Dietary Fibre as a Unifying Remedy for the Whole Spectrum of Obesity-Associated Cardiovascular Risk
Abstract
1. Introduction
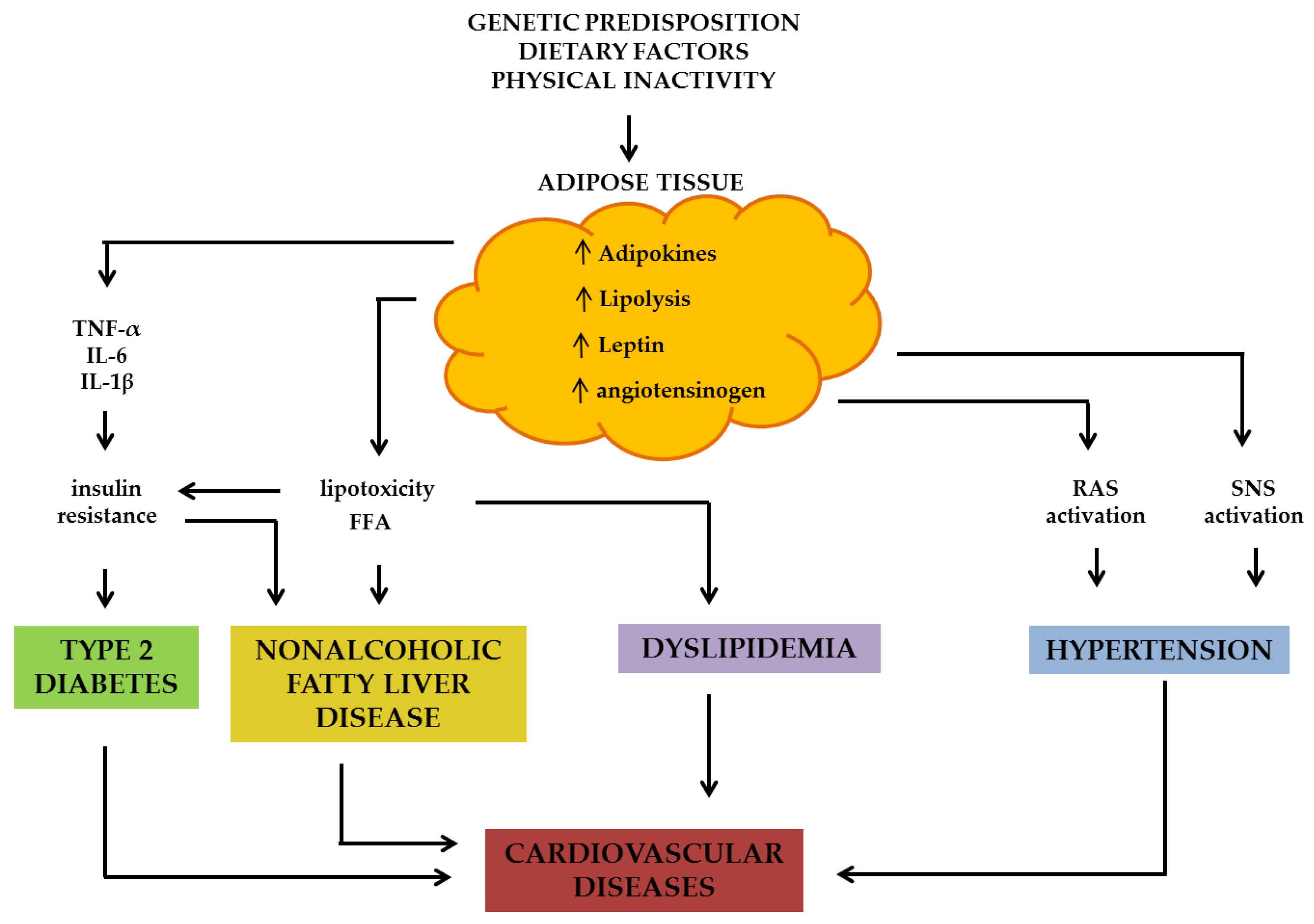
1.1. Pathophysiology of Obesity and Related Cardiovascular Risk Factors
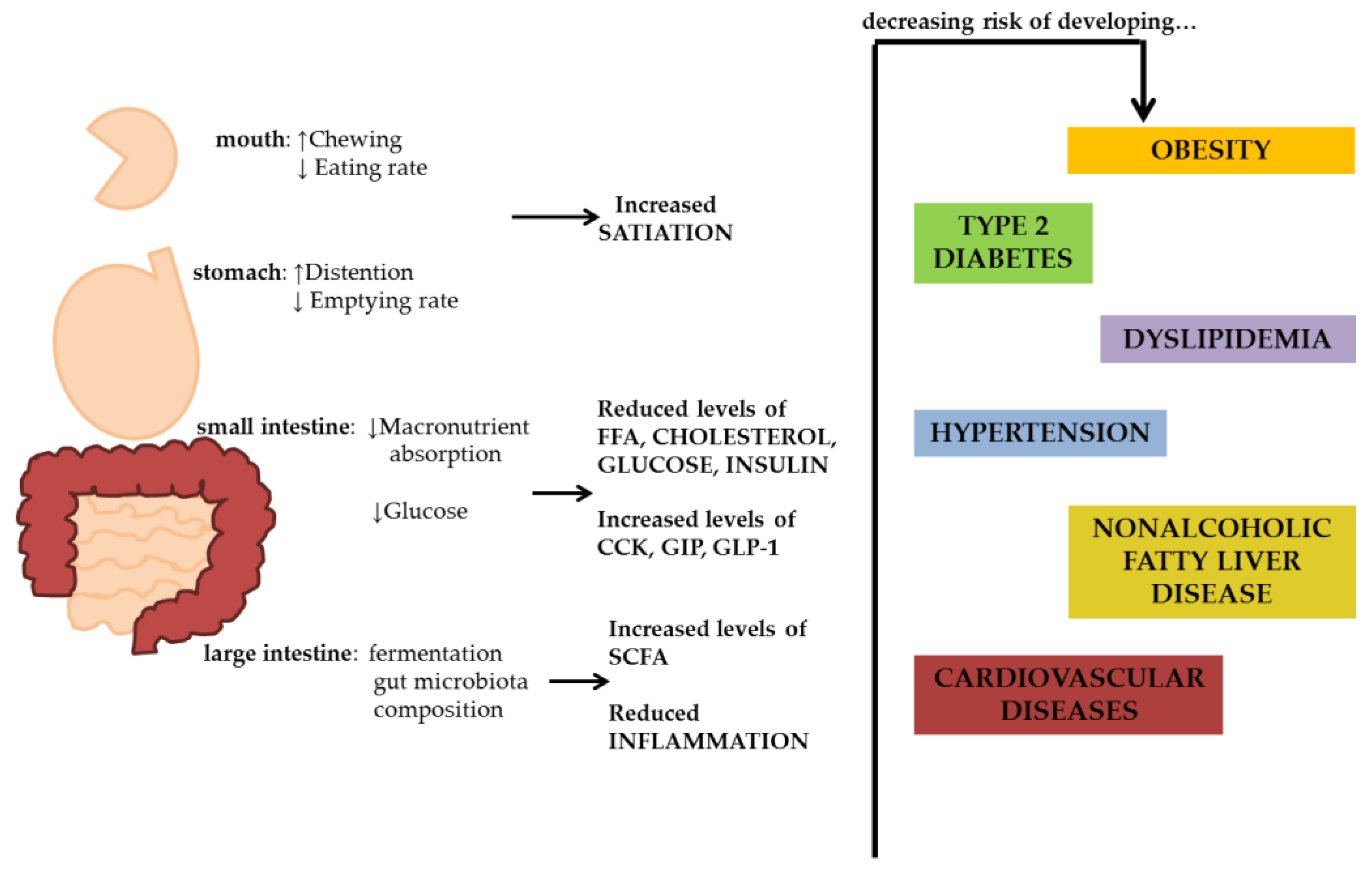
1.2. Dietary Fibre
- Non-viscous, insoluble, non-fermentable fibre. It is an insoluble fibre that is very poorly fermented in the intestine. It has mechanical and laxative effects, contributing to regulate digestive function. Bran, cellulose, hemicellulose and lignin are the main fibres representative of this group.
- Non-viscous, soluble, fermentable fibre. It is quickly and greatly fermented by the intestinal microbiota. It may have a prebiotic effect, but it does not induce laxative effects. Inulin, dextrin, oligosaccharides, resistant starch are the main fibres representative of this group.
- Viscous, soluble, fermentable fibre. It can form a viscous gel that reduces nutrient absorption in the intestine. Moreover, it is rapidly fermented by the intestinal microbiota. Pectin, β-glucan, guar gum, and glucomannan are the main fibres representative of this group.
- Viscous, soluble, non-fermentable fibre. It reduces the absorption of nutrients due to its viscosity and exerts laxative effects. Psyllium and methylcellulose are the main fibres representative of this group.
2. Body Weight Regulation
2.1. Epidemiological Studies
2.2. Randomized Controlled Trials
2.3. Possible Mechanisms of Fibre Effects on Body Weight Regulation
3. Insulin Resistance, Type 2 Diabetes Risk, and Blood Glucose Control in Diabetes
3.1. Epidemiological Studies
3.2. Randomized Controlled Trials
3.3. Possible Mechanisms of Fibre Effects on Insulin Resistance
3.4. Diabetes Risk
3.5. Blood Glucose Control
3.6. Possible Mechanisms of Fibre Effects on Blood Glucose Control
3.7. Conclusions
4. Dyslipidaemia
4.1. Epidemiological Studies
4.2. Randomized Controlled Trials
4.3. Possible Mechanisms of Fibre Effects on Dyslipidaemia.
4.4. Conclusions
5. Blood Pressure/Hypertension
5.1. Epidemiological Studies
5.2. Randomized Controlled Trials
5.3. Possible Mechanisms of Fibre Effects on Blood Pressure
5.4. Conclusions
6. Non Alcoholic Fatty Liver Disease
6.1. Epidemiological Studies
6.2. Randomized Controlled trials
6.3. Possible Mechanisms of Fibre Effects on NAFLD
7. Cardiovascular Disease
7.1. Possible Mechanisms of Fibre Effects on Cardiovascular Disease
7.2. Conclusion
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- The GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar]
- Pigeyre, M.; Yazdi, F.T.; Kaur, Y.; Meyre, D. Recent progress in genetics, epigenetics and metagenomics unveils the pathophysiology of human obesity. Clin. Sci. 2016, 130, 943–986. [Google Scholar] [CrossRef] [PubMed]
- Van der Klaauw, A.A.; Farooqi, I.S. The hunger genes: Pathways to obesity. Cell 2015, 161, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Grant, R.W.; Dixit, V.D. Adipose tissue as an immunological organ. Obesity 2015, 23, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; Prinster, A.; Mancini, M.; Giacco, R.; De Natale, C.; Salvatore, M.; Riccardi, G.; Rivellese, A.A.; Annuzzi, G. Liver fat in obesity: Role of type 2 diabetes mellitus and adipose tissue distribution. Eur. J. Clin. Investig. 2011, 41, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Costabile, G.; Annuzzi, G.; Di Marino, L.; De Natale, C.; Giacco, R.; Bozzetto, L.; Cipriano, P.; Santangelo, C.; Masella, R.; Rivellese, A.A. Fasting and post-prandial adipose tissue lipoprotein lipase and hormone-sensitive lipase in obesity and type 2 diabetes. J. Endocrinol. Investig. 2011, 34, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Tchkonia, T.; Thomou, T.; Zhu, Y.; Karagiannides, I.; Pothoulakis, C.; Jensen, M.D.; Kirkland, J.L. Mechanisms and metabolic implications of regional differences among fat depots. Cell MeTable 2013, 17, 644–656. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J. A comprehensive review on metabolic syndrome. Cardiol. Res. Pract. 2014, 2014, 943162. [Google Scholar] [CrossRef] [PubMed]
- Neuschwander-Tetri, B.A.; Caldwell, S.H. Nonalcoholic steatohepatitis: Summary of an AASLD single topic conference. Hepatology 2003, 37, 1202–1219. [Google Scholar] [CrossRef] [PubMed]
- Masulli, M.; Patti, L.; Riccardi, G.; Vaccaro, O.; Annuzzi, G.; Ebbesson, S.O.; Fabsitz, R.R.; Howard, W.J.; Otvos, J.D.; Roman, M.J.; et al. Relation among lipoprotein subfractions and carotid atherosclerosis in Alaskan Eskimos (from the GOCADAN Study). Am. J. Cardiol. 2009, 104, 1516–1521. [Google Scholar] [CrossRef] [PubMed]
- McCullough, A.J. The clinical features, diagnosis and natural history of nonalcoholic fatty liver disease. Clin. Liver Dis. 2004, 8, 521–533. [Google Scholar] [CrossRef] [PubMed]
- Annuzzi, G.; Rivellese, A.A.; Wang, H.; Patti, L.; Vaccaro, O.; Riccardi, G.; Ebbesson, S.O.; Comuzzie, A.G.; Umans, J.G.; Howard, B.V. Lipoprotein subfractions and dietary intake of n − 3 fatty acid: The Genetics of Coronary Artery Disease in Alaska Natives study. Am. J. Clin. Nutr. 2012, 95, 1315–1322. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E.; da Silva, A.A.; do Carmo, J.M.; Dubinion, J.; Hamza, S.; Munusamy, S.; Smith, G.; Stec, D.E. Obesity-induced hypertension: Role of sympathetic nervous system, leptin, and melanocortins. J. Biol. Chem. 2010, 285, 17271–17276. [Google Scholar] [CrossRef] [PubMed]
- DeVries, J.W. The definition of dietary fibre. Cereal Foods World 2001, 46, 112–129. [Google Scholar]
- McRorie, J.W., Jr. Evidence-based approach to fiber supplements and clinically meaningful health benefits, part 1: What to look for and how to recommend an effective fiber therapy. Nutr. Today 2015, 50, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Apovian, C.M.; Aronne, L.J.; Bessesen, D.H.; McDonnell, M.E.; Murad, M.H.; Pagotto, U.; Ryan, D.H.; Still, C.D.; Endocrine Society. Pharmacological management of obesity: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. MeTab. 2015, 100, 342–362. [Google Scholar] [CrossRef] [PubMed]
- Garve, W.T.; Mechanick, J.I.; Brett, E.M.; Garber, A.J.; Hurley, D.L.; Jastreboff, A.M.; Nadolsky, K.; Pessah-Pollack, R.; Plodkowski, R.; Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr. Pract. 2016, 22, S1–S203. [Google Scholar] [CrossRef] [PubMed]
- American College of Cardiology/American Heart Association Task Force on Practice Guidelines, Obesity Expert Panel, 2013. Expert Panel Report: Guidelines (2013) for the management of overweight and obesity in adults. Obesity 2014, 22, S41–S410. [Google Scholar]
- Newby, P.K.; Maras, J.; Bakun, P.; Muller, D.; Ferrucci, L.; Tucker, K.L. Intake of whole grains, refined grains, and cereal fibre measured with 7-d diet records and associations with risk factors for chronic disease. Am. J. Clin. Nutr. 2007, 86, 1745–1753. [Google Scholar] [CrossRef] [PubMed]
- McKeown, N.M.; Yoshida, M.; Shea, M.K.; Jacques, P.F.; Lichtenstein, A.H.; Rogers, G.; Booth, S.L.; Saltzman, E. Whole-Grain Intake and Cereal Fibre Are Associated with Lower Abdominal Adiposity in Older Adults. J. Nutr. 2009, 139, 1950–1955. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Willett, W.C.; Manson, J.E.; Hu, F.B.; Rosner, B.; Colditz, G. Relation between changes in intakes of dietary fibre and grain products and changes in weight and development of obesity among middle-aged women. Am. J. Clin. Nutr. 2003, 78, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Pereira, M.A.; Kroenke, C.H.; Hilner, J.E.; Van Horn, L.; Slattery, M.L.; Jacobs, D.R. Dietary fibre, weight gain, and cardiovascular disease risk factors in young adults. JAMA 1999, 282, 1539–1546. [Google Scholar] [CrossRef] [PubMed]
- Koh-Banerjee, P.; Franz, M.; Sampson, L.; Liu, S.; Jacobs, D.R.J.; Spiegelman, D.; Willett, W.; Rimm, E. Changes in whole-grain, bran, and cereal fibre consumption in relation to 8-yr weight gain among men. Am. J. Clin. Nutr. 2004, 80, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Schulz, M.; Nothlings, U.; Hoffmann, K.; Bergmann, M.M.; Boeing, H. Identification of a food pattern characterized by high-fibre and low-fat food choices associated with low prospective weight change in the EPIC-Potsdam cohort. J. Nutr. 2005, 135, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Alexander, K.E.; Ventura, E.E.; Toledo-Corral, C.M.; Goran, M.I. Inverse relation between dietary fibre intake and visceral adiposity in overweight Latino youth. Am. J. Clin. Nutr. 2009, 90, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Du, H.; van der A, D.L.; Boshuizen, H.C.; Forouhi, N.G.; Wareham, N.J.; Halkjær, J.; Tjønneland, A.; Overvad, K.; Jakobsen, M.U.; Boeing, H.; et al. Dietary fibre and subsequent changes in body weight and waist circumference in European men and women. Am. J. Clin. Nutr. 2010, 91, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Koh-Banerjee, P.; Chu, N.F.; Spiegelman, D.M.; Rosner, B.; Colditz, G.; Willett, W.; Rimm, E. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16,587 US men. Am. J. Clin. Nutr. 2003, 78, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Pol, K.; Christensen, R.; Bartels, E.M.; Raben, A.; Tetens, I.; Kristensen, M. Whole grain and body weight changes in apparently healthy adults: A systematic review and meta-analysis of randomized controlled studies. Am. J. Clin. Nutr. 2013, 98, 872–884. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; de Souza, R.J.; Choo, V.L.; Ha, V.; Cozma, A.I.; Chiavaroli, L.; Mirrahimi, A.; Blanco Mejia, S.; Di Buono, M.; Bernstein, A.M.; et al. Effects of dietary pulse consumption on body weight: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2016, 103, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Mytton, O.T.; Nnoaham, K.; Eyles, H.; Scarborough, P.; Mhurchu, C.N. Systematic review and meta-analysis of the effect of increased vegetable and fruit consumption on body weight and energy intake. BMC Public Health 2014, 14, 886–897. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.V.; Hannon, B.A.; An, R.; Holscher, H.D. Effects of isolated soluble fibre supplementation on body weight, glycemia, and insulinemia in adults with overweight and obesity: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2017, 106, 1514–1528. [Google Scholar] [CrossRef] [PubMed]
- McRae, M.P. Health Benefits of Dietary Whole Grain: An Umbrella Review of Meta-analyses. J. Chiropr. Med. 2017, 16, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Kirwan, J.P.; Malin, S.K.; Scelsi, A.R.; Kullman, E.L.; Navaneethan, S.D.; Pagadala, M.R.; Haus, J.M.; Filion, J.; Godin, J.P.; Kochhar, S.; et al. A Whole-Grain Diet reduces Cardiovascular Risk Factors in Overweight and Obese Adults: A Randomized Controlled Trial. J. Nutr. 2016, 146, 2244–2251. [Google Scholar] [CrossRef] [PubMed]
- Papathanasopoulos, A.; Camilleri, M. Dietary Fibre Supplements: Effects in Obesity and Metabolic Syndrome and Relationship to Gastrointestinal Functions. Gastroenterology 2010, 138, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Karl, J.P.; Saltzman, E. The Role of Whole Grains in Body Weight Regulation. Adv. Nutr. 2012, 3, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, D.; Miguel, M.; Aleixandre, A. Dietary fibre, gut peptides, and adipocytokines. J. Med. Food 2012, 15, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Costabile, G.; Griffo, E.; Cipriano, P.; Vetrani, C.; Vitale, M.; Mamone, G.; Rivellese, AA.; Riccardi, G.; Giacco, R. Subjective satiety and plasma PYY concentration after wholemeal pasta. Appetite 2018, 125, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.A.; Grant, L.J.; Gidley, M.J.; Mikkelsen, D. Gut Fermentation of Dietary Fibres: Physico-Chemistry of Plant Cell Walls and Implications for Health. Int. J. Mol. Sci. 2017, 18, 2203. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, D.K.; Puniya, M.; Shandilya, U.K.; Dhewa, T.; Kumar, N.; Kumar, S.; Puniya, A.K.; Shukla, P. Gut Microbiota Modulation and Its Relationship with Obesity Using Prebiotic Fibres and Probiotics: A Review. Front. Microbiol. 2017, 8, 563. [Google Scholar] [CrossRef] [PubMed]
- Sleeth, M.L.; Thompson, E.L.; Ford, H.E.; Zac-Varghese, S.E.; Frost, G. Free fatty acid receptor 2 and nutrient sensing: A proposed role for fibre, fermentable carbohydrates and short-chain fatty acids in appetite regulation. Nutr. Res. Rev. 2010, 23, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Kasubuchi, M.; Hasegawa, S.; Hiramatsu, T.; Ichimura, A.; Kimura, I. Dietary gut microbial metabolites, short-chain fatty acids, and host metabolic regulation. Forum Nutr. 2015, 7, 2839–2849. [Google Scholar] [CrossRef] [PubMed]
- Giacco, R.; Della Pepa, G.; Luongo, D.; Riccardi, G. Whole grain intake in relation to body weight: From epidemiological evidence to clinical trials. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 901–908. [Google Scholar] [CrossRef] [PubMed]
- Parkar, S.G.; Stevenson, D.E.; Skinner, M.A. The potential influence of fruit polyphenols on colonic microflora and human gut health. Int. J. Food Microbiol. 2008, 124, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Simpson, H.L.; Campbell, B.J. Review article: Dietary fibre-microbiota interactions. Aliment. Pharmacol. Ther. 2015, 42, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Roach, A.K.; Sparks, K.C.; Marquart, L.; D’Agostino, R.B., Jr.; Mayer-Davis, E.J. Whole-grain intake and insulin sensitivity: The Insulin Resistance Atherosclerosis Study. Am. J. Clin. Nutr. 2003, 78, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.A.; Jacobs, D.R., Jr.; Pins, J.J.; Raatz, S.K.; Gross, M.D.; Slavin, J.L.; Seaquist, E.R. Effect of whole grains on insulin sensitivity in overweight hyperinsulinemic adults. Am. J. Clin. Nutr. 2002, 75, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Juntunen, K.S.; Laaksonen, D.E.; Poutanen, K.S.; Niskanen, L.K.; Mykkänen, H.M. High fiber rye bread and insulin secretion and sensitivity in healthy postmenopausal women. Am. J. Clin. Nutr. 2003, 77, 385–391. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, G.H.; Noakes, M.; Royle, P.J.; Foster, P.R. Whole grain rye and wheat foods and markers of bowel health in overweight middle aged men. Am. J. Clin. Nutr. 2003, 77, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Andersson, A.; Tengblad, S.; Karlström, B.; Kamal Eldin, A.; Landberg, R.; Basu, S.; Aman, P.; Vessby, B. Whole grain foods do not affect insulin sensitivity or markers of lipid peroxidation and inflammation in healthy, moderately overweight subjects. J. Nutr. 2007, 137, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Katcher, H.I.; Legro, R.S.; Kunselman, A.R.; Gillies, P.J.; Demers, L.M.; Bagshaw, D.M.; Kris-Etherton, P.M. The effects of a whole grain enriched hypocaloric diet on cardiovascular disease risk factors in men and women with metabolic syndrome. Am. J. Clin. Nutr. 2008, 87, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Giacco, R.; Clemente, G.; Cipriano, D.; Luongo, D.; Viscovo, D.; Patti, L.; Di Marino, L.; Giacco, A.; Naviglio, D.; Bianchi, M.A.; et al. Effects of the regular consumption of wholemeal wheat foods on cardiovascular risk factors in healthy people. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Brownlee, I.A.; Moore, C.; Chatfield, M.; Richardson, D.P.; Ashby, P.; Kuznesof, S.A.; Jebb, S.A.; Seal, C.J. Markers of cardiovascular risk are not changed by increased whole grain intake: The WHOLEheart study, a randomised, controlled dietary intervention. Br. J. Nutr. 2010, 104, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Giacco, R.; Lappi, J.; Costabile, G.; Kolehmainen, M.; Schwab, U.; Landberg, R.; Uusitupa, M.; Poutanen, K.; Pacini, G.; Rivellese, A.A.; et al. Effects of rye and whole wheat versus refined cereal foods on metabolic risk factors: A randomised controlled two-centre intervention study. Clin. Nutr. 2013, 32, 941–949. [Google Scholar] [CrossRef] [PubMed]
- Giacco, R.; Costabile, G.; Della Pepa, G.; Anniballi, G.; Griffo, E.; Mangione, A.; Cipriano, P.; Viscovo, D.; Clemente, G.; Landberg, R.; et al. A whole-grain cereal-based diet lowers postprandial plasma insulin and triglyceride levels in individuals with metabolic syndrome. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 837–844. [Google Scholar] [CrossRef] [PubMed]
- He, L.X.; Zhao, J.; Huang, Y.S.; Li, Y. The difference between oats and beta-glucan extract intake in the management of HbA1c, fasting glucose and insulin sensitivity: A meta-analysis of randomized controlled trials. Food Funct. 2016, 7, 1413–1428. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, C.; Kishimoto, Y.; Kanahori, S.; Yamamoto, T.; Okuma, K.; Yamamoto, K. Improvement effect of resistant maltodextrin in humans with metabolic syndrome by continuous administration. J. Nutr. Sci. Vitaminol. 2012, 58, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Guerin-Deremaux, L.; Pochat, M.; Wils, D.; Reifer, C.; Miller, L.E. NUTRIOSE dietary fiber supplementation improves insulin resistance and determinants of metabolic syndrome in overweight men: A double-blind, randomized, placebo-controlled study. Appl. Physiol. Nutr. MeTable 2010, 35, 773–782. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.L.; Thomas, E.L.; Bell, J.D.; Frost, G.S.; Robertson, M.D. Resistant starch improves insulin sensitivity in metabolic syndrome. Diabet. Med. 2010, 27, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.D.; Wright, J.W.; Loizon, E.; Debard, C.; Vidal, H.; Shojaee-Moradie, F.; Russell-Jones, D.; Umpleby, A.M. Insulin-sensitizing effects on muscle and adipose tissue after dietary fiber intake in men and women with metabolic syndrome. J. Clin. Endocrinol. MeTable 2012, 97, 3326–3332. [Google Scholar] [CrossRef] [PubMed]
- Layden, B.T.; Yalamanchi, S.K.; Wolever, T.M.; Dunaif, A.; Lowe, W.L., Jr. Negative association of acetate with visceral adipose tissue and insulin levels. Diabetes Metab. Syndr. Obes. 2012, 5, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Canfora, E.E.; Jocken, J.W.; Blaak, E.E. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat. Rev. Endocrinol. 2015, 11, 577–591. [Google Scholar] [CrossRef] [PubMed]
- Vetrani, C.; Costabile, G.; Luongo, D.; Naviglio, D.; Rivellese, A.A.; Riccardi, G.; Giacco, R. Effects of whole-grain cereal foods on plasma short chain fatty acid concentrations in individuals with the metabolic syndrome. Nutrition 2016, 32, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Weitkunat, K.; Stuhlmann, C.; Postel, A.; Rumberger, S.; Fankhänel, M.; Woting, A.; Petzke, K.J.; Gohlke, S.; Schulz, T.J.; Blaut, M.; et al. Short-chain fatty acids and inulin, but not guar gum, prevent diet-induced obesity and insulin resistance through differential mechanisms in mice. Sci Rep. 2017, 7, 6109. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.; Kassis, A.; Major, G.; Chou, C.J. Is the gut microbiota a new factor contributing to obesity and its metabolic disorders? J. Obes. 2012, 2012, 879151. [Google Scholar] [PubMed]
- Caricilli, A.M.; Saad, M.J. The role of gut microbiota on insulin resistance. Nutrients 2013, 5, 829–851. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, S.T.; dos Santos, C.A.; Bressan, J. Intestinal microbiota; relevance to obesity and modulation by prebiotics and probiotics. Nutr. Hosp. 2013, 28, 1039–1048. [Google Scholar] [PubMed]
- Cameron-Smith, D.; Habito, R.; Barnett, M.; Collier, G.R. Dietary guar gum improves insulin sensitivity in streptozotocin-induced diabetic rats. J. Nutr. 1997, 127, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.J.; Sawamura, M.; Ikeda, K.; Igawa, S.; Yamori, Y. Soluble dietary fibre improves insulin sensitivity by increasing muscle GLUT-4 content in stroke-prone spontaneously hypertensive rats. Clin. Exp. Pharmacol. Physiol. 2000, 27, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Salmerón, J.; Manson, J.E.; Stampfer, M.J.; Colditz, G.A.; Wing, A.L.; Willett, W.C. Dietary fibre, glycaemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA 1997, 277, 472–477. [Google Scholar] [CrossRef] [PubMed]
- The InterAct Consortium. Dietary fibre and incidence of type 2 diabetes in eight European countries: The EPIC-InterAct study and a meta-analysis of prospective studies. Diabetologia 2015, 58, 1394–1408. [Google Scholar]
- King, D.E.; Mainous, A.G.; Lambourne, C.A. Trends in dietary fibre intake in the United States, 1999–2008. J. Acad. Nutr. Diet. 2012, 112, 642–648. [Google Scholar] [CrossRef] [PubMed]
- McGill, C.R.; Fulgoni, V.L.; Devareddy, L. Ten-year trends in fibre and whole grain intakes and food sources for the United States population: National health and nutrition examination survey 2001–2010. Nutrients 2015, 7, 1119–1130. [Google Scholar] [CrossRef] [PubMed]
- Fungwe, T.V.; Bente, L.; Hiza, H. Food Supply and Dietary Fibre: Its Availability and Effect on Health; Nutrition Insights 36; USDA Center for Nutrition Policy and Promotion: Alexandria, VA, USA, 2007.
- Lindström, J.; Peltonen, M.; Eriksson, J.G.; Louheranta, A.; Fogelholm, M.; Uusitupa, M.; Tuomilehto, J. High-fibre, low-fat diet predicts long-term weight loss and decreased type 2 diabetes risk: The Finnish Diabetes Prevention Study. Diabetologia 2006, 49, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Von Ruesten, A.; Feller, S.; Bergmann, M.M.; Boeing, H. Diet and risk of chronic diseases: Results from the first 8 years of follow-up in the EPIC-Potsdam study. Eur. J. Clin. Nutr. 2013, 67, 412–419. [Google Scholar] [CrossRef] [PubMed]
- InterAct, Consortium; Romaguera, D.; Guevara, M.; Norat, T.; Langenberg, C.; Forouhi, N.G.; Sharp, S.; Slimani, N.; Schulze, M.B.; Buijsse, B.; et al. Mediterranean diet and type 2 diabetes risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) study: The InterAct project. Diabetes Care 2011, 34, 1913–1918. [Google Scholar]
- Martinez-Gonzalez, M.A.; Salas-Salvado, J.; Estruch, R.; Corella, D.; Fito, M.; Ros, E. Benefits of the Mediterranean diet: Insights from the PREDIMED study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Vitale, M.; Masulli, M.; Rivellese, A.A.; Babini, A.C.; Boemi, M.; Bonora, E.; Buzzetti, R.; Ciano, O.; Cignarelli, M.; Cigolini, M.; et al. Influence of dietary fat and carbohydrates proportions on plasma lipids, glucose control and low grade inflammation in patients with type 2 diabetes—The TOSCA.IT Study. Eur. J. Nutr. 2016, 55, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- Post, R.E.; Mainous, A.G.; King, D.E.; Simpson, K.N. Dietary fibre for the treatment of type 2 diabetes mellitus: A meta-analysis. J. Am. Board Fam. Med. 2012, 25, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.M.; Kramer, C.K.; de Almeida, J.C.; Steemburgo, T.; Gross, J.L.; Azevedo, M.J. Fiber intake and glycemic control in patients with type 2 diabetes mellitus: A systematic review with meta-analysis of randomized controlled trials. Nutr. Rev. 2013, 71, 790–801. [Google Scholar] [CrossRef] [PubMed]
- Gibb, R.D.; McRorie, J.W., Jr.; Russell, D.A.; Hasselblad, V.; D’Alessio, D.A. Psyllium fiber improves glycemic control proportional to loss of glycemic control: A meta-analysis of data in euglycemic subjects, patients at risk of type 2 diabetes mellitus, and patients being treated for type 2 diabetes mellitus. Am. J. Clin. Nutr. 2015, 102, 1604–1614. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Chaimani, A.; Hoffmann, G.; Schwedhelm, C.; Boeing, H. A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus. Eur. J. Epidemiol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Marventano, S.; Vetrani, C.; Vitale, M.; Godos, J.; Riccardi, G.; Grosso, G. Whole Grain Intake and Glycaemic Control in Healthy Subjects: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2017, 19, 9. [Google Scholar] [CrossRef] [PubMed]
- Christensen, A.S.; Viggers, L.; Hasselström, K.; Gregersen, S. Effect of fruit restriction on glycemic control in patients with type 2 diabetes—A randomized trial. Nutr. J. 2013, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Muraki, I.; Imamura, F.; Manson, J.E.; Hu, F.B.; Willett, W.C.; van Dam, R.M.; Sun, Q. Fruit consumption and risk of type 2 diabetes: Results from three prospective longitudinal cohort studies. BMJ 2013, 347, f5001. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; Alderisio, A.; Giorgini, M.; Barone, F.; Giacco, A.; Riccardi, G.; Rivellese, A.A.; Annuzzi, G. Extra-Virgin Olive Oil Reduces Glycemic Response to a High-Glycemic Index Meal in Patients With Type 1 Diabetes: A Randomized Controlled Trial. Diabetes Care 2016, 39, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Bowman, R.; Welch, A.A.; Luben, R.N.; Wareham, N.; Khaw, K.-T.; Bingham, S.A. Apolipoprotein E polymorphisms, dietary fat and fibre, and serum lipids: The EPIC Norfolk study. Eur. Heart J. 2007, 28, 2930–2936. [Google Scholar] [CrossRef] [PubMed]
- Vitale, M.; Masulli, M.; Cocozza, S.; Anichini, R.; Babini, A.C.; Boemi, M.; Bonora, E.; Buzzetti, R.; Carpinteri, R.; Caselli, C.; et al. Sex differences in food choices, adherence to dietary recommendations and plasma lipid profile in type 2 diabetes e The TOSCA.IT study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Ye, E.; Chacko, S.; Chou, E.; Kugizaki, M.; Liu, S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J. Nutr. 2012, 142, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Hollander, P.; Ross, A.; Kristensen, M. Whole-grain and blood lipid changes in apparently healthy adults: A systematic review and meta-analysis of randomized controlled studies. Am. J. Clin. Nutr. 2015, 102, 556–572. [Google Scholar] [CrossRef] [PubMed]
- Hartley, L.; May, M.D.; Loveman, E.; Colquitt, J.L.; Rees, K. Dietary fibre for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.A.; Hartley, L.; Loveman, E.; Colquitt, J.L.; Jones, H.M.; Al-Khudairy, L.; Clar, C.; Germanò, R.; Lunn, H.R.; Frost, G.; et al. Whole grain cereals for the primary or secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, A.; Beck, E.J.; Tosh, S.; Wolever, T.M.S. Cholesterol-lowering effects of oat β-glucan: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2014, 100, 1413–1421. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Sun, X.; Wang, M.; Zhang, C.; Cao, Y.; Mo, G.; Liang, J.; Zhu, S. Quantitative assessment of the effects of β-glucan consumption on serum lipid profile and glucose level in hypercholesterolemic subjects. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.V.; Sievenpiper, J.L.; Zurbau, A.; Blanco Mejia, S.; Jovanovski, E.; Au-Yeung, F.; Jenkins, A.L.; Vuksan, V. A systematic review and meta-analysis of randomized controlled trials of the effect of barley β-glucan on LDL-C, non-HDL-C and apoB for cardiovascular disease risk reduction. Eur. J. Clin. Nutr. 2016, 70, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.V.T.; Sievenpiper, J.L.; Zurbau, A.; Blanco Mejia, S.; Jovanovski, E.; Au-Yeung, F.; Jenkins, A.L.; Vuksan, V. The effect of oat β-glucan on LDL-cholesterol, non-HDL-cholesterol and apoB for CVD risk reduction: A systematic review and meta-analysis of randomised-controlled trials. Br. J. Nutr. 2016, 116, 1369–1382. [Google Scholar] [CrossRef] [PubMed]
- Bazzano, L.; Thompson, A.; Tees, M.; Nguyen, C.; Winham, D. Non-Soy Legume Consumption Lowers Cholesterol Levels: A Meta-Analysis of Randomized Controlled Trials. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, A.M.; Titgemeier, B.; Kirkpatrick, K.; Golubic, M.; Roizen, M.F. Major Cereal Grain Fibres and Psyllium in Relation to Cardiovascular Health. Nutrients 2013, 5, 1471–1487. [Google Scholar] [CrossRef] [PubMed]
- Ha, V.; Sievenpiper, J.L.; de Souza, R.J.; Jayalath, V.H.; Mirrahimi, A.; Agarwal, A.; Chiavaroli, L.; Blanco Mejia, S.; Sacks, F.M.; Di Buono, M.; et al. Effect of dietary pulse intake on established therapeutic lipid targets for cardiovascular risk reduction: A systematic review and meta-analysis of randomized controlled trials. CMAJ 2014, 186, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Pirro, M.; Vetrani, C.; Bianchi, C.; Mannarino, M.R.; Bernini, F.; Rivellese, A.A. Joint position statement on “Nutraceuticals for the treatment of hypercholesterolemia” of the Italian Society of Diabetology (SID) and of the Italian Society for the Study of Arteriosclerosis (SISA). Nutr. Metab. Cardiovasc. Dis. 2017, 27, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Prabhakar, M.; Ju, J.; Long, H.; Zhou, H.W. Effect of inulin-type fructans on blood lipid profile and glucose level: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Clin. Nutr. 2017, 71, 9–20. [Google Scholar] [CrossRef] [PubMed]
- De Natale, C.; Annuzzi, G.; Bozzetto, L.; Mazzarella, R.; Costabile, G.; Ciano, O.; Riccardi, G.; Rivellese, A.A. Effects of a Plant-Based High-Carbohydrate/High-Fibre Diet Versus High-Monounsaturated Fat/Low-Carbohydrate Diet on Postprandial Lipids in Type 2 Diabetic Patients. Diabetes Care 2009, 32, 2168–2173. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; De Natale, C.; Di Capua, L.; Della Corte, G.; Patti, L.; Maione, S.; Riccardi, G.; Rivellese, A.A.; Annuzzi, G. The association of hs-CRP with fasting and postprandial plasma lipids in patients with type 2 diabetes is disrupted by dietary monounsaturated fatty acids. Acta Diabetol. 2013, 50, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; Annuzzi, G.; Costabile, G.; Costagliola, L.; Giorgini, M.; Alderisio, A.; Strazzullo, A.; Patti, L.; Cipriano, P.; Mangione, A.; et al. A CHO/fibre diet reduces and a MUFA diet increases postprandial lipaemia in type 2 diabetes: No supplementary effects of low-volume physical training. Acta Diabetol. 2014, 51, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Othman, R.A.; Moghadasian, M.H.; Jones, P.J. Cholesterol-lowering effects of oat β-glucan. Nutr. Rev. 2011, 69, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; Annuzzi, G.; Corte, G.D.; Patti, L.; Cipriano, P.; Mangione, A.; Riccardi, G.; Rivellese, A.A. Ezetimibe beneficially influences fasting and postprandial triglyceride-rich lipoproteins in type 2 diabetes. Atherosclerosis 2011, 217, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Desroches, S.; Jenkins, D.J.; Kendall, C.W.; Marchie, A.; Faulkner, D.; Vidgen, E.; Lapsley, K.G.; Trautwein, E.A.; Parker, T.L.; et al. Combined effects of a dietary portfolio of plant sterols, vegetable protein, viscous fibre and almonds on LDL particle size. Br. J. Nutr. 2004, 92, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Lairon, D.; Play, B.; Jourdheuil-Rahmani, D. Digestible and indigestible carbohydrates: Interactions with postprandial lipid metabolism. J. Nutr. Biochem. 2007, 18, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Vernay, M.; Aïdara, M.; Salanave, B.; Deschamps, V.; Malon, A.; Oleko, A.; Mallion, J.M.; Hercberg, S.; Castetbon, K. Diet and blood pressure in 18–74-year-old adults: The French Nutrition and Health Survey (ENNS, 2006–2007). J. Hypertens. 2012, 30, 1920–1927. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Flood, V.M.; Rochtchina, E.; Baur, L.A.; Smith, W.; Mitchell, P. Influence of High Glycemic Index and Glycemic Load Diets on Blood Pressure During Adolescence. Hypertension 2012, 59, 1272–1277. [Google Scholar] [CrossRef] [PubMed]
- Aljuraiban, G.S.; Griep, L.M.O.; Chan, Q.; Daviglus, M.L.; Stamler, J.; Van Horn, L.; Elliott, P.; Frost, G.S. Total, insoluble and soluble dietary fibre intake in relation to blood pressure: The INTERMAP Study. Br. J. Nutr. 2015, 114, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Lairon, D.; Arnault, N.; Bertrais, S.; Planells, R.; Clero, E.; Hercberg, S.; Boutron-Ruault, M.C. Dietary fiber intake and risk factors for cardiovascular disease in French adults. Am. J. Clin. Nutr. 2005, 82, 1185–1194. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Gaziano, J.M.; Liu, S.; Manson, J.E.; Buring, J.E.; Sesso, H.D. Whole- and refined-grain intakes and the risk of hypertension in women. Am. J. Clin. Nutr. 2007, 86, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Streppel, M.T.; Arends, L.R.; Van’t Veer, P.; Grobbee, D.E.; Geleijnse, J.M. Dietary fiber and blood pressure: A meta-analysis of randomized placebo-controlled trials. Arch. Intern. Med. 2005, 165, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Whelton, S.P.; Hyre, A.D.; Pedersen, B.; Yi, Y.; Whelton, P.K.; He, J. Effect of dietary fiber intake on blood pressure: A meta-analysis of randomized, controlled clinical trials. J. Hypertens. 2005, 23, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.L.; Greenwood, D.C.; Threapleton, D.E.; Cleghorn, C.L.; Nykjaer, C.; Woodhead, C.E.; Gale, C.P.; Burley, V.J. Effects of dietary fibre type on blood pressure: A systematic review and meta-analysis of randomized controlled trials of healthy individuals. J. Hypertens. 2015, 33, 897–911. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.; Jovanovski, E.; Ho, H.V.T.; Marques, A.C.R.; Zurbau, A.; Mejia, S.B.; Sievenpiper, J.L.; Vuksan, V. The effect of viscous soluble fiber on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Schulman, I.H.; Zhou, M.S. Vascular insulin resistance: A potential link between cardiovascular and metabolic diseases. Curr. Hypertens. Rep. 2009, 11, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.S.; Schulman, I.H.; Raij, L. Vascular inflammation, insulin resistance, and endothelial dysfunction in salt-sensitive hypertension: Role of nuclear factor kappa B activation. J. Hypertens. 2010, 28, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, G.; Sachinidis, A.; Michaelsen, F.; Bohm, M.; Seewald, S.; Vetter, H. Upregulation of vascular angiotensin II receptor gene expression by low-density lipoprotein in vascular smooth muscle cells. Circulation 1997, 95, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Haas, J.T.; Francque, S.; Stael, B. Pathophysiology and mechanisms of nonalcoholic fatty liver disease. Annu. Rev. Physiol. 2016, 78, 181–205. [Google Scholar] [CrossRef] [PubMed]
- Della Pepa, G.; Vetrani, C.; Lombardi, G.; Bozzetto, L.; Annuzzi, G.; Rivellese, A.A. Isocaloric dietary changes and non-alcoholic fatty liver disease in high cardiometabolic risk individuals. Nutrients 2017, 9, 1065. [Google Scholar] [CrossRef] [PubMed]
- Cortez-Pinto, H.; Jesus, L.; Barros, H.; Lopes, C.; Moura, M.C.; Camilo, M.E. How different is the dietary pattern in non-alcoholic steatohepatitis patients? Clin. Nutr. 2006, 25, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; De Michieli, F.; Cassader, M.; Rizzetto, M.; Durazzo, M.; Faga, E.; Silli, B.; Pagano, G. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology 2003, 37, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Mirmiran, P.; Amirhamidi, Z.; Ejtahed, H.S.; Bahadoran, Z.; Azizi, F. Relationship between Diet and Non-alcoholic Fatty Liver Disease: A Review Article. Iran J. Public Health 2017, 46, 1007–1017. [Google Scholar] [PubMed]
- Razavi Zade, M.; Telkabadi, M.H.; Bahmani, F.; Salehi, B.; Farshbaf, S.; Asemi, Z. The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: A randomized clinical trial. Liver Int. 2016, 36, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Zelber-Sagi, S.; Salomone, F.; Mlynarsky, L. The Mediterranean dietary pattern as the diet of choice for non-alcoholic fatty liver disease: Evidence and plausible mechanisms. Liver Int. 2017, 37, 936–949. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; Prinster, A.; Annuzzi, G.; Costagliola, L.; Mangione, A.; Vitelli, A.; Mazzarella, R.; Longobardo, M.; Mancini, M.; Vigorito, C.; et al. Liver fat is reduced by an isoenergetic MUFA diet in a controlled randomized study in type 2 diabetic patients. Diabetes Care 2012, 35, 1429–1435. [Google Scholar] [CrossRef] [PubMed]
- Daubioul, C.A.; Horsmans, Y.; Lambert, P.; Danse, E.; Delzenne, N.M. Effects of oligofructose on glucose and lipid metabolism in patients with nonalcoholic steatohepatitis: Results of a pilot study. Eur. J. Clin. Nutr. 2005, 59, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Barrera, F.; George, J. The role of diet and nutritional intervention for the management of patients with NAFLD. Clin. Liver Dis. 2014, 18, 91–112. [Google Scholar] [CrossRef] [PubMed]
- Parnell, J.A.; Reimer, A.R. Prebiotic fiber modulation of the gut microbiota improves risk factors for obesity and the metabolic syndrome. Gut Microbes 2012, 3, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, L.; Annuzzi, G.; Ragucci, M.; Di Donato, O.; Della Pepa, G.; Della Corte, G.; Griffo, E.; Anniballi, G.; Giacco, A.; Mancini, M.; et al. Insulin resistance, postprandial GLP-1 and adaptive immunity are the main predictors of NAFLD in a homogeneous population at high cardiovascular risk. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Threapleton, D.E.; Greenwood, D.C.; Evans, C.E.; Cleghorn, C.L.; Nykjaer, C.; Woodhead, C.; Cade, J.E.; Gale, C.P.; Burley, V.J. Dietary fibre intake and risk of cardiovascular disease: Systematic review and meta-analysis. BMJ 2013, 347, f6879. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Qian, Y.; Pan, Y.; Li, P.; Yang, J.; Ye, X.; Xu, G. Association between dietary fibre intake and risk of coronary heart disease: A meta-analysis. Clin. Nutr. 2015, 34, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Ning, H.; Van Horn, L.; Shay, C.M.; Lloyd-Jones, D.M. Associations of dietary fibre intake with long-term predicted cardiovascular disease risk and C-reactive protein levels (from the National Health and Nutrition Examination Survey Data [2005–2010]). Am. J. Cardiol. 2014, 113, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Buil-Cosiales, P.; Zazpe, I.; Toledo, E.; Corella, D.; Salas-Salvadó, J.; Diez-Espino, J.; Ros, E.; Fernandez-Creuet Navajas, J.; Santos-Lozano, J.M.; Arós, F.; et al. Fibre intake and all-cause mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am. J. Clin. Nutr. 2014, 100, 1498–1507. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Je, Y. Dietary fibre intake and mortality from cardiovascular disease and all cancers: A meta-analysis of prospective cohort studies. Arch. Cardiovasc. Dis. 2016, 109, 39–54. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
| Fibres | Functional Properties | Main Sources | ||
|---|---|---|---|---|
| Viscosity | Solubility | Fermentation | ||
| Bran | Low | Low | Low | Wholegrain |
| Cellulose | Vegetables | |||
| Hemicellulose | Vegetables | |||
| Lignin | Seeds | |||
| Inulin | Low | High | High | Roots and tubers |
| Dextrin | Chemically altered wheat and corn starch | |||
| Oligosaccharides | Fruits, vegetables, legumes, grains | |||
| Resistant starch | Type I: Wholegrain; Type II: High-amylose maize starch, raw potato and banana; Type III: Cooked and cooled starchy foods; Type IV: Chemically modified starches; Type V: Amylose-lipid complex | |||
| Pectin | High | High | High | Fruits, vegetables, legumes |
| β-Glucan | Oat and barley | |||
| Glucomannan | Tuberous roots of the Konjac plant | |||
| Guar gum | Leguminous seed plants (guar, locust bean), seaweed extracts (carrageenan, alginates), microbial gums (xanthan, gellan) | |||
| Psyllium | High | High | Low | Husks of ripe seeds from Plantago ovate |
| Methylcellulose | Food additive | |||
| Author, Year [Reference] | Study Design | Study Population Participants Age BMI Health Status | Intervention and Doses | Duration Weeks | Observed Effects |
|---|---|---|---|---|---|
| Pol, 2013 [28] | Meta-analysis of 26 RCTs | 2060 M/F 18–70 years 18.5–35.8 kg/m2 Healthy | Whole grain (mean dose: 84.1 g/day) vs. refined grain | 2–16 | = BW ↓ body fat: −0.48% vs. refined grain |
| Kim, 2016 [29] | Meta-analysis of 21 RCTs | 940 M/F 47–57 years 27.6–31.4 kg/m2 Metabolic syndrome | Dietary pulses (mean dose: 142 g/day) vs. control | 4–12 | ↓ BW: −0.34 kg vs. control |
| Mytton, 2014 [30] | Meta-analysis of 8 RCTs | 1026 M/F 30–75 years 23.7–37.8 kg/m2 Healthy | High fruit and vegetables vs. low fruit and vegetables consumption (mean dose difference in vegetables and fruit consumption between arms 133 g/day) | 4–52 | ↓ BW: −0.54 kg vs. low fruit and vegetables |
| Thompson, 2017 [31] | Meta-analysis of 12 RCTs | 609 M/F 20–70 years 25–35 kg/m2 Healthy | Soluble fibre supplementation (mean dose: 18.5 g/day) vs. control | 2–17 | ↓ BMI: −0.84 kg ↓ BW: −2.52 kg ↓ body fat: −0.41% vs. control |
| Author, Year [Reference] | Study Design | Study Population Participants Age BMI Health Status | Intervention and Doses | Duration Weeks | Observed Effects |
|---|---|---|---|---|---|
| Fibre from whole grain | |||||
| Pereira, 2002 [46] | RCT | 11 M/F 41.6 years 30.2 kg/m2 Hyperinsulinemic | Whole-grain products (fibre 28 g/day) vs. refined-grain products (fibre 18 g/day) | 6 | ↑ Insulin sensitivity (euglycemic hyperinsulinemic clamp tests): +0.07 × 10−4 mmol·kg−1·min−1 per pmol/L = BW vs. refined-grain products |
| Juntunen, 2003 [47] | RCT | 20 F 59 years 28 kg/m2 Healthy | Rye whole-grain bread (fibre 46 g/day) vs. White wheat bread (fibre 14 g/day) | 8 | = Insulin sensitivity (FSIGT) = BW vs. White wheat bread |
| McIntosh, 2003 [48] | RCT | 28 M 40–65 years 30 kg/m2 Healthy | Rye whole-grain diet (fibre 32 g/day) vs. Wheat whole-grain diet (fibre 32 g/day) vs. Low fibre diet (fibre 19 g/day) | 4 | = Insulin resistance (HOMA) = BW vs. Low fibre diet |
| Andersson, 2007 [49] | RCT | 30 M/F 59 years 28.3 kg/m2 Healthy | Whole-grain products (fibre 18 g/day) vs. refined-grain products (fibre 6 g/day) | 6 | = Insulin sensitivity (euglycemic hyperinsulinemic clamp tests) ↑ BW vs. refined-grain products |
| Katcher, 2008 [50] | RCT | 47 M/F 46 years 36 kg/m2 Metabolic syndrome | Whole-grain products (fibre 12.9 g/1000 kcal) vs. refined-grain products (fibre 9.7 g/1000 kcal) | 12 | = Insulin sensitivity (ISI index during OGTT) ↓BW vs. refined-grain products |
| Giacco, 2010 [51] | RCT | 15 M/F 55 years 27 kg/m2 Healthy | Whole-grain products (fibre 32 g/day) vs. refined-grain products (fibre 20 g/day) | 3 | = Insulin resistance (HOMA) = BW vs. refined-grain products |
| Brownlee, 2010 [52] | RCT | 216 M/F 46 years 30 kg/m2 Healthy | Whole-grain products (60 g/day) vs. Whole-grain products (120 g/day) vs. refined-grain products | 16 | = Insulin sensitivity (QUICKI) = BW vs. refined-grain products |
| Giacco, 2013 [53] | RCT | 133 M/F 40–65 years 31.4 kg/m2 Metabolic syndrome | Whole-grain products (fibre 33 g/day) vs. refined-grain products (fibre 20 g/day) | 12 | = Insulin sensitivity (FSIGT) = BW vs. refined-grain products |
| Giacco, 2014 [54] | RCT | 54 M/F 40–65 years 31.7 kg/m2 Metabolic syndrome | Whole-grain products (fibre 33 g/day) vs. refined-grain products (fibre 20 g/day) | 12 | = Insulin resistance (HOMA) = BW vs. refined-grain products |
| Fibre from other sources | |||||
| He, 2016 [55] | Meta-analysis of 18 RCTs | 298 M/F 53 years 26 kg/m2 Any | Oat-based products (20–136 g/day) vs. β-glucan extract (3–10 g/day) vs. refined-grain products | 4-12 | = Insulin resistance (HOMA) = BW vs. refined-grain products |
| Hashizume, 2012 [56] | RCT | 30 M/F 60.6 years 72.5 kg/m2 Metabolic syndrome | Resistant maltodextrin (27 g/day) vs. placebo | 12 | ↓ Insulin resistance (HOMA): −0.5% = BW vs. placebo |
| Li, 2010 [57] | RCT | 120M 31 years 24.5 kg/m2 Healthy | NUTRIOSE * (27 g/day) vs. placebo | 12 | ↓ Insulin resistance (HOMA): −12% ↓ BW: −1.5 kg |
| Johnston, 2010 [58] | RCT | 20 M/F 47.6 years 30.8 kg/m2 Metabolic syndrome | Resistant starch (40 g/day) vs. placebo | 12 | ↑ Insulin sensitivity (euglycemic hyperinsulinemic clamp tests tests): +0.9 mg·kg−1·min−1 per pmol/L = BW vs. placebo |
| Robertson, 2012 [59] | RCT | 15 M/F 48.9 years 33.8 kg/m2 Metabolic syndrome | Resistant starch (40 g/day) vs. placebo | 8 | ↓ Insulin resistance (HOMA): −0.4% = BW vs. placebo |
| Author, Year [Reference] | Study Design | Study Population Participants Age BMI Health Status | Intervention and Doses | Duration Weeks | Observed Effects |
|---|---|---|---|---|---|
| Post, 2002 [79] | Meta-analysis of 15 RCTs | 400 M/F 52–69 years 23.4–32.5 kg/m2 Type 2 diabetes | High fibre diet vs. low-fibre diet (4–40 g/day) | 3–12 | ↓ Fasting glucose:−15 mg/dL ↓ HbA1c: −0.26% vs. low-fibre diet (4–40 g/day) |
| Silva, 2013 [80] | Meta-analysis of 13 RCTs | 605 M/F 62 years n.a. Type 2 diabetes | High fibre foods vs. low-fibre foods (3–22.5 g/day) | 8–24 | ↓ Fasting glucose:−9.97 mg/dL ↓ HbA1c: −0.55% vs. low-fibre foods |
| Gibb, 2015 [81] | Meta-analysis of 35 RCTs | 1075 M/F 52.3 years n.a. Type 2 diabetes | Psyllium (3–10 g/day) vs. placebo | 2–26 | ↓ Fasting glucose: −37 mg/dL ↓ HbA1c: −0.97% vs. placebo |
| Schwingshackl, 2018 [82] | Meta-analysis of 56 RCTs | 4937 M/F 44–67 years 25–43 kg/m2 Type 2 diabetes | Mediterranean diet vs. control diet | 3–48 | ↓ Fasting glucose: −11.0 mg/dL ↓ HbA1c: −0.32% vs. control diet |
| Marventano, 2017 [83] | Meta-analysis of 14 RCTs | 377 M/F 50 years 28 kg/m2 Healthy | Whole-grain products vs. refined-grain products | 2–16 | = Fasting glucose = Fasting insulin vs. refined-grain products |
| Thompson, 2017 [31] | Meta-analysis of 12 RCTs | 200 M/F 20–70 years 25–45 kg/m2 Healthy | Soluble fibre supplementation (3–34 g/day) vs. Non-fibre placebo | 2–17 | ↓ Fasting glucose: −3.0 mg/dL ↓ Fasting insulin: −2.29 μU/mL ↓ BW: −2.52 kg vs. Non-fibre placebo |
| Author, Year [Reference] | Study Design | Study Population Participants Age BMI Health Status | Intervention and Doses | Duration Weeks | Observed Effects |
|---|---|---|---|---|---|
| Fibre from whole grain | |||||
| Ye, 2012 [89] | Meta-analysis of 21 RCTs | 1281 M/F 20–74 years n.a. Healthy/Hypertension | Whole-grain diet vs. control diet | 4–16 | ↓ TC: −32 mg/dL ↓ LDL-C: −28 mg/dL = BW vs. control |
| Hollander, 2015 [90] | Meta-analysis of 24 RCTs | 2275 M/F 18–75 years ≥18 kg/m2 Dyslipidemia | Whole-grain products (fibre 20 g/day) vs. refined-grain products (fibre 14 g/day) | 2–16 | ↓ TC: −5.0 mg/dL ↓ LDL-C: −3.0 mg/dL No effect on HDL-C and TG = BW vs. refined products |
| Kelly, 2017 [92] | Meta-analysis of 9 RCTs | 1414 M/F 24–70 years n.a. Any | Whole-grain products (fibre 21 g/day) vs. control products (fibre 13 g/day) | 12–16 | No effect on TC and LDL-C = BW vs. control products |
| Giacco, 2014 [54] | RCT | 54 M/F 57 ± 8 years 32 ± 5kg/m2 Metabolic syndrome | Whole-grain products (fibre 40 g/day) vs. refined-grain products (fibre 22 g/day) | 12 | Postprandial TG (IAUC) −43% = BW vs. refined products |
| Fibre from other sources | |||||
| Hartley, 2016 [91] | Meta-analysis of 23 RCTs | 1513 M/F ≥18 years n.a. High CV risk | Fibre supplementation (1.2–27.5 g/day) vs. control diet | 12 | ↓ TC: −8.0 mg/dL ↓ LDL-C: −5.0 mg/dL No effect on TG = BW vs. control |
| Whitehead, 2014 [93] | Meta-analysis of 28 RCTs | 1914 M/F 25–63 years Any | Oat β-glucan supplementation (≥3 g/day) vs. refined products | 2–12 | ↓ TC: −12 mg/dL ↓ LDL-C: −10 mg/dL vs. refined products |
| Zhu, 2015 [94] | Meta-analysis of 17 RCTs | 916 M/F 54 years 27 kg/m2 Hypercholesterolemia | Oat/Barley β-glucan-rich diet (5 g/day) vs. control diet | 7 | ↓ TC: −10 mg/dL ↓ LDL-C: −8.0 mg/dL No effect on HDL-C and TG vs. control |
| Ho, 2016 [95] | Meta-analysis of 14 RCTs | 723 M/F 47 years 26.1 kg/m2 Any | Barley β-glucan-rich diet (6 g/day) vs. control diet | 4 | ↓ LDL-C: −10 mg/dL vs. control |
| Ho, 2016 [96] | Meta-analysis of 56 RCTs | 3745 50 years 27 kg/m2 Any | Oat β-glucan-rich diet (4 g/day) vs. control diet | 6 | ↓ LDL-C: −7.0 mg/dL vs. control |
| Bazzano, 2011 [97] | Meta-analysis of 10 RCTs | 268 M/F 18–66 years n.a. Dyslipidemia | Non-Soy Legume diet (80–440 g/day; fibre 23 g/day) vs. control diet (fibre 18 g/day) | 3–8 | ↓ TC: −11.8 mg/dL ↓ LDL-C: −8.0 mg/dL No effect on HDL-C and TG = BW vs. control |
| Ha, 2014 [99] | Meta-analysis of 26 RCTs | 1037 M/F 29–64 years ≥18 kg/m2 Any | Legume-rich diet (130 g/day; fibre 26 g/day) vs. control diet (fibre 20 g/day) | 3–48 | ↓ LDL-C: −7.0 mg/dL No effect on HDL-C = BW vs. control |
| Liu, 2017 [101] | Meta-analysis of 20 RCTs | 607 M/F 18–67years 19–39 kg/m2 Any | Inulin-type fructans supplementation (7.4–30 g/day) vs. control diet | 2.5–24 | ↓ LDL-C: −6.0 mg/dL = BW vs. control |
| De Natale, 2009 [102] | RCT | 18 M/F 59 ± 5 years 27 ± 3 kg/m2 Type 2 diabetes | High-Carbohydrate/High-Fibre diet (fibre 28 g/1000 kcal) vs. High–MUFA/Low-Carbohydrate diet (fibre 8 g/1000 kcal) | 4 | Postprandial TG (IAUC) −31% = BW vs. High–MUFA/Low-Carbohydrate diet |
| Author, Year [Reference] | Study Design | Study Population Participants Age BMI Health Status | Intervention and Doses | Duration Weeks | Observed Effects |
|---|---|---|---|---|---|
| Streppel, 2005 [115] | Meta-analysis of 24 RCTs | 1404 M/F 23–63 years n.a. normotensive and hypertensive | Soluble/insoluble fibre supplementation (mean dose: 11.5 g/day) vs. placebo | 2–24 | ↓ SBP: −1.13 mm Hg ↓ DBP: −1.26 mmHg = BW vs. placebo |
| Hartley, 2016 [91] | Meta-analysis of 23 RCTs | 1513 M/F ≥18 years n.a. any | Soluble/insoluble fibre supplementation (1.2–27.5 g/day) vs. control diet | 12 | ↓ DBP: −1.77 mmHg = BW vs. control diet |
| Whelton, 2005 [116] | Meta-analysis of 25 RCTs | 1477 M/F 16–85 years n.a. normotensive and hypertensive | Fruit/vegetables/cereals/pectins/ guar gum rich diets or supplementation (10.7 g/day) * vs. control diet/placebo | 2–26 | ↓ DBP: −1.65 mm Hg In hypertensive subjects: ↓ SBP: −5.95 mm Hg ↓ DBP: −4.20 mmHg ↓ BW in n.9 RCTs vs. control diet/placebo |
| Evans, 2015 [117] | Meta-analysis of 28 RCTs | 1333 M/F 29–60 years n.a. healthy | Whole oats, oat bran-supplemented foods or oat-based breakfast cereals (mean dose: 4 g/day) vs. wheat-based foods | 6–14 | ↓ SBP: −2.7 mm Hg ↓ DBP: −1.5 mmHg = BW vs. wheat-based foods |
| Khan, 2018 [118] | Meta-analysis of 22 RCTs | 1430 M/F 15–69 years n.a. any | Viscous fibre supplementation (b-glucan from oats and barley, guar gum, konjac, pectin and psyllium supplementation) (fibre 8.7 g/day) vs. control products | 4–24 | ↓ SBP: −1.59 mm Hg ↓ DBP: −0.39 mmHg Psyllium fibre supplementation: ↓ SBP: −2.39 mm Hg = BW vs. control products |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bozzetto, L.; Costabile, G.; Della Pepa, G.; Ciciola, P.; Vetrani, C.; Vitale, M.; Rivellese, A.A.; Annuzzi, G. Dietary Fibre as a Unifying Remedy for the Whole Spectrum of Obesity-Associated Cardiovascular Risk. Nutrients 2018, 10, 943. https://doi.org/10.3390/nu10070943
Bozzetto L, Costabile G, Della Pepa G, Ciciola P, Vetrani C, Vitale M, Rivellese AA, Annuzzi G. Dietary Fibre as a Unifying Remedy for the Whole Spectrum of Obesity-Associated Cardiovascular Risk. Nutrients. 2018; 10(7):943. https://doi.org/10.3390/nu10070943
Chicago/Turabian StyleBozzetto, Lutgarda, Giuseppina Costabile, Giuseppe Della Pepa, Paola Ciciola, Claudia Vetrani, Marilena Vitale, Angela A. Rivellese, and Giovanni Annuzzi. 2018. "Dietary Fibre as a Unifying Remedy for the Whole Spectrum of Obesity-Associated Cardiovascular Risk" Nutrients 10, no. 7: 943. https://doi.org/10.3390/nu10070943
APA StyleBozzetto, L., Costabile, G., Della Pepa, G., Ciciola, P., Vetrani, C., Vitale, M., Rivellese, A. A., & Annuzzi, G. (2018). Dietary Fibre as a Unifying Remedy for the Whole Spectrum of Obesity-Associated Cardiovascular Risk. Nutrients, 10(7), 943. https://doi.org/10.3390/nu10070943






