Relationship between Nutrition Intake and 28-Day Mortality Using Modified NUTRIC Score in Patients with Sepsis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
Ethical Statement
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patients Characteristics
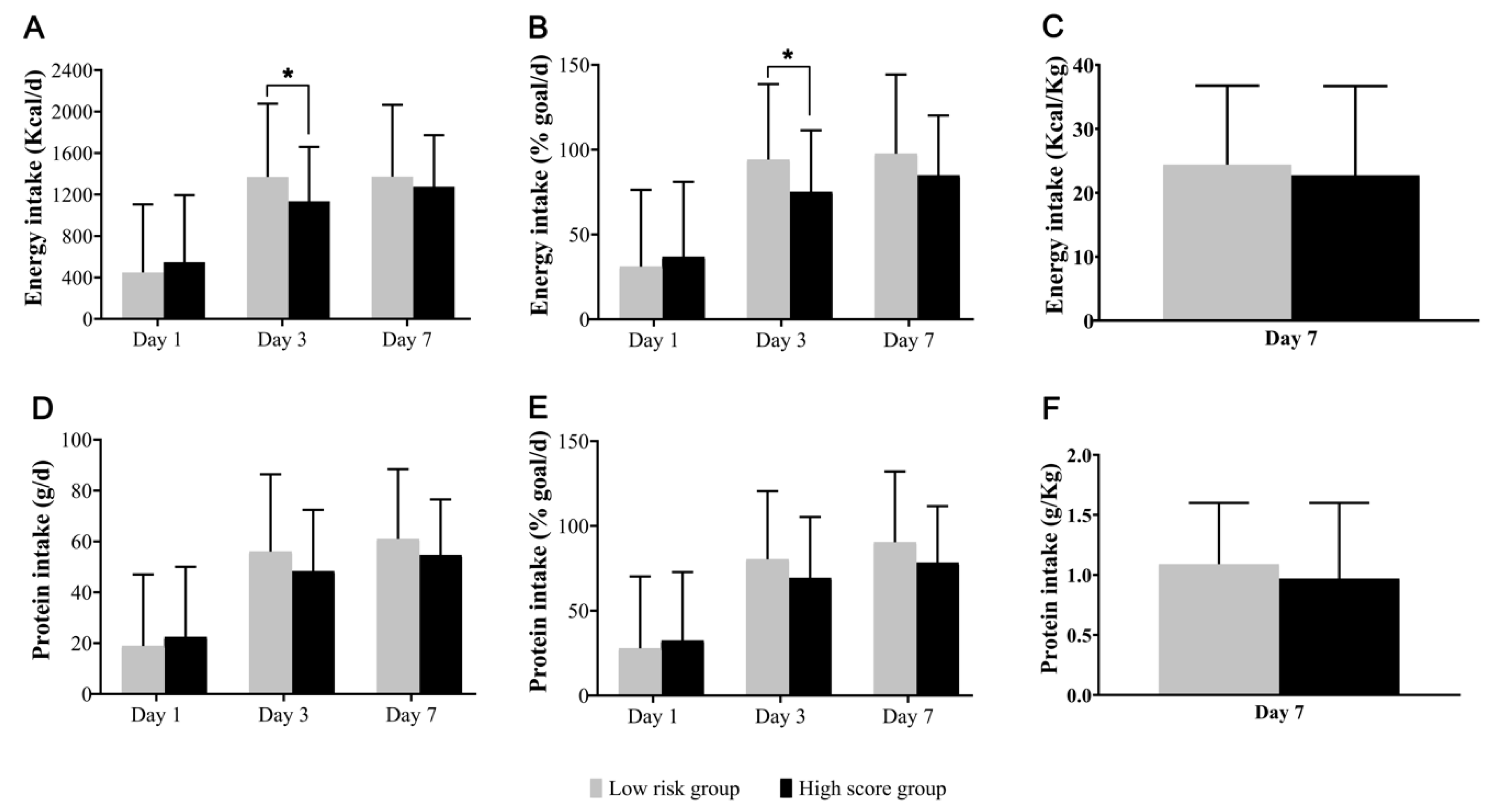
3.2. Nutritional Profiles
3.3. Nutritional Intakes and 28-Day Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Edington, J.; Boorman, J.; Durrant, E.R.; Perkins, A.; Giffin, C.V.; James, R.; Thomson, J.M.; Oldroyd, J.C.; Smith, J.C.; Torrance, A.D.; et al. Prevalence of malnutrition on admission to four hospitals in england. Clin. Nutr. 2000, 19, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Johansen, N.; Plum, L.M.; Bak, L.; Larsen, I.H.; Martinsen, A.; Andersen, J.R.; Baernthsen, H.; Bunch, E.; Lauesen, N. Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin. Nutr. 2002, 21, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Correia, M.I.; Campos, A.C.; Elan Cooperative Study. Prevalence of hospital malnutrition in latin america: The multicenter elan study. Nutrition 2003, 19, 823–825. [Google Scholar] [CrossRef]
- McWhirter, J.P.; Pennington, C.R. Incidence and recognition of malnutrition in hospital. BMJ 1994, 308, 945–948. [Google Scholar] [CrossRef] [PubMed]
- Villet, S.; Chiolero, R.L.; Bollmann, M.D.; Revelly, J.P.; Cayeux, R.N.M.; Delarue, J.; Berger, M.M. Negative impact of hypocaloric feeding and energy balance on clinical outcome in icu patients. Clin. Nutr. 2005, 24, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Doig, G.S.; Simpson, F.; Finfer, S.; Delaney, A.; Davies, A.R.; Mitchell, I.; Dobb, G.; Nutrition Guidelines Investigators of the Anzics Clinical Trials Group. Effect of evidence-based feeding guidelines on mortality of critically ill adults: A cluster randomized controlled trial. JAMA 2008, 300, 2731–2741. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.M.; Veyres, P.; Pivot, X.; Soummer, A.M.; Jambou, P.; Filippi, J.; van Obberghen, E.; Hebuterne, X. Malnutrition is an independent factor associated with nosocomial infections. Br. J. Nutr. 2004, 92, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Pirlich, M.; Schuetz, T.; Lochs, H.; Pichard, C. Is nutritional depletion by nutritional risk index associated with increased length of hospital stay? A population-based study. JPEN J. Parenter. Enteral Nutr. 2004, 28, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Giner, M.; Laviano, A.; Meguid, M.M.; Gleason, J.R. In 1995 a correlation between malnutrition and poor outcome in critically ill patients still exists. Nutrition 1996, 12, 23–29. [Google Scholar] [CrossRef]
- Liu, M.J.; Bao, S.; Napolitano, J.R.; Burris, D.L.; Yu, L.; Tridandapani, S.; Knoell, D.L. Zinc regulates the acute phase response and serum amyloid a production in response to sepsis through jak-stat3 signaling. PLoS ONE 2014, 9, e94934. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- McClave, S.A.; Taylor, B.E.; Martindale, R.G.; Warren, M.M.; Johnson, D.R.; Braunschweig, C.; McCarthy, M.S.; Davanos, E.; Rice, T.W.; Cresci, G.A.; et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of critical care medicine (sccm) and american society for parenteral and enteral nutrition (a.S.P.E.N.). JPEN J. Parenter. Enteral Nutr. 2016, 40, 159–211. [Google Scholar] [CrossRef] [PubMed]
- Weijs, P.J.; Cynober, L.; DeLegge, M.; Kreymann, G.; Wernerman, J.; Wolfe, R.R. Proteins and amino acids are fundamental to optimal nutrition support in critically ill patients. Crit. Care 2014, 18, 591. [Google Scholar] [CrossRef] [PubMed]
- Weijs, P.J.; Stapel, S.N.; de Groot, S.D.; Driessen, R.H.; de Jong, E.; Girbes, A.R.; Strack van Schijndel, R.J.; Beishuizen, A. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: A prospective observational cohort study. JPEN J. Parenter. Enteral Nutr. 2012, 36, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Allingstrup, M.J.; Esmailzadeh, N.; Wilkens Knudsen, A.; Espersen, K.; Hartvig Jensen, T.; Wiis, J.; Perner, A.; Kondrup, J. Provision of protein and energy in relation to measured requirements in intensive care patients. Clin. Nutr. 2012, 31, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Hurt, R.T.; McClave, S.A.; Martindale, R.G.; Ochoa Gautier, J.B.; Coss-Bu, J.A.; Dickerson, R.N.; Heyland, D.K.; Hoffer, L.J.; Moore, F.A.; Morris, C.R.; et al. Summary points and consensus recommendations from the international protein summit. Nutr. Clin. Pract. 2017, 32, 142S–151S. [Google Scholar] [CrossRef] [PubMed]
- Charles, E.J.; Petroze, R.T.; Metzger, R.; Hranjec, T.; Rosenberger, L.H.; Riccio, L.M.; McLeod, M.D.; Guidry, C.A.; Stukenborg, G.J.; Swenson, B.R.; et al. Hypocaloric compared with eucaloric nutritional support and its effect on infection rates in a surgical intensive care unit: A randomized controlled trial. Am. J. Clin. Nutr. 2014, 100, 1337–1343. [Google Scholar] [CrossRef]
- Arabi, Y.M.; Aldawood, A.S.; Haddad, S.H.; Al-Dorzi, H.M.; Tamim, H.M.; Jones, G.; Mehta, S.; McIntyre, L.; Solaiman, O.; Sakkijha, M.H.; et al. Permissive underfeeding or standard enteral feeding in critically ill adults. N. Engl. J. Med. 2015, 372, 2398–2408. [Google Scholar] [CrossRef] [PubMed]
- Arabi, Y.M.; Haddad, S.H.; Tamim, H.M.; Rishu, A.H.; Sakkijha, M.H.; Kahoul, S.H.; Britts, R.J. Near-target caloric intake in critically ill medical-surgical patients is associated with adverse outcomes. JPEN J. Parenter. Enteral Nutr. 2010, 34, 280–288. [Google Scholar] [CrossRef]
- Petros, S.; Horbach, M.; Seidel, F.; Weidhase, L. Hypocaloric vs normocaloric nutrition in critically ill patients: A prospective randomized pilot trial. JPEN J. Parenter. Enteral Nutr. 2016, 40, 242–249. [Google Scholar] [CrossRef]
- Compher, C.; Chittams, J.; Sammarco, T.; Nicolo, M.; Heyland, D.K. Greater protein and energy intake may be associated with improved mortality in higher risk critically ill patients: A multicenter, multinational observational study. Crit. Care Med. 2017, 45, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Hasan, R.M.; Agarwala, R.; Martin, C.; Day, A.G.; Heyland, D.K. Identifying critically-ill patients who will benefit most from nutritional therapy: Further validation of the “modified nutric” nutritional risk assessment tool. Clin. Nutr. 2016, 35, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.C.; Bielemann, R.M.; Kruschardt, P.P.; Orlandi, S.P. Complementarity of nutric score and subjective global assessment for predicting 28-day mortality in critically ill patients. Clin. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Reignier, J.; Boisrame-Helms, J.; Brisard, L.; Lascarrou, J.B.; Ait Hssain, A.; Anguel, N.; Argaud, L.; Asehnoune, K.; Asfar, P.; Bellec, F.; et al. Enteral versus parenteral early nutrition in ventilated adults with shock: A randomised, controlled, multicentre, open-label, parallel-group study (nutrirea-2). Lancet 2018, 391, 133–143. [Google Scholar] [CrossRef]
- Heidegger, C.P.; Berger, M.M.; Graf, S.; Zingg, W.; Darmon, P.; Costanza, M.C.; Thibault, R.; Pichard, C. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: A randomised controlled clinical trial. Lancet 2013, 381, 385–393. [Google Scholar] [CrossRef]
- Arabi, Y.M.; Tamim, H.M.; Dhar, G.S.; Al-Dawood, A.; Al-Sultan, M.; Sakkijha, M.H.; Kahoul, S.H.; Brits, R. Permissive underfeeding and intensive insulin therapy in critically ill patients: A randomized controlled trial. Am. J. Clin. Nutr. 2011, 93, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Chapman, M.; Peake, S.L.; Bellomo, R.; Davies, A.; Deane, A.; Horowitz, M.; Hurford, S.; Lange, K.; Little, L.; et al.; TARGET Investigators, for the ANZICS Clinical Trials Group Energy-dense versus routine enteral nutrition in the critically ill. N. Engl. J. Med. 2018, 379, 1823–1834. [Google Scholar] [CrossRef]
- Alberda, C.; Gramlich, L.; Jones, N.; Jeejeebhoy, K.; Day, A.G.; Dhaliwal, R.; Heyland, D.K. The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. Intensive Care Med. 2009, 35, 1728–1737. [Google Scholar] [CrossRef]
- Wei, X.; Day, A.G.; Ouellette-Kuntz, H.; Heyland, D.K. The association between nutritional adequacy and long-term outcomes in critically ill patients requiring prolonged mechanical ventilation: A multicenter cohort study. Crit. Care Med. 2015, 43, 1569–1579. [Google Scholar] [CrossRef]
- Nicolo, M.; Heyland, D.K.; Chittams, J.; Sammarco, T.; Compher, C. Clinical outcomes related to protein delivery in a critically ill population: A multicenter, multinational observation study. JPEN J. Parenter. Enteral Nutr. 2016, 40, 45–51. [Google Scholar] [CrossRef]
- Weijs, P.J.; Looijaard, W.G.; Beishuizen, A.; Girbes, A.R.; Oudemans-van Straaten, H.M. Early high protein intake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients. Crit. Care 2014, 18, 701. [Google Scholar] [CrossRef] [PubMed]
- Perner, A.; Rhodes, A.; Venkatesh, B.; Angus, D.C.; Martin-Loeches, I.; Preiser, J.C.; Vincent, J.L.; Marshall, J.; Reinhart, K.; Joannidis, M.; et al. Sepsis: Frontiers in supportive care, organisation and research. Intensive Care Med. 2017, 43, 496–508. [Google Scholar] [CrossRef] [PubMed]
- Artinian, V.; Krayem, H.; DiGiovine, B. Effects of early enteral feeding on the outcome of critically ill mechanically ventilated medical patients. Chest 2006, 129, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Heyland, D.K.; Dhaliwal, R.; Jiang, X.; Day, A.G. Identifying critically ill patients who benefit the most from nutrition therapy: The development and initial validation of a novel risk assessment tool. Crit. Care 2011, 15, R268. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, A.; Henry, J.; Ong, V.; Leong, C.S.; Teh, A.L.; van Dam, R.M.; Kowitlawakul, Y. Association of modified nutric score with 28-day mortality in critically ill patients. Clin. Nutr. 2017, 36, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Arabi, Y.M.; Aldawood, A.S.; Al-Dorzi, H.M.; Tamim, H.M.; Haddad, S.H.; Jones, G.; McIntyre, L.; Solaiman, O.; Sakkijha, M.H.; Sadat, M.; et al. Permissive underfeeding or standard enteral feeding in high- and low-nutritional-risk critically ill adults. Post hoc analysis of the permit trial. Am. J. Respir. Crit. Care Med. 2017, 195, 652–662. [Google Scholar] [CrossRef]
- Compher, C.; Chittams, J.; Sammarco, T.; Higashibeppu, N.; Higashiguchi, T.; Heyland, D.K. Greater nutrient intake is associated with lower mortality in western and eastern critically ill patients with low bmi: A multicenter, multinational observational study. JPEN J. Parenter. Enteral Nutr. 2019, 43, 63–69. [Google Scholar] [CrossRef] [PubMed]
| Variable | Modified NUTRIC Score (n = 248) | ||
|---|---|---|---|
| Low Score | High Score | p-Value | |
| (n = 28) | (n = 220) | ||
| Age, years | 54 (42–70) | 68 (58–75) | 0.001 |
| Height, cm | 164 (160–170) | 163 (155–170) | 0.375 |
| Weight, kg | 57 (49–61) | 60 (51–67) | 0.548 |
| BMI, kg/m2 | 21 (18–24) | 23 (19–25) | 0.156 |
| Female, n (%) | 7 (25.0) | 68 (30.9) | 0.521 |
| APACHE II score | 15 (13–18) | 24 (20–28) | <0.001 |
| SOFA score | 6 (4–8) | 12 (9–14) | <0.001 |
| Days from hospital to ICU | 0 (0–2) | 0 (0–6) | 0.510 |
| Co-morbidities | 1 (1–2) | 2 (1–3) | 0.013 |
| LOS in ICU, days | 11 (9–19) | 14 (9–25) | 0.586 |
| MV | 21 (75.0) | 196 (89.1) | 0.034 |
| Vasopressor use | 22 (78.6) | 204 (92.7)) | 0.013 |
| RRT | 4 (14.3) | 100 (45.5) | 0.002 |
| Diagnosis | 0.434 | ||
| Respiratory disease | 19 (62.9) | 119 (54.1) | |
| Liver/GI disease | 3 (10.7) | 35 (15.9) | |
| Cardiovascular disease | 0 (0) | 8 (3.6) | |
| Renal disease | 1 (3.6) | 14 (6.4) | |
| Febrile neutropenia | 0 (0) | 11 (5.0) | |
| SSTI | 0 (0) | 8 (3.6) | |
| Other | 5 (17.9) | 25 (11.4) | |
| VAP | 0 (0) | 19 (8.6) | 0.106 |
| Bacteremia | 8 (28.6) | 77 (35.0) | 0.500 |
| Sepsis severity | <0.001 | ||
| Sepsis | 0 (0) | 6 (2.7) | |
| Severe sepsis | 19 (67.9) | 65 (29.5) | |
| Septic shock | 9 (32.1) | 149 (67.7) | |
| 28-day mortality | 5 (17.9) | 80 (36.4) | 0.052 |
| Sepsis related deaths | 4 (80) | 40 (50) | 0.193 |
| Low Score (n = 28) | p-Value | High Score (n = 220) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Energy intake (kcal/kg) | <20 | 20 to <25 | ≥25 | <20 | 20 to <25 | ≥25 | ||
| No. of patients | 10 | 3 | 15 | 90 | 53 | 77 | ||
| Deaths | 3 (30.0) | 0 (0) | 2 (13.3) | 0.323 | 39 (43.3) | 19 (35.8) | 22 (28.6) | 0.048 |
| Protein intake (g/kg) | <1.0 | 1.0 to <1.2 | ≥1.2 | <1.0 | 1.0 to <1.2 | ≥1.2 | ||
| No. of patients | 12 | 5 | 11 | 128 | 40 | 52 | ||
| Deaths | 3 (25.0) | 1 (20.0) | 1 (9.1) | 0.330 | 52 (40.6) | 13 (32.5) | 15 (28.8) | 0.117 |
| Variables | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 1.008 (0.992–1.015) | 0.334 | 1.015 (0.998–1.032) | 0.091 |
| Sex | 1.823 (1.177–2.826) | 0.007 | 2.009 (1.285–3.140) | 0.002 |
| BMI | 1.051 (1.007–1.098) | 0.024 | .. | .. |
| Co-morbidities | 1.054 (0.849–1.309) | 0.631 | .. | .. |
| Energy intake (kcal/kg) | ||||
| <20 | Reference | Reference | ||
| 20 to <25 | 0.865 (0.503–1.487) | 0.599 | 0.883 (0.513–1.520) | 0.654 |
| ≥25 | 0.562 (0.340–0.929) | 0.025 | 0.534 (0.322–0.887) | 0.015 |
| Protein intake (g/kg) | ||||
| <1.0 | Reference | Reference | ||
| 1.0 to <1.2 | 0.793 (0.441–1.427) | 0.643 | 0.860 (0.476–1.555) | 0.618 |
| ≥1.2 | 0.506 (0.289–0.886) | 0.017 | 0.475 (0.270–0.836) | 0.010 |
| Variables | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 0.993 (0.954–1.034) | 0.742 | ||
| Sex | 1.001 (0.274–3.657) | 0.999 | ||
| BMI | 1.050 (0.931–1.184) | 0.424 | 1.081 (0.927–1.260) | 0.320 |
| Co-morbidities | 0.565 (0.296–1.078) | 0.083 | ||
| Energy intake (kcal/kg) | ||||
| <20 | Reference | Reference | ||
| 20 to <25 | 0 (0) | 0.989 | 0 (0) | 0.988 |
| ≥25 | 0.400 (0.062–2.563) | 0.334 | 0.193 (0.013–2.840) | 0.231 |
| Protein intake (g/kg) | ||||
| <1.0 | Reference | Reference | ||
| 1.0 to <1.2 | 0.806 (0.079–8.187) | 0.855 | 0.021 (0.000–9.343) | 0.214 |
| ≥1.2 | 0.285 (0.028–2.909) | 0.289 | 0.256 (0.013–5.176) | 0.375 |
| Variables | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 1.009 (0.990–1.028) | 0.345 | ||
| Sex | 1.977 (1.235–3.165) | 0.005 | 1.970 (1.239–3.132) | 0.004 |
| BMI | 1.049 (1.001–1.099) | 0.044 | ||
| Co-morbidities | 1.117 (0.884–1.411) | 0.354 | ||
| Energy intake (kcal/kg) | ||||
| <20 | Reference | Reference | ||
| 20 to <25 | 0.864 (0.499–1.495) | 0.601 | 0.901 (0.520–1.561) | 0.709 |
| ≥25 | 0.582 (0.344–0.982) | 0.043 | 0.569 (0.337–0.962) | 0.035 |
| Protein intake (g/kg) | ||||
| <1.0 | Reference | Reference | ||
| 1.0 to <1.2 | 0.780 (0.425–1.432) | 0.423 | 0.857 (0.464–1.583) | 0.622 |
| ≥1.2 | 0.537 (0.301–0.956) | 0.035 | 0.502 (0.280–0.900) | 0.021 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, D.H.; Hong, S.-B.; Lim, C.-M.; Koh, Y.; Seo, J.; Kim, Y.; Min, J.-Y.; Huh, J.W. Relationship between Nutrition Intake and 28-Day Mortality Using Modified NUTRIC Score in Patients with Sepsis. Nutrients 2019, 11, 1906. https://doi.org/10.3390/nu11081906
Jeong DH, Hong S-B, Lim C-M, Koh Y, Seo J, Kim Y, Min J-Y, Huh JW. Relationship between Nutrition Intake and 28-Day Mortality Using Modified NUTRIC Score in Patients with Sepsis. Nutrients. 2019; 11(8):1906. https://doi.org/10.3390/nu11081906
Chicago/Turabian StyleJeong, Dae Hyun, Sang-Bum Hong, Chae-Man Lim, Younsuck Koh, Jarim Seo, Younkyoung Kim, Ji-Yeon Min, and Jin Won Huh. 2019. "Relationship between Nutrition Intake and 28-Day Mortality Using Modified NUTRIC Score in Patients with Sepsis" Nutrients 11, no. 8: 1906. https://doi.org/10.3390/nu11081906
APA StyleJeong, D. H., Hong, S.-B., Lim, C.-M., Koh, Y., Seo, J., Kim, Y., Min, J.-Y., & Huh, J. W. (2019). Relationship between Nutrition Intake and 28-Day Mortality Using Modified NUTRIC Score in Patients with Sepsis. Nutrients, 11(8), 1906. https://doi.org/10.3390/nu11081906





