Enteral and Parenteral Nutrition in the Perioperative Period: State of the Art
Abstract
:1. Introduction
2. Nutritional Assessment and Population at Risk for Perioperative Malnutrition
| Nutritional Risk Scoring (NRS) | ||||
|---|---|---|---|---|
| Initial Screening | ||||
| Yes | No | |||
| Is BMI < 20.5? | ||||
| Has the patient lost weight within the last 3 months? | ||||
| Has the patient reduced dietary intake in the last week? | ||||
| Is the patient severely ill (e.g., in intensive therapy)? | ||||
| Yes: If the answer is “Yes” to any question, the final screening is performed. | ||||
| No: If the answer is “No” to all questions, the patient is re-screened at weekly intervals. If the patient, e.g., is scheduled for a major operation, a preventative nutritional care plan is considered to avoid the associated risk status. | ||||
| Final Screening | ||||
| Impaired Nutritional Status | Severity of Disease (≈Increase in Requirements) | |||
| Absent Score 0 | Normal Nutritional Status | Absent Score 0 | Normal Nutritional Requirements | |
| Mild Score 1 | Wt loss >5% in 3 months or Food intake below 50%–75% of normal requirement in preceding week | Mild Score 1 | Hip fracture * Chronic patients, in particular with acute complications: Cirrhosis *, COPD *. Chronic hemodialysis, diabetes, oncology | |
| Moderate Score 2 | Wt loss >5% in 2 months or BMI 18.5–20.5+ impaired general condition or food intake 25%–60% of normal requirement in preceding week | Moderate Score 2 | Major abdominal surgery * Stroke * Severe pneumonia, hematologic malignancy | |
| Severe Score 3 | Wt loss >5% in 1 month (>15% in 3 months) or BMI > 18.5+ impaired general condition or Food intake 0%–25% of normal requirement in preceding week in preceding week. | Severe Score 3 | Head injury * Bone marrow transplantation * Intensive care patients (APACHE410) | |
| Score | + | Score | =Total score: | |
| Score ≥3: The patient is nutritionally at-risk and a nutritional care plan is initiated. | ||||
| Score <3: Weekly rescreening of the patient. If the patient, e.g., is scheduled for a major operation, a preventive nutritional care plan is considered to avoid the associated risk status. | ||||
| * Indicates that a trial directly supports the categorization of patients with that diagnosis. | ||||
3. Parenteral Nutrition
3.1. Benefits
| Vitamin/Trace Element | Requirement |
|---|---|
| Thiamin (B1) | 6 mg |
| Riboflavin (B2) | 3.6 mg |
| Niacin (B3) | 40 mg |
| Folic Acid | 600 μg |
| Panthotenic Acid | 15 mg |
| Pyridoxine | 6 mg |
| Cyanocobalamin (B12) | 5 μg |
| Biotin | 60 μg |
| Ascorbic Acid (C) | 200 mg |
| Vitamin A | 3300 IU |
| Vitamin D | 200 IU |
| Vitamin E | 10 IU |
| Vitamin K | 150 μg |
| Chromium | 10–15 μg |
| Copper | 0.3–0.5 mg |
| Iron | 1.0–1.2 mg |
| Manganese | 0.2–0.3 mg |
| Selenium | 20–60 μg |
| Zinc | 2.5–5 mg |
| Molybdenum | 20 μg |
| Iodine | 100 μg |
| Fluoride | 1 mg |
3.2. Risks and Complications of TPN
| Catheter Insertion Complications |
| Arterial puncture |
| Pneumothorax |
| Hemothorax |
| Catheter & wire tip embolization |
| Air embolism |
| Thoracic duct injury |
| Catheter malposition |
| Cardiac arrhythmias |
| Mediastinal air/hematoma |
| Cardiac perforation |
| Brachial plexus injury |
| Catheter Related Complications |
| Subclavian vein, internal jogular vein or Superior vena cava thrombosis |
| Catheter site infection |
| Septic phlebitis |
| Catheter associated blood stream infection |
| Metabolic Complications |
| Hyperglycemia or hypoglycemia |
| Ketoacidosis |
| Azotemia & Hyperosmolar state |
| Electrolyte imbalance |
| Hypertriglyceridemia |
| Metabolic acidosis |
| Hepatic dysfunction |
| Fluid overload |
| Coagulopathy |
3.3. Preoperative TPN Use
3.4. Postoperative TPN Use
4. Enteral Nutrition
4.1. Benefits
4.2. Risks and Complications of EN
| Mechanical Complications |
| Aspiration |
| Tube malposition |
| Tube clogging |
| Gastrointestinal Complications |
| Nausea and vomiting |
| Diarrhea or constipation |
| Malabsorption/maldigestion |
| Metabolic Complications |
| Hyperglycemia or hypoglycemia |
| Electrolyte imbalance |
| Early satiety |
| Dehydration |
| Refeeding syndrome |
4.3. Preoperative Use
4.4. Postoperative Use
5. TPN vs. EN
Cost Effectiveness
6. Combined EN and TPN
7. Immunonutrition
8. Conclusion
Conflict of Interest
References
- Ward, N. Nutrition support to patients undergoing gastrointestinal surgery. Nutr. J. 2003, 2, 18. [Google Scholar] [CrossRef]
- Studley, H.O. Percentage of weight loss: A basic indicator of surgical risk in patients with chronic peptic ulcer. 1936. Nutr. Hosp. 2001, 16, 141–143. [Google Scholar]
- Braga, M.; Gianotti, L.; Gentilini, O.; Parisi, V.; Salis, C.; di Carlo, V. Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit. Care Med. 2001, 29, 242–248. [Google Scholar] [CrossRef]
- Palesty, J.A.; Dudrick, S.J. Cachexia, malnutrition, the refeeding syndrome, and lessons from Goldilocks. Surg. Clin. North Am. 2011, 91, 653–673. [Google Scholar] [CrossRef]
- Bozzetti, F. Nutritional support in oncologic patients: Where we are and where we are going. Clin. Nutr. 2011, 30, 714–717. [Google Scholar] [CrossRef]
- Bozzetti, F. Perioperative nutritional management. Proc. Nutr. Soc. 2011, 70, 305–310. [Google Scholar] [CrossRef]
- Beattie, A.H.; Prach, A.T.; Baxter, J.P.; Pennington, C.R. A randomised controlled trial evaluating the use of enteral nutritional supplements postoperatively in malnourished surgical patients. Gut 2000, 46, 813–818. [Google Scholar] [CrossRef]
- Fujita, T.; Daiko, H.; Nishimura, M. Early enteral nutrition reduces the rate of life-threatening complications after thoracic esophagectomy in patients with esophageal cancer. Eur. Surg. Res. 2012, 48, 79–84. [Google Scholar] [CrossRef]
- Van Der Hulst, R.R.; von Meyenfeldt, M.F.; van Kreel, B.K.; Thunnissen, F.B.; Brummer, R.J.; Arends, J.W.; Soeters, P.B. Gut permeability, intestinal morphology, and nutritional depletion. Nutrition 1998, 14, 1–6. [Google Scholar] [CrossRef]
- Visser, M.; Davids, M.; Verberne, H.J.; Kok, W.E.; Niessen, H.W.; van Venrooij, L.M.; Cocchieri, R.; Wisselink, W.; de Mol, B.A.; van Leeuwen, P.A. Rationale and design of a proof-of-concept trial investigating the effect of uninterrupted perioperative (par)enteral nutrition on amino acid profile, cardiomyocytes structure, and cardiac perfusion and metabolism of patients undergoing coronary artery bypass grafting. J. Cardiothorac. Surg. 2011, 6, 36. [Google Scholar] [CrossRef]
- Brady, M.; Kinn, S.; Stuart, P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst. Rev. 2003, 4, CD004423. [Google Scholar]
- Lennard, T.W.; Shenton, B.K.; Borzotta, A.; Donnelly, P.K.; White, M.; Gerrie, L.M.; Proud, G.; Taylor, R.M. The influence of surgical operations on components of the human immune system. Br. J. Surg. 1985, 72, 771–776. [Google Scholar] [CrossRef]
- Thorell, A.; Nygren, J.; Ljungqvist, O. Insulin resistance: A marker of surgical stress. Curr. Opin. Clin. Nutr. Metab. Care 1999, 2, 69–78. [Google Scholar] [CrossRef]
- Hausel, J.; Nygren, J.; Lagerkranser, M.; Hellstrom, P.M.; Hammarqvist, F.; Almstrom, C.; Lindh, A.; Thorell, A.; Ljungqvist, O. A carbohydrate-rich drink reduces preoperative discomfort in elective surgery patients. Anesth. Analg. 2001, 93, 1344–1350. [Google Scholar] [CrossRef]
- Hausel, J.; Nygren, J.; Thorell, A.; Lagerkranser, M.; Ljungqvist, O. Randomized clinical trial of the effects of oral preoperative carbohydrates on postoperative nausea and vomiting after laparoscopic cholecystectomy. Br. J. Surg. 2005, 92, 415–421. [Google Scholar] [CrossRef]
- Noblett, S.E.; Watson, D.S.; Huong, H.; Davison, B.; Hainsworth, P.J.; Horgan, A.F. Pre-operative oral carbohydrate loading in colorectal surgery: A randomized controlled trial. Colorectal Dis. 2006, 8, 563–569. [Google Scholar] [CrossRef]
- Gustafsson, U.O.; Nygren, J.; Thorell, A.; Soop, M.; Hellstrom, P.M.; Ljungqvist, O.; Hagstrom-Toft, E. Pre-operative carbohydrate loading may be used in type 2 diabetes patients. Acta Anaesthesiol. Scand. 2008, 52, 946–951. [Google Scholar] [CrossRef]
- Braunschweig, C.L.; Levy, P.; Sheean, P.M.; Wang, X. Enteral compared with parenteral nutrition: A meta-analysis. Am. J. Clin. Nutr. 2001, 74, 534–542. [Google Scholar]
- Hulsewe, K.W.; Deutz, N.E.; de Blaauw, I.; van der Hulst, R.R.; von Meyenfeldt, M.M.; Soeters, P.B. Liver protein and glutamine metabolism during cachexia. Proc. Nutr. Soc. 1997, 56, 801–806. [Google Scholar] [CrossRef]
- Braga, M.; Ljungqvist, O.; Soeters, P.; Fearon, K.; Weimann, A.; Bozzetti, F. ESPEN Guidelines on Parenteral Nutrition: Surgery. Clin. Nutr. 2009, 28, 378–386. [Google Scholar] [CrossRef]
- Bollschweiler, E.; Schroder, W.; Holscher, A.H.; Siewert, J.R. Preoperative risk analysis in patients with adenocarcinoma or squamous cell carcinoma of the oesophagus. Br. J. Surg. 2000, 87, 1106–1110. [Google Scholar] [CrossRef]
- Butters, M.; Straub, M.; Kraft, K.; Bittner, R. Studies on nutritional status in general surgery patients by clinical, anthropometric, and laboratory parameters. Nutrition 1996, 12, 405–410. [Google Scholar] [CrossRef]
- Correia, M.I.; Caiaffa, W.T.; da Silva, A.L.; Waitzberg, D.L. Risk factors for malnutrition in patients undergoing gastroenterological and hernia surgery: An analysis of 374 patients. Nutr. Hosp. 2001, 16, 59–64. [Google Scholar]
- Durkin, M.T.; Mercer, K.G.; McNulty, M.F.; Phipps, L.; Upperton, J.; Giles, M.; Scott, D.J. Vascular surgical society of great britain and ireland: Contribution of malnutrition to postoperative morbidity in vascular surgical patients. Br. J. Surg. 1999, 86, 702. [Google Scholar]
- Haugen, M.; Homme, K.A.; Reigstad, A.; Teigland, J. Assessment of nutritional status in patients with rheumatoid arthritis and osteoarthritis undergoing joint replacement surgery. Arthritis Care Res. 1999, 12, 26–32. [Google Scholar] [CrossRef]
- Lumbers, M.; New, S.A.; Gibson, S.; Murphy, M.C. Nutritional status in elderly female hip fracture patients: Comparison with an age-matched home living group attending day centres. Br. J. Nutr. 2001, 85, 733–740. [Google Scholar] [CrossRef]
- Padillo, F.J.; Andicoberry, B.; Muntane, J.; Lozano, J.M.; Mino, G.; Sitges-Serra, A.; Pera-Madrazo, C. Factors predicting nutritional derangements in patients with obstructive jaundice: Multivariate analysis. World J. Surg. 2001, 25, 413–418. [Google Scholar] [CrossRef]
- Takagi, K.; Yamamori, H.; Morishima, Y.; Toyoda, Y.; Nakajima, N.; Tashiro, T. Preoperative immunosuppression: Its relationship with high morbidity and mortality in patients receiving thoracic esophagectomy. Nutrition 2001, 17, 13–17. [Google Scholar] [CrossRef]
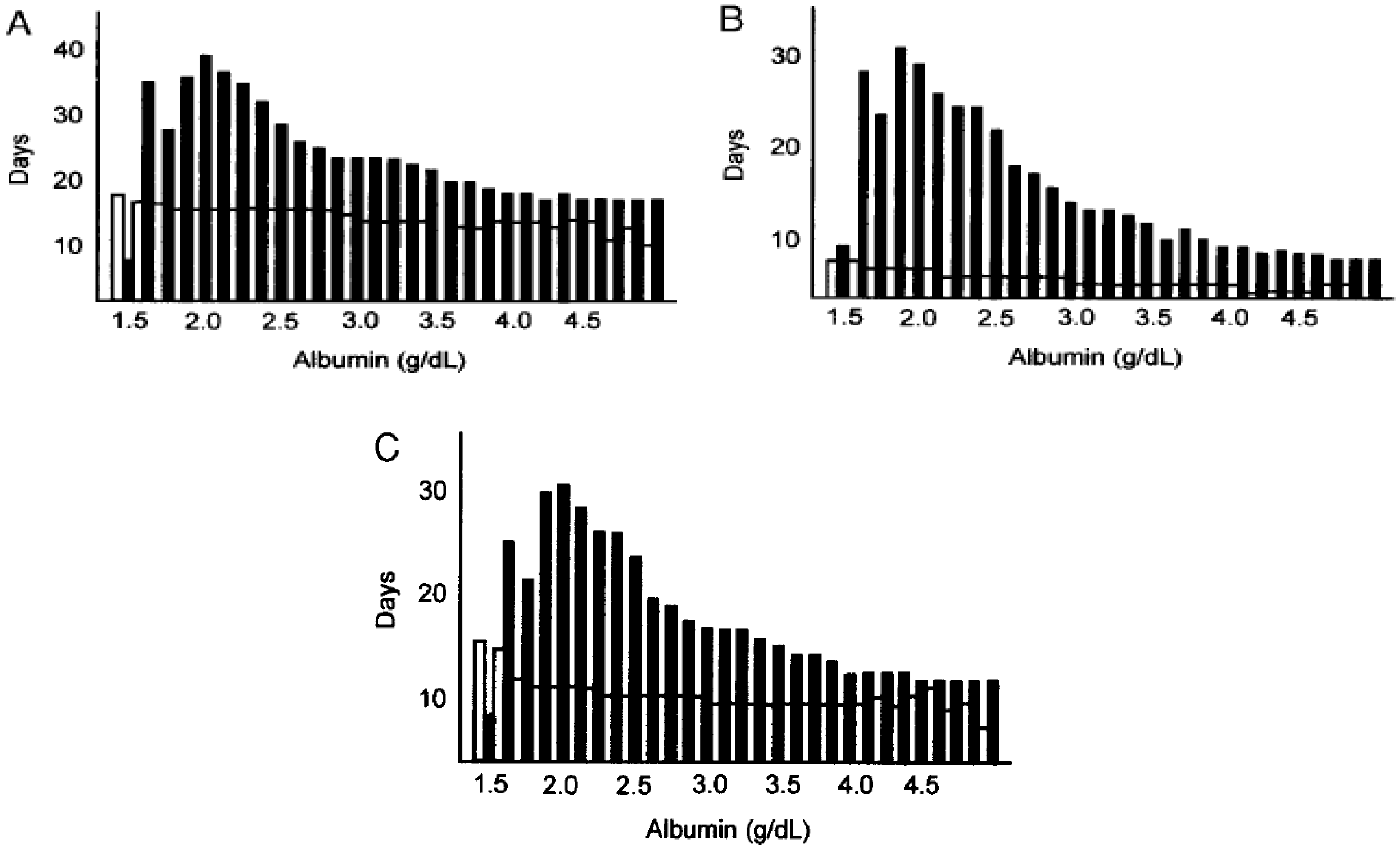
- Kudsk, K.A.; Tolley, E.A.; DeWitt, R.C.; Janu, P.G.; Blackwell, A.P.; Yeary, S.; King, B.K. Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J. Parenter. Enteral Nutr. 2003, 27, 1–9. [Google Scholar] [CrossRef]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Soeters, P.B.; Schols, A.M. Advances in understanding and assessing malnutrition. Curr. Opin. Clin. Nutr. Metab. Care 2009, 12, 487–494. [Google Scholar] [CrossRef]
- Giner, M.; Laviano, A.; Meguid, M.M.; Gleason, J.R. In 1995 a correlation between malnutrition and poor outcome in critically ill patients still exists. Nutrition 1996, 12, 23–29. [Google Scholar] [CrossRef]
- Gustafsson, U.O.; Ljungqvist, O. Perioperative nutritional management in digestive tract surgery. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 504–509. [Google Scholar] [CrossRef]
- Torosian, M.H. Perioperative nutrition support for patients undergoing gastrointestinal surgery: Critical analysis and recommendations. World J. Surg. 1999, 23, 565–569. [Google Scholar] [CrossRef]
- Jie, B.; Jiang, Z.M.; Nolan, M.T.; Zhu, S.N.; Yu, K.; Kondrup, J. Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition 2012, 28, 1022–1027. [Google Scholar] [CrossRef]
- Visser, M.; van Venrooij, L.M.; Vulperhorst, L.; de Vos, R.; Wisselink, W.; van Leeuwen, P.A.; de Mol, B.A. Sarcopenic obesity is associated with adverse clinical outcome after cardiac surgery. Nutr. Metab. Cardiovasc. Dis. 2012. [Google Scholar] [CrossRef]
- Stenholm, S.; Harris, T.B.; Rantanen, T.; Visser, M.; Kritchevsky, S.B.; Ferrucci, L. Sarcopenic obesity: Definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 693–700. [Google Scholar] [CrossRef]
- Van Venrooij, L.M.; de Vos, R.; Zijlstra, E.; Borgmeijer-Hoelen, M.M.; van Leeuwen, P.A.; de Mol, B.A. The impact of low preoperative fat-free body mass on infections and length of stay after cardiac surgery: A prospective cohort study. J. Thorac. Cardiovasc. Surg. 2011, 142, 1263–1269. [Google Scholar] [CrossRef]
- Mercadante, S. Bowel obstruction in home-care cancer patients: 4 years experience. Support. Care Cancer 1995, 3, 190–193. [Google Scholar] [CrossRef]
- Buzby, G.P.; Williford, W.O.; Peterson, O.L.; Crosby, L.O.; Page, C.P.; Reinhardt, G.F.; Mullen, J.L. A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: The rationale and impact of previous clinical trials and pilot study on protocol design. Am. J. Clin. Nutr. 1988, 47, 357–365. [Google Scholar]
- Detsky, A.S.; Baker, J.P.; O’Rourke, K.; Goel, V. Perioperative parenteral nutrition: A meta-analysis. Ann. Intern. Med. 1987, 107, 195–203. [Google Scholar]
- Klek, S.; Sierzega, M.; Szybinski, P.; Szczepanek, K.; Scislo, L.; Walewska, E.; Kulig, J. Perioperative nutrition in malnourished surgical cancer patients—A prospective, randomized, controlled clinical trial. Clin. Nutr. 2011, 30, 708–713. [Google Scholar] [CrossRef]
- Compher, C.W.; Spencer, C.; Kinosian, B.P. Perioperative parenteral nutrition: Impact on morbidity and mortality in surgical patients. Nutr. Clin. Pract. 2005, 20, 460–467. [Google Scholar] [CrossRef]
- Morlion, B.J.; Stehle, P.; Wachtler, P.; Siedhoff, H.P.; Koller, M.; Konig, W.; Furst, P.; Puchstein, C. Total parenteral nutrition with glutamine dipeptide after major abdominal surgery: A randomized, double-blind, controlled study. Ann. Surg. 1998, 227, 302–308. [Google Scholar] [CrossRef]
- Bozzetti, F.; Gavazzi, C.; Miceli, R.; Rossi, N.; Mariani, L.; Cozzaglio, L.; Bonfanti, G.; Piacenza, S. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: A randomized, clinical trial. JPEN J. Parenter. Enteral Nutr. 2000, 24, 7–14. [Google Scholar]
- Bagdade, J.D.; Stewart, M.; Walters, E. Impaired granulocyte adherence. A reversible defect in host defense in patients with poorly controlled diabetes. Diabetes 1978, 27, 677–681. [Google Scholar]
- Ortmeyer, J.; Mohsenin, V. Glucosesuppresses superoxide generation in normal neutrophils: Interference in phospholipase deactivation. Am. J. Physiol. 1993, 264, 402–410. [Google Scholar]
- Rossi, F.; Grzeskowiak, M.; Della Bianca, V.; Sbarbati, A. De novo synthesis of diacylglycerol from glucose. A new pathway of signal transduction in human neutrophils stimulated during phagocytosis of beta-glucan particles. J. Biol. Chem. 1991, 266, 8034–8038. [Google Scholar]
- Klein, C.J.; Stanek, G.S.; Wiles, C.E., III. Overfeeding macronutrients to critically ill adults: Metabolic complications. J. Am. Diet. Assoc. 1998, 98, 795–806. [Google Scholar] [CrossRef]
- Heyland, D.K.; Montalvo, M.; MacDonald, S.; Keefe, L.; Su, X.Y.; Drover, J.W. Total parenteral nutrition in the surgical patient: A meta-analysis. Can. J. Surg. 2001, 44, 102–111. [Google Scholar]
- Beier-Holgersen, R.; Boesby, S. Influence of postoperative enteral nutrition on postsurgical infections. Gut 1996, 39, 833–835. [Google Scholar] [CrossRef]
- Schroeder, D.; Gillanders, L.; Mahr, K.; Hill, G.L. Effects of immediate postoperative enteral nutrition on body composition, muscle function, and wound healing. JPEN J. Parenter. Enteral Nutr. 1991, 15, 376–383. [Google Scholar]
- Saito, H.; Trocki, O.; Alexander, J.W.; Kopcha, R.; Heyd, T.; Joffe, S.N. The effect of route of nutrient administration on the nutritional state, catabolic hormone secretion, and gut mucosal integrity after burn injury. JPEN J. Parenter. Enteral Nutr. 1987, 11, 1–7. [Google Scholar]
- Moskovitz, D.N.; Kim, Y.I. Does perioperative immunonutrition reduce postoperative complications in patients with gastrointestinal cancer undergoing operations? Nutr. Rev. 2004, 62, 443–447. [Google Scholar] [CrossRef]
- Woods, J.H.; Erickson, L.W.; Condon, R.E.; Schulte, W.J.; Sillin, L.F. Postoperative ileus: A colonic problem? Surgery 1978, 84, 527–533. [Google Scholar]
- Bozzetti, F.; Braga, M.; Gianotti, L.; Gavazzi, C.; Mariani, L. Postoperative enteral versus parenteral nutrition in malnourished patients with gastrointestinal cancer: A randomised multicentre trial. Lancet 2001, 358, 1487–1492. [Google Scholar] [CrossRef]
- Heidegger, C.P.; Berger, M.M.; Graf, S.; Zingg, W.; Darmon, P.; Costanza, M.C.; Thibault, R.; Pichard, C. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: A randomised controlled clinical trial. Lancet 2012, 381, 385–393. [Google Scholar]
- Singh, A.; Chen, M.; Li, T.; Yang, X.L.; Li, J.Z.; Gong, J.P. Parenteral nutrition combined with enteral nutrition for severe acute pancreatitis. ISRN Gastroenterol. 2012, 2012, 791383. [Google Scholar]
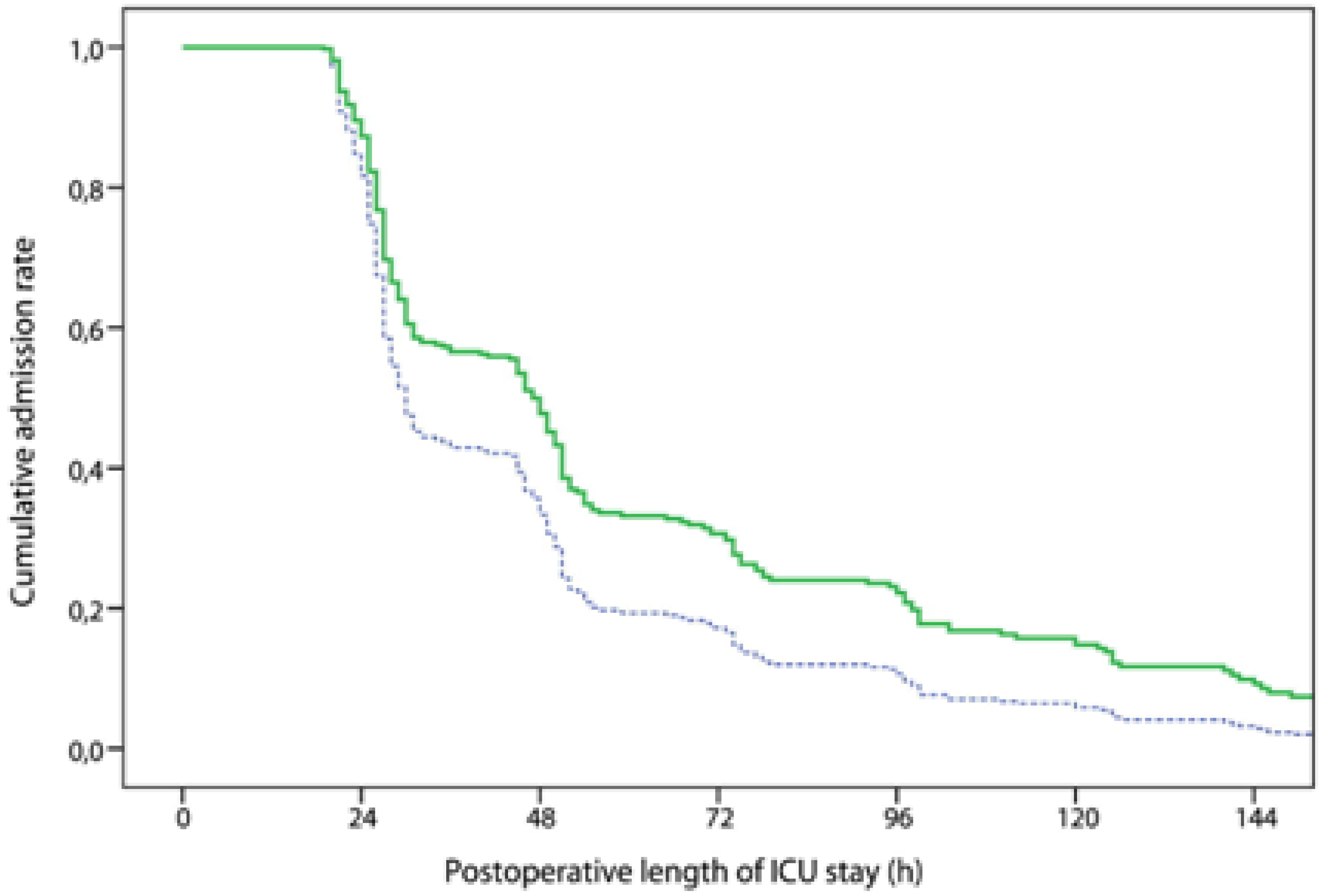
- Hsu, M.H.; Yu, Y.E.; Tsai, Y.M.; Lee, H.C.; Huang, Y.C.; Hsu, H.S. Combined enteral feeding and total parenteral nutritional support improves outcome in surgical intensive care unit patients. J. Chin. Med. Assoc. 2012, 75, 459–463. [Google Scholar] [CrossRef]
- Omata, J.; Fukatsu, K.; Maeshima, Y.; Moriya, T.; Murakoshi, S.; Noguchi, M.; Okamoto, K.; Fukazawa, S.; Saitoh, D.; Mochizuki, H.; et al. Enteral nutrition rapidly reverses total parenteral nutrition-induced impairment of hepatic immunity in a murine model. Clin. Nutr. 2009, 28, 668–673. [Google Scholar] [CrossRef]
- Zheng, Y.; Li, F.; Qi, B.; Luo, B.; Sun, H.; Liu, S.; Wu, X. Application of perioperative immunonutrition for gastrointestinal surgery: A meta-analysis of randomized controlled trials. Asia Pac. J. Clin. Nutr. 2007, 16, 253–257. [Google Scholar]
- Zhang, Y.; Gu, Y.; Guo, T.; Li, Y.; Cai, H. Perioperative immunonutrition for gastrointestinal cancer: A systematic review of randomized controlled trials. Surg. Oncol. 2012, 21, e87–e95. [Google Scholar] [CrossRef]
- Zheng, Y.M.; Li, F.; Zhang, M.M.; Wu, X.T. Glutamine dipeptide for parenteral nutrition in abdominal surgery: A meta-analysis of randomized controlled trials. World J. Gastroenterol. 2006, 12, 7537–7541. [Google Scholar]
- O’Riordain, M.G.; Fearon, K.C.; Ross, J.A.; Rogers, P.; Falconer, J.S.; Bartolo, D.C.; Garden, O.J.; Carter, D.C. Glutamine-supplemented total parenteral nutrition enhances T-lymphocyte response in surgical patients undergoing colorectal resection. Ann. Surg. 1994, 220, 212–221. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Abunnaja, S.; Cuviello, A.; Sanchez, J.A. Enteral and Parenteral Nutrition in the Perioperative Period: State of the Art. Nutrients 2013, 5, 608-623. https://doi.org/10.3390/nu5020608
Abunnaja S, Cuviello A, Sanchez JA. Enteral and Parenteral Nutrition in the Perioperative Period: State of the Art. Nutrients. 2013; 5(2):608-623. https://doi.org/10.3390/nu5020608
Chicago/Turabian StyleAbunnaja, Salim, Andrea Cuviello, and Juan A. Sanchez. 2013. "Enteral and Parenteral Nutrition in the Perioperative Period: State of the Art" Nutrients 5, no. 2: 608-623. https://doi.org/10.3390/nu5020608
APA StyleAbunnaja, S., Cuviello, A., & Sanchez, J. A. (2013). Enteral and Parenteral Nutrition in the Perioperative Period: State of the Art. Nutrients, 5(2), 608-623. https://doi.org/10.3390/nu5020608




