Assessing the Relationship between Vitamin D3 and Stratum Corneum Hydration for the Treatment of Xerotic Skin
Abstract
:1. Introduction
2. Methods
2.1. Baseline Study
2.2. Treatment Study
2.3. Statistical Analysis
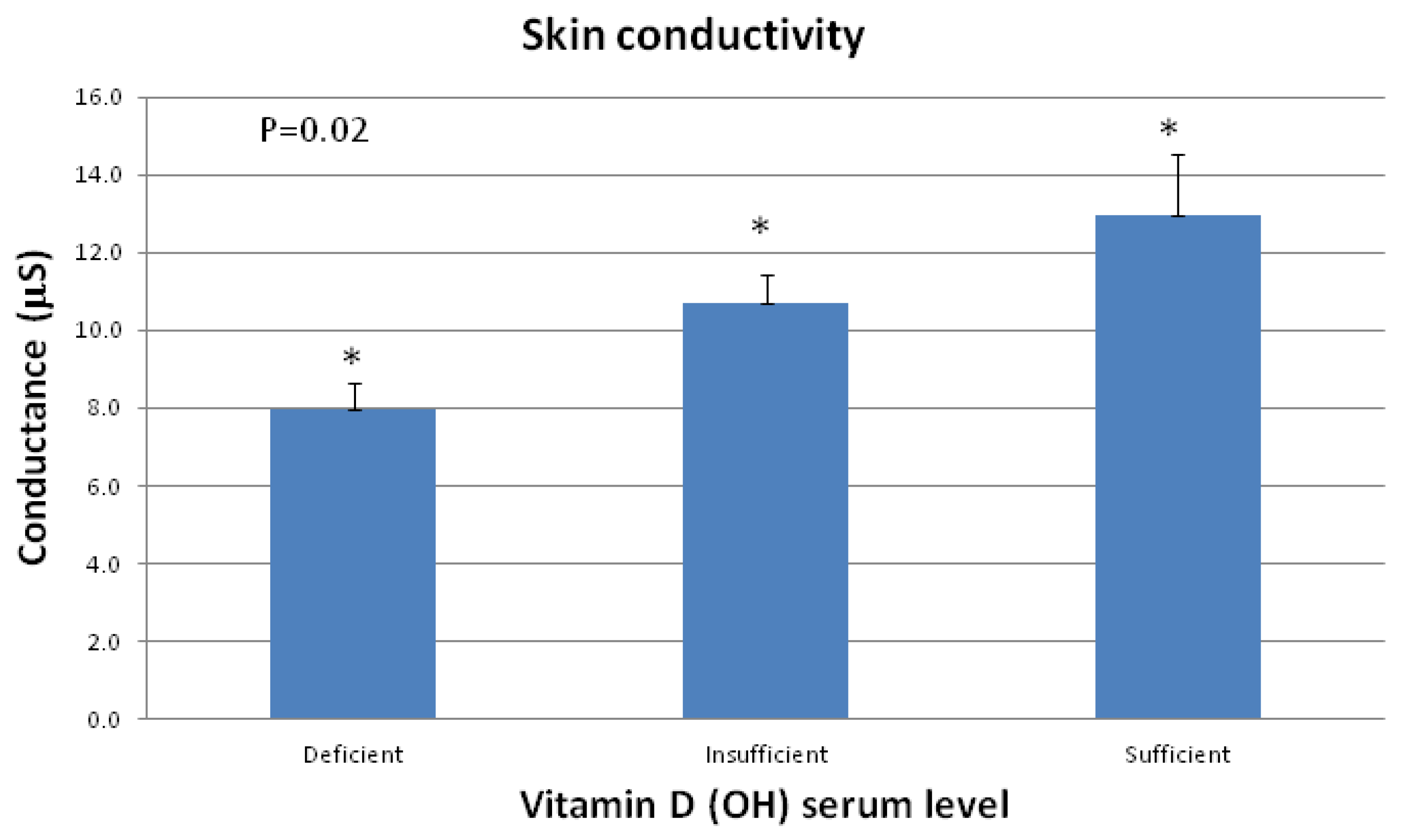
3. Results

4. Discussion
5. Conclusions
Acknowledgments
Conflict of Interest
References
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Holick, M.F. The Vitamin D Solution A 3-Step Stategy to Cure Our Most Common Health Problem; Hudson Street Press: New York, NY, USA, 2010. [Google Scholar]
- Gibbs, S.; Backendorf, C.; Ponec, M. Regulation of keratinocyte proliferation and differentiation by all-trans-retinoic acid, 9-cis-retinoic acid and 1,25-dihydroxy vitamin D3. Arch. Dermatol. Res. 1996, 288, 729–738. [Google Scholar]
- Peroni, D.G.; Piacentini, G.L.; Cametti, E.; Chinellato, I.; Boner, A.L. Correlation between serum 25-hydroxyvitamin D levels and severity of atopic dermatitis in children. Br. J. Dermatol. 2011, 164, 1078–1082. [Google Scholar] [CrossRef]
- Asgari, M.M.; Tang, J.; Warton, M.E.; Chren, M.M.; Quesenberry, C.P., Jr.; Bikle, D.; Horst, R.L.; Orentreich, N.; Vogelman, J.H.; Friedman, G.D. Association of prediagnostic serum vitamin D levels with the development of basal cell carcinoma. J. Invest. Dermatol. 2010, 130, 1438–1443. [Google Scholar]
- Berardesca, E. EEMCO guidance for the assessment of stratum corneum hydration: Electrical methods. Skin Res. Technol. 1997, 3, 126–132. [Google Scholar] [CrossRef]
- Chen, T.C.; Chimeh, F.; Lu, Z.; Mathieu, J.; Person, K.S.; Zhang, A.; Kohn, N.; Martinello, S.; Berkowitz, R.; Holick, M.F. Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Arch. Biochem. Biophys. 2007, 460, 213–217. [Google Scholar]
- Yetley, E.A. Assessing the vitamin D status of the US population. Am. J. Clin. Nutr. 2008, 88, 558S–564S. [Google Scholar]
- Ginde, A.A.; Liu, M.C.; Camargo, C.A., Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch. Intern. Med. 2009, 169, 626–632. [Google Scholar]
- Harris, S.S.; Dawson-Hughes, B. Seasonal changes in plasma 25-hydroxyvitamin D concentrations of young American black and white women. Am. J. Clin. Nutr. 1998, 67, 1232–1236. [Google Scholar]
- Skin Moisturization (Cosmetic Science and Technology); Leyden, J.J.; Rawlings, A.V. (Eds.) Marcel Dekker, Inc.: New York, NY, USA, 2002; Volume 25, p. 138.
- Reichrath, J.; Müller, S.M.; Kerber, A.; Baum, H.P.; Bahmer, F.A. Biologic effects of topical calcipotriol (MC 903) treatment in psoriatic skin. J. Am. Acad. Dermatol. 1997, 36, 19–28. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Russell, M. Assessing the Relationship between Vitamin D3 and Stratum Corneum Hydration for the Treatment of Xerotic Skin. Nutrients 2012, 4, 1213-1218. https://doi.org/10.3390/nu4091213
Russell M. Assessing the Relationship between Vitamin D3 and Stratum Corneum Hydration for the Treatment of Xerotic Skin. Nutrients. 2012; 4(9):1213-1218. https://doi.org/10.3390/nu4091213
Chicago/Turabian StyleRussell, Meghan. 2012. "Assessing the Relationship between Vitamin D3 and Stratum Corneum Hydration for the Treatment of Xerotic Skin" Nutrients 4, no. 9: 1213-1218. https://doi.org/10.3390/nu4091213