Norepinephrine Administration Is Associated with Higher Mortality in Dialysis Requiring Acute Kidney Injury Patients with Septic Shock
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Population
2.2. Data Collection and Variable Definitions
2.3. Statistical Analyses
2.4. Ethics Approval and Consent to Participate
3. Results
3.1. Baseline Characteristics of the Study Cohort
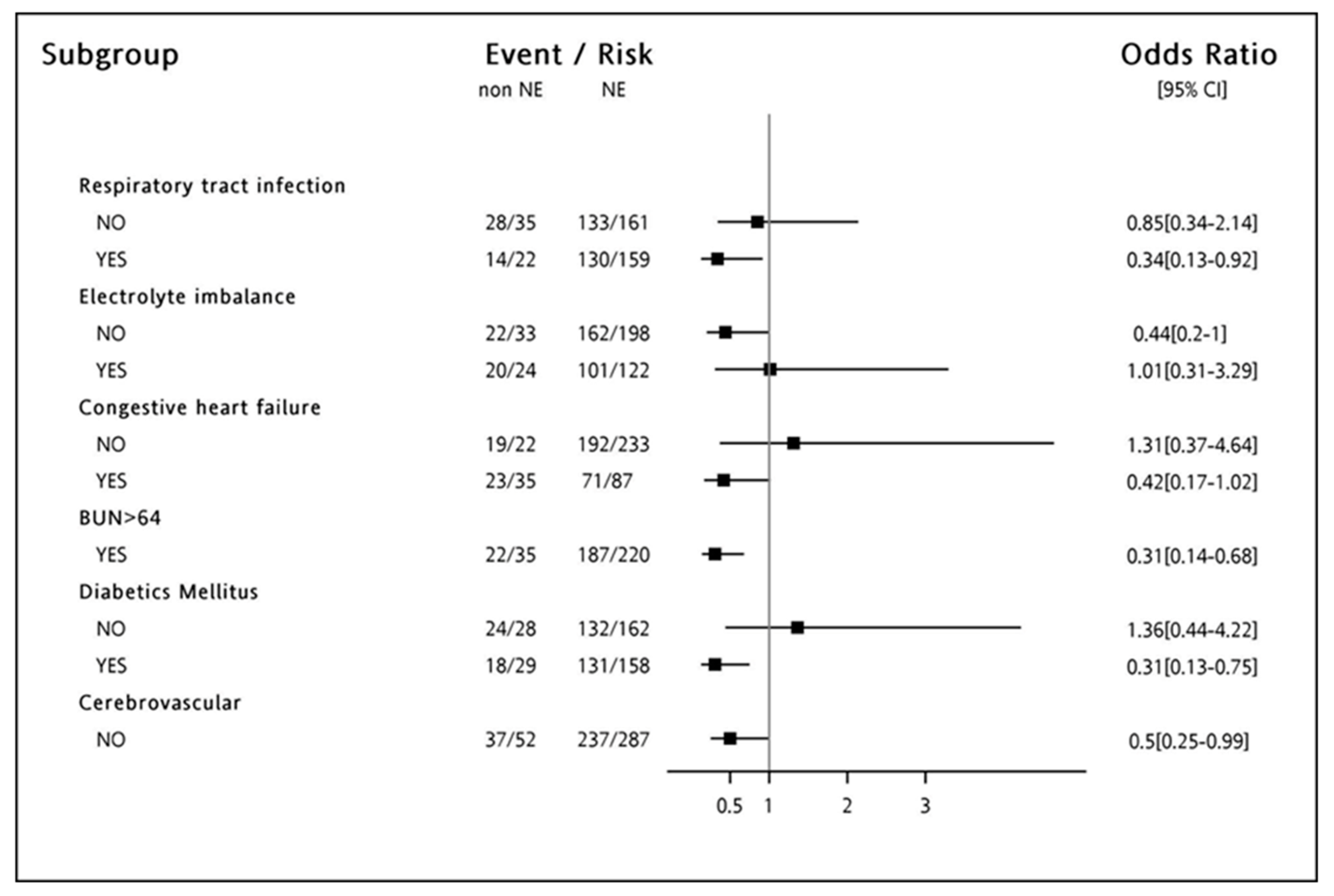
3.2. 90-Day Mortality in Septic-Shock-Related AKI-D
3.3. The Dose-Response Relationship between NE and 90-Day Mortality
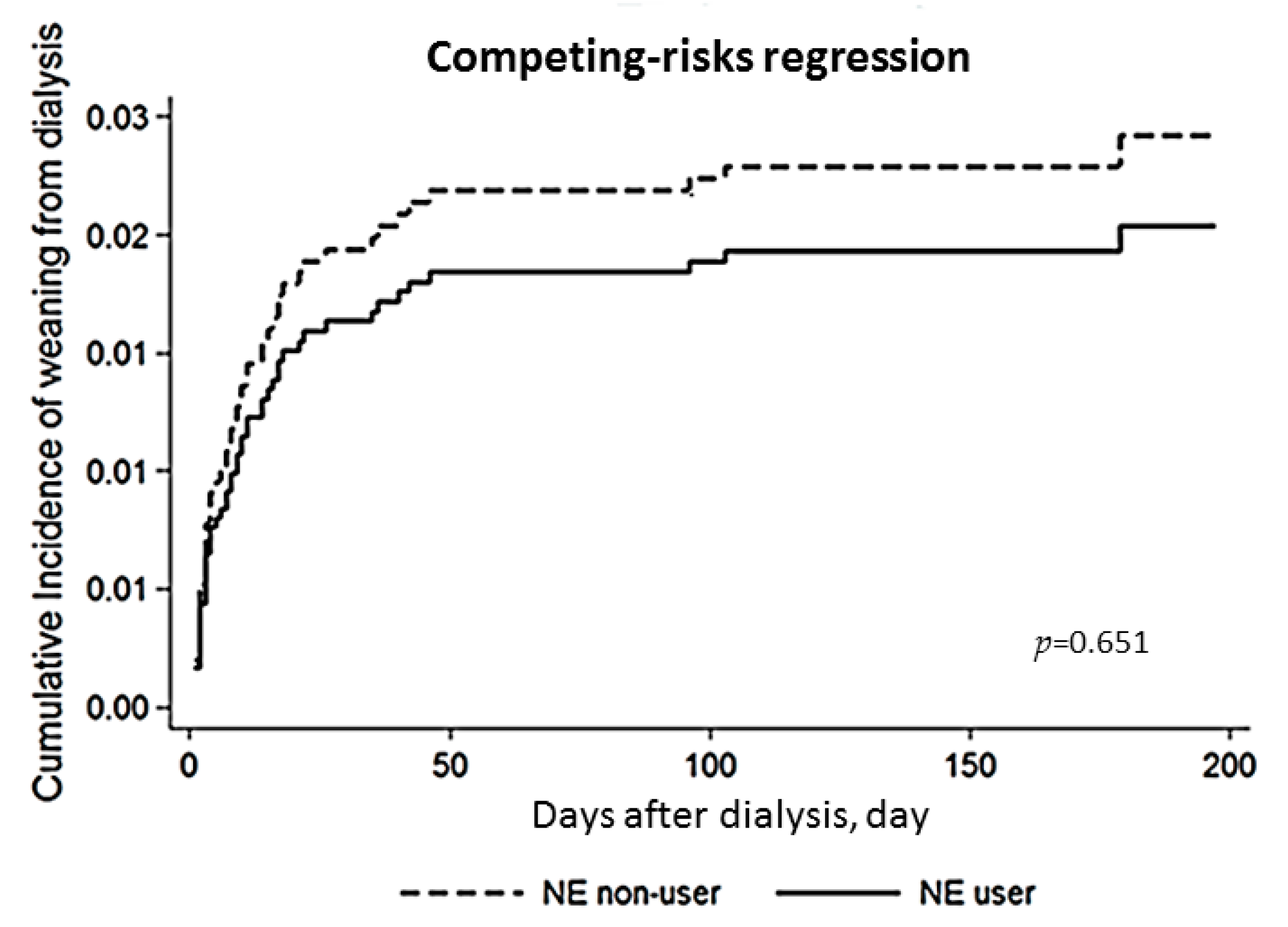
3.4. Dialysis Dependency in Septic Shock Patients with or without NE
4. Discussion
4.1. Main Finding
4.2. The Use of NE in AKI-D Patients with Septic Shock
4.3. NE and Renal Recovery
4.4. Study Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoste, E.A.; Bagshaw, S.M.; Bellomo, R.; Cely, C.M.; Colman, R.; Cruz, D.N.; Edipidis, K.; Forni, L.G.; Gomersall, C.D.; Govil, D.; et al. Epidemiology of acute kidney injury in critically ill patients: The multinational AKI-EPI study. Intensive Care Med. 2015, 41, 1411–1423. [Google Scholar] [CrossRef] [PubMed]
- Uchino, S.; Kellum, J.A.; Bellomo, R.; Doig, G.S.; Morimatsu, H.; Morgera, S.; Schetz, M.; Tan, I.; Bouman, C.; Macedo, E.; et al. Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA 2005, 294, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.; Dantes, R.; Epstein, L.; Murphy, D.J.; Seymour, C.W.; Iwashyna, T.J.; Kadri, S.S.; Angus, D.C.; Danner, R.L.; Fiore, A.E.; et al. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs. Claims Data, 2009-2014. JAMA 2017, 318, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- Bagshaw, S.M.; George, C.; Bellomo, R. Committee ADM: Early acute kidney injury and sepsis: A multicentre evaluation. Crit. Care 2008, 12, R47. [Google Scholar] [CrossRef] [PubMed]
- Thakar, C.V.; Christianson, A.; Freyberg, R.; Almenoff, P.; Render, M.L. Incidence and outcomes of acute kidney injury in intensive care units: A Veterans Administration study. Crit. Care Med. 2009, 37, 2552–2558. [Google Scholar] [CrossRef] [PubMed]
- Bagshaw, S.M.; Uchino, S.; Bellomo, R.; Morimatsu, H.; Morgera, S.; Schetz, M.; Tan, I.; Bouman, C.; Macedo, E.; Gibney, N.; et al. Septic acute kidney injury in critically ill patients: Clinical characteristics and outcomes. Clin. J. Am. Soc. Nephrol. 2007, 2, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Chawla, L.S.; Busse, L.; Brasha-Mitchell, E.; Davison, D.; Honiq, J.; Alotaibi, Z.; Seneff, M.G. Intravenous angiotensin II for the treatment of high-output shock (ATHOS trial): A pilot study. Crit. Care 2014, 18, 534. [Google Scholar] [CrossRef] [PubMed]
- Myburgh, J.A.; Higgins, A.; Jovanovska, A.; Lipman, J.; Ramakrishnan, N.; Santamaria, J. Investigators CATS: A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med. 2008, 34, 2226–2234. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef] [PubMed]
- Shiao, C.C.; Wu, P.C.; Wu, V.C.; Lin, J.H.; Pan, H.C.; Yang, Y.F.; Lai, T.S.; Huang, T.M.; Wu, C.H.; Yang, W.S.; et al. Nationwide epidemiology and prognosis of dialysis-requiring acute kidney injury (NEP-AKI-D) study: Design and methods. Nephrology (Carlton) 2016, 21, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Ko, W.J.; Chang, H.W.; Chen, Y.W.; Lin, Y.F.; Shiao, C.C.; Chen, Y.M.; Chen, Y.S.; Tsai, P.R.; Hu, F.C.; et al. Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med. 2008, 34, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Ko, W.J.; Chang, H.W.; Chen, Y.S.; Chen, Y.W.; Chen, Y.M.; Hu, F.C.; Lin, Y.H.; Tsai, P.R.; Wu, K.D. Early renal replacement therapy in patients with postoperative acute liver failure associated with acute renal failure: Effect on postoperative outcomes. J. Am. Coll. Surg. 2007, 205, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.S.; Ko, W.J.; Lin, F.Y.; Huang, S.C.; Chou, T.F.; Chou, N.K.; Hsu, R.B.; Wang, S.S.; Chu, S.H. Preliminary result of an algorithm to select proper ventricular assist devices for high-risk patients with extracorporeal membrane oxygenation support. J. Heart Lung Transplant. 2001, 20, 850–857. [Google Scholar] [CrossRef]
- Gaies, M.G.; Jeffries, H.E.; Niebler, R.A.; Pasquali, S.K.; Donohue, J.E.; Yu, S.; Gall, C.; Rice, T.B.; Thiagarajan, R.R. Vasoactive-inotropic score is associated with outcome after infant cardiac surgery: An analysis from the Pediatric Cardiac Critical Care Consortium and Virtual PICU System Registries. Pediatr. Crit. Care Med. 2014, 15, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Gaies, M.G.; Gurney, J.G.; Yen, A.H.; Napoli, M.L.; Gajarski, R.J.; Ohye, R.G.; Charpie, J.R.; Hirsch, J.C. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr. Crit. Care Med. 2010, 11, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Sharma, R.; Sethi, S.K.; Bazaz, S.; Sharma, P.; Bhan, A.; Kher, V. Vasoactive Inotrope Score as a tool for clinical care in children post cardiac surgery. Indian J. Crit. Care Med. 2014, 18, 653–658. [Google Scholar] [PubMed]
- McIntosh, A.M.; Tong, S.; Deakyne, S.J.; Davidson, J.A.; Scott, H.F. Validation of the Vasoactive-Inotropic Score in Pediatric Sepsis. Pediatr. Crit. Care Med. 2017, 18, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Hu, Y.H.; Wu, C.H.; Kao, C.C.; Wang, C.Y.; Yang, W.S.; Lee, H.H.; Chang, Y.S.; Lin, Y.H.; Wang, S.M.; et al. Administrative data on diagnosis and mineralocorticoid receptor antagonist prescription identified patients with primary aldosteronism in Taiwan. J. Clin. Epidemiol. 2014, 67, 1139–1149. [Google Scholar] [CrossRef] [PubMed]
- Roy, J.; Lum, K.J.; Daniels, M.J. A Bayesian nonparametric approach to marginal structural models for point treatments and a continuous or survival outcome. Biostatistics 2017, 18, 32–47. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Young, G.H.; Huang, P.H.; Lo, S.C.; Wang, K.C.; Sun, C.Y.; Liang, C.J.; Huang, T.M.; Chen, J.H.; Chang, F.C.; et al. In acute kidney injury, indoxyl sulfate impairs human endothelial progenitor cells: Modulation by statin. Angiogenesis 2013, 16, 609–624. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Huang, T.M.; Shiao, C.C.; Lai, C.F.; Tsai, P.R.; Wang, W.J.; Huang, H.Y.; Wang, K.C.; Ko, W.J.; Wu, K.D.; et al. The hemodynamic effects during sustained low-efficiency dialysis versus continuous veno-venous hemofiltration for uremic patients with brain hemorrhage: A crossover study. J. Neurosurg. 2013, 119, 1288–1295. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.H.; Yang, Y.W.; Hung, S.C.; Tsai, Y.C.; Hu, Y.H.; Lin, Y.H.; Chu, T.S.; Wu, K.D.; Wu, V.C. Effect of Treatment on Body Fluid in Patients with Unilateral Aldosterone Producing Adenoma: Adrenalectomy versus Spironolactone. Sci. Rep. 2015, 5, 15297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, V.C.; Chang, C.H.; Wang, C.Y.; Lin, Y.H.; Kao, T.W.; Lin, P.C.; Chu, T.S.; Chang, Y.S.; Chen, L.; Wu, K.D.; et al. Risk of Fracture in Primary Aldosteronism: A Population-Based Cohort Study. J. Bone Miner. Res. 2017, 32, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Chueh, S.J.; Chen, L.; Chang, C.H.; Hu, Y.H.; Lin, Y.H.; Wu, K.D.; Yang, W.S.; Group, T.S. Risk of new-onset diabetes mellitus in primary aldosteronism: A population study over 5 years. J. Hypertens. 2017, 35, 1698–1708. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. Variance estimation when using inverse probability of treatment weighting (IPTW) with survival analysis. Stat. Med. 2016, 35, 5642–5655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dellinger, R.P.; Levy, M.M.; Rhodes, A.; Annane, D.; Gerlach, H.; Opal, S.M.; Sevransky, J.E.; Sprung, C.L.; Douglas, I.S.; Jaeschke, R.; et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013, 39, 165–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, C.Y.; Yeh, H.C.; Chen, W.; Liu, J.H.; Lin, H.H.; Liu, Y.L.; Yang, Y.F.; Wang, S.M.; Huang, C.C. Norepinephrine and hospital mortality in critically ill patients undergoing continuous renal replacement therapy. Artif. Organs 2011, 35, E11–E17. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.; Dusang, B.; Annane, D.; Gibot, S.; Bollaert, P.E. College Interregional des Reanimateurs du N-E: Cardiovascular response to dopamine and early prediction of outcome in septic shock: A prospective multiple-center study. Crit. Care Med. 2005, 33, 2172–2177. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.C.; Russell, J.A.; Walley, K.R.; Singer, J.; Ayers, D.; Storms, M.M.; Holmes, C.L.; Hebert, P.C.; Cooper, D.J.; Mehta, S.; et al. The effects of vasopressin on acute kidney injury in septic shock. Intensive Care Med. 2010, 36, 83–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, J.A.; Walley, K.R.; Singer, J.; Gordon, A.C.; Hebert, P.C.; Cooper, D.J.; Holmes, C.L.; Mehta, S.; Granton, J.T.; Storms, M.M.; et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N. Engl. J. Med. 2008, 358, 877–887. [Google Scholar] [CrossRef] [PubMed]
- da Hora Passos, R.; Ramos, J.G.; Mendonca, E.J.; Miranda, E.A.; Dutra, F.R.; Coelho, M.F.; Pedroza, A.C.; Correia, L.C.; Batista, P.B.; Macedo, E.; et al. A clinical score to predict mortality in septic acute kidney injury patients requiring continuous renal replacement therapy: The HELENICC score. BMC Anesthesiol. 2017, 17, 21. [Google Scholar] [CrossRef] [PubMed]
- Povoa, P.R.; Carneiro, A.H.; Ribeiro, O.S.; Pereira, A.C. Portuguese Community-Acquired Sepsis Study G: Influence of vasopressor agent in septic shock mortality. Results from the Portuguese Community-Acquired Sepsis Study (SACiUCI study). Crit. Care Med. 2009, 37, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Gerlach, H. Fluid resuscitation in severe sepsis and septic shock: An evidence-based review. Crit. Care Med. 2004, 32 (Suppl. 11), S451–S454. [Google Scholar] [CrossRef] [PubMed]
- Abou Dagher, G.; Harmouche, E.; Jabbour, E.; Bachir, R.; Zebian, D.; Bou Chebl, R. Sepsis in hemodialysis patients. BMC Emerg. Med. 2015, 15, 30. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, F.L.; Bota, D.P.; Bross, A.; Melot, C.; Vincent, J.L. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 2001, 286, 1754–1758. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.; Viviand, X.; Leone, M.; Thirion, X. Effect of norepinephrine on the outcome of septic shock. Crit. Care Med. 2000, 28, 2758–2765. [Google Scholar] [CrossRef] [PubMed]
- De Backer, D.; Biston, P.; Devriendt, J.; Madl, C.; Chochrad, D.; Aldecoa, C.; Brasseur, A.; Defrance, P.; Gottignies, P.; Vincent, J.L.; et al. Comparison of dopamine and norepinephrine in the treatment of shock. N. Engl. J. Med. 2010, 362, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.C.; Mason, A.J.; Thirunavukkarasu, N.; Perkins, G.D.; Cecconi, M.; Cepkova, M.; Pogson, D.G.; Aya, H.D.; Anjum, A.; Frazier, G.J.; et al. Effect of Early Vasopressin vs. Norepinephrine on Kidney Failure in Patients With Septic Shock: The VANISH Randomized Clinical Trial. JAMA 2016, 316, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Richer, M.; Robert, S.; Lebel, M. Renal hemodynamics during norepinephrine and low-dose dopamine infusions in man. Crit. Care Med. 1996, 24, 1150–1156. [Google Scholar] [CrossRef] [PubMed]
- Cronin, R.E.; Erickson, A.M.; de Torrente, A.; McDonald, K.M.; Schrier, R.W. Norepinephrine-induced acute renal failure: A reversible ischemic model of acute renal failure. Kidney Int. 1978, 14, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Lankadeva, Y.R.; Kosaka, J.; Evans, R.G.; Bailey, S.R.; Bellomo, R.; May, C.N. Intrarenal and urinary oxygenation during norepinephrine resuscitation in ovine septic acute kidney injury. Kidney Int. 2016, 90, 100–108. [Google Scholar] [CrossRef] [PubMed]

| Variables | Before IPTW | After IPTW | ||||
|---|---|---|---|---|---|---|
| NE Non-User (n = 57) | NE User (n = 315) | p * Value | NE Non-User (n = 57) | NE User (n = 315) | p * Value | |
| Age (year) | 65.79 ± 15.22 | 64.77 ± 15.72 | 0.637 | 66.56 ± 14.53 | 64.66 ± 15.95 | 0.587 |
| Gender (male) | 36 (63.16%) | 224 (71.11%) | 0.272 | 21 (31.11%) | 91 (29.82%) | 0.797 |
| DM | 29 (50.88%) | 155 (49.21%) | 0.886 | 29 (47.73%) | 155 (50.00%) | 0.772 |
| CAD | 17 (29.82%) | 65 (20.63%) | 0.163 | 17 (22.22%) | 65 (22.59%) | 0.946 |
| CVA | 5 (8.77%) | 33 (10.48%) | 0.816 | 5 (11.11%) | 33 (16.27%) | 0.293 |
| CHF | ||||||
| I | 13 (22.81%) | 3 (5.26%) | <0.001 | 13 (31.11%) | 3 (41.99%) | 0.551 |
| II | 12 (21.05%) | 153 (48.57%) | 12 (28.89%) | 153 (22.66%) | ||
| III | 12 (21.05%) | 68 (21.59%) | 12 (26.67%) | 68 (16.92%) | ||
| IV | 17 (29.82%) | 59 (18.73%) | 17 (11.11%) | 59 (10.57%) | ||
| BUN (mg/dL) | 57.59 ± 47.42 | 50.19 ± 40.14 | 0.225 | 51.01 ± 49.62 | 50.19 ± 39.48 | 0.700 |
| Lactate(mmol/L) | 10.65 ± 9.03 | 8.77 ± 6.98 | 0.160 | 9.14 ± 8 | 9.62 ± 7.36 | 0.734 |
| Baseline Cr (mg/dL) | 1.62 ± 1.16 | 1.36 ± 1.02 | 0.074 | 1.65 ± 1.18 | 1.37 ± 1.03 | 0.254 |
| eGFR (mL/min/1.73 m2) | 57.03 ± 35.28 | 69.63 ± 46.76 | 0.048 | 57.34 ± 36.15 | 68.12 ± 44.9 | 0.319 |
| Etiology of AKI | ||||||
| Shock | 29 (50.88%) | 242 (76.83%) | <0.001 | 29 (60.00%) | 242 (68.37%) | 0.306 |
| CRS | 34 (59.65%) | 82 (26.03%) | <0.001 | 34 (35.56%) | 82 (33.13%) | 0.663 |
| Drug | 2 (3.51%) | 21 (6.67%) | 0.551 | 2 (8.89%) | 21 (5.72%) | 0.363 |
| Rhabdomyolysis | 4 (7.02%) | 43 (13.65%) | 0.198 | 4 (4.44%) | 43 (13.86%) | 0.054 |
| Pigmentation | 0 (0.00%) | 14 (4.44%) | 0.140 | 0 (0.00%) | 14 (6.02%) | 0.092 |
| Hepatorenal | 4 (7.02%) | 23 (7.30%) | 0.999 | 4 (8.89%) | 23 (6.93%) | 0.648 |
| Contrast | 4 (7.02%) | 24 (7.62%) | 0.999 | 4 (11.11%) | 24 (10.54%) | 0.956 |
| Others | 4 (7.02%) | 33 (10.48%) | 0.630 | 4 (4.44%) | 33 (9.04%) | 0.299 |
| Infection site | ||||||
| Respiratory | 22 (38.60%) | 157 (49.84%) | 0.149 | 22 (46.67%) | 157 (46.08%) | 0.999 |
| GU | 19 (33.33%) | 77 (24.44%) | 0.188 | 19 (20.00%) | 77 (22.36%) | 0.738 |
| Bacteremia | 12 (21.05%) | 96 (30.48%) | 0.204 | 12 (26.67%) | 96 (28.61%) | 0.903 |
| Abdomen | 3 (5.26%) | 53 (16.83%) | 0.026 | 3 (6.67%) | 53 (14.16%) | 0.157 |
| Others | 6 (10.53%) | 39 (12.38%) | 0.827 | 6 (8.89%) | 39 (12.95%) | 0.435 |
| Disease severity score | ||||||
| Total IE Score | 13.97 ± 14.11 | 31.99 ± 25.36 | <0.001 | 24.23 ± 23.62 | 29.17 ± 24.21 | 0.261 |
| SIRS | 2.7 ± 0.89 | 2.92 ± 0.83 | 0.080 | 2.87 ± 0.95 | 2.87 ± 0.81 | 0.822 |
| SOFA | 14.02 ± 2.66 | 15.6 ± 2.96 | <0.001 | 15.42 ± 2.69 | 15.28 ± 2.99 | 0.663 |
| qSOFA | 2.3 ± 0.46 | 2.37 ± 0.48 | 0.311 | 2.25 ± 0.45 | 2.35 ± 0.48 | 0.300 |
| APACHEII | 25.79 ± 7.57 | 27.27 ± 6.46 | 0.289 | 26.51 ± 6.74 | 27.21 ± 6.49 | 0.851 |
| Outcome | ||||||
| ICU day | 28.65 ± 38.07 | 17.22 ± 17.88 | 0.014 | 30.94 ± 37.27 | 17.58 ± 18.32 | 0.204 |
| Length of hospital dialysis | 26.07 ± 36.97 | 12.68 ± 19.19 | <0.001 | 18.67 ± 27.78 | 12.85 ± 19.47 | 0.012 |
| Hospital Mortality | 41 (71.93%) | 252 (80.00%) | 0.217 | 41 (75.56%) | 252 (81.02%) | 0.330 |
| 90-day outcome | 0.142 | 0.753 | ||||
| Mortality | 42 (73.68%) | 260 (82.54%) | 42 (76.09%) | 260 (83.13%) | ||
| Recovery from dialysis | 13 (22.81%) | 52 (16.51%) | 13 (21.74%) | 52 (15.66%) | ||
| Dialysis-dependent | 2 (3.51%) | 3 (0.95%) | 2 (2.17%) | 3 (1.20%) | ||
| Variables | HR | Lower 95% CI | 95% CI | p |
|---|---|---|---|---|
| NE user (yes) | 1.497 | 1.046 | 2.141 | 0.027 |
| Hepatorenal syndrome (yes) | 1.992 | 1.320 | 3.007 | 0.001 |
| Cr (mg/dL) | 0.840 | 0.776 | 0.910 | <0.001 |
| BUN (mg/dL) | 1.008 | 1.004 | 1.012 | <0.001 |
| APACHEII Score | 1.042 | 1.030 | 1.836 | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-Y.; Wu, V.-C.; Huang, W.-C.; Yeh, Y.-C.; Wu, M.-S.; Huang, C.-C.; Wu, K.-D.; Fang, J.-T.; Wu, C.-J.; The NSARF; et al. Norepinephrine Administration Is Associated with Higher Mortality in Dialysis Requiring Acute Kidney Injury Patients with Septic Shock. J. Clin. Med. 2018, 7, 274. https://doi.org/10.3390/jcm7090274
Chen Y-Y, Wu V-C, Huang W-C, Yeh Y-C, Wu M-S, Huang C-C, Wu K-D, Fang J-T, Wu C-J, The NSARF, et al. Norepinephrine Administration Is Associated with Higher Mortality in Dialysis Requiring Acute Kidney Injury Patients with Septic Shock. Journal of Clinical Medicine. 2018; 7(9):274. https://doi.org/10.3390/jcm7090274
Chicago/Turabian StyleChen, Ying-Ying, Vin-Cent Wu, Wei-Chieh Huang, Yu-Chang Yeh, Mai-Szu Wu, Chiu-Ching Huang, Kwan-Dun Wu, Ji-Tseng Fang, Chih-Jen Wu, The NSARF, and et al. 2018. "Norepinephrine Administration Is Associated with Higher Mortality in Dialysis Requiring Acute Kidney Injury Patients with Septic Shock" Journal of Clinical Medicine 7, no. 9: 274. https://doi.org/10.3390/jcm7090274





