Simple Scores of Fibrosis and Mortality in Patients with NAFLD: A Systematic Review with Meta-Analysis
Abstract
:1. Introduction
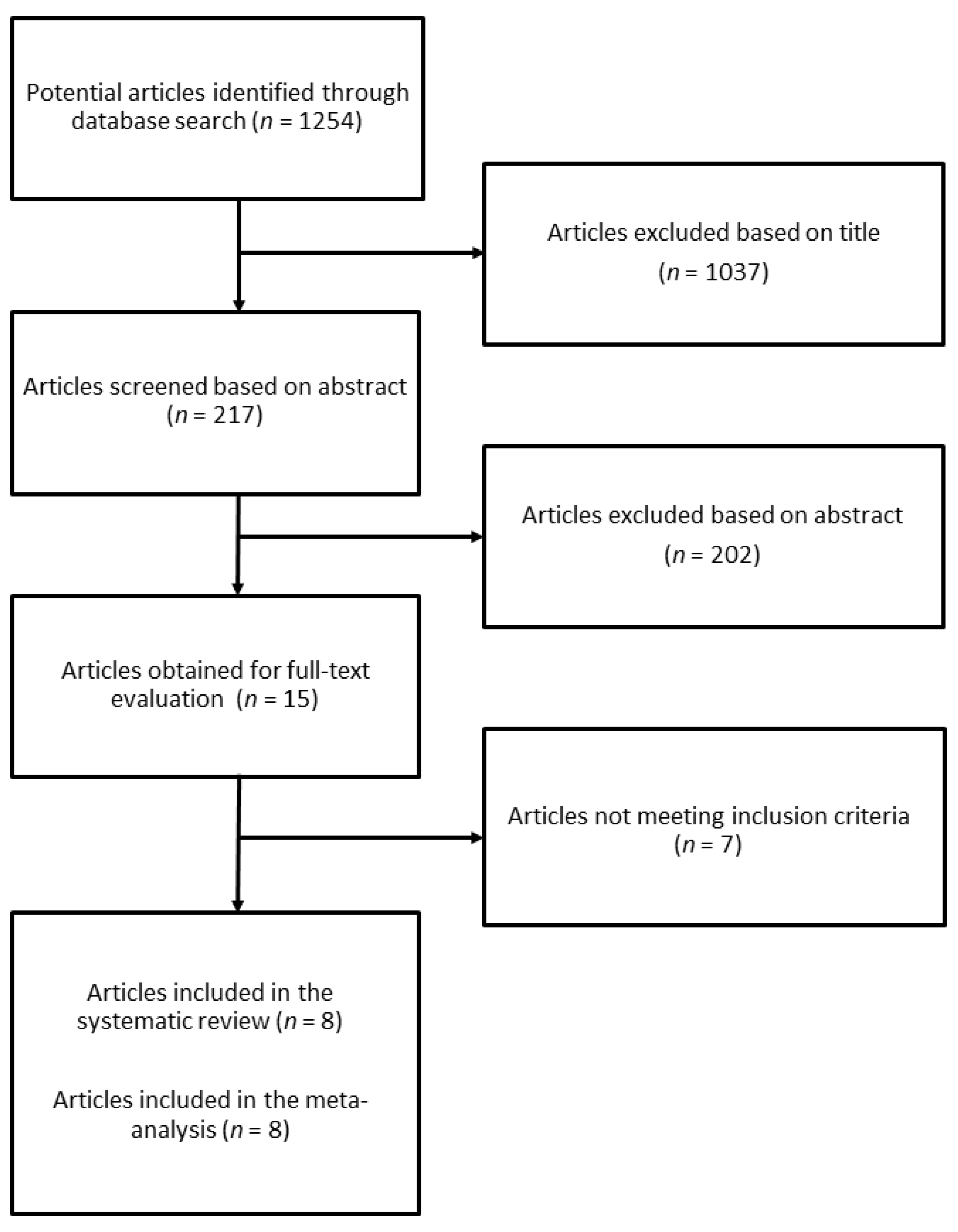
2. Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Statistical Analysis
3. Results
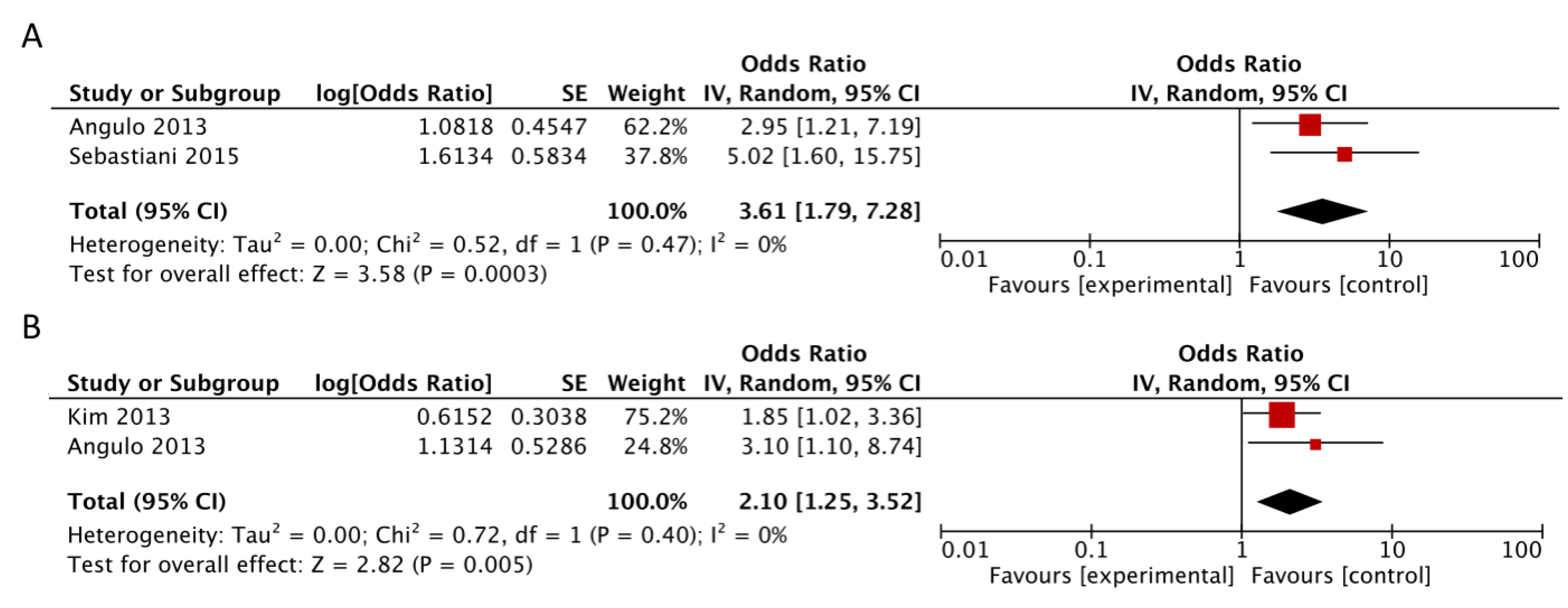
3.1. NAFLD Fibrosis Score
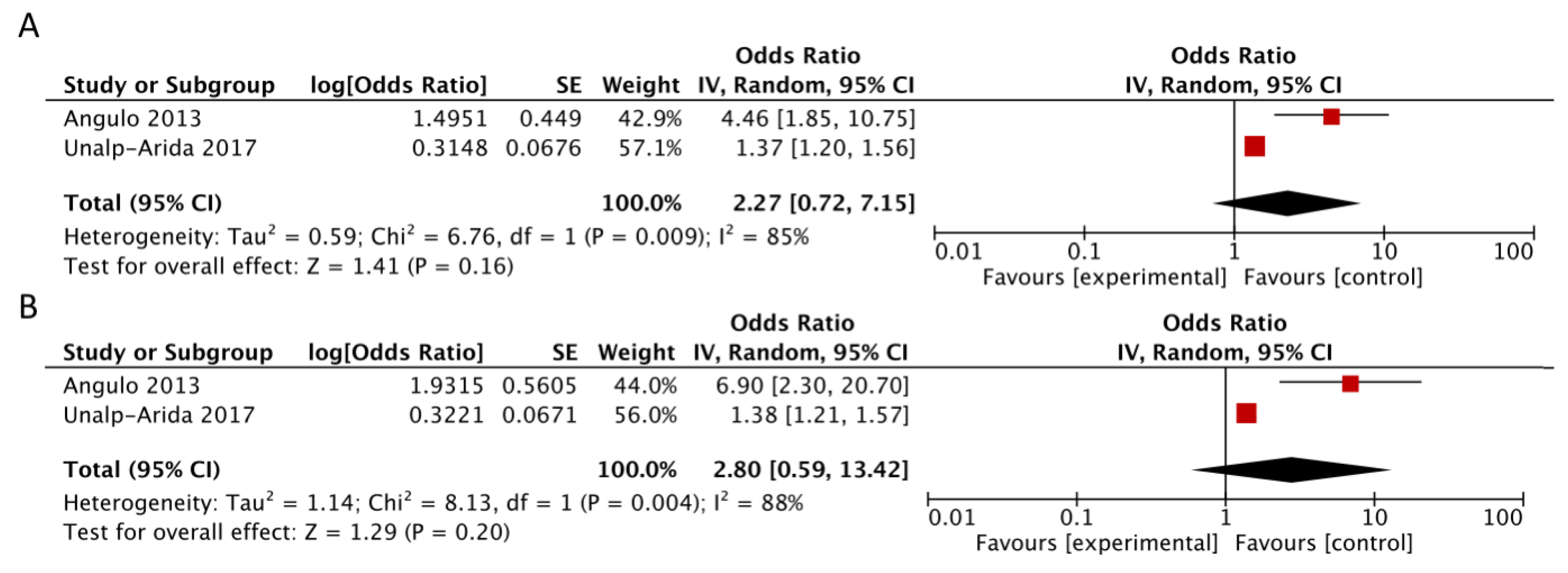
3.2. APRI and FIB4
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; George, J.; Bugianesi, E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Dulai, P.S.; Singh, S.; Patel, J.; Soni, M.; Prokop, L.J.; Younossi, Z.; Sebastiani, G.; Ekstedt, M.; Hagstrom, H.; Nasr, P.; et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology 2017, 65, 1557–1565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American association for the study of liver diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver; European Association for the Study of Diabetes; European Association for the Study of Obesity. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef] [PubMed]
- Vilar-Gomez, E.; Chalasani, N. Non-invasive assessment of non-alcoholic fatty liver disease: Clinical prediction rules and blood-based biomarkers. J. Hepatol. 2018, 68, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R. Role of imaging-based biomarkers in NAFLD: Recent advances in clinical application and future research directions. J. Hepatol. 2018, 68, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P.; Hui, J.M.; Marchesini, G.; Bugianesi, E.; George, J.; Farrell, G.C.; Enders, F.; Saksena, S.; Burt, A.D.; Bida, J.P.; et al. The nafld fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007, 45, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Xiao, G.; Zhu, S.; Xiao, X.; Yan, L.; Yang, J.; Wu, G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology 2017, 66, 1486–1501. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, W.R.; Kim, H.J.; Therneau, T.M. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology 2013, 57, 1357–1365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treeprasertsuk, S.; Bjornsson, E.; Enders, F.; Suwanwalaikorn, S.; Lindor, K.D. Nafld fibrosis score: A prognostic predictor for mortality and liver complications among NAFLD patients. World J. Gastroenterol. 2013, 19, 1219–1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angulo, P.; Bugianesi, E.; Bjornsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Barrera, F.; Haflidadottir, S.; Day, C.P.; George, J. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2013, 145, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Xun, Y.H.; Guo, J.C.; Lou, G.Q.; Jiang, Y.M.; Zhuang, Z.J.; Zhu, M.F.; Luo, Y.; Ma, X.J.; Liu, J.; Bian, D.X.; et al. Non-alcoholic fatty liver disease (NAFLD) fibrosis score predicts 6.6-year overall mortality of chinese patients with NAFLD. Clin. Exp. Pharmacol. Physiol. 2014, 41, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Sebastiani, G.; Alshaalan, R.; Wong, P.; Rubino, M.; Salman, A.; Metrakos, P.; Deschenes, M.; Ghali, P. Prognostic value of non-invasive fibrosis and steatosis tools, hepatic venous pressure gradient (hvpg) and histology in nonalcoholic steatohepatitis. PLoS ONE 2015, 10, e0128774. [Google Scholar] [CrossRef] [PubMed]
- Unalp-Arida, A.; Ruhl, C.E. Liver fibrosis scores predict liver disease mortality in the United States population. Hepatology 2017, 66, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Le, M.H.; Devaki, P.; Ha, N.B.; Jun, D.W.; Te, H.S.; Cheung, R.C.; Nguyen, M.H. Prevalence of non-alcoholic fatty liver disease and risk factors for advanced fibrosis and mortality in the United States. PLoS ONE 2017, 12, e0173499. [Google Scholar] [CrossRef] [PubMed]
- Yoshihisa, A.; Sato, Y.; Yokokawa, T.; Sato, T.; Suzuki, S.; Oikawa, M.; Kobayashi, A.; Yamaki, T.; Kunii, H.; Nakazato, K.; et al. Liver fibrosis score predicts mortality in heart failure patients with preserved ejection fraction. ESC Heart Fail. 2017, 5, 262–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Available online: www.prisma-statement.org (accessed on 14 August 2018).
- Orsini, N.; Li, R.; Wolk, A.; Khudyakov, P.; Spiegelman, D. Meta-analysis for linear and nonlinear dose-response relations: Examples, an evaluation of approximations, and software. Am. J. Epidemiol. 2012, 175, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Wai, C.T.; Greenson, J.K.; Fontana, R.J.; Kalbfleisch, J.D.; Marrero, J.A.; Conjeevaram, H.S.; Lok, A.S. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003, 38, 518–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J.; Nash Clinical Research, N. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Maida, M.; Macaluso, F.S.; Salomone, F.; Petta, S. Non-invasive assessment of liver injury in non-alcoholic fatty liver disease: A review of literature. Curr. Mol. Med. 2016, 16, 721–737. [Google Scholar] [CrossRef] [PubMed]
- Guha, I.N.; Parkes, J.; Roderick, P.; Chattopadhyay, D.; Cross, R.; Harris, S.; Kaye, P.; Burt, A.D.; Ryder, S.D.; Aithal, G.P.; et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: Validating the European liver fibrosis panel and exploring simple markers. Hepatology 2008, 47, 455–460. [Google Scholar] [CrossRef] [PubMed]


| Author, Year, Country | Cohort, Study Design | Number of Participants | Age | Male Gender | Follow-up Duration | NAFLD Diagnosis |
|---|---|---|---|---|---|---|
| Kim, 2013, USA | Population-based, prospective | 4081 NAFLD individuals with available APRI, FIB-4, NFS | 45.5 years (mean) | 50.3% | 14.5 years (median) | Ultrasonography |
| Treeprasertsuk, 2013, USA | Community-based, retrospective | 302 NAFLD individuals with available NFS | 47.3 years (mean) | 44% | 12 years (mean) | Liver biopsy |
| Angulo, 2013, Multi-country | Hospital-based, multicenter, retrospective | 320 NAFLD individuals with available APRI, FIB-4, NFS | 52 years (median) | 43% | 8.7 years (104.8 months) (median) | Liver biopsy |
| Xun, 2014, China | Hospital-based single center, retrospective | 180 NAFLD individuals with available APRI, FIB-4, NFS | 39 years (median) | 53.3% | 6.6 years (median) | Ultrasonography |
| Sebastiani, 2015, Canada | Hospital-based single center, retrospective cohort | 148 NAFLD individuals with available NFS | 49.5 years (mean) | 69.6% | 5 years (median) | Liver biopsy |
| Unalp-Arida, 2017, USA | Population-based, prospective | 14841 individuals for APRI and FIB-4, 14741 for NFS | NA | NA | 19.3 years (median) | Negative for viral hepatitis markers |
| Le, 2017, USA | Population-based, prospective | 1936 NAFLD individuals with available NFS | 53.2 years (mean) | 59.2% | 13 years (up to) | United States Fatty Liver Index (USFLI) |
| Yoshihisa, 2017, Japan | Hospital-based single center, prospective | 492 patients with heart failure and preserved ejection fraction | NA | NA | 3.0 years (1096 days) (mean) | Not assessed |
| Subgroup | No. of Studies | RR (95% CI) | I2 | Pheterogeneity |
|---|---|---|---|---|
| Total | 6 | 3.85 (2.08, 7.11) | 92% | <0.00001 |
| Study design | ||||
| Prospective | 2 | 2.70 (0.98, 7.44) | 98% | <0.00001 |
| Retrospective | 4 | 4.72 (2.50, 8.93) | 55% | 0.08 |
| Geographical location | ||||
| North America | 4 | 3.88 (1.80, 8.37) | 95% | <0.00001 |
| Asia | 1 | 7.00 (2.46, 19.92) | NA | NA |
| Multicountry | 1 | 2.39 (1.20–4.76) | NA | NA |
| Liver biopsy | ||||
| Yes | 3 | 4.33 (1.99, 9.43) | 64% | 0.06 |
| No | 3 | 3.43 (1.42, 8.28) | 96% | <0.00001 |
| Adjustment for confounding factors | ||||
| Yes | 3 | 4.45 (2.35, 8.43) | 67% | 0.05 |
| No | 3 | 3.23 (1.32, 7.91) | 85% | 0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salomone, F.; Micek, A.; Godos, J. Simple Scores of Fibrosis and Mortality in Patients with NAFLD: A Systematic Review with Meta-Analysis. J. Clin. Med. 2018, 7, 219. https://doi.org/10.3390/jcm7080219
Salomone F, Micek A, Godos J. Simple Scores of Fibrosis and Mortality in Patients with NAFLD: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2018; 7(8):219. https://doi.org/10.3390/jcm7080219
Chicago/Turabian StyleSalomone, Federico, Agnieszka Micek, and Justyna Godos. 2018. "Simple Scores of Fibrosis and Mortality in Patients with NAFLD: A Systematic Review with Meta-Analysis" Journal of Clinical Medicine 7, no. 8: 219. https://doi.org/10.3390/jcm7080219






