Primary Signet Ring Cell Carcinoma of the Prostate: A Rare Case Report
Abstract
:1. Introduction
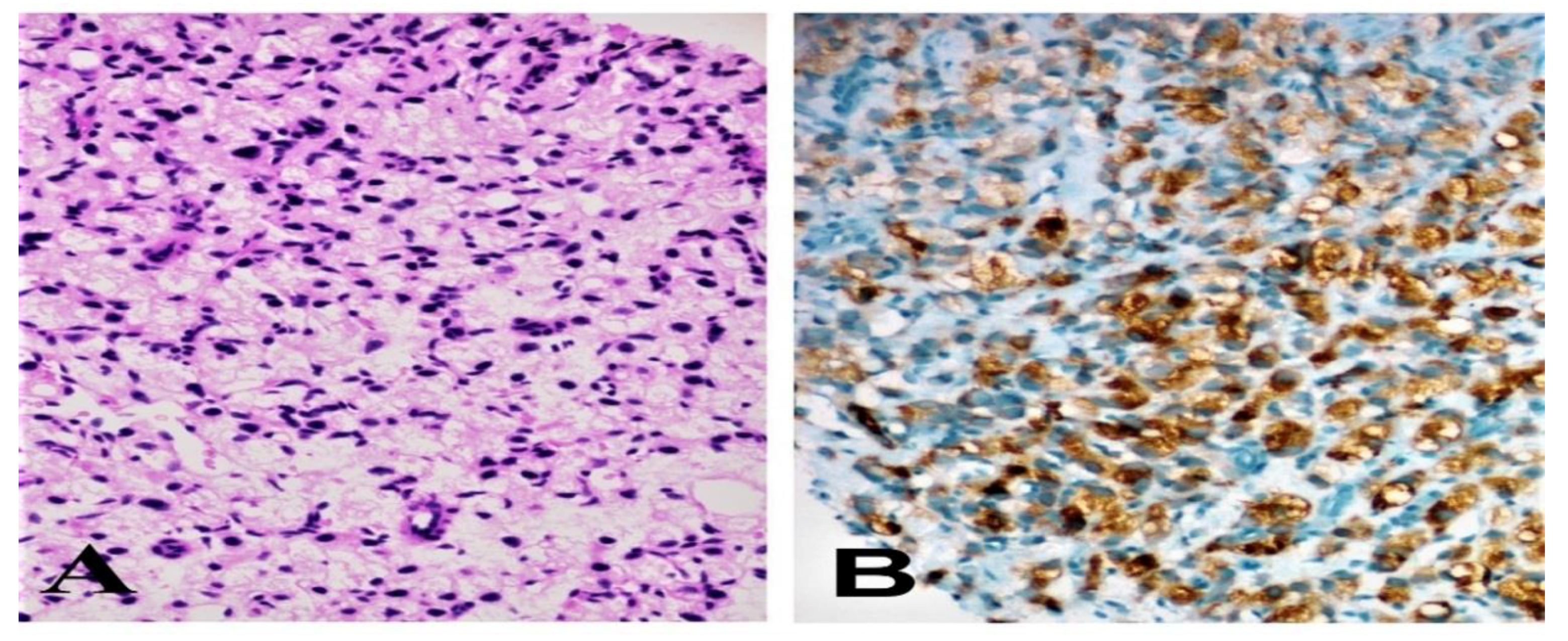
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Warner, J.N.; Nakamura, L.Y.; Pacelli, A.; Humphreys, M.R.; Castle, E.P. Primary signet ring cell carcinoma of the prostate. Mayo Clin. Proc. 2010, 85, 1130–1136. [Google Scholar] [CrossRef] [PubMed]
- Fujita, K.; Sugao, H.; Gotoh, T.; Yokomizo, S.; Itoh, Y. Primary signet ring cell carcinoma of the prostate: Report and review of 42 cases. Int. J. Urol. 2004, 11, 178–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Randolph, T.L.; Amin, M.B.; Ro, J.Y.; Ayala, A.G. Histologic variants of adenocarcinoma and other carcinomas of prostate: Pathologic criteria and clinical significance. Mod. Pathol. 1997, 10, 612–629. [Google Scholar] [PubMed]
- Ro, J.Y.; el-Naggar, A.; Ayala, A.G.; Mody, D.R.; Ordonez, N.G. Signet-ring-cell carcinoma of the prostate. Electron-microscopic and immunohistochemical studies of eight cases. Am. J. Surg. Pathol. 1988, 12, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Torbenson, M.; Dhir, R.; Nangia, A.; Becich, M.J.; Kapadia, S.B. Prostatic carcinoma with signet ring cells: A clinicopathologic and immunohistochemical analysis of 12 cases, with review of the literature. Mod. Pathol. 1998, 11, 552–559. [Google Scholar] [PubMed]
- Guerin, D.; Hasan, N.; Keen, C.E. Signet ring cell differentiation in adenocarcinoma of the prostate: A study of five cases. Histopathology 1993, 22, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Saito, S.; Iwaki, H. Mucin-producing carcinoma of the prostate: Review of 88 cases. Urology 1999, 54, 141–144. [Google Scholar] [CrossRef]
- Roldan, A.M.; Nunez, N.F.; Grande, E.; Garcia, A.A.; Anton-Aparicio, L.M. A primary signet ring cell carcinoma of the prostate with bone metastasis with impressive response to FOLFOX and cetuximab. Clin. Genitourin. Cancer 2012, 10, 199–201. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, K.; Fukui, I.; Ishikawa, Y.; Maeda, H.; Yamauchi, T.; Kawai, T. Locally-confined signet-ring cell carcinoma of the prostate: A case report of a long-term survivor. Int. J. Urol. 1996, 3, 406–407. [Google Scholar] [CrossRef] [PubMed]
- Lilleby, W.; Axcrona, K.; Alfsen, G.C.; Urnes, T.; Hole, K.H. Diagnosis and treatment of primary signet-ring cell carcinoma of the prostate. Acta Oncol. 2007, 46, 1195–1197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gök, A.; Tuygun, C.; Akmansu, M.; Uslu, A.A.; Kartal, I.G.; Sandikçi, F.; Karabacak, O.R.; Sağnak, A.L.; Topaloğlu, H.; Ersoy, H. Primary Signet Ring Cell Carcinoma of the Prostate: A Rare Case Report. J. Clin. Med. 2018, 7, 218. https://doi.org/10.3390/jcm7080218
Gök A, Tuygun C, Akmansu M, Uslu AA, Kartal IG, Sandikçi F, Karabacak OR, Sağnak AL, Topaloğlu H, Ersoy H. Primary Signet Ring Cell Carcinoma of the Prostate: A Rare Case Report. Journal of Clinical Medicine. 2018; 7(8):218. https://doi.org/10.3390/jcm7080218
Chicago/Turabian StyleGök, Alper, Can Tuygun, Müge Akmansu, Ayşegül Aksakal Uslu, Ibrahim Güven Kartal, Fatih Sandikçi, Osman Raif Karabacak, Azmi Levent Sağnak, Hikmet Topaloğlu, and Hamit Ersoy. 2018. "Primary Signet Ring Cell Carcinoma of the Prostate: A Rare Case Report" Journal of Clinical Medicine 7, no. 8: 218. https://doi.org/10.3390/jcm7080218




