Knowledge and Educational Needs about Pre-Implantation Genetic Diagnosis (PGD) among Oncology Nurses
Abstract
:1. Introduction
1.1. Background on PGD
1.2. Patient and Family Attitudes toward PGD
1.3. Nurses Involvement with PGD
1.4. Importance of Studying Nurse Knowledge and Needs for Education
1.5. Study Aims
2. Experimental Section
2.1. Participants and Recruitment Procedures
2.2. Measures
2.3. Procedures
2.4. Data Analysis
3. Results and Discussion
3.1. Participant Demographics
| Gender | Total |
|---|---|
| Male | 13 |
| Female | 188 |
| Age | |
| 25 or under | 4 |
| 26–35 | 33 |
| 36–45 | 47 |
| 46–55 | 64 |
| 56–65 | 44 |
| 66 or above | 4 |
| Ethnicity | |
| White | 175 |
| Black or African American | 6 |
| Asian | 5 |
| More than one race | 6 |
| Other | 5 |
| Prefer not to respond | 4 |
| Education | Total |
| BSN | 83 |
| Associates Degree | 72 |
| MSN | 25 |
| Diploma | 14 |
| Other | 1 |
| Inpatient or Outpatient | |
| Outpatient | 102 |
| Inpatient | 77 |
| Clinic Type | |
| Breast | 12 |
| Hematology | 9 |
| Infusion Center | 8 |
| Gastrointestinal | 6 |
| Gynecology | 5 |
| Radiation Oncology | 5 |
| Thoracic | 4 |
| Genitourinary | 3 |
| Neuro | 2 |
| Other | 41 |
| Religion | |
| Catholic | 81 |
| Atheist/Agnostic | 63 |
| Protestant (Baptist, Presbyterian, etc.) | 8 |
| Islamic | 3 |
| Prefer not to respond | 23 |
| Other | 22 |
3.2. Knowledge and Awareness
| Prior to this survey, have you ever heard of preimplantation genetic diagnosis? | ||||
|---|---|---|---|---|
| Aware | Not Aware | Total * | ||
| Gender (p = 0.276) | Male | 1 | 12 | 13 |
| Female | 36 | 144 | 180 | |
| Total | 37 | 156 | 193 | |
| Ethnicity (p = 0.123) | Hispanic or Latino | 1 | 17 | 18 |
| Not Hispanic or Latino | 36 | 139 | 175 | |
| Total | 37 | 156 | 193 | |
| Race (p = 0.817) | Caucasian | 33 | 137 | 170 |
| Not Caucasian | 4 | 19 | 23 | |
| Total | 37 | 156 | 193 | |
| Education (p = 0.191) | AA/Diploma | 25 | 87 | 112 |
| BSN/MSN/PHD/Other | 12 | 69 | 81 | |
| Total | 37 | 156 | 193 | |
| Inpatient or outpatient (p = 0.310) | Inpatient | 12 | 59 | 71 |
| Outpatient | 23 | 78 | 101 | |
| Total | 37 | 156 | 193 | |
| Clinic Type (p = 0.261) | Women’s Cancer (Breast, GYN) | 5 | 12 | 17 |
| Others | 32 | 144 | 176 | |
| Total | 37 | 156 | 193 | |
| Age (p = 0.417) | 35 and under | 5 | 30 | 35 |
| 36 and over | 32 | 126 | 158 | |
| Total | 37 | 156 | 193 | |
| Religion (p = 0.017) | Atheist/Agnostic | 14 | 49 | 63 |
| Catholic | 20 | 59 | 79 | |
| Others | 3 | 48 | 51 | |
| Total | 37 | 156 | 193 | |
| Have Children (p = 0.806) | Yes | 28 | 121 | 149 |
| No | 9 | 35 | 44 | |
| Total | 37 | 156 | 193 | |
| Future Children (p = 0.465) | Yes | 4 | 23 | 27 |
| No | 32 | 121 | 153 | |
| Total | 36 | 144 | 180 ** | |
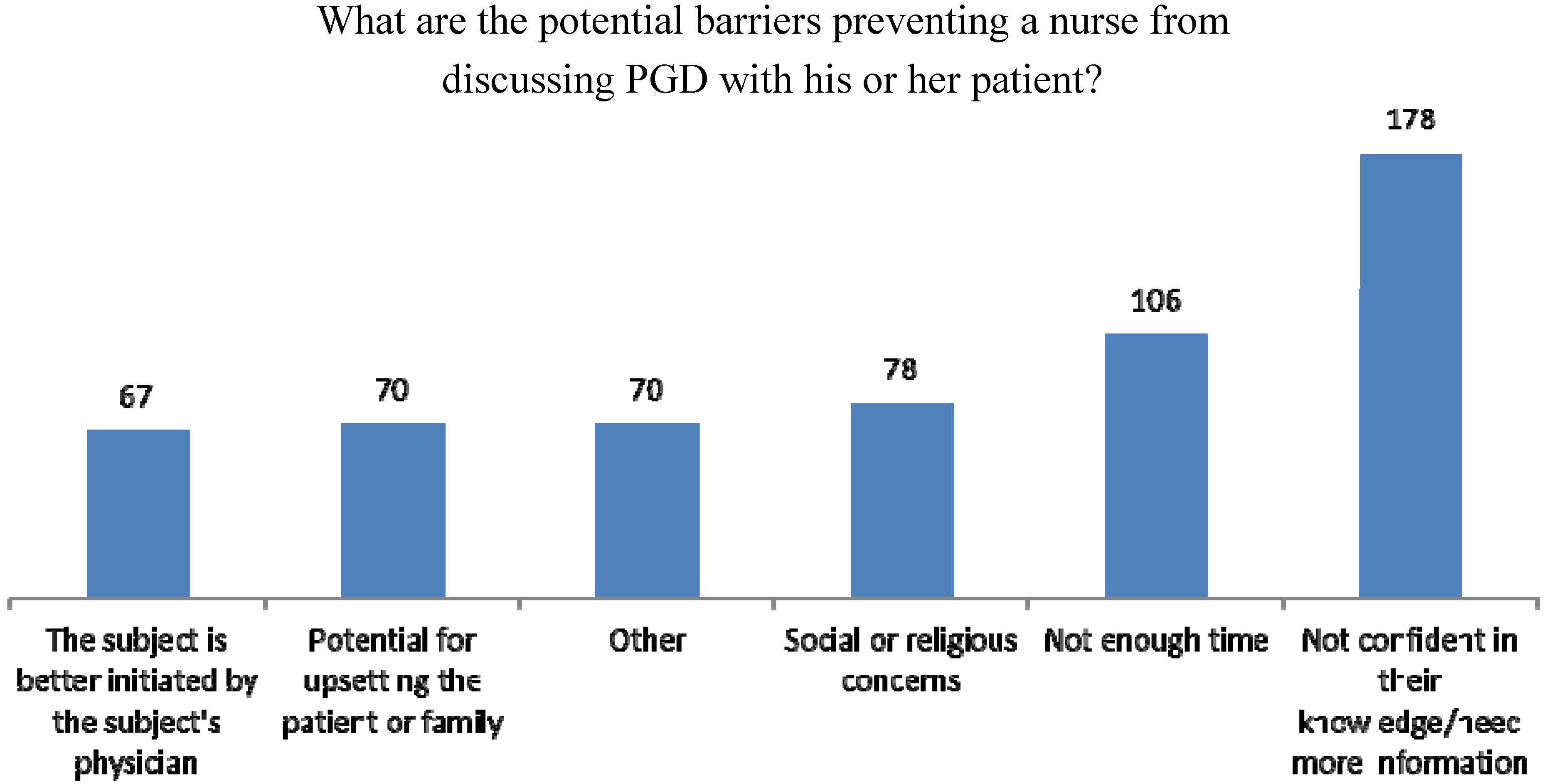
3.3. Educational Needs
4. Discussion
| Syndrome Name | Genes Responsible | Major Tumors/Cancers | Interventions |
|---|---|---|---|
| Cowden Syndrome | PTEN | Breast, thyroid, uterine; other benign tumors of various organs | Increased screening for all cancer/tumor types a |
| Familial Adenomatous Polyposis and MutYH-Associated Polyposis | APC, MutYH | Colon cancer and polyps; small intestinal cancer | Prophylactic removal of colon, increased screening for other cancers |
| Familial Paraganglioma Syndrome | SDHB, SDHC, SDHD | Paragangliomas of head, neck, and abdomen | Increased screening for paragangliomas |
| Hereditary Breast-Ovarian Cancer Syndrome | BRCA1, BRCA2 | Breast and ovarian cancer; prostate cancer in males; some other cancers slightly elevated | Increased breast screening, chemoprevention, and/or mastectomy; prophylactic removal of ovaries/fallopian tubes |
| Lynch Syndrome | MLH1, MSH2, MSH6, PMS2 | Colon and uterine cancer; other cancers such as stomach, ovarian, urinary tract | Increased colon cancer screening and chemoprevention; prophylactic removal of uterus/ovaries; screening for other cancers |
| Juvenile Polyposis Syndrome | MADH4 (aka SMAD4), BMPR1A | Gastrointestinal cancers, benign colon polyps | Increased screening for colon and small intestinal cancers |
| Li-Fraumeni Syndrome | TP53 | Breast, brain, lung cancer, leukemia | Increased screening for breast cancer; consider research-based imaging for other cancers |
| Multiple Endocrine Neoplasia type 1 | MEN1 | Pancreatic cancer (neuroendocrine); pituitary and parathyroid tumors | Increased screening for pancreatic and other tumors |
| Multiple Endocrine Neoplasia type 2 | RET | Medullary thyroid cancer; adrenal and parathyroid tumors | Prophylactic removal of thyroid; increased screening for other tumors |
| Peutz-Jeghers Syndrome | LKB1 (aka STK11) | Gastrointestinal, breast cancer | Increased screening for colon, small intestinal, and breast cancer |
| Von Hippel-Lindau Syndrome | VHL | Renal cell carcinoma, brain cancer (hemangioblastoma), other benign tumors | Increased screening for all cancers/tumors |
5. Limitations
6. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Handyside, A.H.; Kontogianni, E.H.; Hardy, K.; Winston, R. Pregnancies from biopsied human preimplantation embryos sexed by Y-specific DNA amplification. Nature 1990, 344, 768–770. [Google Scholar] [CrossRef]
- Sermon, K.; van Steirteghem, A.; Liebaers, I. Preimplantation genetic diagnosis. Lancet 2004, 363, 1633–1641. [Google Scholar] [CrossRef]
- Edwards, R.; Gardner, R. Choosing sex before birth. New Sci. 1968, 38, 218–220. [Google Scholar]
- Harper, J.; Wilton, L.; Traeger-Synodinos, J.; Goossens, V.; Moutou, C.; SenGupta, S.; Budak, T.P.; Renwick, P.; de Rycke, M.; Geraedts, J. The eshre PGD consortium: 10 years of data collection. Hum. Reprod. Update 2012, 18, 234–247. [Google Scholar] [CrossRef]
- Staton, A.D.; Kurian, A.W.; Cobb, K.; Mills, M.A.; Ford, J.M. Cancer risk reduction and reproductive concerns in female BRCA1/2 mutation carriers. Fam. Cancer 2008, 7, 179–186. [Google Scholar] [CrossRef]
- Ao, A.; Wells, D.; Handyside, A.H.; Winston, R.M.; Delhanty, J.D. Preimplantation genetic diagnosis of inherited cancer: Familial adenomatous polyposis coli. J. Assist. Reprod. Genet. 1998, 15, 140–144. [Google Scholar] [CrossRef]
- Offit, K.; Kohut, K.; Clagett, B.; Wadsworth, E.A.; Lafaro, K.J.; Cummings, S.; White, M.; Sagi, M.; Bernstein, D.; Davis, J.G. Cancer genetic testing and assisted reproduction. J. Clin. Oncol. 2006, 24, 4775–4782. [Google Scholar] [CrossRef]
- Schover, L.R. Psychosocial aspects of infertility and decisions about reproduction in young cancer survivors: A review. Med. Pediatr. Oncol. 1999, 33, 53–59. [Google Scholar] [CrossRef]
- Lavery, S.; Aurell, R.; Turner, C.; Castello, C.; Veiga, A.; Barri, P.N.; Winston, R. Preimplantation genetic diagnosis: Patients’ experiences and attitudes. Hum. Reprod. 2002, 17, 2464–2467. [Google Scholar] [CrossRef]
- Kuliev, A.; Rechitsky, S.; Verlinsky, O. Preimplantation testing for chromosomal disorders improves reproductive outcome of poor-prognosis patients. Reprod. Biomed. Online 2005, 11, 219–225. [Google Scholar] [CrossRef]
- Gianaroli, L.; Magli, M.C.; Ferraretti, A.P.; Tabanelli, C.; Trengia, V.; Farfalli, V.; Cavallini, G. The beneficial effects of preimplantation genetic diagnosis for aneuploidy support extensive clinical application. Reprod. Biomed. Online 2005, 10, 633–640. [Google Scholar] [CrossRef]
- Banerjee, I.; Shevlin, M.; Taranissi, M.; Thornhill, A.; Abdalla, H.; Ozturk, O.; Barnes, J.; Sutcliffe, A. Health of children conceived after preimplantation genetic diagnosis: A preliminary outcome study. Reprod. Biomed. Online 2008, 16, 376–381. [Google Scholar] [CrossRef]
- Smith, K.R.; Ellington, L.; Chan, A.Y.; Croyle, R.T.; Botkin, J.R. Fertility intentions following testing for a BRCA1 gene mutation. Cancer Epidemiol. Biomark. Prev. 2004, 13, 733–740. [Google Scholar]
- Kalfoglou, A.L.; Doksum, T.; Bernhardt, B.; Geller, G.; LeRoy, L.; Mathews, D.J.; Evans, J.H.; Doukas, D.J.; Reame, N.; Scott, J. Opinions about new reproductive genetic technologies: Hopes and fears for our genetic future. Fertil. Steril. 2005, 83, 1612–1621. [Google Scholar] [CrossRef]
- Karatas, J.; Strong, K.; Barlow-Stewart, K.; McMahon, C.; Meiser, B.; Roberts, C. Psychological impact of preimplantation genetic diagnosis: A review of the literature. Reprod. Biomed. Online 2010, 20, 83–91. [Google Scholar]
- Quinn, G.; Vadaparampil, S.; Wilson, C.; King, L.; Choi, J.; Miree, C.; Friedman, S. Attitudes of high-risk women toward preimplantation genetic diagnosis. Fertil. Steril. 2009, 91, 2361–2368. [Google Scholar] [CrossRef]
- Lammens, C.; Bleiker, E.; Aaronson, N.; Vriends, A.; Ausems, M.; Jansweijer, M.; Wagner, A.; Sijmons, R.; van den Ouweland, A.; van der Luijt, R. Attitude towards pre-implantation genetic diagnosis for hereditary cancer. Fam. Cancer 2009, 8, 457–464. [Google Scholar] [CrossRef]
- Alsulaiman, A.; Hewison, J. Attitudes to prenatal and preimplantation diagnosis in Saudi parents at genetic risk. Prenat. Diagn. 2006, 26, 1010–1014. [Google Scholar] [CrossRef]
- Fortuny, D.; Balmaña, J.; Graña, B.; Torres, A.; y Cajal, T.R.; Darder, E.; Gadea, N.; Velasco, A.; López, C.; Sanz, J. Opinion about reproductive decision making among individuals undergoing BRCA1/2 genetic testing in a multicentre spanish cohort. Hum. Reprod. 2009, 24, 1000–1006. [Google Scholar]
- Menon, U.; Harper, J.; Sharma, A.; Fraser, L.; Burnell, M.; ElMasry, K.; Rodeck, C.; Jacobs, I. Views of BRCA gene mutation carriers on preimplantation genetic diagnosis as a reproductive option for hereditary breast and ovarian cancer. Hum. Reprod. 2007, 22, 1573–1577. [Google Scholar] [CrossRef]
- Karatas, J.; Barlow-Stewart, K.; Meiser, B.; McMahon, C.; Strong, K.; Hill, W.; Roberts, C.; Kelly, P. A prospective study assessing anxiety, depression and maternal-fetal attachment in women using PGD. Hum. Reprod. 2011, 26, 148–156. [Google Scholar]
- Eugster, A.; Vingerhoets, A. Psychological aspects of in vitro fertilization: A review. Soc. Sci. Med. 1999, 48, 575–589. [Google Scholar]
- Kuliev, A.; Rechitsky, S.; Laziuk, K.; Verlinsky, O.; Tur-Kaspa, I.; Verlinsky, Y. Pre-embryonic diagnosis for sandhoff disease. Reprod. Biomed. Online 2006, 12, 328–333. [Google Scholar] [CrossRef]
- Farra, C.; Nassar, A.H.; Usta, I.M.; Salameh, P.; Souaid, M.; Awwad, J. Acceptance of preimplantation genetic diagnosis for β - thalassemia in lebanese women with previously affected children. Prenat. Diagn. 2008, 28, 828–832. [Google Scholar] [CrossRef]
- Pergament, E. Preimplantation diagnosis: A patient perspective. Prenat. Diagn. 1991, 11, 493–500. [Google Scholar] [CrossRef]
- Kalfoglou, A.L.; Scott, J.; Hudson, K. PGD patients’ and providers’ attitudes to the use and regulation of preimplantation genetic diagnosis. Reprod. Biomed. Online 2005, 11, 486–496. [Google Scholar]
- Hershberger, P.E.; Pierce, P.F. Conceptualizing couples’ decision making in PGD: Emerging cognitive, emotional, and moral dimensions. Patient Educ. Couns. 2010, 81, 53–62. [Google Scholar] [CrossRef]
- Krones, T.; Schlüter, E.; Manolopoulos, K.; Bock, K.; Tinneberg, H.-R.; Koch, M.C.; Lindner, M.; Hoffmann, G.F.; Mayatepek, E.; Huels, G. Public, expert and patients’ opinions on preimplantation genetic diagnosis (PGD) in germany. Reprod. Biomed. Online 2005, 10, 116–123. [Google Scholar]
- Keye, W.R., Jr.; Bradshaw, K.D. A survey of the practices and opinions of the domestic members of the american society for reproductive medicine. Fertil. Steril. 2004, 82, 536–542. [Google Scholar] [CrossRef]
- Brandt, A.C.; Tschirgi, M.L.; Ready, K.J.; Sun, C.; Darilek, S.; Hecht, J.; Arun, B.K.; Lu, K.H. Knowledge, attitudes, and clinical experience of physicians regarding preimplantation genetic diagnosis for hereditary cancer predisposition syndromes. Fam. Cancer 2010, 9, 479–487. [Google Scholar] [CrossRef]
- Klitzman, R.; Chung, W.; Marder, K.; Shanmugham, A.; Chin, L.J.; Stark, M.; Leu, C.-S.; Appelbaum, P.S. Views of internists towards uses of PGD. Reprod. Biomed. Online 2013, 26, 142–147. [Google Scholar] [CrossRef]
- Kalfoglou, A.; Suthers, K.; Scott, J.; Hudson, K. Reproductive Genetic Testing: What America Thinks; Genetics and Public Policy Center: Washington, DC, USA, 2004. [Google Scholar]
- Practice Committee of the Society for Assisted Reproductive Technology; Practice Committee of the American Society for Reproductive Medicine. Preimplantation genetic testing: A practice committee opinion. Fertil. Steril. 2008, 88, 1497–1504. [Google Scholar]
- Sussner, K.M.; Jandorf, L.; Valdimarsdottir, H.B. Educational needs about cancer family history and genetic counseling for cancer risk among frontline healthcare clinicians in new york city. Genet. Med. 2011, 13, 785–793. [Google Scholar] [CrossRef]
- Masny, A.; Daly, M.; Ross, E.; Balshem, A.; Gillespie, D.; Weil, S. A training course for oncology nurses in familial cancer risk assessment: Evaluation of knowledge and practice. J. Cancer Educ. 2003, 18, 20–25. [Google Scholar]
- Masny, A.; Ropka, M.E.; Peterson, C.; Fetzer, D.; Daly, M.B. Mentoring nurses in familial cancer risk assessment and counseling: Lessons learned from a formative evaluation. J. Genet. Couns. 2008, 17, 196–207. [Google Scholar]
- Lee, J.; Jung Cho, H.; Yoo, H.-W.; Park, S.K.; Yang, J.J.; Kim, S.-W.; Kang, E.; Ahn, S.-H.; Lee, S.-J.; Jin Suh, Y.; et al. The effects of a genetic counseling educational program on hereditary breast cancer for korean healthcare providers. J. Breast Cancer 2013, 16, 335–341. [Google Scholar]
- Prows, C.A.; Glass, M.; Nicol, M.J.; Skirton, H.; Janet, W. Genomics in nursing education. J. Nurs. Scholarsh. 2005, 37, 196–202. [Google Scholar] [CrossRef]
- Jenkins, J.; Calzone, K.A. Establishing the essential nursing competencies for genetics and genomics. J. Nurs. Scholarsh. 2007, 39, 10–16. [Google Scholar] [CrossRef]
- Calzone, K.A.; Jenkins, J.; Masny, A. Core competencies in cancer genetics for advanced practice oncology nurses. Oncol. Nurs. Forum 2002, 29, 1327–1333. [Google Scholar] [CrossRef]
- Lewis, J.A.; Calzone, K.M.; Jenkins, J. Essential nursing competencies and curricula guidelines for genetics and genomics. MCN Am. J. Matern. Child Nurs. 2006, 31, 146–153. [Google Scholar] [CrossRef]
- National Human Genome Research Institute. Essential Nursing Competencies and Curricula Guidelines for Genetics and Genomics. Available online: http://www.Genome.Gov/pages/careers/healthprofessionaleducation/geneticscompetency.Pdf (accessed on 21–22 September 2005).
- Incollingo, B.F. Genetic Counseling in Cancer Care: What is the Role of Oncology Nurses? Oncol. Nurs. News. Available online: http://nursing.Onclive.Com/publications/oncology-nurse/2012/february-2012/genetic-counseling-in-cancer-care-what-is-the-role-of-oncology-nurses (accessed on 6 March 2012).
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Quinn, G.P.; Knapp, C.; Sehovic, I.; Ung, D.; Bowman, M.; Gonzalez, L.; Vadaparampil, S.T. Knowledge and Educational Needs about Pre-Implantation Genetic Diagnosis (PGD) among Oncology Nurses. J. Clin. Med. 2014, 3, 632-645. https://doi.org/10.3390/jcm3020632
Quinn GP, Knapp C, Sehovic I, Ung D, Bowman M, Gonzalez L, Vadaparampil ST. Knowledge and Educational Needs about Pre-Implantation Genetic Diagnosis (PGD) among Oncology Nurses. Journal of Clinical Medicine. 2014; 3(2):632-645. https://doi.org/10.3390/jcm3020632
Chicago/Turabian StyleQuinn, Gwendolyn P., Caprice Knapp, Ivana Sehovic, Danielle Ung, Meghan Bowman, Luis Gonzalez, and Susan T. Vadaparampil. 2014. "Knowledge and Educational Needs about Pre-Implantation Genetic Diagnosis (PGD) among Oncology Nurses" Journal of Clinical Medicine 3, no. 2: 632-645. https://doi.org/10.3390/jcm3020632





