Do Overweight Adolescents Adhere to Dietary Intervention Messages? Twelve-Month Detailed Dietary Outcomes from Curtin University’s Activity, Food and Attitudes Program
Abstract
:1. Introduction
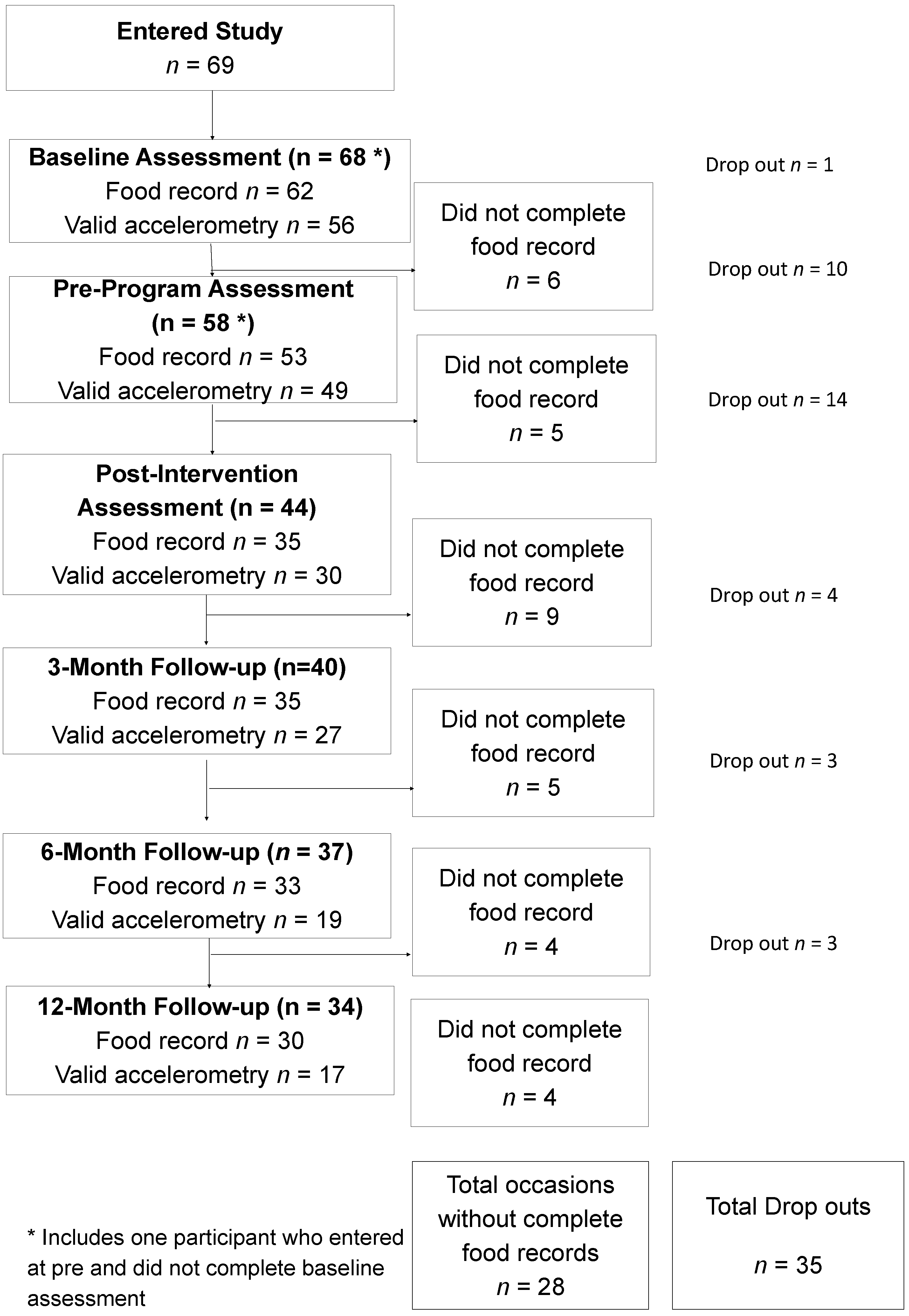
2. Experimental Section
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Dietary Intervention
2.5. Dietary Assessment
2.5.1. Nutrient Intake
2.5.2. Adherence to Intervention Messages
2.5.3. Eating Behaviors
2.6. Statistical Analysis
3. Results
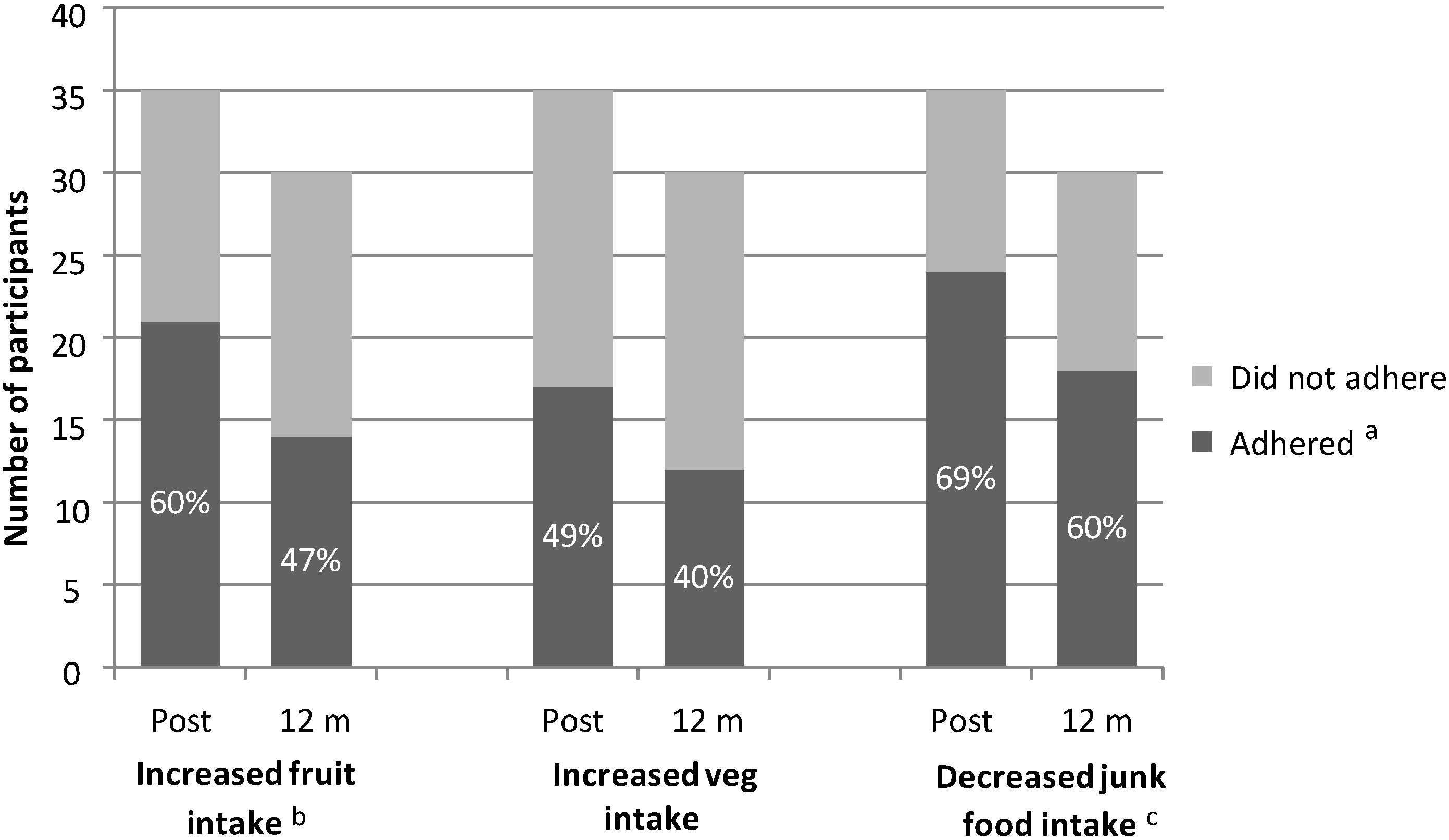
3.1. Adherence to Intervention Messages
3.2. Eating Behaviors
3.3. Detailed Nutrient Intakes
| Mean (SE) * | Period of Change | Mean Δ per Month (95% CI) | p-value Compared to Baseline to Pre d | ||
|---|---|---|---|---|---|
| Frequency of breakfast | Baseline | 3.0 (0.1) | |||
| Pre | 2.9 (0.1) | Baseline to Pre | −0.03 (−0.13, 0.08) | ref | |
| Post | 3.1 (0.1) | Pre to Post | 0.13 (−0.04, 0.29) | 0.208 | |
| 3 months | 3.4 (0.1) a,b | Post to 3 m | 0.07 (−0.03, 0.18) | 0.180 | |
| 6 months | 3.2 (0.2) | 3 m to 6 m | −0.05 (−0.18, 0.08) | 0.793 | |
| 12 months | 2.8 (0.2) | 6 m to 12 m | 0.07 (−0.14, −0.004) c | 0.475 | |
| Maintenance | Post-12 m | −0.03 (−0.06, 0) | 0.958 | ||
| Frequency of fast food | Baseline | 0.6 (0.05) | |||
| Pre | 0.5 (0.1) | Baseline to Pre | −0.01 (−0.06, 0.04) | ref | |
| Post | 0.4 (0.1) | Pre to Post | −0.05 (−0.15, 0.06) | 0.578 | |
| 3 months | 0.3 (0.1) a,b | Post to 3 m | −0.03 (−0.11, 0.05) | 0.639 | |
| 6 months | 0.3 (0.1) a,b | 3 m to 6 m | −0.01 (−0.08, 0.05) | 0.972 | |
| 12 months | 0.3 (0.1) a,b | 6 m to 12 m | −0.01 (−0.05, 0.04) | 0.881 | |
| Maintenance | −0.01 (−0.04, 0.01) | 0.907 | |||
| Frequency of sweetened beverages | Baseline | 1.5 (0.1) | |||
| Pre | 1.3 (0.1) | Baseline to Pre | −0.04 (−0.13, 0.05) | ref | |
| Post | 1.1 (0.1) a | Pre to Post | −0.14 (−0.03, 0.03) | 0.353 | |
| 3 months | 1.1 (0.1) a | Post to 3 m | 0.01 (−0.10, 0.12) | 0.521 | |
| 6 months | 0.9 (0.1) a,b | 3 m to 6 m | −0.06 (−0.17, 0.07) | 0.800 | |
| 12 months | 0.8 (0.1) a,b | 6 m to 12 m | −0.02 (−0.09, 0.05) | 0.759 | |
| Maintenance | Post to 12 m | −0.02 (−0.05, 0.01) | 0.741 | ||
| Perceived daily fruit serves | Baseline | 1.6 (0.1) | |||
| Pre | 1.5 (0.1) | Baseline to Pre | −0.03 (−0.10, 0.04) | ref | |
| Post | 1.9 (0.1) a,b | Pre to Post | 0.17 (0.06, 0.28) c | 0.011 | |
| 3 months | 1.8 (0.1) b | Post to 3 m | −0.02 (−0.10, 0.06) | 0.892 | |
| 6 months | 1.8 (0.1) b | 3 m to 6 m | −0.01 (−0.09, 0.06) | 0.785 | |
| 12 months | 1.9 (0.1) b | 6 m to 12 m | 0.01 (−0.04, 0.06) | 0.333 | |
| Maintenance | Post to 12 m | 0 (−0.03, 0.02) | 0.476 | ||
| Perceived daily vegetable serves | Baseline | 2.5 (0.1) | |||
| Pre | 2.4 (0.1) | Baseline to Pre | −0.03 (−0.13, 0.07) | ref | |
| Post | 2.9 (0.1) a,b | Pre to Post | 0.25 (0.07, 0.42) c | 0.022 | |
| 3 months | 3.0 (0.1) a,b | Post to 3 m | 0.02 (−0.11, 0.15) | 0.557 | |
| 6 months | 3.1 (0.1) a,b | 3 m to 6 m | 0.05 (−0.08, 0.17) | 0.351 | |
| 12 months | 3.3 (0.2) a,b | 6 m to 12 m | 0.03 (−0.05, 0.11) | 0.348 | |
| Maintenance | Post to 12 m | 0.03 (−0.01, 0.08) | 0.272 | ||
| Perceived daily junk food serves | Baseline | 1.6 (0.1) | |||
| Pre | 1.7 (0.1) | Baseline to Pre | 0.03 (−0.08, 0.15) | ref | |
| Post | 1.5 (0.1) | Pre to Post | −0.07 (−0.21, 0.06) | 0.331 | |
| 3 months | 1.4 (0.1) | Post to 3 m | −0.03 (−0.13, 0.07) | 0.437 | |
| 6 months | 1.5 (0.1) | 3 m to 6 m | 0.07 (−0.04, 0.19) | 0.617 | |
| 12 months | 1.6 (0.2) | 6 m to 12 m | −0.01 (−0.08, 0.06) | 0.551 | |
| Maintenance | Post to 12 m | 0.01 (−0.03, 0.04) | 0.667 |
| Mean (SE) * | Period of Change | Mean Δ per Month (95% CI) | p-value Compared to Baseline to Pre d | ||
|---|---|---|---|---|---|
| Energy (kJ) | Baseline | 6969 (46.9) | |||
| Pre | 6972 (50.8) | Baseline to Pre | 1.0 (−50.5, 52.4) | ref | |
| Post | 6965 (60.0) | Pre to Post | −3.2 (−86.9, 80.3) | 0.942 | |
| 3 months | 6946 (58.2) | Post to 3 m | −6.7 (−58.4, 45.0) | 0.834 | |
| 6 months | 6987 (68.2) | 3 m to 6 m | 13.9 (−43.1, 71.0) | 0.745 | |
| 12 months | 7133 (86.0) | 6 m to 12 m | 24.2 (−10.4, 58.8) | 0.473 | |
| Maintenance | Post to 12 m | 13.9 (−2.2, 30.0) | 0.644 | ||
| Protein (g) | Baseline | 69.1 (1.4) | |||
| Pre | 74.5 (1.8) a | Baseline to Pre | 1.8 (0.2, 3.4) c | ref | |
| Post | 75.3 (2.3) a | Pre to Post | 0.4 (−2.7, 3.4) | 0.489 | |
| 3 months | 76.1 (2.1) a | Post to 3 m | 0.3 (−1.7, 2.2) | 0.213 | |
| 6 months | 76.6 (2.2) a | 3 m to 6 m | 0.2 (−1.7, 2.0) | 0.189 | |
| 12 months | 72.2 (2.5) a | 6 m to 12 m | −0.7 (−1.8, 0.4) | 0.010 | |
| Maintenance | . | Post to 12 m | −0.3 (−0.8, 0.3) | 0.015 | |
| Fat (g) | Baseline | 63.4 (1.3) | |||
| Pre | 66.0 (1.3) | Baseline to Pre | 0.8 (−0.5, 2.2) | ref | |
| Post | 59.3 (1.6) b | Pre to Post | −3.3 (−5.4, −1.2) c | 0.005 | |
| 3 months | 62.6 (1.6) | Post to 3 m | 1.1 (−0.3, 2.5) | 0.800 | |
| 6 months | 62.8 (1.8) | 3 m to 6 m | 0.1 (−1.4, 1.5) | 0.432 | |
| 12 months | 64.7 (1.8) | 6 m to 12 m | 0.3 (−0.5, 1.1) | 0.489 | |
| Maintenance | Post to 12m | 0.5 (0.1, 0.8) c | 0.568 | ||
| Saturated fat (g) | Baseline | 26.9 (0.8) | |||
| Pre | 27.5 (0.8) | Baseline to Pre | 0.2 (−0.6, 0.9) | ref | |
| Post | 23.6 (0.9) a b | Pre to Post | −2.0 (−3.1, −0.8) c | 0.011 | |
| 3 months | 25.4 (0.9) | Post to 3 m | 0.6 (−0.2, 1.4) | 0.416 | |
| 6 months | 25.8 (0.8) | 3 m to 6 m | 0.1 (−0.6, 0.9) | 0.939 | |
| 12 months | 26.5 (0.8) | 6 m to 12 m | 0.1 (−2.5, 0.4) | 0.854 | |
| Maintenance | Post to 12 m | 0.2 (0.1, 0.4) c | 0.876 | ||
| Carbo-hydrate (g) | Baseline | 202.1 (3.6) b | |||
| Pre | 188.9 (3.9) a | Baseline to Pre | −4.4 (−8.3, −0.5) c | ref | |
| Post | 199.4 (4.8) a | Pre to Post | 5.2 (−1.3, 11.8) | 0.032 | |
| 3 months | 189.1 (4.0) a b | Post to 3 m | −3.4 (−7.6, 0.7) | 0.739 | |
| 6 months | 190.0 (5.4) a b | 3 m to 6 m | 0.3 (−3.8, 4.4) | 0.110 | |
| 12 months | 196.1 (4.7) a b | 6 m to 12 m | 1.0 (−1.1, 3.2) | 0.018 | |
| Maintenance | Post to 12 m | −0.3 (−1.3, 0.8) | 0.048 | ||
| Sugar (g) | Baseline | 88.4 (3.5) | |||
| Pre | 76.2 (3.2) a | Baseline to Pre | −4.1 (−7.5, −0.7) c | ref | |
| Post | 83.6 (5.5) | Pre to Post | 3.7 (−2.9, 10.4) | 0.066 | |
| 3 months | 81.3 (4.1) | Post to 3 m | −0.8 (−5.3, 3.8) | 0.250 | |
| 6 months | 77.4 (4.9) | 3 m to 6 m | −1.3 (−5.3, 2.7) | 0.300 | |
| 12 months | 82.7 (4.6) | 6 m to 12 m | 0.9 (−1.2, 3.0) | 0.014 | |
| Maintenance | Post to 12 m | −0.1 (−1.1, 1.0) | 0.027 | ||
| Fiber (g) | Baseline | 16.1 (0.4) | |||
| Pre | 15.2 (0.5) | Baseline to Pre | −0.3 (−0.7, 0.1) | ref | |
| Post | 16.8 (0.5) b | Pre to Post | 0.8 (0.1, 1.4) c | 0.017 | |
| 3 months | 16.8 (0.6) b | Post to 3 m | 0 (−0.5, 0.5) | 0.326 | |
| 6 months | 18.4 (0.8) a b | 3 m to 6 m | 0.5 (−0.03, 1.1) | 0.016 | |
| 12 months | 17.1 (0.6) b | 6 m to 12 m | −0.2 (−0.5, 0.1) | 0.692 | |
| Maintenance | Post to 12 m | 0.03 (−0.1, 0.2) | 0.123 | ||
| kJ from protein (%) | Baseline | 17.5 (0.3) | |||
| Pre | 18.4 (0.4) | Baseline to Pre | 0.3 (−0.04, 0.7) | ref | |
| Post | 19.1 (0.5) a | Pre to Post | 0.4 (−0.3, 1.1) | 0.869 | |
| 3 months | 19.2 (0.5) a | Post to 3 m | 0.02 (−0.4, 0.5) | 0.327 | |
| 6 months | 19.4 (0.5) a | 3 m to 6 m | 0.05 (−0.4, 0.5) | 0.364 | |
| 12 months | 18.2 (0.6) | 6 m to 12 m | −0.2 (−0.5, 0.1) | 0.022 | |
| Maintenance | Post to 12 m | −0.1 (−0.2, 0.05) | 0.037 | ||
| kJ from fat (%) | Baseline | 33.1 (0.6) | |||
| Pre | 34.8 (0.6) | Baseline to Pre | 0.5 (−0.04, 1.1) | ref | |
| Post | 31.2 (0.8) b | Pre to Post | −1.7 (−2.7, −0.8) c | 0.001 | |
| 3 months | 33.9 (0.8) | Post to 3 m | 0.9 (0.1, 1.6) c | 0.471 | |
| 6 months | 33.5 (1.0) | 3 m to 6 m | −0.1 (−1.0, 0.7) | 0.212 | |
| 12 months | 34.1 (1.0) | 6 m to 12 m | 0.1 (−0.4, 0.5) | 0.224 | |
| Maintenance | Post to 12 m | 0.2 (0.05, 0.4) c | 0.343 | ||
| kJ from sat fat (%) | Baseline | 14.0 (0.4) | |||
| Pre | 14.4 (0.3) | Baseline to Pre | 0.1 (−0.2, 0.4) | ref | |
| Post | 12.3 (0.4) a b | Pre to Post | −1.1 (−1.6, −0.5) c | 0.002 | |
| 3 months | 13.8 (0.5) | Post to 3 m | 0.5 (0.1, 1.0) c | 0.146 | |
| 6 months | 13.8 (0.4) | 3 m to 6 m | 0.02 (−0.5, 0.5) | 0.706 | |
| 12 months | 14.0 (0.4) | 6 m to 12 m | 0.03 (−0.2, 0.2) | 0.611 | |
| Maintenance | Post to 12 m | 0.1 (0.1, 0.2) c | 0.902 | ||
| kJ from Carbo-hydrate (%) | Baseline | 46.6 (0.6) | |||
| Pre | 44.6 (0.7) a | Baseline to Pre | −0.7 (−1.3, −0.01) c | ref | |
| Post | 47.0 (1.0) | Pre to Post | 1.2 (−0.1, 2.5) | 0.032 | |
| 3 months | 44.0 (0.9) a | Post to 3 m | −1.0 (−2.0, −0.1) c | 0.547 | |
| 6 months | 44.3 (1.0) | 3 m to 6 m | 0.1 (−0.8, 1.0) | 0.164 | |
| 12 months | 44.7 (1.2) | 6 m to 12 m | 0.1 (−0.5, 0.6) | 0.093 | |
| Maintenance | Post to 12 m | −0.2 (−0.5, 0.1) | 0.181 | ||
| Calcium (mg) | Baseline | 601.8 (22.8) | |||
| Pre | 598.9 (25.0) | Baseline to Pre | −1.0 (−24.9, 22.9) | ref | |
| Post | 606.2 (25.5) | Pre to Post | 3.6 (−33.5, 40.7) | 0.864 | |
| 3 months | 663.6 (30.5) | Post to 3 m | 19.1 (−6.5, 44.7) | 0.255 | |
| 6 months | 646.6 (37.9) | 3 m to 6 m | −5.7 (−35.2, 23.9) | 0.811 | |
| 12 months | 663.9 (34.0) | 6 m to 12 m | 2.9 (−13.8, 19.5) | 0.784 | |
| Maintenance | Post to 12 m | 4.8 (−1.9, 11.5) | 0.635 |
4. Discussion
4.1. Adherence
4.2. Eating Behaviors
4.3. Nutrient Intakes
4.4. Dietary Assessment Methods
4.5. Strengths and Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Maggio, A.B.; Martin, X.E.; Saunders Gasser, C.; Gal-Duding, C.; Beghetti, M.; Farpour-Lambert, N.J.; Chamay-Weber, C. Medical and non-medical complications among children and adolescents with excessive body weight. BMC Pediatr. 2014, 14, 232. [Google Scholar] [PubMed]
- Trasande, L.; Chatterjee, S. The impact of obesity on health service utilization and costs in childhood. Obesity 2009, 17, 1749–1754. [Google Scholar] [CrossRef] [PubMed]
- Barlow, S.E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef] [PubMed]
- Oude Luttikhuis, H.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O'Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane. Database Syst. Rev. 2009, 1, CD001872. [Google Scholar] [PubMed]
- Collins, C.E.; Warren, J.M.; Neve, M.; McCoy, P.; Stokes, B. Systematic review of interventions in the management of overweight and obese children which include a dietary component. Int. J. Evid. Based Healthc. 2007, 5, 2–53. [Google Scholar] [PubMed]
- Ho, M.; Garnett, S.P.; Baur, L.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Effectiveness of lifestyle interventions in child obesity: Systematic review with meta-analysis. Pediatrics 2012, 130, e1647–e1671. [Google Scholar] [CrossRef] [PubMed]
- Denney-Wilson, E.; Baur, L. Adolescent obesity: Making a difference to the epidemic. Int. J. Adolesc. Med. Health 2007, 19, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Warren, J.; Neve, M.; McCoy, P.; Stokes, B.J. Measuring effectiveness of dietetic interventions in child obesity: A systematic review of randomized trials. Arch. Pediatr. Adolesc. Med. 2006, 160, 906–922. [Google Scholar] [CrossRef] [PubMed]
- Savoye, M.; Nowicka, P.; Shaw, M.; Yu, S.; Dziura, J.; Chavent, G.; O'Malley, G.; Serrecchia, J.B.; Tamborlane, W.V.; Caprio, S. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics 2011, 127, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Steele, R.G.; Aylward, B.S.; Jensen, C.D.; Cushing, C.C.; Davis, A.M.; Bovaird, J.A. Comparison of a family-based group intervention for youths with obesity to a brief individual family intervention: A practical clinical trial of positively fit. J. Pediatr. Psychol. 2012, 37, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Kelly, L.A.; Lane, C.J.; Ventura, E.E.; Byrd-Williams, C.E.; Alexandar, K.A.; Azen, S.P.; Chou, C.P.; Spruijt-Metz, D.; Weigensberg, M.J.; et al. Randomized control trial to improve adiposity and insulin resistance in overweight latino adolescents. Obesity 2009, 17, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- Shaibi, G.Q.; Konopken, Y.; Hoppin, E.; Keller, C.S.; Ortega, R.; Castro, F.G. Effects of a culturally grounded community-based diabetes prevention program for obese latino adolescents. Diabetes Educ. 2012, 38, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Shrewsbury, V.; O’Connor, J.; Steinbeck, K.; Stevenson, K.; Lee, A.; Hill, A.; Kohn, M.; Shah, S.; Torvaldsen, S.; Baur, L. A randomised controlled trial of a community-based healthy lifestyle program for overweight and obese adolescents: The loozit® study protocol. BMC Public Health 2009, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Janicke, D.M.; Sallinen, B.J.; Perri, M.G.; Lutes, L.D.; Huerta, M.; Silverstein, J.H.; Brumback, B. Comparison of parent-only vs family-based interventions for overweight children in underserved rural settings: Outcomes from project story. Arch. Pediatr. Adolesc. Med. 2008, 162, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.; Shrewsbury, V.A.; O'Connor, J.; Steinbeck, K.S.; Hill, A.J.; Shah, S.; Kohn, M.R.; Torvaldsen, S.; Baur, L.A. Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: The loozit randomized controlled trial. Int. J. Obes. 2013, 37, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Bean, M.K.; Mazzeo, S.E.; Stern, M.; Evans, R.K.; Bryan, D.; Ning, Y.; Wickham, E.P., III; Laver, J. Six-month dietary changes in ethnically diverse, obese adolescents participating in a multidisciplinary weight management program. Clin. Pediatr. 2011, 50, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Harp, J.B.; Reitman, M.L.; Beetsch, J.W.; Schoeller, D.A.; Erondu, N.; Pietrobelli, A. Why do obese patients not lose more weight when treated with low-calorie diets? A mechanistic perspective. Am. J. Clin. Nutr. 2007, 85, 346–354. [Google Scholar] [PubMed]
- Ho, M.; Garnett, S.P.; Baur, L.A.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Impact of dietary and exercise interventions on weight change and metabolic outcomes in obese children and adolescents a systematic review and meta-analysis of randomized trials. JAMA Pediatr. 2013, 167, 759–768. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Tung, A.; Chak, S.S.; Ventura, E.E.; Byrd-Williams, C.E.; Alexander, K.E.; Lane, C.J.; Weigensberg, M.J.; Spruijt-Metz, D.; Goran, M.I. Aerobic and strength training reduces adiposity in overweight latina adolescents. Med. Sci. Sports Exerc. 2009, 41, 1494–1503. [Google Scholar] [CrossRef] [PubMed]
- Straker, L.M.; Smith, K.L.; Fenner, A.A.; Kerr, D.A.; McManus, A.; Davis, M.C.; Fielding, A.M.; Olds, T.S.; Hagger, M.S.; Smith, A.J.; et al. Rationale, design and methods for a staggered-entry, waitlist controlled clinical trial of the impact of a community-based, family-centred, multidisciplinary program focussed on activity, food and attitude habits (curtin university’s activity, food and attitudes program-cafap) among overweight adolescents. BMC Public Health 2012, 12, 471. [Google Scholar] [PubMed]
- Warren, J.M.; Golley, R.K.; Collins, C.E.; Okely, A.D.; Jones, R.A.; Morgan, P.J.; Perry, R.A.; Baur, L.A.; Steele, J.R.; Magarey, A.M. Randomised controlled trials in overweight children: Practicalities and realities. Int. J. Pediatr. Obes. 2007, 2, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, Z.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC growth charts: United States. Adv. Data. 2000, 314, 1–27. [Google Scholar] [PubMed]
- Fenner, A.A.; Straker, L.M.; Davis, M.C.; Hagger, M.S. Theoretical underpinnings of a need-supportive intervention to address sustained healthy lifestyle changes in overweight and obese adolescents. Psychol. Sport Exerc. 2013, 14, 819–829. [Google Scholar] [CrossRef]
- Savoye, M.; Shaw, M.; Dziura, J.; Tamborlane, W.V.; Rose, P.; Guandalini, C.; Goldberg-Gell, R.; Burgert, T.S.; Cali, A.M.; Weiss, R.; et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. JAMA 2007, 297, 2697–2704. [Google Scholar] [CrossRef] [PubMed]
- Rangan, A.M.; Randall, D.; Hector, D.J.; Gill, T.P.; Webb, K.L. Consumption of “extra” foods by australian children: Types, quantities and contribution to energy and nutrient intakes. Eur. J. Clin. Nutr. 2008, 62, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Dixon, H.G.; Scully, M.L.; Wakefield, M.A.; White, V.M.; Crawford, D.A. The effects of television advertisements for junk food versus nutritious food on children’s food attitudes and preferences. Soc. Sci. Med. 2007, 65, 1311–1323. [Google Scholar] [CrossRef] [PubMed]
- Johnston, L.F.; National Health and Medical Research Council. Educator guide; National Health and Medical Research Council: Canberra, Australia, 2013; pp. 5–6. [Google Scholar]
- Thompson, F.E.; Subar, A.F. Dietary assessment methodology. In Nutrition in the prevention and treatment of disease, 2nd ed.; Coulston, A.M., Boushey, C.J., Eds.; Elsevier Academic Press: Burlington, MA, USA, 2013; pp. 5–46. [Google Scholar]
- Livingstone, M.B.E.; Robson, P.J. Measurement of dietary intake in children. Proc. Nutr. Soc. 2000, 59, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Watson, J.; Burrows, T. Measuring dietary intake in children and adolescents in the context of overweight and obesity. Int. J. Obesity 2010, 34, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.J.; Kerr, D.A.; Wright, J.; Lutes, K.D.; Ebert, D.S.; Delp, E.J. Use of technology in children’s dietary assessment. Eur. J. Clin. Nutr. 2009, 63, S50–S57. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.; Rosenberg, M.; Miller, M.; French, S.; McCormack, G.; Bull, F.; Giles-Corti, B.; Pratt, S. Trends in physical activity, nutrition and body size in western australian children and adolescents: The child and adolescent physical activity and nutrition survey (capans); Move and Munch Final Report; The Western Australian Government: Perth, Australia, 2008.
- Rutishauser, I.; Webb, K.; Abraham, B.; Allsopp, R. Evaluation of short dietary questions from the 1995 national nutrition survey; Australian Food and Nutrition Monitoring Unit, The University of Queensland: Canberra, Austrilia, 2001. [Google Scholar]
- Singh, R.; Martin, B.R.; Hickey, Y.; Teegarden, D.; Campbell, W.W.; Craig, B.A.; Schoeller, D.A.; Kerr, D.A.; Weaver, C.M. Comparison of self-reported and measured metabolizable energy intake with total energy expenditure in overweight teens. Am. J. Clin. Nutr. 2009, 89, 1744–1750. [Google Scholar] [CrossRef] [PubMed]
- Rennie, K.L.; Coward, A.; Jebb, S.A. Estimating under-reporting of energy intake in dietary surveys using an individualised method. Br. J. Nutr. 2007, 97, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Jennings, A.; Cassidy, A.; van Sluijs, E.M.; Griffin, S.J.; Welch, A.A. Associations between eating frequency, adiposity, diet, and activity in 9–10 year old healthy-weight and centrally obese children. Obesity 2012, 20, 1462–1468. [Google Scholar] [CrossRef] [PubMed]
- Henes, S.T.; Cummings, D.M.; Hickner, R.C.; Houmard, J.A.; Kolasa, K.M.; Lazorick, S.; Collier, D.N. Comparison of predictive equations and measured resting energy expenditure among obese youth attending a pediatric healthy weight clinic: One size does not fit all. Nutr. Clin. Pract. 2013, 28, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Puyau, M.R.; Adolph, A.L.; Vohra, F.A.; Zakeri, I.; Butte, N.F. Prediction of activity energy expenditure using accelerometers in children. Med. Sci. Sports Exerc. 2004, 36, 1625–1631. [Google Scholar] [PubMed]
- Straker, L.M.; Howie, E.K.; Smith, K.L.; Fenner, A.A.; Kerr, D.A.; Olds, T.S.; Abbott, R.A.; Smith, A.J. The impact of curtin university’s activity, food and attitudes program on physical activity, sedentary time and fruit, vegetable and junk food consumption among overweight and obese adolescents: A waitlist controlled trial. PLoS One 2014, 9, e111954. [Google Scholar] [CrossRef] [PubMed]
- Skelton, J.A.; Beech, B.M. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, e273–e281. [Google Scholar] [CrossRef] [PubMed]
- Vitolins, M.Z.; Rand, C.S.; Rapp, S.R.; Ribisl, P.M.; Sevick, M.A. Measuring adherence to behavioral and medical interventions. Control. Clin. Trials 2000, 21, 188S–194S. [Google Scholar] [CrossRef]
- Foraker, R.E.; Pennell, M.; Sprangers, P.; Vitolins, M.Z.; DeGraffinreid, C.; Paskett, E.D. Effect of a low-fat or low-carbohydrate weight-loss diet on markers of cardiovascular risk among premenopausal women: A randomized trial. J. Womens Health 2014, 23, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Kristal, A.R.; Ollberding, N.J. Evaluation of nutrition interventions. In Nutrition in the prevention and treatment of disease, 3rd ed.; Coulston, A.M., Boushey, C.J., Ferruzzi, M.G., Eds.; Elsevier Inc.: San Diego, California, CA, USA, 2013; pp. 191–205. [Google Scholar]
- DeBar, L.L.; Stevens, V.J.; Perrin, N.; Wu, P.; Pearson, J.; Yarborough, B.J.; Dickerson, J.; Lynch, F. A primary care-based, multicomponent lifestyle intervention for overweight adolescent females. Pediatrics 2012, 129, e611–e620. [Google Scholar] [CrossRef] [PubMed]
- Tsiros, M.D.; Sinn, N.; Brennan, L.; Coates, A.M.; Walkley, J.W.; Petkov, J.; Howe, P.R.; Buckley, J.D. Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am. J. Clin. Nutr. 2008, 87, 1134–1140. [Google Scholar] [PubMed]
- Davis, J.N.; Gyllenhammer, L.E.; Vanni, A.A.; Meija, M.; Tung, A.; Schroeder, E.T.; Spruijt-Metz, D.; Goran, M.I. Startup circuit training program reduces metabolic risk in latino adolescents. Med. Sci. Sport Exer. 2011, 43, 2195–2203. [Google Scholar] [CrossRef] [PubMed]
- Park, T.G.; Hong, H.R.; Lee, J.; Kang, H.S. Lifestyle plus exercise intervention improves metabolic syndrome markers without change in adiponectin in obese girls. Ann. Nutr. Metab. 2007, 51, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Saelens, B.E.; Sallis, J.F.; Wilfley, D.E.; Patrick, K.; Cella, J.A.; Buchta, R. Behavioral weight control for overweight adolescents initiated in primary care. Obes. Res. 2002, 10, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, T.; Mannisto, S.; Roos, E.; Pietinen, P. Increasing prevalence of underreporting does not necessarily distort dietary surveys. Eur. J. Clin. Nutr. 1997, 51, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Ball, G.D.; Mackenzie-Rife, K.A.; Newton, M.S.; Alloway, C.A.; Slack, J.M.; Plotnikoff, R.C.; Goran, M.I. One-on-one lifestyle coaching for managing adolescent obesity: Findings from a pilot, randomized controlled trial in a real-world, clinical setting. Paediatr. Child. Health 2011, 16, 345–350. [Google Scholar] [PubMed]
- Smith, K.L.; Kerr, D.A.; Fenner, A.A.; Straker, L.M. Adolescents just do not know what they want: A qualitative study to describe obese adolescents’ experiences of text messaging to support behavior change maintenance post intervention. J. Med. Internet. Res. 2014, 16, e103. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.; Abdel-Maksoud, M.; Crane, L.; Marcus, A.; Byers, T. Effects of social approval bias on self-reported fruit and vegetable consumption: A randomized controlled trial. Nutr. J. 2008, 7, 18. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; Straker, L.M.; Kerr, D.A.; Smith, A.J. Overweight adolescents eat what? And when? Analysis of consumption patterns to guide dietary message development for intervention. J. Hum. Nutr. Diet. 2014, 28, 80–93. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, K.L.; Kerr, D.A.; Howie, E.K.; Straker, L.M. Do Overweight Adolescents Adhere to Dietary Intervention Messages? Twelve-Month Detailed Dietary Outcomes from Curtin University’s Activity, Food and Attitudes Program. Nutrients 2015, 7, 4363-4382. https://doi.org/10.3390/nu7064363
Smith KL, Kerr DA, Howie EK, Straker LM. Do Overweight Adolescents Adhere to Dietary Intervention Messages? Twelve-Month Detailed Dietary Outcomes from Curtin University’s Activity, Food and Attitudes Program. Nutrients. 2015; 7(6):4363-4382. https://doi.org/10.3390/nu7064363
Chicago/Turabian StyleSmith, Kyla L., Deborah A. Kerr, Erin K. Howie, and Leon M. Straker. 2015. "Do Overweight Adolescents Adhere to Dietary Intervention Messages? Twelve-Month Detailed Dietary Outcomes from Curtin University’s Activity, Food and Attitudes Program" Nutrients 7, no. 6: 4363-4382. https://doi.org/10.3390/nu7064363
APA StyleSmith, K. L., Kerr, D. A., Howie, E. K., & Straker, L. M. (2015). Do Overweight Adolescents Adhere to Dietary Intervention Messages? Twelve-Month Detailed Dietary Outcomes from Curtin University’s Activity, Food and Attitudes Program. Nutrients, 7(6), 4363-4382. https://doi.org/10.3390/nu7064363





