Virus-Like Particle Vaccination Protects Nonhuman Primates from Lethal Aerosol Exposure with Marburgvirus (VLP Vaccination Protects Macaques against Aerosol Challenges)
Abstract
:1. Introduction
2. Materials and Methods
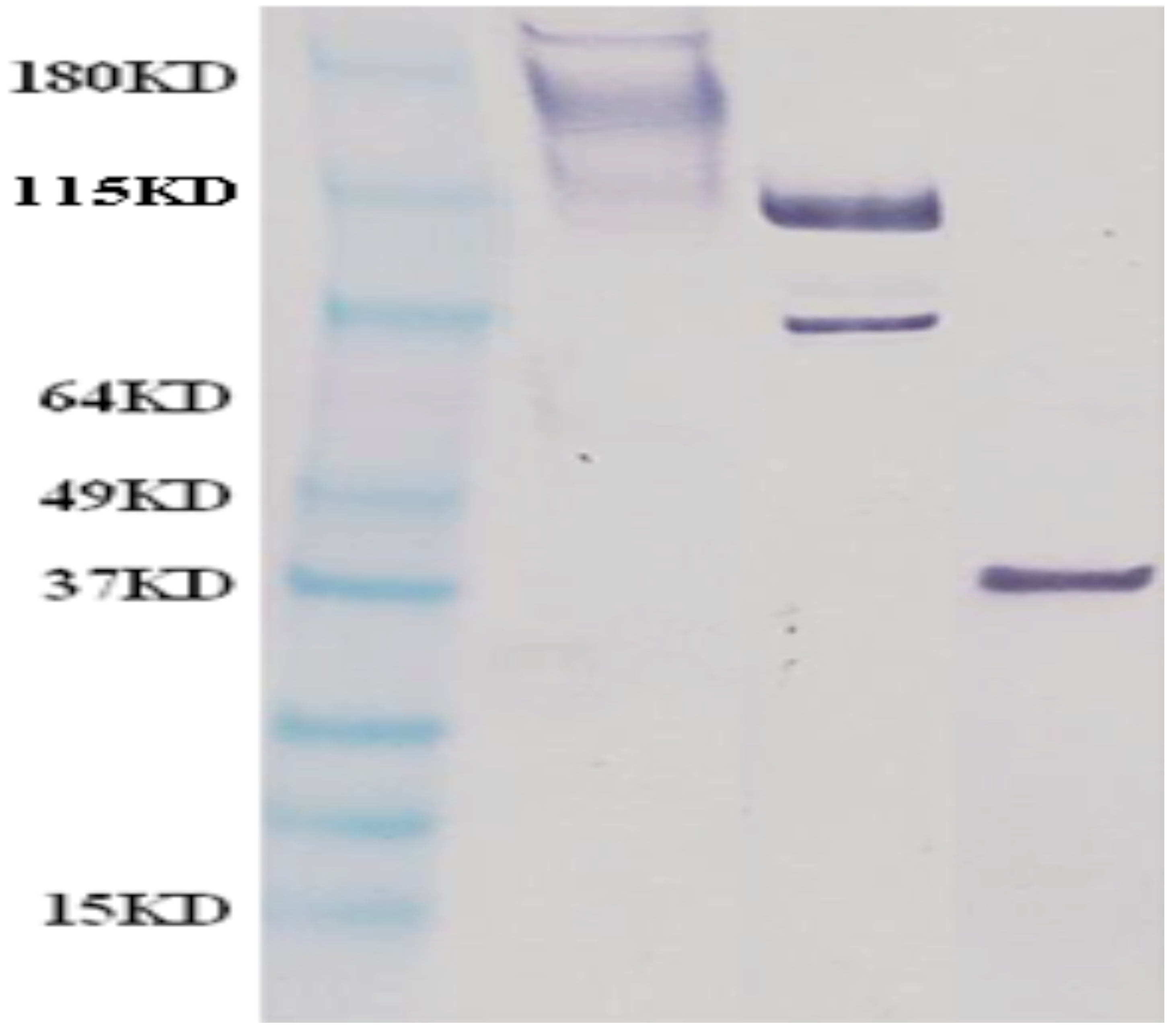
2.1. MARV VLP Production
2.2. Animal Care and Use
2.3. VLP Vaccination
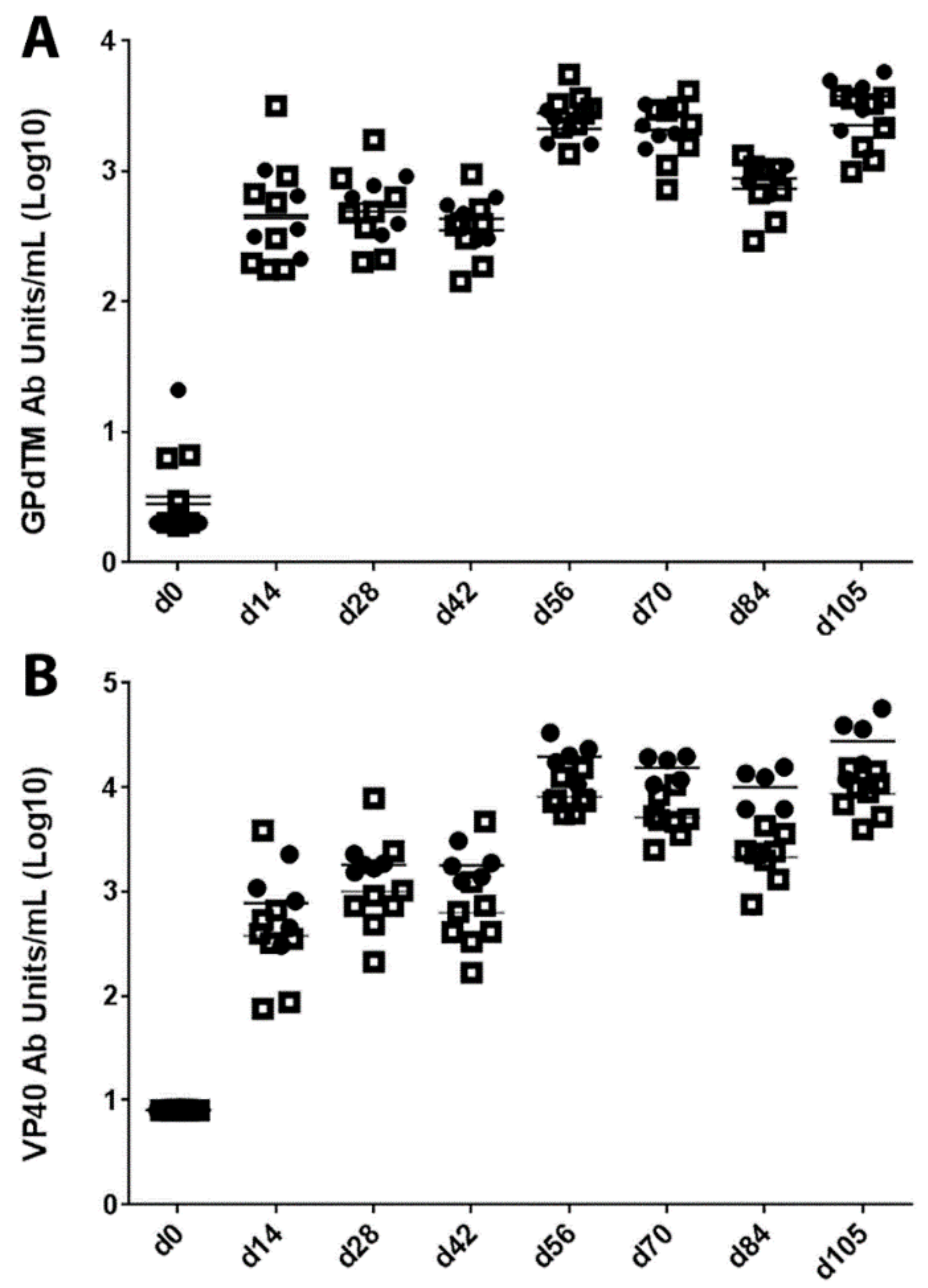
2.4. Determination of IgG Antibody Titers against GP and VP40
2.5. Virus Challenge Procedures
2.6. Post-Challenge Sample Analytics
3. Results
3.1. Antibody Responses in Vaccinated Macaques
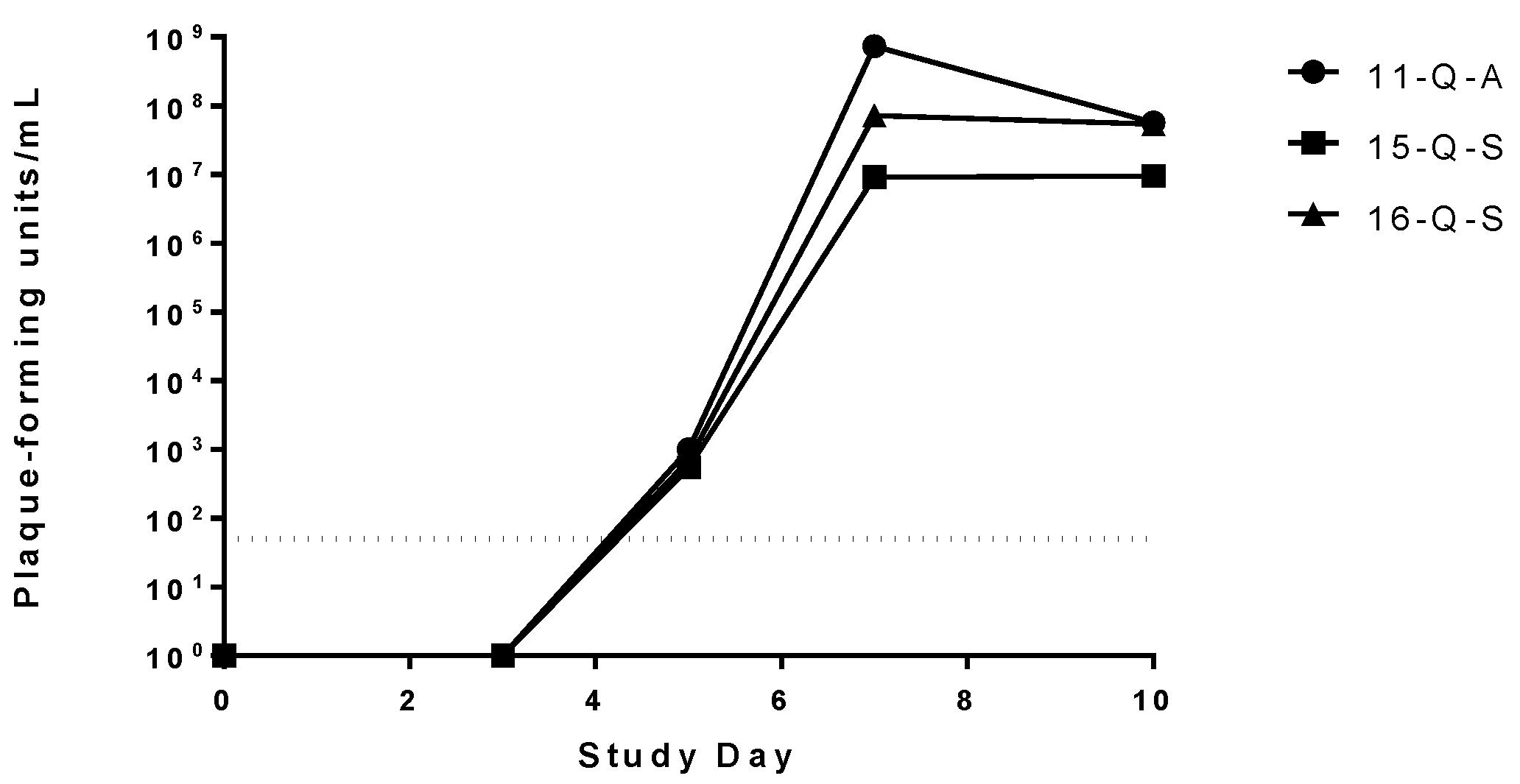
3.2. Quantitation of Virus Inocula
3.3. Post-Challenge Observations
3.3.1. Behavioral and Other Visible Clinical Signs
3.3.2. Temperatures
3.3.3. Hematological and Clinical Chemistry Parameters
3.3.4. Viremia
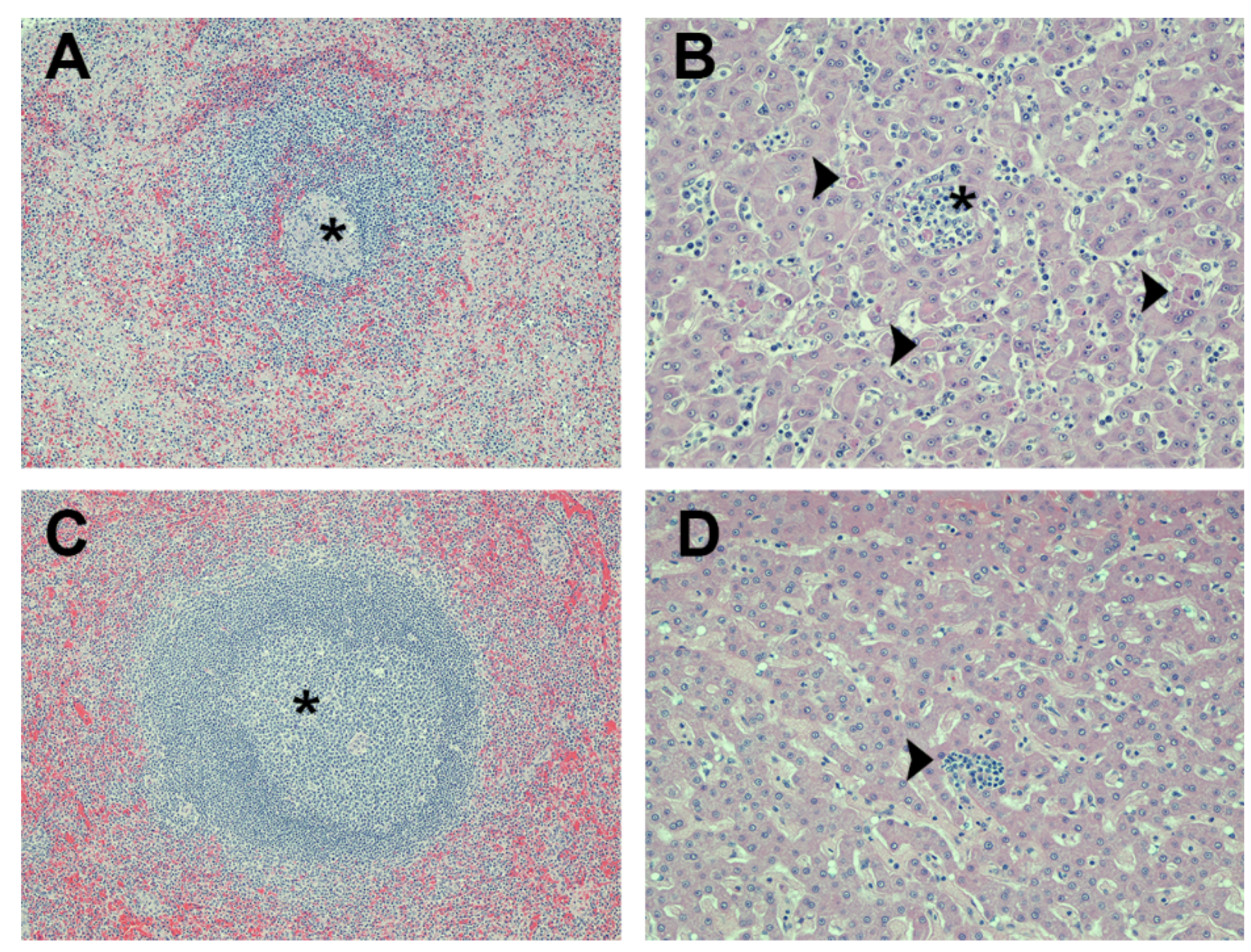
3.3.5. Necropsy Findings
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Brauburger, K.; Hume, A.J.; Muhlberger, E.; Olejnik, J. Forty-five years of marburg virus research. Viruses 2012, 4, 1878–1927. [Google Scholar] [CrossRef] [PubMed]
- Martini, G.A.; Siegert, R. Marburg Virus Disease; Springer-Verlag: Berlin, Germany, 1971. [Google Scholar]
- Smith, D.H.; Johnson, B.K.; Isaacson, M.; Swanapoel, R.; Johnson, K.M.; Killey, M.; Bagshawe, A.; Siongok, T.; Keruga, W.K. Marburg-virus disease in Kenya. Lancet 1982, 1, 816–820. [Google Scholar] [CrossRef]
- Kuhn, J.H.; Becker, S.; Ebihara, H.; Geisbert, T.W.; Johnson, K.M.; Kawaoka, Y.; Lipkin, W.I.; Negredo, A.I.; Netesov, S.V.; Nichol, S.T.; et al. Proposal for a revised taxonomy of the family filoviridae: Classification, names of taxa and viruses, and virus abbreviations. Arch. Virol. 2010, 155, 2083–2103. [Google Scholar] [CrossRef] [PubMed]
- Zeller, H. Lessons from the marburg virus epidemic in Durba, Democratic Republic of the Congo (1998–2000). Med. Trop. (Mars) 2000, 60, 23–26. [Google Scholar] [PubMed]
- Colebunders, R.; Sleurs, H.; Pirard, P.; Borchert, M.; Libande, M.; Mustin, J.P.; Tshomba, A.; Kinuani, L.; Olinda, L.A.; Tshioko, F.; et al. Organisation of health care during an outbreak of Marburg haemorrhagic fever in the Democratic Republic of Congo, 1999. J. Infect. 2004, 48, 347–353. [Google Scholar] [CrossRef] [Green Version]
- Towner, J.S.; Khristova, M.L.; Sealy, T.K.; Vincent, M.J.; Erickson, B.R.; Bawiec, D.A.; Hartman, A.L.; Comer, J.A.; Zaki, S.R.; Stroher, U.; et al. Marburgvirus genomics and association with a large hemorrhagic fever outbreak in Angola. J. Virol. 2006, 80, 6497–6516. [Google Scholar] [CrossRef] [PubMed]
- Mbonye, A.; Wamala, J.; Winyi, K.; Tugumizemo, V.; Aceng, J.; Makumbi, I. Repeated outbreaks of viral hemorrhagic fevers in Uganda. Afr. health sci. 2012, 12, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, T.W.; Bausch, D.G.; Feldmann, H. Prospects for immunisation against Marburg and Ebola viruses. Rev. Med. Virol. 2010, 20, 344–357. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Jaax, N.K.; Deal, E.M.; Swenson, D.L.; Larsen, T.; Bavari, S. Viral hemorrhagic fevers. In Biodefense: Research Methodology and Animal Models; Swearengen, J.R., Ed.; Taylor & Francis Group: Boca Raton, London, UK, 2005; pp. 227–258. [Google Scholar]
- Bradfute, S.B.; Dye, J.M., Jr.; Bavari, S. Filovirus vaccines. Hum. Vaccines 2011, 7, 701–711. [Google Scholar] [CrossRef]
- Geisbert, T.W.; Pushko, P.; Anderson, K.; Smith, J.; Davis, K.J.; Jahrling, P.B. Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg. Infect. Dis. 2002, 8, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Hevey, M.; Negley, D.; Vanderzanden, L.; Tammariello, R.F.; Geisbert, J.; Schmaljohn, C.; Smith, J.F.; Jahrling, P.B.; Schmaljohn, A. Marburg virus vaccines, comparing classical and new approaches. Vaccine 2002, 20, 586–593. [Google Scholar] [CrossRef]
- Cooper, C.L.; Bavari, S. A race for an Ebola vaccine: Promises and obstacles. Trends Microbiol. 2015, 23, 65–66. [Google Scholar] [CrossRef] [PubMed]
- Hevey, M.; Negley, D.; Pushko, P.; Smith, J.; Schmaljohn, A. Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates. Virology 1998, 251, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, N.J.; Sanchez, A.; Rollin, P.E.; Yang, Z.Y.; Nabel, G.J. Development of a preventive vaccine for Ebola virus infection in primates. Nature 2000, 408, 605–609. [Google Scholar] [PubMed]
- Herbert, A.S.; Kuehne, A.I.; Barth, J.F.; Ortiz, R.A.; Nichols, D.K.; Zak, S.E.; Stonier, S.W.; Muhammad, M.A.; Bakken, R.R.; Prugar, L.I.; et al. Venezuelan equine encephalitis virus replicon particle vaccine protects nonhuman primates from intramuscular and aerosol challenge with ebolavirus. J. Virol. 2013, 87, 4952–4964. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, T.W.; Bailey, M.; Geisbert, J.B.; Asiedu, C.; Roederer, M.; Grazia-Pau, M.; Custers, J.; Jahrling, P.; Goudsmit, J.; Koup, R.; et al. Vector choice determines immunogenicity and potency of genetic vaccines against Angola Marburg virus in nonhuman primates. J. Virol. 2010, 84, 10386–10394. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.M.; Feldmann, H.; Stroher, U.; Geisbert, J.B.; Fernando, L.; Grolla, A.; Klenk, H.D.; Sullivan, N.J.; Volchkov, V.E.; Fritz, E.A.; et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat. Med. 2005, 11, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, T.W.; Geisbert, J.B.; Leung, A.; Daddario-DiCaprio, K.M.; Hensley, L.E.; Grolla, A.; Feldmann, H. Single-injection vaccine protects nonhuman primates against infection with Marburg virus and three species of Ebola virus. J. Virol. 2009, 83, 7296–7304. [Google Scholar] [CrossRef] [PubMed]
- Bukreyev, A.; Rollin, P.E.; Tate, M.K.; Yang, L.; Zaki, S.R.; Shieh, W.J.; Murphy, B.R.; Collins, P.L.; Sanchez, A. Successful topical respiratory tract immunization of primates against Ebola virus. J. Virol. 2007, 81, 6379–6388. [Google Scholar] [CrossRef] [PubMed]
- Blaney, J.E.; Marzi, A.; Willet, M.; Papaneri, A.B.; Wirblich, C.; Feldmann, F.; Holbrook, M.; Jahrling, P.; Feldmann, H.; Schnell, M.J. Antibody quality and protection from lethal Ebola virus challenge in nonhuman primates immunized with rabies virus based bivalent vaccine. PLoS Pathog. 2013, 9, e1003389. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Swenson, D.L.; Olinger, G.G.; Kalina, W.V.; Aman, M.J.; Bavari, S. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal ebola virus challenge. J. Infect. Dis. 2007, 196 (Suppl. 2), S430–S437. [Google Scholar] [CrossRef] [PubMed]
- Swenson, D.L.; Warfield, K.L.; Larsen, T.; Alves, D.A.; Coberley, S.S.; Bavari, S. Monovalent virus-like particle vaccine protects guinea pigs and nonhuman primates against infection with multiple Marburg viruses. Expert Rev. Vaccines 2008, 7, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Buonaguro, L.; Tornesello, M.L.; Buonaguro, F.M. Virus-like particles as particulate vaccines. Curr. HIV Res. 2010, 8, 299–309. [Google Scholar] [CrossRef]
- Noad, R.; Roy, P. Virus-like particles as immunogens. Trends Microbiol. 2003, 11, 438–444. [Google Scholar] [CrossRef]
- Naslund, J.; Lagerqvist, N.; Habjan, M.; Lundkvist, A.; Evander, M.; Ahlm, C.; Weber, F.; Bucht, G. Vaccination with virus-like particles protects mice from lethal infection of rift valley fever virus. Virology 2009, 385, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Conner, M.E.; Zarley, C.D.; Hu, B.; Parsons, S.; Drabinski, D.; Greiner, S.; Smith, R.; Jiang, B.; Corsaro, B.; Barniak, V.; et al. Virus-like particles as a rotavirus subunit vaccine. J. Infect Dis. 1996, 174 (Suppl. 1), S88–S92. [Google Scholar] [CrossRef] [PubMed]
- Tacket, C.O.; Sztein, M.B.; Losonsky, G.A.; Wasserman, S.S.; Estes, M.K. Humoral, mucosal, and cellular immune responses to oral norwalk virus-like particles in volunteers. Clin. Immunol. 2003, 108, 241–247. [Google Scholar] [CrossRef]
- Roldao, A.; Mellado, M.C.; Castilho, L.R.; Carrondo, M.J.; Alves, P.M. Virus-like particles in vaccine development. Expert Rev. Vaccines 2010, 9, 1149–1176. [Google Scholar] [CrossRef] [PubMed]
- Bavari, S.; Bosio, C.M.; Wiegand, E.; Ruthel, G.; Will, A.B.; Geisbert, T.W.; Hevey, M.; Schmaljohn, C.; Schmaljohn, A.; Aman, M.J. Lipid raft microdomains: A gateway for compartmentalized trafficking of Ebola and Marburg viruses. J. Exp. Med. 2002, 195, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Swenson, D.L.; Warfield, K.L.; Negley, D.L.; Schmaljohn, A.; Aman, M.J.; Bavari, S. Virus-like particles exhibit potential as a pan-filovirus vaccine for both ebola and Marburg viral infections. Vaccine 2005, 23, 3033–3042. [Google Scholar] [CrossRef] [PubMed]
- Noda, T.; Watanabe, S.; Sagara, H.; Kawaoka, Y. Mapping of the VP40-binding regions of the nucleoprotein of Ebola virus. J. Virol. 2007, 81, 3554–3562. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.A.; Hart, M.K. Protection from ebola virus mediated by cytotoxic t lymphocytes specific for the viral nucleoprotein. J. Virol. 2001, 75, 2660–2664. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Dye, J.M.; Wells, J.B.; Unfer, R.C.; Holtsberg, F.W.; Shulenin, S.; Vu, H.; Swenson, D.L.; Bavari, S.; Aman, M.J. Homologous and heterologous protection of nonhuman primates by Zaire and Sudan ebolavirus virus-like particles. PLoS ONE 2014, 10, e0118881. [Google Scholar]
- Jaax, N.K.; Davis, K.J.; Geisbert, T.J.; Vogel, P.; Jaax, G.P.; Topper, M.; Jahrling, P.B. Lethal experimental infection of rhesus monkeys with ebola-Zaire (mayinga) virus by the oral and conjunctival route of exposure. Arch. Pathol. Lab. Med. 1996, 120, 140–155. [Google Scholar] [PubMed]
- Leffel, E.K.; Reed, D.S. Marburg and Ebola viruses as aerosol threats. Biosecur. Bioterror. 2004, 2, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Swenson, D.L.; Negley, D.L.; Schmaljohn, A.L.; Aman, M.J.; Bavari, S. Marburg virus-like particles protect guinea pigs from lethal marburg virus infection. Vaccine 2004, 22, 3495–3502. [Google Scholar] [CrossRef] [PubMed]
- Swenson, D.L.; Warfield, K.L.; Kuehl, K.; Larsen, T.; Hevey, M.C.; Schmaljohn, A.; Bavari, S.; Aman, M.J. Generation of Marburg virus-like particles by co-expression of glycoprotein and matrix protein. FEMS Immunol. Med. Microbiol. 2004, 40, 27–31. [Google Scholar] [CrossRef]
- Warfield, K.L.; Bosio, C.M.; Welcher, B.C.; Deal, E.M.; Mohamadzadeh, M.; Schmaljohn, A.; Aman, M.J.; Bavari, S. Ebola virus-like particles protect from lethal Ebola virus infection. Proc. Natl. Acad. Sci. 2003, 100, 15889–15894. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Posten, N.A.; Swenson, D.L.; Olinger, G.G.; Esposito, D.; Gillette, W.K.; Hopkins, R.F.; Costantino, J.; Panchal, R.G.; Hartley, J.L.; et al. Filovirus-like particles produced in insect cells: Immunogenicity and protection in rodents. J. Infect. Dis. 2007, 196 (Suppl. 2), S421–S429. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Fusco, M.L.; Hessell, A.J.; Oswald, W.B.; Burton, D.R.; Saphire, E.O. Structure of the ebola virus glycoprotein bound to an antibody from a human survivor. Nature 2008, 454, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Moe, J.B.; Lambert, R.D.; Lupton, H.W. Plaque assay for Ebola virus. J. Clin. Microbiol. 1981, 13, 791–793. [Google Scholar] [PubMed]
- Pratt, W.D.; Wang, D.; Nichols, D.K.; Luo, M.; Woraratanadharm, J.; Dye, J.M.; Holman, D.H.; Dong, J.Y. Protection of nonhuman primates against two species of Ebola virus infection with a single complex adenovirus vector. Clin. Vaccine Immunol. 2010, 17, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, T.W.; Daddario-Dicaprio, K.M.; Geisbert, J.B.; Reed, D.S.; Feldmann, F.; Grolla, A.; Stroher, U.; Fritz, E.A.; Hensley, L.E.; Jones, S.M.; et al. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 2008, 26, 6894–6900. [Google Scholar] [CrossRef] [PubMed]
- Hartings, J.M.; Roy, C.J. The automated bioaerosol exposure system: Preclinical platform development and a respiratory dosimetry application with nonhuman primates. J. Pharmacol. Toxicol. Methods 2004, 49, 39–55. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.J.; Pitt, L.M. Infectious disease aerobiology: Aerosol challenge methods. In Biodefense: Research Methodology and Animal Models; Swearengen, J.R., Ed.; Taylor & Francis Group: Boca Raton, London, UK, 2006; pp. 61–76. [Google Scholar]
- Stahl-Hennig, C.; Eisenblatter, M.; Jasny, E.; Rzehak, T.; Tenner-Racz, K.; Trumpfheller, C.; Salazar, A.M.; Uberla, K.; Nieto, K.; Kleinschmidt, J.; et al. Synthetic double-stranded rnas are adjuvants for the induction of t helper 1 and humoral immune responses to human Papillomavirus in rhesus macaques. PLoS Pathog. 2009, 5, e1000373. [Google Scholar] [CrossRef] [PubMed]
- Longhi, M.P.; Trumpfheller, C.; Idoyaga, J.; Caskey, M.; Matos, I.; Kluger, C.; Salazar, A.M.; Colonna, M.; Steinman, R.M. Dendritic cells require a systemic type I interferon response to mature and induce CD4+ TH1 immunity with poly ic as adjuvant. J. Exp. Med. 2009, 206, 1589–1602. [Google Scholar] [CrossRef] [PubMed]
- Martins, K.A.; Steffens, J.T.; van Tongeren, S.A.; Wells, J.B.; Bergeron, A.A.; Dickson, S.P.; Dye, J.M.; Salazar, A.M.; Bavari, S. Toll-like receptor agonist augments virus-like particle-mediated protection from Ebola virus with transient immune activation. PLoS ONE 2014, 9, e89735. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.H.; Dodd, L.E.; Wahl-Jensen, V.; Radoshitzky, S.R.; Bavari, S.; Jahrling, P.B. Evaluation of perceived threat differences posed by filovirus variants. Biosecur. Bioterror. 2011, 9, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J. Largest-ever Ebola outbreak still simmering in West Africa. JAMA 2014, 312, 476. [Google Scholar] [CrossRef] [PubMed]
- Gire, S.K.; Goba, A.; Andersen, K.G.; Sealfon, R.S.; Park, D.J.; Kanneh, L.; Jalloh, S.; Momoh, M.; Fullah, M.; Dudas, G.; et al. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science 2014, 345, 1369–1372. [Google Scholar] [CrossRef] [PubMed]
| Group Description | ID | Challenge Route | Challenge Dose (pfu) | Day Post Challenge | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 and 3 | 5 | 7 | 10 | 14 | 21 | 28 | |||||
| Group 1: mVLP + Poly-IC adjuvant | 1-MP-A | Aerosol | 40 | N.S. | N.S. | N.S. | N.S | N.S. | N.S. | N.S. | Survived |
| 2-MP-A | 105 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | Survived | ||
| 3-MP-A | 122 | N.S. | ↑ALT | ↑ALT | Fever | N.S. | N.S. | N.S. | Survived | ||
| 4-MP-A | 113 | N.S. | N.S. | ↓Plt | N.S. | N.S. | N.S. | N.S. | Survived | ||
| 5-MP-A | 113 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | Survived | ||
| Group 2: mVLP + QS-21 adjuvant | 6-MQ-A | Aerosol | 135 | N.S. | N.S. | N.S. | N.S. | ↑↑ALP | ↑ALP | N.S. | Survived |
| 7-MQ-A | 113 | N.S. | N.S. | N.S. | Fever | Fever | Fever | N.S. | Survived | ||
| 8-MQ-A | 83 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S | N.S. | Survived | ||
| 9-MQ-A | 93 | 9.5% weight loss (day 3) | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | Survived | ||
| 10-MQ-A | 117 | N.S. | N.S. | N.S. | ↑WBC, ↓Plt | N.S. | N.S. | N.S. | Survived | ||
| Group 3: QS-21 only | 11-Q-A | Aerosol | 113 | N.S. | N.S. | ↑↑ALP, ↑ALT, ↑↑↑AST | Severely depressed, severe rash, no food, ↑↑WBC, ↑↑↑BUN, ↑↑↑ALP, ↑↑↑ALT, ↑↑↑AST, ↑↑CRE, ↓GLU | Euthanized day 122 | |||
| Group 4: mVLP + QS-21 adjuvant | 12-MQ-S | SQ | 315 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | Survived |
| 13-MQ-S | 315 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | Survived | ||
| 14-MQ-S | 315 | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | N.S. | Survived | ||
| Group 5: QS-21 only | 15-Q-S | SQ | 315 | N.S. | N.S. | ↑ALP, ↑ALT, ↑↑↑AST, ↑↑CRE, ↓GLU | Severely depressed, severe rash, no food, ↑WBC, ↑↑BUN, ↑↑↑ALP, ↑↑↑ALT, ↑↑↑AST, ↑↑↑CRE, ↓↓↓GLU | Euthanized day 122 | |||
| Group 6: Poly-IC only | 16-P-S | SQ | 315 | N.S. | N.S. | ↑ALT, ↑↑↑AST | Severely depressed, moderate rash, no food, ↑WBC, ↑BUN, ↑↑↑ALP, ↑↑↑ALT, ↑↑↑AST, ↑↑↑CRE, ↓↓↓GLU, Temp Drop | Euthanized day 122 | |||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dye, J.M.; Warfield, K.L.; Wells, J.B.; Unfer, R.C.; Shulenin, S.; Vu, H.; Nichols, D.K.; Aman, M.J.; Bavari, S. Virus-Like Particle Vaccination Protects Nonhuman Primates from Lethal Aerosol Exposure with Marburgvirus (VLP Vaccination Protects Macaques against Aerosol Challenges). Viruses 2016, 8, 94. https://doi.org/10.3390/v8040094
Dye JM, Warfield KL, Wells JB, Unfer RC, Shulenin S, Vu H, Nichols DK, Aman MJ, Bavari S. Virus-Like Particle Vaccination Protects Nonhuman Primates from Lethal Aerosol Exposure with Marburgvirus (VLP Vaccination Protects Macaques against Aerosol Challenges). Viruses. 2016; 8(4):94. https://doi.org/10.3390/v8040094
Chicago/Turabian StyleDye, John M., Kelly L. Warfield, Jay B. Wells, Robert C. Unfer, Sergey Shulenin, Hong Vu, Donald K. Nichols, M. Javad Aman, and Sina Bavari. 2016. "Virus-Like Particle Vaccination Protects Nonhuman Primates from Lethal Aerosol Exposure with Marburgvirus (VLP Vaccination Protects Macaques against Aerosol Challenges)" Viruses 8, no. 4: 94. https://doi.org/10.3390/v8040094
APA StyleDye, J. M., Warfield, K. L., Wells, J. B., Unfer, R. C., Shulenin, S., Vu, H., Nichols, D. K., Aman, M. J., & Bavari, S. (2016). Virus-Like Particle Vaccination Protects Nonhuman Primates from Lethal Aerosol Exposure with Marburgvirus (VLP Vaccination Protects Macaques against Aerosol Challenges). Viruses, 8(4), 94. https://doi.org/10.3390/v8040094





