Flexible, Penetrating Brain Probes Enabled by Advances in Polymer Microfabrication
Abstract
:1. Introduction
2. Probe Fabrication and Material Selection
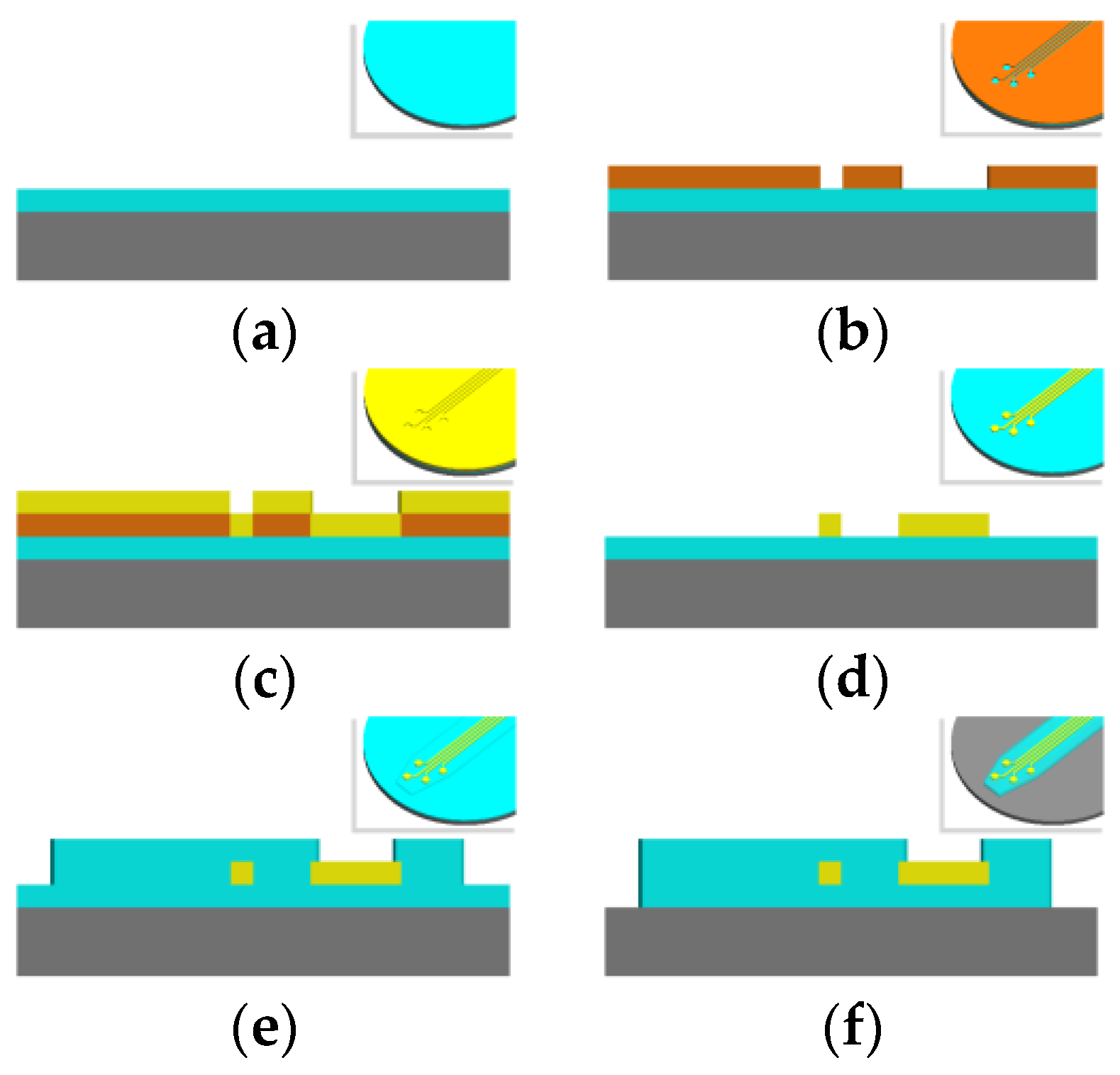
2.1. Basics of Microfabrication
2.2. Polymer Choices
2.3. Methods of Polymer Deposition
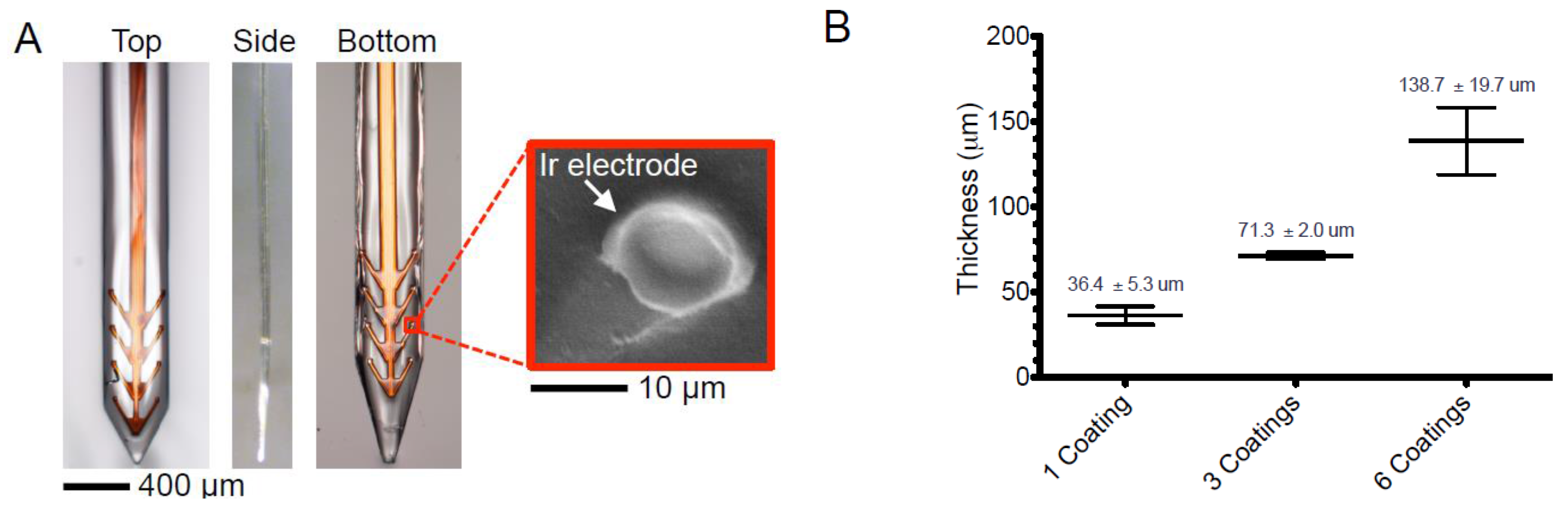
2.4. Choice of Conductive Layer: Deposition, Patterning, and Electrode Surface Modifications
3. Design Considerations for Fabricating Flexible, Neural Probes
3.1. Using Anchors to Attenuate Micromotion of Flexible Probes
3.2. Minimizing Cross-Sectional Footprint of Probes to Decrease Immune Response
3.3. Placement of Active Sites Away from Probe Body, or Deeper Along Body to Limit Tissue Disruption
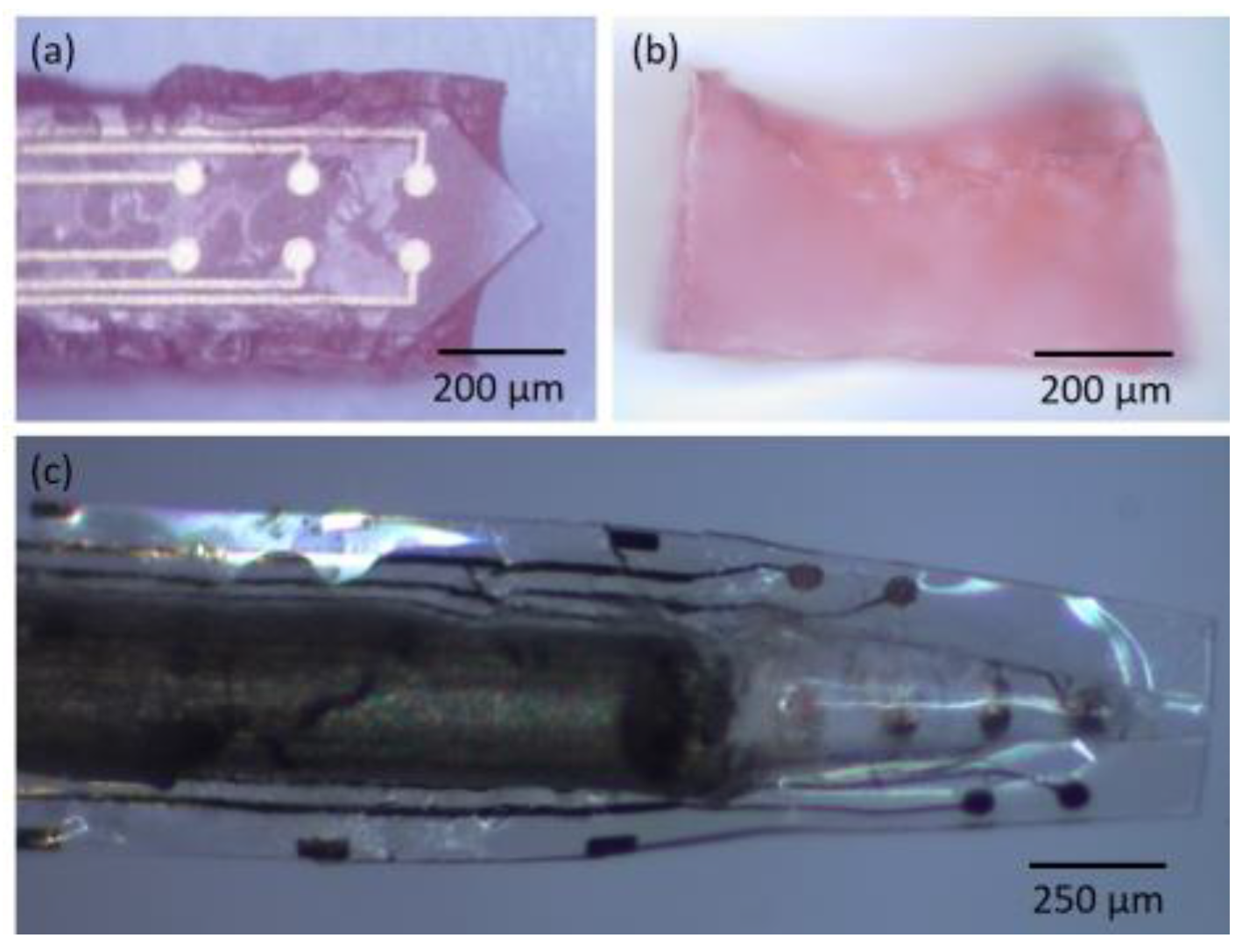
3.4. Open Architecture Design
3.5. Untethered Probes
4. Insertion Requirements
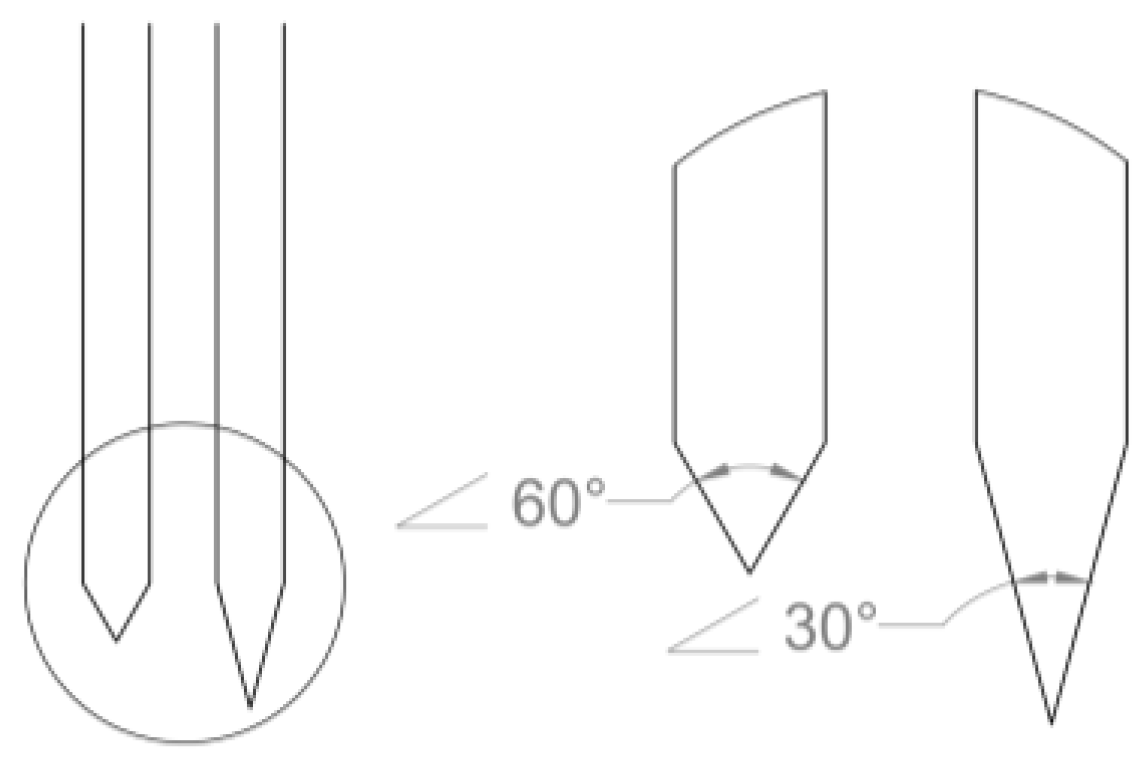
4.1. Determining Force of Penetration
4.1.1. Tissue Properties
4.1.2. Geometrical and Probe Surface Considerations
4.1.3. Variations in Insertion Speed
4.1.4. Current Consensus Regarding Penetration Force
4.2. Buckling Force Threshold Calculations
5. Techniques for Temporarily Stiffening Probes During Insertion
5.1. Coatings
5.1.1. Coating Materials
5.1.2. Coating Methods
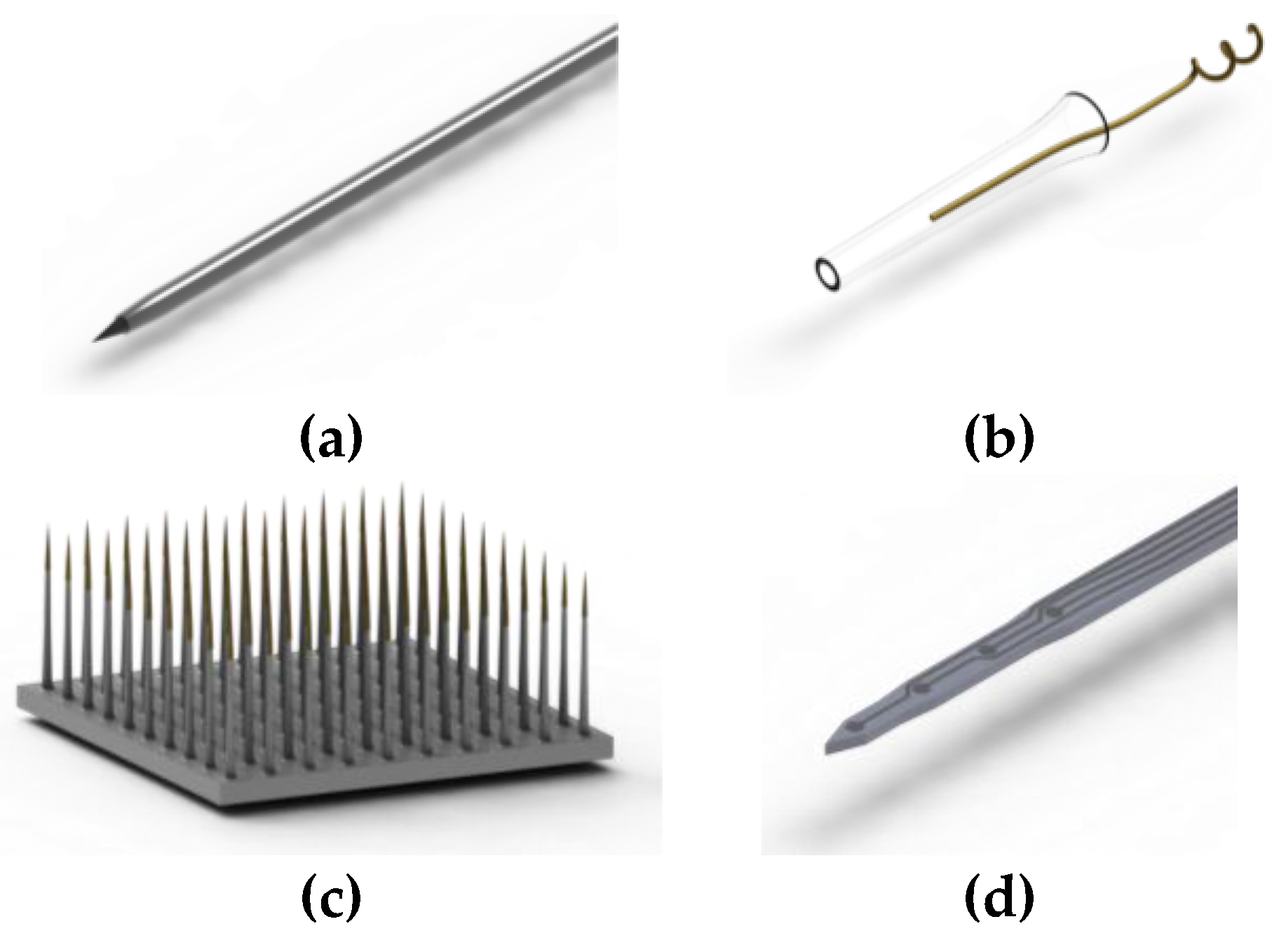
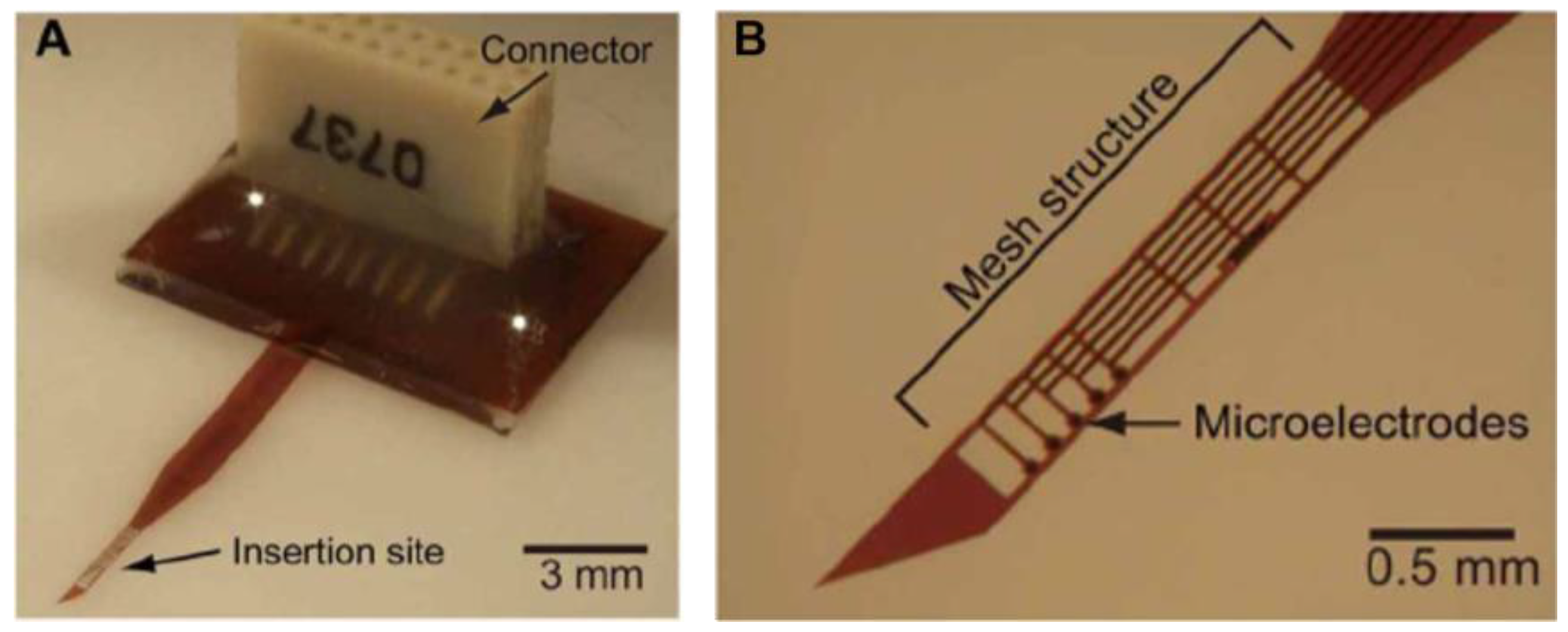
5.2. Structural Shuttle
5.3. Other Insertion Solutions
6. Packaging
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fattahi, P.; Yang, G.; Kim, G.; Abidian, M.R. A review of organic and inorganic biomaterials for neural interfaces. Adv. Mater. 2014, 26, 1846–1885. [Google Scholar] [CrossRef] [PubMed]
- Jorfi, M.; Skousen, J.L.; Weder, C.; Capadona, J.R. Progress towards biocompatible intracortical microelectrodes for neural interfacing applications. J. Neural Eng. 2015, 12, 011001. [Google Scholar] [CrossRef] [PubMed]
- HajjHassan, M.; Chodavarapu, V.; Musallam, S. NeuroMEMS: Neural probe microtechnologies. Sensors 2008, 8, 6704–6726. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, Q.; Li, Y.; Wang, Y.; Zhu, J.; Zhang, S.; Zheng, X. Long-term decoding stability of local field potentials from silicon arrays in primate motor cortex during a 2d center out task. J. Neural Eng. 2014, 11, 036009. [Google Scholar] [CrossRef] [PubMed]
- Vetter, R.J.; Williams, J.C.; Hetke, J.F.; Nunamaker, E.A.; Kipke, D.R. Chronic neural recording using silicon-substrate microelectrode arrays implanted in cerebral cortex. IEEE Trans. Biomed. Eng. 2004, 51, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.C.; Rennaker, R.L.; Kipke, D.R. Long-term neural recording characteristics of wire microelectrode arrays implanted in cerebral cortex. Brain Res. Protoc. 1999, 4, 303–313. [Google Scholar] [CrossRef]
- Takeuchi, S.; Suzuki, T.; Mabuchi, K.; Fujita, H. 3D flexible multichannel neural probe array. J. Micromech. Microeng. 2004, 14, 104–107. [Google Scholar] [CrossRef]
- Takeuchi, S.; Ziegler, D.; Yoshida, Y.; Mabuchi, K.; Suzuki, T. Parylene flexible neural probes integrated with microfluidic channels. Lab Chip 2005, 5, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Mercanzini, A.; Cheung, K.; Buhl, D.L.; Boers, M.; Maillard, A.; Colin, P.; Bensadoun, J.-C.; Bertsch, A.; Renaud, P. Demonstration of cortical recording using novel flexible polymer neural probes. Sens. Actuators A Phys. 2008, 143, 90–96. [Google Scholar] [CrossRef]
- Seymour, J.P.; Kipke, D.R. Neural probe design for reduced tissue encapsulation in CNS. Biomaterials 2007, 28, 3594–3607. [Google Scholar] [CrossRef] [PubMed]
- Sharp, A.; Ortega, A.M.; Restrepo, D.; Curran-Everett, D.; Gall, K. In vivo penetration mechanics and mechanical properties of mouse brain tissue at micrometer scales. IEEE Trans. Biomed. Eng. 2009, 56, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Elkin, B.S.; Azeloglu, E.U.; Costa, K.D.; Morrison, B. Mechanical heterogeneity of the rat hippocampus measured by atomic force microscope indentation. J. Neurotrauma 2007, 24, 812–822. [Google Scholar] [CrossRef] [PubMed]
- Elkin, B.S.; Ilankovan, A.; Morrison, B. Age-dependent regional mechanical properties of the rat hippocampus and cortex. J. Biomech. Eng. 2010, 132, 011010. [Google Scholar] [CrossRef] [PubMed]
- Christ, A.F.; Franze, K.; Gautier, H.; Moshayedi, P.; Fawcett, J.; Franklin, R.J.; Karadottir, R.T.; Guck, J. Mechanical difference between white and gray matter in the rat cerebellum measured by scanning force microscopy. J. Biomech. 2010, 43, 2986–2992. [Google Scholar] [CrossRef] [PubMed]
- Maikos, J.T.; Elias, R.A.; Shreiber, D.I. Mechanical properties of dura mater from the rat brain and spinal cord. J. Neurotrauma 2008, 25, 38–51. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.-Y. Numerical human head model for traumatic injury assessment. KSME Int. J. 2001, 15, 995–1001. [Google Scholar] [CrossRef]
- McGarvey, K.A.; Lee, J.M.; Boughner, D.R. Mechanical suitability of glycerol-preserved human dura mater for construction of prosthetic cardiac valves. Biomaterials 1984, 5, 109–117. [Google Scholar] [CrossRef]
- Kelly, P.F. Properties of Materials; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Suzuki, T.; Mabuchi, K.; Takeuchi, S. A 3D flexible parylene probe array for multichannel neural recording. In Proceedings of the 1st International IEEE/EMBS Conference on Neural Engineering (NER), Capri Island, Italy, 22 March 2003; pp. 154–156.
- Rousche, P.J.; Pellinen, D.S.; Pivin, D.P.; Williams, J.C.; Vetter, R.J.; Kipke, D.R. Flexible polyimide-based intracortical electrode arrays with bioactive capability. IEEE Trans. Biomed. Eng. 2001, 48, 361–371. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, D.P.; Nichols, T.R.; Allen, M.G. Flexible microelectrode arrays with integrated insertion devices. In Proceedings of the 14th IEEE International Conference on Micro Electro Mechanical Systems (MEMS), Interlaken, Switzerland, 21 January 2001; pp. 216–219.
- Stieglitz, T.; Beutel, H.; Meyer, J.-U. A flexible, light-weight multichannel sieve electrode with integrated cables for interfacing regenerating peripheral nerves. Sens. Actuators A Phys. 1997, 60, 240–243. [Google Scholar] [CrossRef]
- Subbaroyan, J.; Martin, D.C.; Kipke, D.R. A finite-element model of the mechanical effects of implantable microelectrodes in the cerebral cortex. J. Neural Eng. 2005, 2, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, L.A.; Ju, Y.-E.; Marg, B.; Osterfield, M.; Janmey, P.A. Neurite branching on deformable substrates. Neuroreport 2002, 13, 2411–2415. [Google Scholar] [CrossRef] [PubMed]
- Balgude, A.; Yu, X.; Szymanski, A.; Bellamkonda, R. Agarose gel stiffness determines rate of drg neurite extension in 3D cultures. Biomaterials 2001, 22, 1077–1084. [Google Scholar] [CrossRef]
- Normand, V.; Lootens, D.L.; Amici, E.; Plucknett, K.P.; Aymard, P. New insight into agarose gel mechanical properties. Biomacromolecules 2000, 1, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Moshayedi, P.; Ng, G.; Kwok, J.C.; Yeo, G.S.; Bryant, C.E.; Fawcett, J.W.; Franze, K.; Guck, J. The relationship between glial cell mechanosensitivity and foreign body reactions in the central nervous system. Biomaterials 2014, 35, 3919–3925. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.K.; Park, D.J.; Skousen, J.L.; Hess-Dunning, A.E.; Tyler, D.J.; Rowan, S.J.; Weder, C.; Capadona, J.R. Mechanically-compliant intracortical implants reduce the neuroinflammatory response. J. Neural Eng. 2014, 11, 056014. [Google Scholar] [CrossRef] [PubMed]
- McConnell, G.C.; Rees, H.D.; Levey, A.I.; Gutekunst, C.A.; Gross, R.E.; Bellamkonda, R.V. Implanted neural electrodes cause chronic, local inflammation that is correlated with local neurodegeneration. J. Neural Eng. 2009, 6, 056003. [Google Scholar] [CrossRef] [PubMed]
- Sohal, H.S.; Jackson, A.; Jackson, R.; Clowry, G.J.; Vassilevski, K.; O’Neill, A.; Baker, S.N. The sinusoidal probe: A new approach to improve electrode longevity. Front. Neuroeng. 2014, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Meng, E. Biomedical Microsystems; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar]
- Judy, J.W. Microelectromechanical systems (MEMS): Fabrication, design and applications. Smart Mater. Struct. 2001, 10, 1115. [Google Scholar] [CrossRef]
- United States Pharmacopoeia. Biological reactivity tests, in vivo. In U.S. Pharmacopeia, 39th ed.; The United States Pharmacopeial Convention Inc.: Rockville, MD, USA, 2016. [Google Scholar]
- International Organization for Standardization. Biological Evaluation of Medical Devices—Part 1: Evaluation and Testing within a Risk Management Process; ISO 10993-1:2009; International Organization for Standardization: Geneva, Switzerland, 2009. [Google Scholar]
- Kim, B.J.; Meng, E. Review of polymer MEMS micromachining. J. Micromech. Microeng. 2015, 26, 013001. [Google Scholar] [CrossRef]
- Hassler, C.; Boretius, T.; Stieglitz, T. Polymers for neural implants. J. Polym. Sci. B Polym. Phys. 2011, 49, 18–33. [Google Scholar] [CrossRef]
- Bae, S.H.; Che, J.-H.; Seo, J.-M.; Jeong, J.; Kim, E.T.; Lee, S.W.; Koo, K.-I.; Suaning, G.J.; Lovell, N.H.; Kim, S.J. In vitro biocompatibility of various polymer-based microelectrode arrays for retinal prosthesismicroelectrode arrays for retinal prosthesis. Investig. Ophthalmol. Vis. Sci. 2012, 53, 2653–2657. [Google Scholar] [CrossRef] [PubMed]
- Stieglitz, T.; Schuettler, M.; Rubehn, B.; Boretius, T.; Badia, J.; Navarro, X. Evaluation of polyimide as substrate material for electrodes to interface the peripheral nervous system. In Proceedings of the 5th International IEEE/EMBS Conference on Neural Engineering (NER), Cancun, Mexico, 27 April 2011; pp. 529–533.
- Jiang, X.; Sui, X.; Lu, Y.; Yan, Y.; Zhou, C.; Li, L.; Ren, Q.; Chai, X. In vitro and in vivo evaluation of a photosensitive polyimide thin-film microelectrode array suitable for epiretinal stimulation. J. Neuro Eng. Rehabil. 2013, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Scholten, K.; Meng, E. Materials for microfabricated implantable devices: A review. Lab Chip 2015, 15, 4256–4272. [Google Scholar] [CrossRef] [PubMed]
- Robin, C.; Vishnoi, A.; Jonnalagadda, K.N. Mechanical behavior and anisotropy of spin-coated SU-8 thin films for MEMS. J. Microelectromech. Syst. 2014, 23, 168–180. [Google Scholar] [CrossRef]
- Lee, K.; Massia, S.; He, J. Biocompatible benzocyclobutene-based intracortical neural implant with surface modification. J. Micromech. Microeng. 2005, 15, 2149. [Google Scholar] [CrossRef]
- LaBianca, N.C.; Gelorme, J.D. High-aspect-ratio resist for thick-film applications. Proc. SPIE 1995, 2438. [Google Scholar] [CrossRef]
- Madou, M.J. Fundamentals of Microfabrication: The Science of Miniaturization; CRC Press: Boca Raton, FL, USA, 2002. [Google Scholar]
- Lago, N.; Ceballos, D.; Rodrı́guez, F.J.; Stieglitz, T.; Navarro, X. Long term assessment of axonal regeneration through polyimide regenerative electrodes to interface the peripheral nerve. Biomaterials 2005, 26, 2021–2031. [Google Scholar] [CrossRef] [PubMed]
- Koeneman, B.A.; Lee, K.-K.; Singh, A.; He, J.; Raupp, G.B.; Panitch, A.; Capco, D.G. An ex vivo method for evaluating the biocompatibility of neural electrodes in rat brain slice cultures. J. Neurosci. Methods 2004, 137, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Kotzar, G.; Freas, M.; Abel, P.; Fleischman, A.; Roy, S.; Zorman, C.; Moran, J.M.; Melzak, J. Evaluation of MEMS materials of construction for implantable medical devices. Biomaterials 2002, 23, 2737–2750. [Google Scholar] [CrossRef]
- Nemani, K.V.; Moodie, K.L.; Brennick, J.B.; Su, A.; Gimi, B. In vitro and in vivo evaluation of SU-8 biocompatibility. Mater. Sci. Eng. C 2013, 33, 4453–4459. [Google Scholar] [CrossRef] [PubMed]
- Kozai, T.D.; Kipke, D.R. Insertion shuttle with carboxyl terminated self-assembled monolayer coatings for implanting flexible polymer neural probes in the brain. J. Neurosci. Methods 2009, 184, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Tien, L.; Chen, F.; Kaplan, D.; Berke, J.; Yoon, E. A multi-shank silk-backed parylene neural probe for reliable chronic recording. In Proceedings of the 17th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS & EUROSENSORS XXVII), Barcelona, Spain, 16 June 2013; pp. 888–891.
- Park, S.; Jang, Y.; Kim, H.C.; Chun, K. Fabrication of drug delivery system with piezoelectric micropump for neural probe. In Proceedings of the 23rd International Technical Conference on Circuits/Systems, Computers and Communications, Shimonoseki, Japan, 6 July 2008; pp. 1149–1152.
- Lee, H.J.; Son, Y.; Kim, J.; Lee, C.J.; Yoon, E.-S.; Cho, I.-J. A multichannel neural probe with embedded microfluidic channels for simultaneous in vivo neural recording and drug delivery. Lab Chip 2015, 15, 1590–1597. [Google Scholar] [CrossRef] [PubMed]
- Agorelius, J.; Tsanakalis, F.; Friberg, A.; Thorbergsson, P.T.; Pettersson, L.M.; Schouenborg, J. An array of highly flexible electrodes with a tailored configuration locked by gelatin during implantation-initial evaluation in cortex cerebri of awake rats. Front. Neurosci. 2015, 9, 331. [Google Scholar] [CrossRef] [PubMed]
- Johnston, I.; McCluskey, D.; Tan, C.; Tracey, M. Mechanical characterization of bulk sylgard 184 for microfluidics and microengineering. J. Micromech. Microeng. 2014, 24, 035017. [Google Scholar] [CrossRef]
- Lee, J.N.; Jiang, X.; Ryan, D.; Whitesides, G.M. Compatibility of mammalian cells on surfaces of poly (dimethylsiloxane). Langmuir 2004, 20, 11684–11691. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Jun, S.B.; Lee, H.J.; Kim, J.; Lee, S.W.; Im, C.; Shin, H.C.; Chang, J.W.; Kim, S.J. A flexible depth probe using liquid crystal polymer. IEEE Trans. Biomed. Eng. 2012, 59, 2085–2094. [Google Scholar] [PubMed]
- Jeong, J.; Bae, S.H.; Seo, J.-M.; Chung, H.; Kim, S.J. Long-term evaluation of a liquid crystal polymer (LCP)-based retinal prosthesis. J. Neural Eng. 2016, 13, 025004. [Google Scholar] [CrossRef] [PubMed]
- Hess-Dunning, A.E.; Smith, R.L.; Zorman, C.A. Development of polynorbornene as a structural material for microfluidics and flexible bioMEMS. J. Appl. Polym. Sci. 2014, 131, 40969. [Google Scholar] [CrossRef]
- Keesara, V.V.; Durand, D.M.; Zorman, C.A. Fabrication and characterization of flexible, microfabricated neural electrode arrays made from liquid crystal polymer and polynorbornene. In Proceedings of the 2006 MRS Spring Meeting, San Francisco, CA, USA, 17–21 April 2006.
- Hess, A.E.; Capadona, J.R.; Shanmuganathan, K.; Hsu, L.; Rowan, S.J.; Weder, C.; Tyler, D.J.; Zorman, C.A. Development of a stimuli-responsive polymer nanocomposite toward biologically optimized, MEMS-based neural probes. J. Micromech. Microeng. 2011, 21, 054009. [Google Scholar] [CrossRef]
- Ejserholm, F.; Vastesson, A.; Haraldsson, T.; van der Wijngaart, W.; Schouenborg, J.; Wallman, L.; Bengtsson, M. A polymer neural probe with tunable flexibility. In Proceedings of the 6th International IEEE/EMBS Conference on Neural Engineering (NER), San Diego, CA, USA, 6 November 2013; pp. 691–694.
- Wester, B.; Lee, R.; LaPlaca, M. Development and characterization of in vivo flexible electrodes compatible with large tissue displacements. J. Neural Eng. 2009, 6, 024002. [Google Scholar] [CrossRef] [PubMed]
- Winslow, B.D.; Christensen, M.B.; Yang, W.-K.; Solzbacher, F.; Tresco, P.A. A comparison of the tissue response to chronically implanted parylene-c-coated and uncoated planar silicon microelectrode arrays in rat cortex. Biomaterials 2010, 31, 9163–9172. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Kuo, J.T.; Hara, S.A.; Lee, C.D.; Yu, L.; Gutierrez, C.A.; Hoang, T.Q.; Pikov, V.; Meng, E. 3D parylene sheath neural probe for chronic recordings. J. Neural Eng. 2013, 10, 045002. [Google Scholar] [CrossRef] [PubMed]
- Fortin, J.B.; Lu, T.-M. Chemical Vapor Deposition Polymerization: The Growth and Properties of Parylene Thin Films; Springer Science & Business Media: Norwell, MA, USA, 2003. [Google Scholar]
- Gilgunn, P.J.; Khilwani, R.; Kozai, T.D.Y.; Weber, D.J.; Cui, X.T.; Erdos, G.; Ozdoganlar, O.B.; Fedder, G.K. An ultra-compliant, scalable neural probe with molded biodissolvable delivery vehicle. In Proceedings of the 2012 IEEE 25th International Conference on Micro Electro Mechanical Systems (MEMS), Paris, France, 29 January–1 February 2012; pp. 56–59.
- Ziegler, D.; Suzuki, T.; Takeuchi, S. Fabrication of flexible neural probes with built-in microfluidic channels by thermal bonding of parylene. J. Microelectromech. Syst. 2006, 15, 1477–1482. [Google Scholar] [CrossRef]
- Kuo, W.-C.; Chen, C.-W. Novel fabrication method for high-aspect-ratio suspended parylene structures. In Proceedings of the 6th IEEE International Conference on Nano/Micro Engineered and Molecular Systems (NEMS), Kaohsiung, Taiwan, 20 February 2011; pp. 585–588.
- Ochoa, M.; Wei, P.; Wolley, A.J.; Otto, K.J.; Ziaie, B. A hybrid pdms-parylene subdural multi-electrode array. Biomed. Microdevices 2013, 15, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Meacham, K.W.; Hochman, S.; DeWeerth, S.P. A pdms-based conical-well microelectrode array for surface stimulation and recording of neural tissues. IEEE Trans. Biomed. Eng. 2010, 57, 2485–2494. [Google Scholar] [PubMed]
- Rodger, D.C.; Fong, A.J.; Li, W.; Ameri, H.; Ahuja, A.K.; Gutierrez, C.; Lavrov, I.; Zhong, H.; Menon, P.R.; Meng, E. Flexible parylene-based multielectrode array technology for high-density neural stimulation and recording. Sens. Actuators B Chem. 2008, 132, 449–460. [Google Scholar] [CrossRef]
- Liu, C. Recent developments in polymer MEMS. Adv. Mater. 2007, 19, 3783–3790. [Google Scholar] [CrossRef]
- Nordström, M.; Johansson, A.; Nogueron, E.S.; Clausen, B.; Calleja, M.; Boisen, A. Investigation of the bond strength between the photo-sensitive polymer SU-8 and gold. Microelectron. Eng. 2005, 78, 152–157. [Google Scholar] [CrossRef]
- Chang, J.H.-C.; Lu, B.; Tai, Y.-C. Adhesion-enhancing surface treatments for parylene deposition. In Proceedings of the 16th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS), Beijing, China, 5 June 2011; pp. 390–393.
- Kim, W.-S.; Yun, I.-H.; Lee, J.-J.; Jung, H.-T. Evaluation of mechanical interlock effect on adhesion strength of polymer–metal interfaces using micro-patterned surface topography. Int. J. Adhes. Adhes. 2010, 30, 408–417. [Google Scholar] [CrossRef]
- Von Metzen, R.P.; Stieglitz, T. The effects of annealing on mechanical, chemical, and physical properties and structural stability of Parylene C. Biomed. Microdevices 2013, 15, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Liston, E.; Martinu, L.; Wertheimer, M. Plasma surface modification of polymers for improved adhesion: A critical review. J. Adhes. Sci. Technol. 1993, 7, 1091–1127. [Google Scholar] [CrossRef]
- Henze, D.A.; Borhegyi, Z.; Csicsvari, J.; Mamiya, A.; Harris, K.D.; Buzsáki, G. Intracellular features predicted by extracellular recordings in the hippocampus in vivo. J. Neurophysiol. 2000, 84, 390–400. [Google Scholar] [PubMed]
- Ghodssi, R.; Lin, P. MEMS Materials and Processes Handbook; Springer Science & Business Media: New York, NY, USA, 2011. [Google Scholar]
- Norlin, P.; Kindlundh, M.; Mouroux, A.; Yoshida, K.; Hofmann, U.G. A 32-site neural recording probe fabricated by drie of SOI substrates. J. Micromech. Microeng. 2002, 12, 414. [Google Scholar] [CrossRef]
- Ejserholm, F.; Kohler, P.; Granmo, M.; Schouenborg, J.; Bengtsson, M.; Wallman, L. μ-foil polymer electrode array for intracortical neural recordings. IEEE J. Trans. Eng. Health Med. 2014, 2, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Felix, S.; Shah, K.; George, D.; Tolosa, V.; Tooker, A.; Sheth, H.; Delima, T.; Pannu, S. Removable silicon insertion stiffeners for neural probes using polyethylene glycol as a biodissolvable adhesive. In Proceedings of the IEEE 34th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), San Diego, CA, USA, 28 August 2012; pp. 871–874.
- Robblee, L.; Lefko, J.; Brummer, S. Activated Ir: An electrode suitable for reversible charge injection in saline solution. J. Electrochem. Soc. 1983, 130, 731–733. [Google Scholar] [CrossRef]
- Mercanzini, A.; Cheung, K.; Buhl, D.; Boers, M.; Maillard, A.; Colin, P.; Bensadoun, J.-C.; Bertsch, A.; Carleton, A.; Renaud, P. Demonstration of cortical recording and reduced inflammatory response using flexible polymer neural probes. In Proceedings of the 20th IEEE International Conference on Micro Electro Mechanical Systems (MEMS), Hyogo, Japan, 21 January 2007; pp. 573–576.
- Weiland, J.D.; Anderson, D.J.; Humayun, M.S. In vitro electrical properties for iridium oxide versus titanium nitride stimulating electrodes. IEEE Trans. Biomed. Eng. 2002, 49, 1574–1579. [Google Scholar] [CrossRef] [PubMed]
- Cogan, S.F.; Plante, T.; Ehrlich, J. Sputtered iridium oxide films (SIROFS) for low-impedance neural stimulation and recording electrodes. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), San Francisco, CA, USA, 1 September 2004; pp. 4153–4156.
- Cogan, S.F.; Ehrlich, J.; Plante, T.D.; Smirnov, A.; Shire, D.B.; Gingerich, M.; Rizzo, J.F. Sputtered iridium oxide films for neural stimulation electrodes. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 89, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Fan, B.; Zhu, Y.; Rechenberg, R.; Becker, M.F.; Li, W. A flexible, large-scale diamond-polymer chemical sensor for neurotransmitter detection. In Proceedings of the Hilton Head Workshop 2016: A Solid-State Sensors, Actuators and Microsystems Workshop, Hilton Head, SC, USA, 5–9 June 2016; pp. 320–323.
- David-Pur, M.; Bareket-Keren, L.; Beit-Yaakov, G.; Raz-Prag, D.; Hanein, Y. All-carbon-nanotube flexible multi-electrode array for neuronal recording and stimulation. Biomed. Microdevices 2014, 16, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Tien, L.W.; Wu, F.; Tang-Schomer, M.D.; Yoon, E.; Omenetto, F.G.; Kaplan, D.L. Silk as a multifunctional biomaterial substrate for reduced glial scarring around brain-penetrating electrodes. Adv. Funct. Mater. 2013, 23, 3185–3193. [Google Scholar] [CrossRef]
- Cogan, S.F. Neural stimulation and recording electrodes. Annu. Rev. Biomed. Eng. 2008, 10, 275–309. [Google Scholar] [CrossRef] [PubMed]
- Ejserholm, F.; Kohler, P.; Bengtsson, M.; Jorntell, H.; Schouenborg, J.; Wallman, L. A polymer based electrode array for recordings in the cerebellum. In Proceedings of the 2011 5th International IEEE/EMBS Conference on Neural Engineering (NER), Cancun, Mexico, 27 April–1 May 2011; pp. 376–379.
- Petrossians, A.; Whalen, J.J.; Weiland, J.D.; Mansfeld, F. Electrodeposition and characterization of thin-film platinum-iridium alloys for biological interfaces. J. Electrochem. Soc. 2011, 158, D269–D276. [Google Scholar] [CrossRef]
- Cui, X.; Hetke, J.F.; Wiler, J.A.; Anderson, D.J.; Martin, D.C. Electrochemical deposition and characterization of conducting polymer polypyrrole/pss on multichannel neural probes. Sens. Actuators A Phys. 2001, 93, 8–18. [Google Scholar] [CrossRef]
- Yang, J.; Kim, D.H.; Hendricks, J.L.; Leach, M.; Northey, R.; Martin, D.C. Ordered surfactant-templated poly (3,4-ethylenedioxythiophene)(PEDOT) conducting polymer on microfabricated neural probes. Acta Biomater. 2005, 1, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Stauffer, W.R.; Cui, X.T. Polypyrrole doped with 2 peptide sequences from laminin. Biomaterials 2006, 27, 2405–2413. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, K.A.; Uram, J.D.; Yang, J.; Martin, D.C.; Kipke, D.R. Chronic neural recordings using silicon microelectrode arrays electrochemically deposited with a poly(3,4-ethylenedioxythiophene) (PEDOT) film. J. Neural Eng. 2006, 3, 59. [Google Scholar] [CrossRef] [PubMed]
- George, P.M.; Lyckman, A.W.; LaVan, D.A.; Hegde, A.; Leung, Y.; Avasare, R.; Testa, C.; Alexander, P.M.; Langer, R.; Sur, M. Fabrication and biocompatibility of polypyrrole implants suitable for neural prosthetics. Biomaterials 2005, 26, 3511–3519. [Google Scholar] [CrossRef] [PubMed]
- Castagnola, V.; Descamps, E.; Lecestre, A.; Dahan, L.; Remaud, J.; Nowak, L.G.; Bergaud, C. Parylene-based flexible neural probes with PEDOT coated surface for brain stimulation and recording. Biosensors Bioelectron. 2015, 67, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Guimard, N.K.; Gomez, N.; Schmidt, C.E. Conducting polymers in biomedical engineering. Prog. Polym. Sci. 2007, 32, 876–921. [Google Scholar] [CrossRef]
- Fomani, A.A.; Mansour, R.R. Fabrication and characterization of the flexible neural microprobes with improved structural design. Sens. Actuators A Phys. 2011, 168, 233–241. [Google Scholar] [CrossRef]
- Metz, S.; Bertsch, A.; Bertrand, D.; Renaud, P. Flexible polyimide probes with microelectrodes and embedded microfluidic channels for simultaneous drug delivery and multi-channel monitoring of bioelectric activity. Biosens. Bioelectron. 2004, 19, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- Köhler, P.; Linsmeier, C.E.; Thelin, J.; Bengtsson, M.; Jörntell, H.; Garwicz, M.; Schouenborg, J.; Wallman, L. Flexible multi electrode brain-machine interface for recording in the cerebellum. In Proceedings of the IEEE 31st Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), Minneapolis, MN, USA, 2 September 2009; pp. 536–538.
- Wu, F.; Im, M.; Yoon, E. A flexible fish-bone-shaped neural probe strengthened by biodegradable silk coating for enhanced biocompatibility. In Proceedings of the 16th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS), Beijing, China, 5 June 2011; pp. 966–969.
- Sanders, J.; Stiles, C.; Hayes, C. Tissue response to single-polymer fibers of varying diameters: Evaluation of fibrous encapsulation and macrophage density. J. Biomed. Mater. Res. 2000, 52, 231–237. [Google Scholar] [CrossRef]
- Bernatchez, S.F.; Parks, P.J.; Gibbons, D.F. Interaction of macrophages with fibrous materials in vitro. Biomaterials 1996, 17, 2077–2086. [Google Scholar] [CrossRef]
- Szarowski, D.H.; Andersen, M.D.; Retterer, S.; Spence, A.J.; Isaacson, M.; Craighead, H.G.; Turner, J.N.; Shain, W. Brain responses to micro-machined silicon devices. Brain Res. 2003, 983, 23–35. [Google Scholar] [CrossRef]
- Thelin, J.; Jorntell, H.; Psouni, E.; Garwicz, M.; Schouenborg, J.; Danielsen, N.; Linsmeier, C.E. Implant size and fixation mode strongly influence tissue reactions in the CNS. PLoS ONE 2011, 6, e16267. [Google Scholar] [CrossRef] [PubMed]
- Stice, P.; Gilletti, A.; Panitch, A.; Muthuswamy, J. Thin microelectrodes reduce GFAP expression in the implant site in rodent somatosensory cortex. J. Neural Eng. 2007, 4, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Edel, D.J.; Toi, V.; McNeil, V.M.; Clark, L.D. Factors influencing the biocompatibility of insertable silicon microshafts in cerebral cortex. IEEE Trans. Biomed. Eng. 1992, 39, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Woolley, A.J.; Desai, H.A.; Otto, K.J. Chronic intracortical microelectrode arrays induce non-uniform, depth-related tissue responses. J. Neural Eng. 2013, 10, 026007. [Google Scholar] [CrossRef] [PubMed]
- Welkenhuysen, M.; Andrei, A.; Ameye, L.; Eberle, W.; Nuttin, B. Effect of insertion speed on tissue response and insertion mechanics of a chronically implanted silicon-based neural probe. IEEE Trans. Biomed. Eng. 2011, 58, 3250–3259. [Google Scholar] [CrossRef] [PubMed]
- Duvvuri, M.; Jiang, Z.; Kruskal, P.; Xie, C.; Suo, Z.; Fang, Y.; Lieber, C.M. Syringe-injectable electronics. Nat. Nanotechnol. 2015, 10, 629–636. [Google Scholar]
- Sridharan, A.; Rajan, S.D.; Muthuswamy, J. Long-term changes in the material properties of brain tissue at the implant-tissue interface. J. Neural Eng. 2013, 10, 066001. [Google Scholar] [CrossRef] [PubMed]
- Muthuswamy, J.; Gilletti, A.; Jain, T.; Okandan, M. Microactuated neural probes to compensate for brain micromotion. In Proceedings of the IEEE 25th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), Cancun, Mexico, 17 September 2003; pp. 1941–1943.
- Biran, R.; Martin, D.C.; Tresco, P.A. The brain tissue response to implanted silicon microelectrode arrays is increased when the device is tethered to the skull. J. Biomed. Mater. Res. A 2007, 82, 169–178. [Google Scholar] [CrossRef] [PubMed]
- McKee, C.T.; Last, J.A.; Russell, P.; Murphy, C.J. Indentation versus tensile measurements of young’s modulus for soft biological tissues. Tissue Eng. B Rev. 2011, 17, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Hajdu, M.A.; Heistad, D.; Siems, J.; Baumbach, G. Effects of aging on mechanics and composition of cerebral arterioles in rats. Circ. Res. 1990, 66, 1747–1754. [Google Scholar] [CrossRef] [PubMed]
- Gefen, A.; Gefen, N.; Zhu, Q.; Raghupathi, R.; Margulies, S.S. Age-dependent changes in material properties of the brain and braincase of the rat. J. Neurotrauma 2003, 20, 1163–1177. [Google Scholar] [CrossRef] [PubMed]
- Jensen, W.; Yoshida, K.; Hofmann, U.G. In vivo implant mechanics of flexible, silicon-based acreo microelectrode arrays in rat cerebral cortex. IEEE Trans. Biomed. Eng. 2006, 53, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Andrei, A.; Welkenhuysen, M.; Nuttin, B.; Eberle, W. A response surface model predicting the in vivo insertion behavior of micromachined neural implants. J. Neural Eng. 2011, 9, 016005. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, N.H.; Hoffmann, R.; Kisban, S.; Stieglitz, T.; Paul, O.; Ruther, P. Comparative study on the insertion behavior of cerebral microprobes. In Proceedings of the IEEE 29th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), Lyon, France, 23 August 2007; pp. 4711–4714.
- Bjornsson, C.; Oh, S.J.; Al-Kofahi, Y.; Lim, Y.; Smith, K.; Turner, J.; De, S.; Roysam, B.; Shain, W.; Kim, S.J. Effects of insertion conditions on tissue strain and vascular damage during neuroprosthetic device insertion. J. Neural Eng. 2006, 3, 196. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.D.; Kao, O.E.; Kipke, D.R. Spatiotemporal ph dynamics following insertion of neural microelectrode arrays. J. Neurosci. Methods 2007, 160, 276–287. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Gutierrez, C.A.; Gerhardt, G.A.; Meng, E. parylene-based electrochemical-MEMS force sensor array for assessing neural probe insertion mechanics. In Proceedings of the 25th IEEE International Conference on Micro Electro Mechanical Systems (MEMS), Paris, France, 29 January 2012; pp. 124–127.
- Lecomte, A.; Castagnola, V.; Descamps, E.; Dahan, L.; Blatché, M.C.; Dinis, T.M.; Leclerc, E.; Egles, C.; Bergaud, C. Silk and peg as means to stiffen a parylene probe for insertion in the brain: Toward a double time-scale tool for local drug delivery. J. Micromech. Microeng. 2015, 25, 125003. [Google Scholar] [CrossRef]
- Chen, C.-H. Three-dimensional flexible microprobe for recording the neural signal. J. Micro/Nanolithogr. MEMS MOEMS 2010, 9, 031007. [Google Scholar] [CrossRef]
- Lo, M.C.; Wang, S.; Singh, S.; Damodaran, V.B.; Kaplan, H.M.; Kohn, J.; Shreiber, D.I.; Zahn, J.D. Coating flexible probes with an ultra fast degrading polymer to aid in tissue insertion. Biomed. Microdevices 2015, 17, 34. [Google Scholar] [CrossRef] [PubMed]
- Lewitus, D.; Smith, K.L.; Shain, W.; Kohn, J. Ultrafast resorbing polymers for use as carriers for cortical neural probes. Acta Biomater. 2011, 7, 2483–2491. [Google Scholar] [CrossRef] [PubMed]
- Lind, G.; Linsmeier, C.E.; Thelin, J.; Schouenborg, J. Gelatine-embedded electrodes-a novel biocompatible vehicle allowing implantation of highly flexible microelectrodes. J. Neural Eng. 2010, 7, 046005. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Zhu, H.; He, J. Improving mechanical stiffness of coated benzocyclobutene (BCB) based neural implant. In Proceedings of the IEEE 26th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), San Francisco, CA, USA, 1 September 2004; pp. 4298–4301.
- Xiang, Z.; Yen, S.-C.; Xue, N.; Sun, T.; Tsang, W.M.; Zhang, S.; Liao, L.-D.; Thakor, N.V.; Lee, C. Ultra-thin flexible polyimide neural probe embedded in a dissolvable maltose-coated microneedle. J. Micromech. Microeng. 2014, 24, 065015. [Google Scholar] [CrossRef]
- Bourke, S.L.; Kohn, J. Polymers derived from the amino acid l-tyrosine: Polycarbonates, polyarylates and copolymers with poly(ethylene glycol). Adv. Drug Deliv. Rev. 2003, 55, 447–466. [Google Scholar] [CrossRef]
- Kozai, T.D.; Gugel, Z.; Li, X.; Gilgunn, P.J.; Khilwani, R.; Ozdoganlar, O.B.; Fedder, G.K.; Weber, D.J.; Cui, X.T. Chronic tissue response to carboxymethyl cellulose based dissolvable insertion needle for ultra-small neural probes. Biomaterials 2014, 35, 9255–9268. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Wang, B. Biodegradation of silk biomaterials. Int. J. Mol. Sci. 2009, 10, 1514–1524. [Google Scholar] [CrossRef] [PubMed]
- Hooper, K.A.; Macon, N.D.; Kohn, J. Comparative histological evaluation of new tyrosine-derived polymers and poly (L-lactic acid) as a function of polymer degradation. J. Biomed. Mater. Res. 1998, 41, 443–454. [Google Scholar] [CrossRef]
- Ertel, S.I.; Kohn, J. Evaluation of a series of tyrosine-derived polycarbonates as degradable biomaterials. J. Biomed. Mater. Res. 1994, 28, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.J.; Park, J.; Karageorgiou, V.; Kim, U.J.; Valluzzi, R.; Cebe, P.; Kaplan, D.L. Water-stable silk films with reduced β-sheet content. Adv. Funct. Mater. 2005, 15, 1241–1247. [Google Scholar] [CrossRef]
- Hu, X.; Shmelev, K.; Sun, L.; Gil, E.S.; Park, S.H.; Cebe, P.; Kaplan, D.L. Regulation of silk material structure by temperature-controlled water vapor annealing. Biomacromolecules 2011, 12, 1686–1696. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Hu, X.; Wang, X.; Kluge, J.A.; Lu, S.; Cebe, P.; Kaplan, D.L. Water-insoluble silk films with silk I structure. Acta Biomater. 2010, 6, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Metallo, C.; Trimmer, B.A. Silk coating as a novel delivery system and reversible adhesive for stiffening and shaping flexible probes. J. Biol. Methods 2015, 2, 13. [Google Scholar] [CrossRef]
- Vepari, C.; Kaplan, D.L. Silk as a biomaterial. Prog. Polym. Sci. 2007, 32, 991–1007. [Google Scholar] [CrossRef] [PubMed]
- Alcantar, N.A.; Aydil, E.S.; Israelachvili, J.N. Polyethylene glycol-coated biocompatible surfaces. J. Biomed. Mater. Res. 2000, 51, 343–351. [Google Scholar] [CrossRef]
- Biran, R.; Martin, D.C.; Tresco, P.A. Neuronal cell loss accompanies the brain tissue response to chronically implanted silicon microelectrode arrays. Exp. Neurol. 2005, 195, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Kipke, D.R.; Pellinen, D.S.; Vetter, R.J. Advanced neural implants using thin-film polymers. In Proceedings of the IEEE International Symposium on Circuits and Systems (ISCAS), Scottsdale, AZ, USA, 26–29 May 2002; pp. 173–176.
- Richter, A.; Xie, Y.; Schumacher, A.; Löffler, S.; Kirch, R.D.; Al-Hasani, J.; Rapoport, D.H.; Kruse, C.; Moser, A.; Tronnier, V.; et al. A simple implantation method for flexible, multisite microelectrodes into rat brains. Front. Neuroeng. 2013, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.; Capadona, J.; Miller, R.H.; Healy, B.; Shanmuganathan, K.; Rowan, S.J.; Weder, C.; Tyler, D.J. Mechanically adaptive intracortical implants improve the proximity of neuronal cell bodies. J. Neural Eng. 2011, 8, 066011. [Google Scholar] [CrossRef] [PubMed]
- Ware, T.; Simon, D.; Arreaga-Salas, D.E.; Reeder, J.; Rennaker, R.; Keefer, E.W.; Voit, W. Fabrication of responsive, softening neural interfaces. Adv. Funct. Mater. 2012, 22, 3470–3479. [Google Scholar] [CrossRef]
- Egert, D.; Peterson, R.L.; Najafi, K. Parylene microprobes with engineered stiffness and shape for improved insertion. In Proceedings of the 16th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS), Beijing, China, 5–9 June 2011; pp. 198–201.
- Andrei, A.; Tutunjyan, N.; Verbinnen, G.; VanPut, S.; Krylychkina, O.; Eberle, W.; Musa, S. Fabrication and successful in vivo implantation of a flexible neural implant with a hybrid polyimide-silicon design. In Proceedings of the IEEE 34th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), San Diego, CA, USA, 28 August–1 September 2012; pp. 3890–3893.
- Barz, F.; Ruther, P.; Takeuchi, S.; Paul, O. Mechanically adaptive silicon-based neural probes for chronic high-resolution neural recording. Proc. Eng. 2015, 120, 952–955. [Google Scholar] [CrossRef]
- Weltman, A.; Xu, H.; Scholten, K.; Berger, T.W.; Meng, E. Deep brain targeting strategy for bare parylene neural probe arrays. In Proceedings of the Hilton Head Workshop 2016: A Solid-State Sensors, Actuators and Microsystems Workshop, Hilton Head, SC, USA, 5–9 June 2016.
- Patel, P.R.; Na, K.; Zhang, H.; Kozai, T.D.; Kotov, N.A.; Yoon, E.; Chestek, C.A. Insertion of linear 8.4 μm diameter 16 channel carbon fiber electrode arrays for single unit recordings. J. Neural Eng. 2015, 12, 046009. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-C.; Lal, A. Detachable ultrasonic enabled inserter for neural probe insertion using biodissolvable polyethylene glycol. In Proceedings of the 18th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS), Anchorage, AL, USA, 21–25 June 2015; pp. 125–128.
- Jaroch, D.B.; Irazoqui, P.; Rickus, J.L. Flexible Neural Probe for Magnetic Insertion. U.S. Patent 8,761,898, 24 June 2014. [Google Scholar]
- Hungar, K.; Mokwa, W. Gold/tin soldering of flexible silicon chips onto polymer tapes. J. Micromech. Microeng. 2008, 18, 064002. [Google Scholar] [CrossRef]
- Cheung, K.C.; Renaud, P.; Tanila, H.; Djupsund, K. Flexible polyimide microelectrode array for in vivo recordings and current source density analysis. Biosens. Bioelectron. 2007, 22, 1783–1790. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y.X.; Furukawa, S.; Samejima, K.; Hironaka, N.; Kashino, M. Photosensitive-polyimide based method for fabricating various neural electrode architectures. Front. Neuroeng. 2012, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.-U.; Stieglitz, T.; Scholz, O.; Haberer, W.; Beutel, H. High density interconnects and flexible hybrid assemblies for active biomedical implants. IEEE Trans. Adv. Packag. 2001, 24, 366–374. [Google Scholar] [CrossRef]
- Stieglitz, T.; Beutel, H.; Keller, R.; Schuettler, M.; Meyer, J.U. Flexible, polyimide-based neural interfaces. In Proceedings of the Seventh International Conference on Microelectronics for Neural, Fuzzy and Bio-Inspired Systems, Granada, Spain, 9 April 1999; pp. 112–119.
- Stieglitz, T.; Schuettler, M.; Meyer, J.-U. Micromachined, polyimide-based devices for flexible neural interfaces. Biomed. Microdevices 2000, 2, 283–294. [Google Scholar] [CrossRef]
- Wise, K.; Anderson, D.; Hetke, J.; Kipke, D.; Najafi, K. Wireless implantable microsystems: High-density electronic interfaces to the nervous system. Proc. IEEE 2004, 92, 76–97. [Google Scholar] [CrossRef]
- Chang, J.H.-C.; Huang, R.; Tai, Y.-C. High-density ic chip integration with parylene pocket. In Proceedings of the 6th IEEE International Conference on Nano/Micro Engineered and Molecular Systems (NEMS), Kaohsiung, Taiwan, 20–23 Feburary 2011; pp. 1067–1070.
- Huang, R.; Pang, C.; Tai, Y.; Emken, J.; Ustun, C.; Andersen, R.; Burdick, J. Integrated parylene-cabled silicon probes for neural prosthetics. In Proceedings of the 21st IEEE International Conference on Micro Electro Mechanical Systems (MEMS), Tucson, AR, USA, 13–17 January 2008; pp. 240–243.
- Tummala, R. Fundamentals of Microsystems Packaging; McGraw Hill Professional: New York, NY, USA, 2001. [Google Scholar]
- Cheng, M.Y.; Je, M.; Tan, K.L.; Tan, E.L.; Lim, R.; Yao, L.; Li, P.; Park, W.T.; Phua, E.J.R.; Gan, C.L.; et al. A low-profile three-dimensional neural probe array using a silicon lead transfer structure. J. Micromech. Microeng. 2013, 23, 095013. [Google Scholar] [CrossRef]
- Kisban, S.; Kenntner, J.; Janssen, P.; Metzen, R.V.; Herwik, S.; Bartsch, U.; Stieglitz, T.; Paul, O.; Ruther, P. A novel assembly method for silicon-based neural devices. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering, Munich, Germany, 2009; pp. 107–110.
- Ok, J.; Greenberg, R.J.; Talbot, N.H.; Little, J.S.; Dai, R.; Neysmith, J.M.; McClure, K.H. Package for an Implantable Neural Stimulation Device. U.S. Patent 8,996,118, 31 March 2015. [Google Scholar]
- Chunyan, L.; Frank, E.S.; Richard, G.A.; Chong, H.A.; Ian, P. Polymer flip-chip bonding of pressure sensors on a flexible kapton film for neonatal catheters. J. Micromech. Microeng. 2005, 15, 1729. [Google Scholar]
- Du, J.; Blanche, T.J.; Harrison, R.R.; Lester, H.A.; Masmanidis, S.C. Multiplexed, high density electrophysiology with nanofabricated neural probes. PLoS ONE 2011, 6, e26204. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-C.; Kim, Y.-H. Review paper: Flip chip bonding with anisotropic conductive film (ACF) and nonconductive adhesive (NCA). Curr. Appl. Phys. 2013, 13, S14–S25. [Google Scholar] [CrossRef]
- Dexerials Corporation. Anisotropic Conductive Film (ACF) for Film on Glass for Small-to-Medium-Sized FPDs; CP13341-18AA/CP13341-25AJ; Dexerials Corporation: Tokyo, Japan; Available online: http://www.dexerials.jp/en/products/a7/cp13341-18aa.html (accessed on 14 September 2016).
- Stieglitz, T. Manufacturing, assembling and packaging of miniaturized implants for neural prostheses and brain-machine interfaces. In Proceedings of the SPIE Europe Microtechnologies for the New Millennium, Dresden, Germany, 4 May 2009; pp. 73610–73620.
- Kim, E.G.R.; John, J.K.; Tu, H.G.; Zheng, Q.L.; Loeb, J.; Zhang, J.S.; Xu, Y. A hybrid silicon-parylene neural probe with locally flexible regions. Sens. Actuators B Chem. 2014, 195, 416–422. [Google Scholar] [CrossRef]
- Johnson, G.A.; Badea, A.; Brandenburg, J.; Cofer, G.; Fubara, B.; Liu, S.; Nissanov, J. Waxholm space: An image-based reference for coordinating mouse brain research. NeuroImage 2010, 53, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Lein, E.S.; Hawrylycz, M.J.; Ao, N.; Ayres, M.; Bensinger, A.; Bernard, A.; Boe, A.F.; Boguski, M.S.; Brockway, K.S.; Byrnes, E.J. Genome-wide atlas of gene expression in the adult mouse brain. Nature 2007, 445, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Papp, E.A.; Leergaard, T.B.; Calabrese, E.; Johnson, G.A.; Bjaalie, J.G. Waxholm space atlas of the sprague dawley rat brain. NeuroImage 2014, 97, 374–386. [Google Scholar] [CrossRef] [PubMed]
- Kjonigsen, L.J.; Lillehaug, S.; Bjaalie, J.G.; Witter, M.P.; Leergaard, T.B. Waxholm space atlas of the rat brain hippocampal region: Three-dimensional delineations based on magnetic resonance and diffusion tensor imaging. NeuroImage 2015, 108, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Sergejeva, M.; Papp, E.A.; Bakker, R.; Gaudnek, M.A.; Okamura-Oho, Y.; Boline, J.; Bjaalie, J.G.; Hess, A. Anatomical landmarks for registration of experimental image data to volumetric rodent brain atlasing templates. J. Neurosci. Methods 2015, 240, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Rumple, A.; McMurray, M.; Johns, J.; Lauder, J.; Makam, P.; Radcliffe, M.; Oguz, I. 3-dimensional diffusion tensor imaging (DTI) atlas of the rat brain. PLoS ONE 2013, 8, e67334. [Google Scholar] [CrossRef] [PubMed]
- Paxinos, G.; Huang, X.-F.; Toga, A.W. The Rhesus Monkey Brain in Stereotaxic Coordinates; Academic Press: Cambridge, MA, USA, 2000. [Google Scholar]
- Calabrese, E.; Badea, A.; Coe, C.L.; Lubach, G.R.; Shi, Y.; Styner, M.A.; Johnson, G.A. A diffusion tensor MRI atlas of the postmortem rhesus macaque brain. NeuroImage 2015, 117, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Amunts, K.; Kedo, O.; Kindler, M.; Pieperhoff, P.; Mohlberg, H.; Shah, N.; Habel, U.; Schneider, F.; Zilles, K. Cytoarchitectonic mapping of the human amygdala, hippocampal region and entorhinal cortex: Intersubject variability and probability maps. Anat. Embryol. 2005, 210, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Behrens, T.; Johansen-Berg, H.; Woolrich, M.; Smith, S.; Wheeler-Kingshott, C.; Boulby, P.; Barker, G.; Sillery, E.; Sheehan, K.; Ciccarelli, O. Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat. Neurosci. 2003, 6, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Bakker, R.; Tiesinga, P.; Kötter, R. The scalable brain atlas: Instant web-based access to public brain atlases and related content. Neuroinformatics 2015, 13, 353–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Species | Young’s Modulus Hippocampus | Young’s Modulus Cerebellum | Young’s Modulus Cerebral Cortex | Young’s Modulus Dura Mater |
|---|---|---|---|---|
| Mouse | - | - | ~7 kPa [11] | - |
| Rat | 0.1 [12]–1.2 kPa [13] | 0.3–0.45 kPa [14] | 0.03–1.75 kPa [13] | 0.4–1.2 MPa [15] |
| Human | - | - | - | 32 MPa [16], 62 MPa [17] |
| Property | Silicon | PDMS | Polyimide | Parylene C | SU-8 | LCP | BCB |
|---|---|---|---|---|---|---|---|
| Young’s Modulus (GPa) | 190 | 3.6 × 10−4–8.7 × 10−4 | 2.3–8.5 | 2.76 | 2.87–4.40 [41] | 10.6 | 3.1 [42] |
| Melting Temperature (°C) | 1414 | - | - | 290 | - | 280 | - |
| Thermal Decomposition Temperature (°C) | - | ~250 | >550 | - | 300–315 | - | - |
| Glass Transition Temperature (°C) | - | 350 (oxidation); 750 (degradation) | 325–410 | 90 | 200 [43] | - | >350 [42] |
| Degradation Temperature (°C) | - | 250 | 510–620 | 125 | 380 | - | - |
| Thermal conductivity (W/cm·K) | 1.56 [44] | 15–25 | 0.29 | 8.2 | 0.002–0.003 | - | 2.9 × 10−3 |
| Dielectric Constant | 11.9 [44] | 2.6–3.8 | 3.5 | 3.1 | 3.2 | 3.0 | 2.65 [42] |
| Achievable Thicknesses (µm) | - | 10–100 (spin coat) | 1–15 | 1–100 | 1–300 | 25–3000 | 7–130 |
| Biocompatibility | - | USP class VI | Yes (in vivo) [36,45] | USP class VI | Mild reactivity (in vivo) [36] | USP class VI | Yes (ex vivo) [46] |
| Type of Coating | Ref. | Coating Method | Substrate Material | Increase in Cross Sectional Area | Increase in Buckling Force Threshold | Scale of Dissolution | Byproducts of Coating and Body’s Mechanism of Clearance |
|---|---|---|---|---|---|---|---|
| Silk | [104] | Dip-coating | Polyimide | N/A | With coating, sufficient to insert into fish brain | 1–6 h anneal, dissolves in protease solution in 0.5–2.5 h | Peptides and amino acids, proteolytic degradation or assumed foreign body response [135] |
| [90] | Layer-by-layer casting in PDMS | Polyimide | 10 µm thick, with coating: to 70 or 1400 µm thick | 0.04 mN, with 70 µm thick coating 12 mN and with 1400 µm thick coating 105 mN. | - | Peptides and amino acids, proteolytic degradation or assumed foreign body response [135] | |
| [126] | PDMS mold | Parylene-C | 24 µm thick, with coating: 250 µm thick | 2.6 mN, with coating: 300 mN | Days–weeks depending on duration of water annealing | Peptides and amino acids, proteolytic degradation or assumed foreign body response [135] | |
| Polyethylene glycol (PEG) | [127] | Dip-coating | Parylene-C | 6 µm thick, with coating: 11 µm thick | With coating, sufficient to insert into Biogel | - | Unknown [129] |
| [8] | Pipetting PEG into Parylene channel | Parylene-C | 10 µm thick, with coating: 20 µm thick | 1 mN, with coating: 12 mN | 200 s | Unknown [129] | |
| [126] | PDMS mold | Parylene-C | 24 µm thick, with coating: 250 µm thick | 2.6 mN, with coating: 47 mN | Within minutes, depending on molecular weight [8,75] | Unknown [129] | |
| [53] | PMMA mold | Milled gold leads coated with Parylene-C | 12 µm thick, with coating: 137 µm thick | With coating, sufficient to insert into rat cortex | Within 3.5 h (gelatin mixture containing PEG) | Unknown [129] for PEG, gelatin breaks down into collagen, degraded by collagenase | |
| Tyrosine-derived | [129] | Dip-coating | Polyimide | 70 µm diameter, with coating: 180 µm diameter = 6.6x increase in cross-sectional area | With coating, sufficient to insert into agarose and parietal cortex of rat | 20 min in vitro, in vivo recordings achieved within 60 min | Non-enzymatic, degraded by random hydrolytic chain cleavage [136,137] |
| [128] | PDMS mold | SU-8 | 20 µm thick and 30 µm wide, with coating: 100 µm thick and 200 µm wide = 33x increase in cross-sectional area | 50 mN with 200 µm thick coating | 60 min in PBS, 120 min in agarose | Non-enzymatic, degraded by random hydrolytic chain cleavage [136,137] | |
| Carboxy-methyl-cellulose (CMC) | [66] | Silicon and polyvinyl siloxane (PVS) mold | Parylene | 2.7 µm thick and 10 µm wide, with coating: 135 µm thick, 100/300 µm wide = 500x–1500x increase in cross-sectional area | With coating, sufficient to insert into rat primary motor cortex | <3 min to become gel. Does not dissolve completely | Monosaccharides, dissolved in water [134] |
| [134] | Spin-casting into silicon mold in centrifuge | No probe, only testing shuttle | N/A | With coating, sufficient to insert into rat motor cortex | Estimated 20 min, in-vivo took days | Monosaccharides, dissolved in water [134] | |
| Sugars | [36] | Dip-coating | Polyimide | - | With coating, sufficient to insert into rat cortex | Dissolves immediately upon contact with cerebrospinal fluid | Monosaccharides, dissolved in water [134] |
| [131] | Dip-coating | Benzocyclobutene (BCB) | - | With coating, buckles upon insertion into brain (species not included), mineral oil allowed penetration | Dissolves immediately upon contact with cerebrospinal fluid mineral oil helps delay dissolution | Monosaccharides, dissolved in water [134] | |
| [132] | Drawing lithography (allows for sharp tip) | Polyimide | 10 µm wide and 10 µm thick, with coating: 40–300 µm added to each dimension | With coating increased up to 3.8 N | <100 s | Monosaccharides, dissolved in water [134] |
| Shuttle Type | Ref. | Coupling Method | Substrate Material | Increase in Cross Sectional Area | Increase in Buckling Force Threshold | Average Probe Displacement |
|---|---|---|---|---|---|---|
| Silicon, “Michigan styled“ neural probe as shuttle | [49] | Electronegative, self-assembled, carboxylic acid terminal monolayer | Polyimide, PDMS probes | Polyimide probe–125 µm thick, 196 wide; PDMS probe-100 µm thick, 200 µm wide. Shuttle added 15 µm of thickness and was 400 µm wide | With shuttle, sufficient to insert into motor cortex of rat | 23 µm with SAM layer, 2365 µm without |
| Silicon backing | [82] | PEG adhesive with wicking channel on silicon stiffener and flip chip alignment | Polyimide | - | With shuttle, sufficient to insert into 0.6% agarose phantom and prefrontal cortex of rat | ~28 µm |
| Nickel backing | [7,19] | Polyimide spin-coated onto electroplated Nickel, permanently attached stiffener | Polyimide | Polyimide probe 20 µm thick, Nickel backing 5 µm thick | With shuttle, sufficient to insert into rat cortex | N/A |
| Stainless steel microwire | [30] | PEG | Parylene C | Parylene encapsulated probe 20 µm thick, microwire 229 µm in diameter | With shuttle, sufficient to insert into rabbit cortex | N/A |
| Tungsten rod | [146] | None, aided by agarose block on top of brain | Polyimide | 20 µm thick, 350 µm wide, tungsten rod adds diameter of 175 µm = 3.5x increase in cross-sectional area | With shuttle sufficient to insert into rat subthalamic nucleus | 100 µm |
| Tungsten microwire | [64] | PEG | Parylene-C | Parylene probe 11 µm thick, tungsten microwire 250 µm thick | With shuttle sufficient to insert into rat cortex | 90 µm |
| Species and Reference | Hippocampus (mm) | Superior Colliculus (mm) | Substantia Nigra (mm) | Thalamus |
|---|---|---|---|---|
| Mouse [175,176] | 1.7–5.3 | 0–6.3 | 4.0–5.9 | 2.3–5.2 |
| Rat [177,178,179,180] | 1.8–9.5 | 0.5–6.3 | 6.8–8.8 | 3.7–7.9 |
| Monkey [181,182] | 19.3–38.0 | - | - | 16.4–30.5 |
| Human [179,183,184] | 73.7–105.3 | - | - | 53.4–84.8 |
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weltman, A.; Yoo, J.; Meng, E. Flexible, Penetrating Brain Probes Enabled by Advances in Polymer Microfabrication. Micromachines 2016, 7, 180. https://doi.org/10.3390/mi7100180
Weltman A, Yoo J, Meng E. Flexible, Penetrating Brain Probes Enabled by Advances in Polymer Microfabrication. Micromachines. 2016; 7(10):180. https://doi.org/10.3390/mi7100180
Chicago/Turabian StyleWeltman, Ahuva, James Yoo, and Ellis Meng. 2016. "Flexible, Penetrating Brain Probes Enabled by Advances in Polymer Microfabrication" Micromachines 7, no. 10: 180. https://doi.org/10.3390/mi7100180





