Are Recent Medical Graduates More Skeptical of Vaccines?
Abstract
:1. Introduction
2. Experimental Section
2.1. Design
2.2. Survey
| Constructs for Provider Vaccine Beliefs | ||
|---|---|---|
| Construct | Question | Disease/Vaccine |
| Disease Susceptibility | How likely do you think an unimmunized child in the United States is to get the following diseases during the next ten years? (Response Options: Impossible, Not Likely, Somewhat likely, Likely, Very Likely) | Polio Invasive Haemophilus influenzae type b (Hib) Varicella/chicken pox Hepatitis B Invasive Pneumococcal Disease Influenza |
| Disease Severity | If an 8-year old child got these diseases, how likely is the child to be seriously ill? (Response Options: Not serious at all, Not very serious, Somewhat serious, Serious, Very Serious) | |
| Vaccine Efficacy | How well do you think each of these vaccines prevents disease? (If the child completes the full recommended series) (Response Options: Not protective at all, Not very protective, Somewhat protective, Protective, Very Protective) | Polio (Inactivated/IPV) vaccine Haemophilus influenzae type B (Hib) conjugate vaccine Varicella/chicken pox vaccine Hepatitis B vaccine S. pneumoniae conjugate (Prevnar/PCV7) vaccine Influenza (inactivated) vaccine |
| Vaccine Safety | How safe do you think these vaccines are? (Response Options: Very unsafe, Unsafe, Somewhat safe, Safe, Very safe) | |
2.3. Data Analysis
3. Results and Discussion
3.1. Results
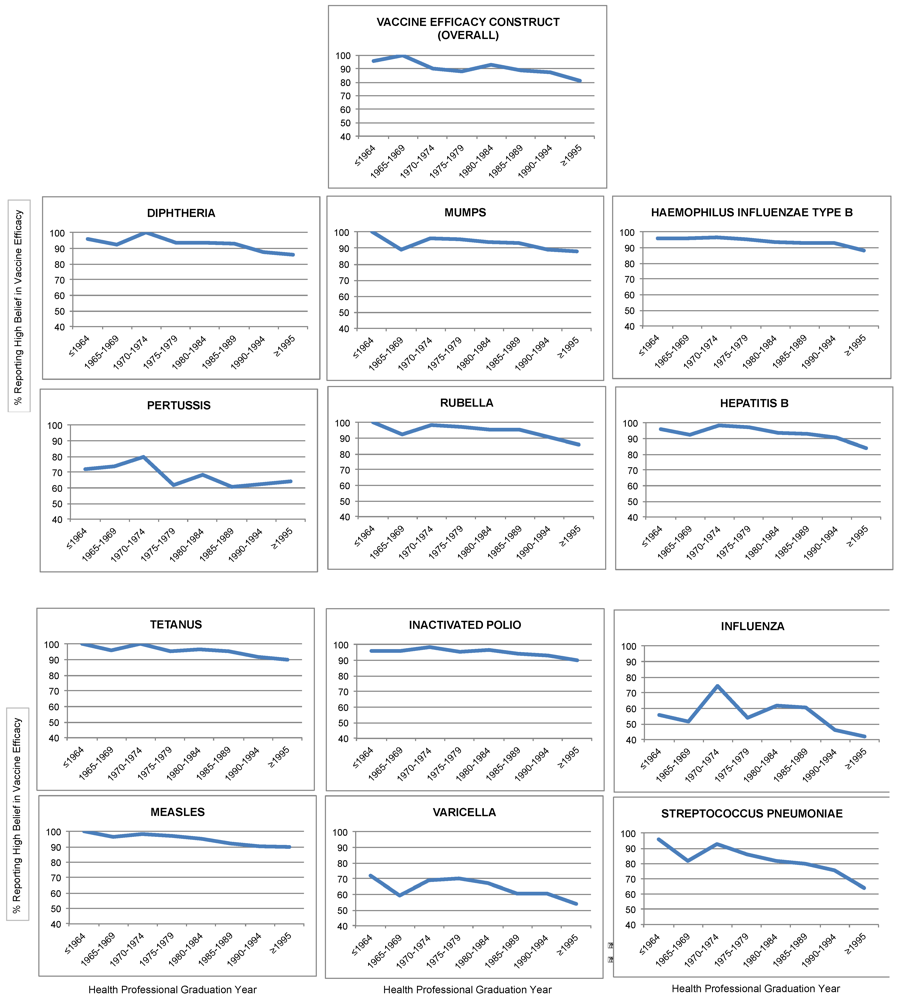
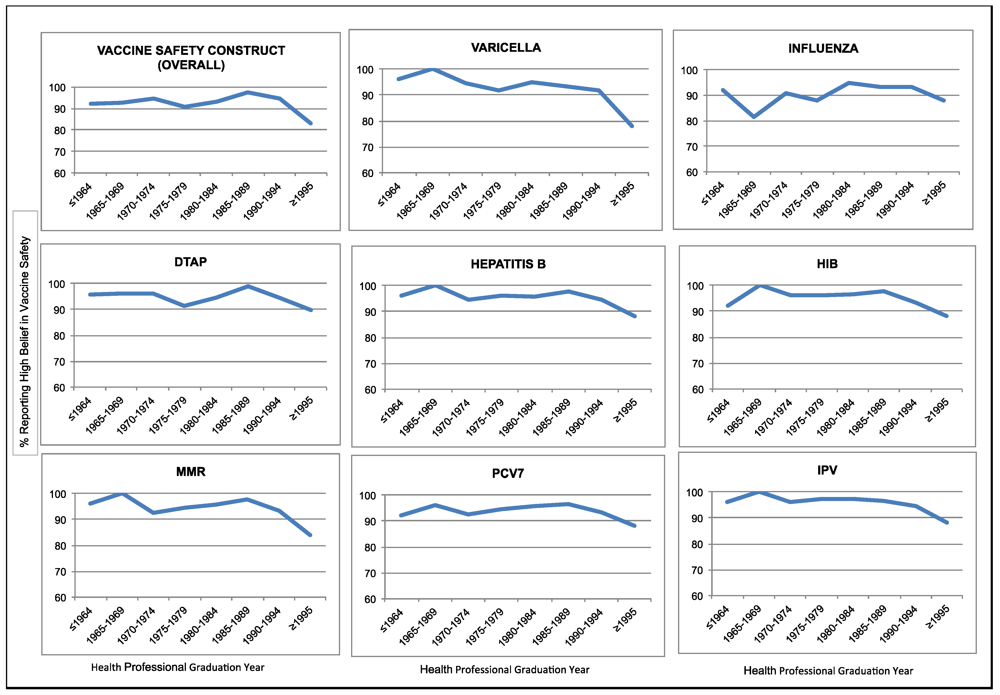
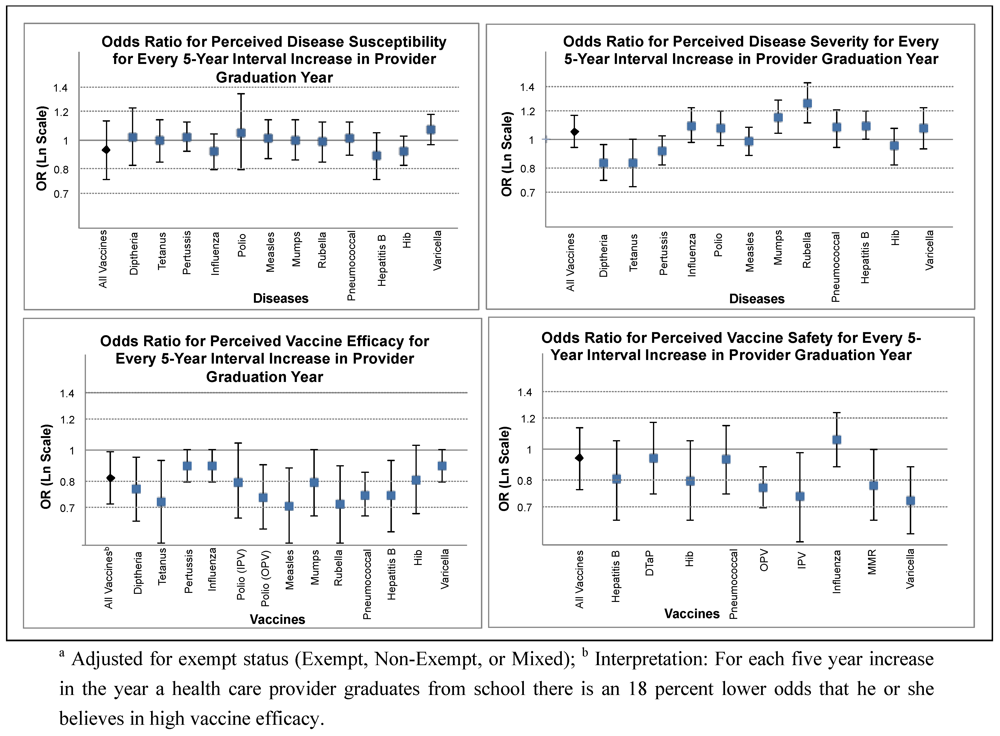
3.2. Discussion
| Key Immunization Beliefs (Response Options: Strongly disagree, Disagree, Neither agree or disagree, Agree, Strongly agree) | Agree or Strongly Agree | |||
|---|---|---|---|---|
| n | % | OR a | 95% CI b | |
| Children should only be immunized against serious diseases | 236 | 44.2 | 0.97 | 0.88–1.1 |
| Children get more immunizations than are good for them | 43 | 8.1 | 1.2 | 1.0–1.4 |
| I am concerned a child’s immune system could be weakened by too many immunizations | 32 | 6.0 | 1.02 | 0.83–1.3 |
| I am more likely to trust immunizations that have been around for a while | 373 | 69.5 | 0.98 | 0.89–1.1 |
| Immunizations are one of the safest forms of medicine ever developed | 431 | 81.2 | 0.76 c,d | 0.67–0.87 |
| Immunizations are getting better and safer all of the time as a result of medical research | 473 | 89.1 | 0.84 | 0.71–0.98 |
| Vaccines strengthen the immune system | 358 | 67.6 | 1.1 | 1.0–1.2 |
| For the overall health of a child, it is better for them to develop immunity by getting sick than to get a vaccine | 28 | 5.2 | 1.2 | 0.92–1.4 |
| Healthy children do not need immunizations | 18 | 3.4 | 1.0 | 0.79–1.3 |
| Immunizations do more harm than good | 21 | 3.9 | 1.3 | 1.0–1.8 |
| I am opposed to school immunization requirements because they go against freedom of choice | 32 | 6.0 | 1.3 | 1.0–1.6 |
| I am opposed to school immunization requirements because parents know what is best for their children | 13 | 2.4 | 1.2 | 0.86–1.6 |
| School immunization requirements protect children against getting diseases from unimmunized children | 474 | 88.4 | 0.91 | 0.78–1.1 |
4. Conclusions
Acknowledgments
Conflict of Interest
References
- Centers for Disease Control and Prevention (CDC). Impact of vaccines universally recommended for children—United States, 1990–1998. MMWR Morb. Mortal. Wkly. Rep. 1999, 48, 243–248.
- Freed, G.L.; Clark, S.J.; Butchart, A.T.; Singer, D.C.; Davis, M.M. Parental vaccine safety concerns in 2009. Pediatrics 2010, 125, 654–659. [Google Scholar]
- Freed, G.L.; Clark, S.J.; Hibbs, B.F.; Santoli, J.M. Parental vaccine safety concerns: The experiences of pediatricians and family physicians. Am. J. Prev. Med. 2004, 26, 11–14. [Google Scholar] [CrossRef]
- Bardenheier, B.; Yusuf, H.; Schwartz, B.; Gust, D.; Barker, L.; Rodewald, L. Are parental vaccine safety concerns associated with receipt of measles-mumps-rubella, diphtheria and tetanus toxoids with acellular pertussis, or hepatitis B vaccines by children? Arc. Pediatr. Adolesc. Med. 2004, 158, 569–575. [Google Scholar] [CrossRef]
- Gust, D.A.; Strine, T.W.; Maurice, E.; Smith, P.; Yusuf, H.; Wilkinson, M.; Battaglia, M.; Wright, R.; Schwartz, R. Underimmunization among children: Effects of vaccine safety concerns on immunization status. Pediatrics 2004, 114, e16–e22. [Google Scholar] [CrossRef]
- Association of State and Territorial Health Offices. Communicating Effectively About Vaccines: Summary of a Survey of U.S. Parents and Guardians, ASTHO. Available online: http://www.astho.org/Communicating_Effectively_About_Vaccines/ (accessed on 12 December 2010).
- Chen, R.T.; Hibbs, B. Vaccine safety: Current and future challenges. Pediatr. Ann. 1998, 27, 445–455. [Google Scholar]
- Salmon, D.A.; Smith, P.J.; Pan, W.K.; Navar, A.M.; Omer, S.B.; Halsey, N.A. Disparities in preschool immunization coverage associated with maternal age. Hum. Vaccines 2009, 5, 557–561. [Google Scholar] [CrossRef]
- Mnookin, S. The Panic Virus: A True Story of Medicine, Science, and Fear; Simon & Schuster: New York, NY, USA, 2011. [Google Scholar]
- Salmon, D.A.; Moulton, L.H.; Omer, S.B.; deHart, M.P.; Stokley, S.; Halsey, N.A. Factors associated with refusal of childhood vaccines among parents of school-aged children: A case-control study. Arch. Pediatr. Adolesc. Med. 2005, 159, 470–476. [Google Scholar] [CrossRef]
- Orenstein, W.A.; Bernier, R.H. Crossing the divide from vaccine technology to vaccine delivery: The critical role of providers. JAMA 1994, 272, 1138–1139. [Google Scholar] [CrossRef]
- Gust, D.A.; Kennedy, A.; Shui, I.; Smith, P.J.; Nowak, G.; Pickering, L.K. Parent attitudes toward immunizations and healthcare providers the role of information. Am. J. Prev. Med. 2005, 29, 105–112. [Google Scholar] [CrossRef]
- Grabowsky, M.; Orenstein, W.A.; Marcuse, E.K. The critical role of provider practices in undervaccination. Pediatrics 1996, 97, 735–737. [Google Scholar]
- Zimmerman, R.K.; Mieczkowski, T.A.; Mainzer, H.M.; Medsger, A.R.; Nowalk, M.P. Understanding physician agreement with varicella immunization guidelines. Prev. Med. 2002, 35, 135–142. [Google Scholar] [CrossRef]
- Taylor, J.A.; Darden, P.M.; Slora, E.; Hasemeier, C.M.; Asmussen, L.; Wasserman, R. The influence of provider behavior, parental characteristics, and a public policy initiative on the immunization status of children followed by private pediatricians: A study from pediatric research in office settings. Pediatrics 1997, 99, 209–215. [Google Scholar]
- Salmon, D.A.; Pan, W.K.Y.; Omer, S.B.; Navar, A.M.; Orenstein, W.; Marcuse, E.K.; Taylor, J.A.; deHart, M.P.; Stokley, S.; Carter, T.; et al. Vaccine knowledge and practices of primary care providers of exempt vs. vaccinated children. Hum. Vaccines 2008, 4, 286–291. [Google Scholar] [CrossRef]
- Zimmerman, R.K.; Bradford, B.J.; Janosky, J.E.; Mieczkowski, T.A.; DeSensi, E.; Grufferman, S. Barriers to measles and pertussis immunization: The knowledge and attitudes of Pennsylvania primary care physicians. Am. J. Prev. Med. 1997, 13, 89–97. [Google Scholar]
- Ehresmann, K.R.; Mills, W.A.; Loewenson, P.R.; Moore, K.A. Attitudes and practices regarding varicella vaccination among physicians in Minnesota: Implications for public health and provider education. Am. J. Public Health 2000, 90, 1917–1920. [Google Scholar] [CrossRef]
- Zimmerman, R.K.; Giebink, G.S.; Street, H.B.; Janosky, J.E. Knowledge and attitudes of Minnesota primary care physicians about barriers to measles and pertussis immunization. J. Am. Board Fam. Pract. 1995, 8, 270–277. [Google Scholar]
- Smith, P.J.; Humiston, S.G.; Parnell, T.; Vannice, K.S.; Salmon, D.A. The association between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Rep. 2010, 125, 534–541. [Google Scholar]
- Chatterjee, A.; O’Keefe, C. Current controversies in the USA regarding vaccine safety. Expert Rev. Vaccines 2010, 9, 497–502. [Google Scholar] [CrossRef]
- Gust, D.; Weber, D.; Weintraub, E.; Kennedy, A.; Soud, F.; Burns, A. Physicians who do and do not recommend children get all vaccinations. J. Health Commun. 2008, 13, 573–582. [Google Scholar] [CrossRef]
- Taylor, J.A.; Darden, P.M.; Brooks, D.A.; Hendricks, J.W.; Baker, A.E.; Wasserman, R.C. Practitioner policies and beliefs and practice immunization rates: A study from pediatric research in office settings and the national medical association. Pediatrics 2002, 109, 294–300. [Google Scholar] [CrossRef]
- Koepke, C.P.; Vogel, C.A.; Kohrt, A.E. Provider characteristics and behaviors as predictors of immunization coverage. Am. J. Prev. Med. 2001, 21, 250–255. [Google Scholar] [CrossRef]
- Chen, R.T.; Rastogi, S.C.; Mullen, J.R.; Hayes, S.W.; Cochi, S.L.; Donlon, J.A.; Wassilak, S.G. The vaccine adverse event reporting system (VAERS). Vaccine 1994, 12, 542–550. [Google Scholar] [CrossRef]
- Zimmerman, R.K.; Schlesselman, J.J.; Baird, A.L.; Mieczkowski, T.A. A national survey to understand why physicians defer childhood immunizations. Arch. Pediatr. Adolesc. Med. 1997, 151, 657–664. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Hughes, M.M.; Omer, S.B.; Pan, W.K.Y.; Navar-Boggan, A.M.; Orenstein, W.; Marcuse, E.K.; Taylor, J.; DeHart, M.P.; Carter, T.C.; Damico, A.; et al. Are Recent Medical Graduates More Skeptical of Vaccines? Vaccines 2013, 1, 154-166. https://doi.org/10.3390/vaccines1020154
Hughes MM, Omer SB, Pan WKY, Navar-Boggan AM, Orenstein W, Marcuse EK, Taylor J, DeHart MP, Carter TC, Damico A, et al. Are Recent Medical Graduates More Skeptical of Vaccines? Vaccines. 2013; 1(2):154-166. https://doi.org/10.3390/vaccines1020154
Chicago/Turabian StyleHughes, Michelle M., Saad B. Omer, William K.Y. Pan, Ann Marie Navar-Boggan, Walter Orenstein, Edgar K. Marcuse, James Taylor, M. Patricia DeHart, Terrell C. Carter, Anthony Damico, and et al. 2013. "Are Recent Medical Graduates More Skeptical of Vaccines?" Vaccines 1, no. 2: 154-166. https://doi.org/10.3390/vaccines1020154
APA StyleHughes, M. M., Omer, S. B., Pan, W. K. Y., Navar-Boggan, A. M., Orenstein, W., Marcuse, E. K., Taylor, J., DeHart, M. P., Carter, T. C., Damico, A., Halsey, N., & Salmon, D. A. (2013). Are Recent Medical Graduates More Skeptical of Vaccines? Vaccines, 1(2), 154-166. https://doi.org/10.3390/vaccines1020154






