff is granted complete access in order to perform their care provision role. Similarly, the emergency team has no access to clinical data; they can only communicate and respond to emergency calls from authorized pregnant women and health professionals. Despite the particular access level, it is the healthcare professionals’ responsibility to protect and maintain the privacy of women’s information and clinical data. Moreover, the online server will be configured to back up necessary data on a weekly basis.
4. Expected Results
It is expected that the PCN system will improve the quality, speediness and efficiency of pregnancy care during pregnancy and childbirth. It will enable effective and easy two-way communication between pregnant women and the healthcare system (including ambulance services) at the community, district and central level. The main objectives and outcomes of the PCN will be an increased awareness of pregnancy-related complications, improved access to antenatal and postnatal care, minimizing home deliveries and enhancing emergency obstetric care. In addition, PCN will provide a database for storing and manipulating clinical records of pregnant women and maternal care delivery.
PCN will make possible easy and useful communication between pregnant women and healthcare providers and will improve women’s knowledge and awareness regarding pre-eclampsia and eclampsia and other pregnancy-related complications and maternal health. It will reduce the different types of delays associated with pregnancy care such as in-home (due to a lack of information and awareness).
PCN will improve antenatal and postnatal care and record keeping and will act as maternal health indicators for policymakers. This network will enable monitoring, follow-up, referrals and interactive information for pregnant women along with continuity of care from the start of the pregnancy all the way through her postpartum period.
PCN will replace traditional paper-based record keeping, which can be tedious, incomplete, fragmented, erroneous and time-consuming. It will provide a single, integrated, shareable, up-to-date, accurate and easily accessible source of information, potentially available anywhere and anytime. It will require less space and administrative resources and has the potential to automate and streamline the flow of clinical information. It will provide integrated support for a wide range of healthcare activities including, monitoring, automatic reminders, electronic appointments and referrals, real-time communications and continuing pregnancy education and awareness. It will increase antenatal care visits through application reminders, enable access/calls to emergency obstetric care when complications arise, will improve referral communication and increase access to quality care. It will provide easy access to women’s clinical data and reduce medical errors.
None of the applications such as [
4,
21,
22,
23,
24] or applications that already exist on Microsoft, Google Play or Apple stores on maternal health issues have all four of the major functionalities of PCN (listed below).
There are four key areas that are the focus and strengths of PCN and that make it better than the already countless applications available on the Internet on different online application stores.