Discriminating Gene Expression Signature of Radiation-Induced Thyroid Tumors after Either External Exposure or Internal Contamination
Abstract
:1. Radiosensitivity of Thyroid Tissue in Childhood
2. Do Radiation-Induced Thyroid Tumors Show Specific Clinical Features?
3. High-Throughput Molecular Studies of Radiation-Induced Thyroid Tumors: Can They Identify Discriminating Radiation-Induced Markers?
4. Highly Discriminating Radiation-Induced Thyroid Tumor Signature: Is It a Question of Methodology?
| Study | Port et al.; 2007 | Detours et al.; 2007 | Stein et al.; 2010 1 | Ugolin et al.; 2,3 | Ory et al.; 2011 3 | Boltze et al.; 2009 | |
| Exposure | Post-Chernobyl | Post-Chernobyl | Post-Chernobyl | Post-Chernobyl | Post-radiotherapy | Post-Chernobyl | |
| Radiation-induced | Tumor set | 11 PTC 6 | 12 PTC | 10 PTC | Learning set: 6 PTC | Learning set: 7 rPTC, 7rFTA | 86 PTC |
| 3 males, 8 females | 4 males, 8 females | Half male and half female | 3 males, 3 females | 4 males, 10 females | 40 males, 46 females | ||
| Age at IR | / | 1b–16 years(M = 8.6 years) | 2 monthb–14 years (M = 6 years) | 10b–16 years (M = 12.7 years) | 3b–14 years (M = 8.6 years) | 3b–23 years (M = 11.8 years) | |
| Age at diagnosis | 15b–22 years (M = 18 years) | 16b–33 years (M = 24 years) | 14b–28 years (M = 20 years) | 27b–33 years (M = 29.2 years) | 20b–56 years (M = 35.1 years) | 12b–28 years (M = 18.6 years) | |
| Latency | Up to 15 years after 1986 | 15b–17 years (M = 16 years) | 14b–16 years (M = 13.6 years) | 16b–17 years (M = 16.5 years) | 11b–48 years (M = 26.5 years) | Up to 15 years after 1986 (mean = 6.8 years) | |
| Dosimetry | 90% at 0.15-1Gy 4 | / | / | / | 12b–42.5 Gy (M = 14.1 Gy) | 90% at 0.15-1Gy 4 | |
| Histology | PTC | 8 PTC, 3 FVPTC, 1 PTC | PTC | ? 7 | 7 FTA; 6 PTC; 1 FVPTC | PTC | |
| Mutations | 2 PTC1; PTC3 6 | 5 BRAF; 5 PTC | 1 PTC; 1 PTC3 | 4 BRAF; 1 RET/PTC | 1 BRAF; 1 RAS | ||
| Others | T2N0M0 to T4N1M1 | / | / | / | 5 with chemotherapy | ||
| Sporadic | Tumor set | 41 PTC | 14 PTC 7 | 20 PTC from He et al. study 5 | Learning set: 7 PTC | Learning set: 7 sPTC, 7sFTA | 91 PTC |
| 19 males, 22 females | 5 males, 9 females | 8 males, 12 females | 4 males, 3 females | 5 males, 9 females | 49 males, 42 females | ||
| Age at diagnosis | 15b–83years (M = 60 years) | 29b–68 years (M = 47 years) | 13b–65 years (M = 44.4 years) | 29b–38 years (M = 34.6 years) | 21b–63 years (M = 37.6 years) | 15b–83 years (M = 50.1 years) | |
| Histology | PTC 6 | 9 PTC, 4 FVPTC, 1 tPTC | 14 PTC; 5 FVPTC; 1 HCC7 | / 7 | 7 FTA; 5 PTC; 2 FVPTC | PTC | |
| Mutations | 5 PTC1 | 5/14 BRAF; 3/14 RET/PTC | / | 2 BRAF; 1 RET/PTC | 4 BRAF; 2 RAS, 1 PTC1, 1 PTC3 | ||
| Others | T1N0-1M0 (n = 26) to T3N1M0 | / | / | None with chemotherapy | |||
| Arrays | Human genome survey microarray V2.0 (Applied Biosystems) (33,000 probes) | Human 1 cDNA Microarray slides (Agilent Technologies). (19,000 probes) | Affymetrix U133A Array (20,000 probes) (Stein et al.) | Dataset retrieved from GEO (GSE3950) | Human 25K 50b–52mer oligo-microarrays (national genomic platform) | (Not relevant) | |
| Hybridized with normal matched tissue | Affymetrix U133 Plus 2.0 Array (50,000 probes) (He et al.) Hybridized with normal matched tissue | Hybridized with an internal reference (pool of normal thyroid tissues) | |||||
| Analysis | Identified 1300 genes up- or downregulated at least fivefold (pool of 10 rPTC vs. pool of 10 sPTC) | (1) Several methods applied for tumor classification | Compared two sets of deregulated genes obtained separately: (1) post-Chernobyl PTC vs. normal tissues and; (2) sporadic PTC vs. normal tissues | 106 genes discriminating signature identified by applying the EMts_PCA on the learning/training set | 322-gene discriminating signature identified by applying the EMts_PCA to the learning/training set | Identification of protein markers by MALDI-TOF mass spectrophotometry | |
| Validation of 92 more deregulated genes in the full tumor series by RT-PCR | (2) Same methods applied for tumor classification by using a γ-irradiation vs. H2O2 lymphocyte response signature. | Retained the genes deregulated in post-Chernobyl PTC only | 651 deregulated genes identified | 1900 deregulated genes identified | 20 candidate protein markers analyzed by immunochemistry | ||
| Results | 10 genes for complete separation of the groups (no validation on an independent tumor sets) | In both cases classification with error rate errors of 8 to 42% for sporadic tumors and 7 to 29% for post-Chernobyl tumors | Identified 177 deregulated genes unique to the radiation-induced tumors | Etiology prediction of the 13 remaining tumors using the 106 gene signature (1 unclassified, non misclassified) | Blind prediction of etiology of the 29 remaining tumors (tumors (13 rPTC or FTA; 16 sPTC FTA) (1 unclassified, 2 misclassified) | Combination of 6 of these markers separates the groups (no validation on an independent tumor sets) |
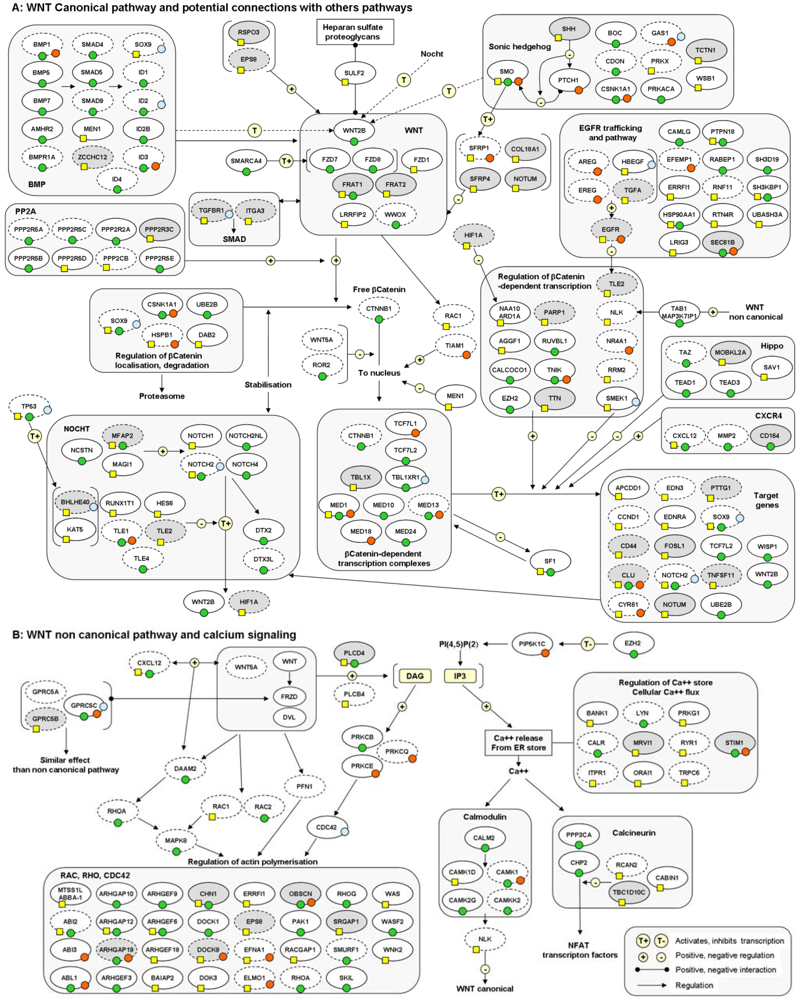
5. Are Specific Molecular Pathways Deregulated in Radiation-Induced Thyroid Tumors?
6. Imprinting of Radiation-Induced Thyroid Tumors: Impact of the Mode of Exposure, Dose and Dose Rate
7. The Persistent Problem of Low Doses: Can We Evaluate the Risk of Thyroid Cancers for Doses Lower Than 0.1 Gy?
8. Conclusions and Perspectives
Acknowledgments
References
- Duffy, B.J., Jr.; Fitzgerald, P.J. Thyroid cancer in childhood and adolescence; a report on 28 cases. Cancer 1950, 3, 1018–1032. [Google Scholar] [CrossRef]
- Ronckers, C.M.; Sigurdson, A.J.; Stovall, M.; Smith, S.A.; Mertens, A.C.; Liu, Y.; Hammond, S.; Land, C.E.; Neglia, J.P.; Donaldson, S.S.; et al. Thyroid cancer in childhood cancer survivors: A detailed evaluation of radiation dose response and its modifiers. Radiat. Res. 2006, 166, 618–628. [Google Scholar] [CrossRef]
- Bhatti, P.; Veiga, L.H.; Ronckers, C.M.; Sigurdson, A.J.; Stovall, M.; Smith, S.A.; Weathers, R.; Leisenring, W.; Mertens, A.C.; Hammond, S.; et al. Risk of second primary thyroid cancer after radiotherapy for a childhood cancer in a large cohort study: An update from the childhood cancer survivor study. Radiat. Res. 2010, 174, 741–752. [Google Scholar] [CrossRef]
- Preston, D.L.; Ron, E.; Tokuoka, S.; Funamoto, S.; Nishi, N.; Soda, M.; Mabuchi, K.; Kodama, K. Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat. Res. 2007, 168, 1–64. [Google Scholar] [CrossRef]
- Tronko, M.D.; Howe, G.R.; Bogdanova, T.I.; Bouville, A.C.; Epstein, O.V.; Brill, A.B.; Likhtarev, I.A.; Fink, D.J.; Markov, V.V.; Greenebaum, E.; et al. A cohort study of thyroid cancer and other thyroid diseases after the chornobyl accident: Thyroid cancer in Ukraine detected during first screening. J. Natl. Cancer Inst. 2006, 98, 897–903. [Google Scholar] [CrossRef]
- Zablotska, L.B.; Ron, E.; Rozhko, A.V.; Hatch, M.; Polyanskaya, O.N.; Brenner, A.V.; Lubin, J.; Romanov, G.N.; McConnell, R.J.; O’Kane, P.; et al. Thyroid cancer risk in Belarus among children and adolescents exposed to radioiodine after the Chornobyl accident. Br. J. Cancer 2011, 104, 181–187. [Google Scholar] [CrossRef]
- Ron, E. Thyroid cancer incidence among people living in areas contaminated by radiation from the Chernobyl accident. Health Phys. 2007, 93, 502–511. [Google Scholar] [CrossRef]
- Cardis, E.; Hatch, M. The Chernobyl accident-an epidemiological perspective. Clin. Oncol. (R. Coll. Radiol.) 2011, 23, 251–260. [Google Scholar] [CrossRef]
- Brenner, A.V.; Tronko, M.D.; Hatch, M.; Bogdanova, T.I.; Oliynik, V.A.; Lubin, J.H.; Zablotska, L.B.; Tereschenko, V.P.; McConnell, R.J.; Zamotaeva, G.A.; et al. I-131 dose response for incident thyroid cancers in ukraine related to the chornobyl accident. Environ. Health Perspect. 2011, 119, 933–939. [Google Scholar] [CrossRef]
- Ron, E.; Lubin, J.H.; Shore, R.E.; Mabuchi, K.; Modan, B.; Pottern, L.M.; Schneider, A.B.; Tucker, M.A.; Boice, J.D., Jr. Thyroid cancer after exposure to external radiation: A pooled analysis of seven studies. Radiat. Res. 1995, 141, 259–277. [Google Scholar] [CrossRef]
- Sadetzki, S.; Chetrit, A.; Lubina, A.; Stovall, M.; Novikov, I. Risk of thyroid cancer after childhood exposure to ionizing radiation for tinea capitis. J. Clin. Endocrinol. Metab. 2006, 91, 4798–4804. [Google Scholar] [CrossRef]
- Tronko, M.D.; Bogdanova, T.I.; Komissarenko, I.V.; Epstein, O.V.; Oliynyk, V.; Kovalenko, A.; Likhtarev, I.A.; Kairo, I.; Peters, S.B.; LiVolsi, V.A. Thyroid carcinoma in children and adolescents in Ukraine after the Chernobyl nuclear accident: Statistical data and clinicomorphologic characteristics. Cancer 1999, 86, 149–156. [Google Scholar] [CrossRef]
- LiVolsi, V.A.; Abrosimov, A.A.; Bogdanova, T.; Fadda, G.; Hunt, J.L.; Ito, M.; Zablotska, L.B.; Tronko, M.D. The Chernobyl thyroid cancer experience: Pathology. Clin. Oncol. (R. Coll. Radiol.) 2011, 23, 261–267. [Google Scholar] [CrossRef]
- Williams, E.D.; Abrosimov, A.; Bogdanova, T.; Demidchik, E.P.; Ito, M.; LiVolsi, V.; Lushnikov, E.; Rosai, J.; Sidorov, Y.; Tronko, M.D.; et al. Thyroid carcinoma after Chernobyl latent period, morphology and aggressiveness. Br. J. Cancer 2004, 90, 2219–2224. [Google Scholar] [CrossRef]
- LiVolsi, V.A.; Abrosimov, A.A.; Bogdanova, T.; Fadda, G.; Hunt, J.L.; Ito, M.; Rosai, J.; Thomas, G.A.; Williams, E.D. The Chernobyl thyroid cancer experience: Pathology. Clin. Oncol. (R. Coll. Radiol.) 2011, 23, 261–267. [Google Scholar] [CrossRef]
- Zablotska, L.B.; Bogdanova, T.I.; Ron, E.; Epstein, O.V.; Robbins, J.; Likhtarev, I.A.; Hatch, M.; Markov, V.V.; Bouville, A.C.; Olijnyk, V.A.; et al. A cohort study of thyroid cancer and other thyroid diseases after the Chornobyl accident: Dose-response analysis of thyroid follicular adenomas detected during first screening in Ukraine (1998-2000). Am. J. Epidemiol. 2008, 167, 305–312. [Google Scholar] [CrossRef]
- Taylor, A.J.; Croft, A.P.; Palace, A.M.; Winter, D.L.; Reulen, R.C.; Stiller, C.A.; Stevens, M.C.; Hawkins, M.M. Risk of thyroid cancer in survivors of childhood cancer: Results from the British Childhood Cancer Survivor Study. Int. J. Cancer 2009, 125, 2400–2405. [Google Scholar] [CrossRef]
- Ron, E.; Brenner, A. Non-malignant thyroid diseases after a wide range of radiation exposures. Radiat. Res. 2011, 174, 877–888. [Google Scholar] [CrossRef]
- Naing, S.; Collins, B.J.; Schneider, A.B. Clinical behavior of radiation-induced thyroid cancer: Factors related to recurrence. Thyroid 2009, 19, 479–485. [Google Scholar] [CrossRef]
- Tuttle, R.M.; Vaisman, F.; Tronko, M.D. Clinical presentation and clinical outcomes in Chernobyl-related paediatric thyroid cancers: What do we know now? What can we expect in the future? Clin. Oncol. (R. Coll. Radiol.) 2011, 23, 268–275. [Google Scholar] [CrossRef]
- Smida, J.; Salassidis, K.; Hieber, L.; Zitzelsberger, H.; Kellerer, A.M.; Demidchik, E.P.; Negele, T.; Spelsberg, F.; Lengfelder, E.; Werner, M.; et al. Distinct frequency of ret rearrangements in papillary thyroid carcinomas of children and adults from Belarus. Int. J. Cancer 1999, 80, 32–38. [Google Scholar] [CrossRef]
- Thomas, G.A.; Bunnell, H.; Cook, H.A.; Williams, E.D.; Nerovnya, A.; Cherstvoy, E.D.; Tronko, N.D.; Bogdanova, T.I.; Chiappetta, G.; Viglietto, G.; et al. High prevalence of RET/PTC rearrangements in Ukrainian and Belarussian post-Chernobyl thyroid papillary carcinomas: A strong correlation between RET/PTC3 and the solid-follicular variant. J. Clin. Endocrinol. Metab. 1999, 84, 4232–4238. [Google Scholar] [CrossRef]
- Powell, N.; Jeremiah, S.; Morishita, M.; Dudley, E.; Bethel, J.; Bogdanova, T.; Tronko, M.; Thomas, G. Frequency of BRAF T1796A mutation in papillary thyroid carcinoma relates to age of patient at diagnosis and not to radiation exposure. J. Pathol. 2005, 205, 558–564. [Google Scholar] [CrossRef]
- Unger, K.; Zurnadzhy, L.; Walch, A.; Mall, M.; Bogdanova, T.; Braselmann, H.; Hieber, L.; Tronko, N.; Hutzler, P.; Jeremiah, S.; et al. RET rearrangements in post-Chernobyl papillary thyroid carcinomas with a short latency analysed by interphase FISH. Br. J. Cancer 2006, 94, 1472–1477. [Google Scholar] [CrossRef]
- Hamatani, K.; Eguchi, H.; Ito, R.; Mukai, M.; Takahashi, K.; Taga, M.; Imai, K.; Cologne, J.; Soda, M.; Arihiro, K.; et al. RET/PTC rearrangements preferentially occurred in papillary thyroid cancer among atomic bomb survivors exposed to high radiation dose. Cancer Res. 2008, 68, 7176–7182. [Google Scholar] [CrossRef]
- Williams, E.D.; Abrosimov, A.; Bogdanova, T.; Demidchik, E.P.; Ito, M.; LiVolsi, V.; Lushnikov, E.; Rosai, J.; Tronko, M.D.; Tsyb, A.F.; et al. Morphologic characteristics of Chernobyl-related childhood papillary thyroid carcinomas are independent of radiation exposure but vary with iodine intake. Thyroid 2008, 18, 847–852. [Google Scholar] [CrossRef]
- Tuttle, R.M.; Lukes, Y.; Onstad, L.; Lushnikov, E.; Abrosimov, A.; Troshin, V.; Tsyb, A.; Davis, S.; Kopecky, K.J.; Francis, G. ret/PTC activation is not associated with individual radiation dose estimates in a pilot study of neoplastic thyroid nodules arising in Russian children and adults exposed to Chernobyl fallout. Thyroid 2008, 18, 839–846. [Google Scholar] [CrossRef]
- Detours, V.; Wattel, S.; Venet, D.; Hutsebaut, N.; Bogdanova, T.; Tronko, M.D.; Dumont, J.E.; Franc, B.; Thomas, G.; Maenhaut, C. Absence of a specific radiation signature in post-Chernobyl thyroid cancers. Br. J. Cancer 2005, 92, 1545–1552. [Google Scholar] [CrossRef]
- Detours, V.; Delys, L.; Libert, F.; Weiss Solis, D.; Bogdanova, T.; Dumont, J.E.; Franc, B.; Thomas, G.; Maenhaut, C. Genome-wide gene expression profiling suggests distinct radiation susceptibilities in sporadic and post-Chernobyl papillary thyroid cancers. Br. J. Cancer 2007, 97, 818–825. [Google Scholar] [CrossRef]
- Port, M.; Boltze, C.; Wang, Y.; Roper, B.; Meineke, V.; Abend, M. A radiation-induced gene signature distinguishes post-chernobyl from sporadic papillary thyroid cancers. Radiat. Res. 2007, 168, 639–649. [Google Scholar] [CrossRef]
- Maenhaut, C.; Detours, V.; Dom, G.; Handkiewicz-Junak, D.; Oczko-Wojciechowska, M.; Jarzab, B. Gene expression profiles for radiation-induced thyroid cancer. Clin. Oncol. (R. Coll. Radiol.) 2011, 23, 282–288. [Google Scholar] [CrossRef]
- Stein, L.; Rothschild, J.; Luce, J.; Cowell, J.K.; Thomas, G.; Bogdanova, T.I.; Tronko, M.D.; Hawthorn, L. Copy number and gene expression alterations in radiation-induced papillary thyroid carcinoma from chernobyl pediatric patients. Thyroid 2010, 20, 475–487. [Google Scholar] [CrossRef]
- Ory, C.; Ugolin, N.; Levalois, C.; Lacroix, L.; Caillou, B.; Bidart, J.M.; Schlumberger, M.; Diallo, I.; de Vathaire, F.; Hofman, P.; et al. Gene expression signature discriminates sporadic from post-radiotherapy-induced thyroid tumors. Endocr. Relat. Cancer 2011, 18, 193–206. [Google Scholar] [CrossRef]
- Ugolin, N.; Ory, C.; Lefevre, E.; Benhabiles, N.; Hofman, P.; Schlumberger, M.; Chevillard, S. Stategy to find molecular signatures in a small series of rare cancers: Validation for radiation-induced breast and thyroid tumors. PloS One 2011, 6. [Google Scholar] [CrossRef]
- Boltze, C.; Riecke, A.; Ruf, C.G.; Port, M.; Nizze, H.; Kugler, C.; Miethke, C.; Wiest, N.; Abend, M. Sporadic and radiation-associated papillary thyroid cancers can be distinguished using routine immunohistochemistry. Oncol. Rep. 2009, 22, 459–467. [Google Scholar] [CrossRef]
- Achille, M.; Boukheris, H.; Caillou, B.; Talbot, M.; de Vathaire, F.; Sabatier, L.; Desmaze, C.; Schlumberger, M.; Soria, J.C. Expression of cell cycle biomarkers and telomere length in papillary thyroid carcinoma: A comparative study between radiation-associated and spontaneous cancers. Am. J. Clin. Oncol. 2009, 32, 1–8. [Google Scholar] [CrossRef]
- Kimmel, R.R.; Zhao, L.P.; Nguyen, D.; Lee, S.; Aronszajn, M.; Cheng, C.; Troshin, V.P.; Abrosimov, A.; Delrow, J.; Tuttle, R.M.; et al. Microarray comparative genomic hybridization reveals genome-wide patterns of DNA gains and losses in post-Chernobyl thyroid cancer. Radiat. Res. 2006, 166, 519–531. [Google Scholar] [CrossRef]
- Hess, J.; Thomas, G.; Braselmann, H.; Bauer, V.; Bogdanova, T.; Wienberg, J.; Zitzelsberger, H.; Unger, K. Gain of chromosome band 7q11 in papillary thyroid carcinomas of young patients is associated with exposure to low-dose irradiation. Proc. Natl. Acad. Sci. USA 2011, 108, 9595–9600. [Google Scholar] [CrossRef]
- Zitzelsberger, H.; Unger, K. DNA copy number alterations in radiation-induced thyroid cancer. Clin. Oncol. (R. Coll. Radiol.) 2011, 23, 289–296. [Google Scholar] [CrossRef]
- Ein-Dor, L.; Zuk, O.; Domany, E. Thousands of samples are needed to generate a robust gene list for predicting outcome in cancer. Proc. Natl. Acad. Sci. USA 2006, 103, 5923–5928. [Google Scholar] [CrossRef]
- Amundson, S.A.; Do, K.T.; Vinikoor, L.; Koch-Paiz, C.A.; Bittner, M.L.; Trent, J.M.; Meltzer, P.; Fornace, A.J., Jr. Stress-specific signatures: Expression profiling of p53 wild-type and -null human cells. Oncogene 2005, 24, 4572–4579. [Google Scholar] [CrossRef]
- Quackenbush, J. Microarray analysis and tumor classification. N. Engl. J. Med. 2006, 354, 2463–2472. [Google Scholar] [CrossRef]
- Hadj-Hamou, N.S.; Ugolin, N.; Ory, C.; Britzen-Laurent, N.; Sastre-Garau, X.; Chevillard, S.; Malfoy, B. A transcriptome signature distinguished sporadic from postradiotherapy radiation-induced sarcomas. Carcinogenesis 2011, 32, 929–934. [Google Scholar] [CrossRef]
- Broeks, A.; Braaf, L.M.; Wessels, L.F.; van de Vijver, M.; de Bruin, M.L.; Stovall, M.; Russell, N.S.; van Leeuwen, F.E.; van ’t Veer, L.J. Radiation-associated breast tumors display a distinct gene expression profile. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 540–547. [Google Scholar] [CrossRef]
- Sanzari, J.K.; Nuth, M.; Kennedy, A.R. Induction of cytokine gene expression in human thyroid epithelial cells irradiated with HZE particles (iron ions). Radiat. Res. 2009, 172, 437–443. [Google Scholar] [CrossRef]
- Abou-El-Ardat, K.; Monsieurs, P.; Anastasov, N.; Atkinson, M.; Derradji, H.; de Meyer, T.; Bekaert, S.; van Criekinge, W.; Baatout, S. Low dose irradiation of thyroid cells reveals a unique transcriptomic and epigenetic signature in RET/PTC-positive cells. Mutat. Res. 2011. [Google Scholar] [CrossRef]
- Adachi, S.; Ryo, H.; Hongyo, T.; Nakajima, H.; Tsuboi-Kikuya, R.; Tokita, Y.; Matsuzuka, F.; Hiramatsu, K.; Fujikawa, K.; Itoh, T.; et al. Effects of fission neutrons on human thyroid tissues maintained in SCID mice. Mutat. Res. 2010, 696, 107–113. [Google Scholar] [CrossRef]
- Bouville, A.; Likhtarev, I.A.; Kovgan, L.N.; Minenko, V.F.; Shinkarev, S.M.; Drozdovitch, V.V. Radiation dosimetry for highly contaminated Belarusian, Russian and Ukrainian populations, and for less contaminated populations in Europe. Health Phys. 2007, 93, 487–501. [Google Scholar] [CrossRef]
- Drozdovitch, V.; Khrouch, V.; Maceika, E.; Zvonova, I.; Vlasov, O.; Bratilova, A.; Gavrilin, Y.; Goulko, G.; Hoshi, M.; Kesminiene, A.; et al. Reconstruction of radiation doses in a case-control study of thyroid cancer following the Chernobyl accident. Health Phys. 2010, 99, 1–16. [Google Scholar] [CrossRef]
- Ory, C.; Ugolin, N.; Hofman, P.; Schlumberger, M.; Chevillard, S. 2011; Unpublished work.
- ICRP, The 2007 Recommendations of the International Commission on Radiological Protection; Elsevier Science: Oxford, UK, 2007; Volume 103.
- Land, C.E. Low-dose extrapolation of radiation health risks: Some implications of uncertainty for radiation protection at low doses. Health Phys. 2009, 97, 407–415. [Google Scholar] [CrossRef]
- Mobbs, S.F.; Muirhead, C.R.; Harrison, J.D. Risks from ionising radiation: An HPA viewpoint paper for Safegrounds. J. Radiol. Prot. 2011, 31, 289–307. [Google Scholar] [CrossRef]
- Leenhardt, L.; Bernier, M.O.; Boin-Pineau, M.H.; Conte Devolx, B.; Marechaud, R.; Niccoli-Sire, P.; Nocaudie, M.; Orgiazzi, J.; Schlumberger, M.; Wemeau, J.L.; et al. Advances in diagnostic practices affect thyroid cancer incidence in France. Eur. J. Endocrinol. 2004, 150, 133–139. [Google Scholar] [CrossRef]
- Davies, L.; Welch, H.G. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 2006, 295, 2164–2167. [Google Scholar] [CrossRef]
- Albores-Saavedra, J.; Henson, D.E.; Glazer, E.; Schwartz, A.M. Changing patterns in the incidence and survival of thyroid cancer with follicular phenotype--papillary, follicular, and anaplastic: A morphological and epidemiological study. Endocr. Pathol. 2007, 18, 1–7. [Google Scholar] [CrossRef]
- Colonna, M.; Guizard, A.V.; Schvartz, C.; Velten, M.; Raverdy, N.; Molinie, F.; Delafosse, P.; Franc, B.; Grosclaude, P. A time trend analysis of papillary and follicular cancers as a function of tumour size: A study of data from six cancer registries in France (1983-2000). Eur. J. Cancer 2007, 43, 891–900. [Google Scholar] [CrossRef]
- Schroeder, A.; Mueller, O.; Stocker, S.; Salowsky, R.; Leiber, M.; Gassmann, M.; Lightfoot, S.; Menzel, W.; Granzow, M.; Ragg, T. The RIN: An RNA integrity number for assigning integrity values to RNA measurements. BMC Mol. Biol. 2006, 7. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Ory, C.; Ugolin, N.; Schlumberger, M.; Hofman, P.; Chevillard, S. Discriminating Gene Expression Signature of Radiation-Induced Thyroid Tumors after Either External Exposure or Internal Contamination. Genes 2012, 3, 19-34. https://doi.org/10.3390/genes3010019
Ory C, Ugolin N, Schlumberger M, Hofman P, Chevillard S. Discriminating Gene Expression Signature of Radiation-Induced Thyroid Tumors after Either External Exposure or Internal Contamination. Genes. 2012; 3(1):19-34. https://doi.org/10.3390/genes3010019
Chicago/Turabian StyleOry, Catherine, Nicolas Ugolin, Martin Schlumberger, Paul Hofman, and Sylvie Chevillard. 2012. "Discriminating Gene Expression Signature of Radiation-Induced Thyroid Tumors after Either External Exposure or Internal Contamination" Genes 3, no. 1: 19-34. https://doi.org/10.3390/genes3010019





