Prediction of Unmet Primary Care Needs for the Medically Vulnerable Post-Disaster: An Interrupted Time-Series Analysis of Health System Responses
Abstract
:1. Introduction
1.1. Secondary Surge Capacity Metric
1.2. Natural Experiment
1.3. Study Objectives
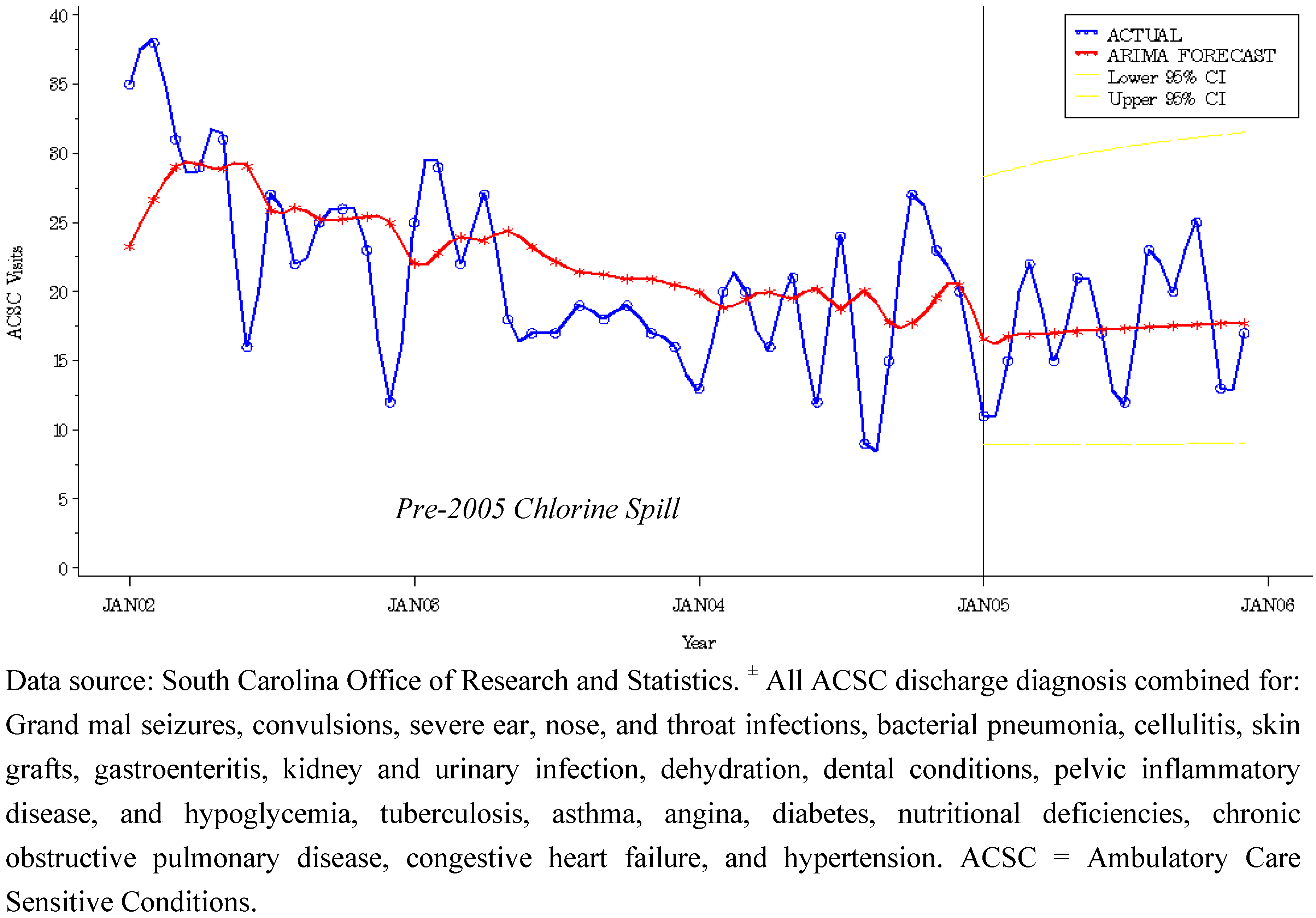
2. Methodology
2.1. ACSC Metric for Unmet Primary Care Need
2.2. Setting
2.3. Study Design and Methods
3. Results
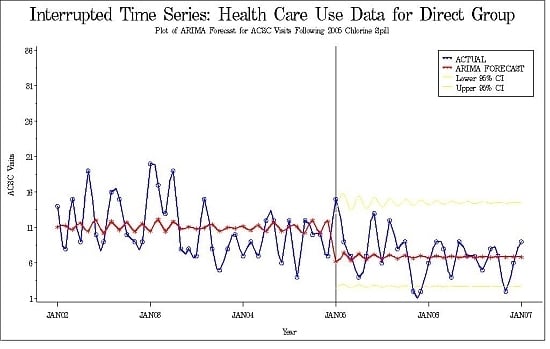
3.1. Intervention Model for Health Care Use Post-Chlorine Spill
| Study Group | Pre-Disaster | Post-Disaster | ||
|---|---|---|---|---|
| N (months) | Mean * (SD) | N (months) | Mean* (SD) | |
| Direct | 36 | 10.8 (4.4) | 24 | 7.0 (3.2) |
| Indirect | 36 | 30.0 (6.8) | 12 | 28.0 (6.1) |
| Parameter | Estimate | Std Error | T | P-value |
|---|---|---|---|---|
| MU | 2.3108 | 0.0780 | 29.48 | <0.0001 |
| MA 1,1 | −0.9642 | 0.1216 | −7.93 | <0.0001 |
| AR 1,1 | −0.8938 | 0.1641 | −5.45 | <0.0001 |
| 2005 Chlorine spill a | −0.4589 | 0.1239 | −3.70 | <0.001 |
3.2. Forecast Modeling of Unmet Primary Care Need

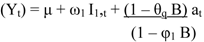
3.3. Intervention Model for Control Community
| Control Group | Estimate | Std Error | T | P-value |
|---|---|---|---|---|
| MU | 3.0945 | 0.1434 | 21.58 | <0.0001 |
| MA 1,1 | 0.7565 | 0.2066 | 3.66 | <0.001 |
| AR 1,1 | 0.9285 | 0.1109 | 8.38 | <0.0001 |
| 2005 Chlorine spill a | −0.2228 | 0.2083 | −1.07 | 0.29 |
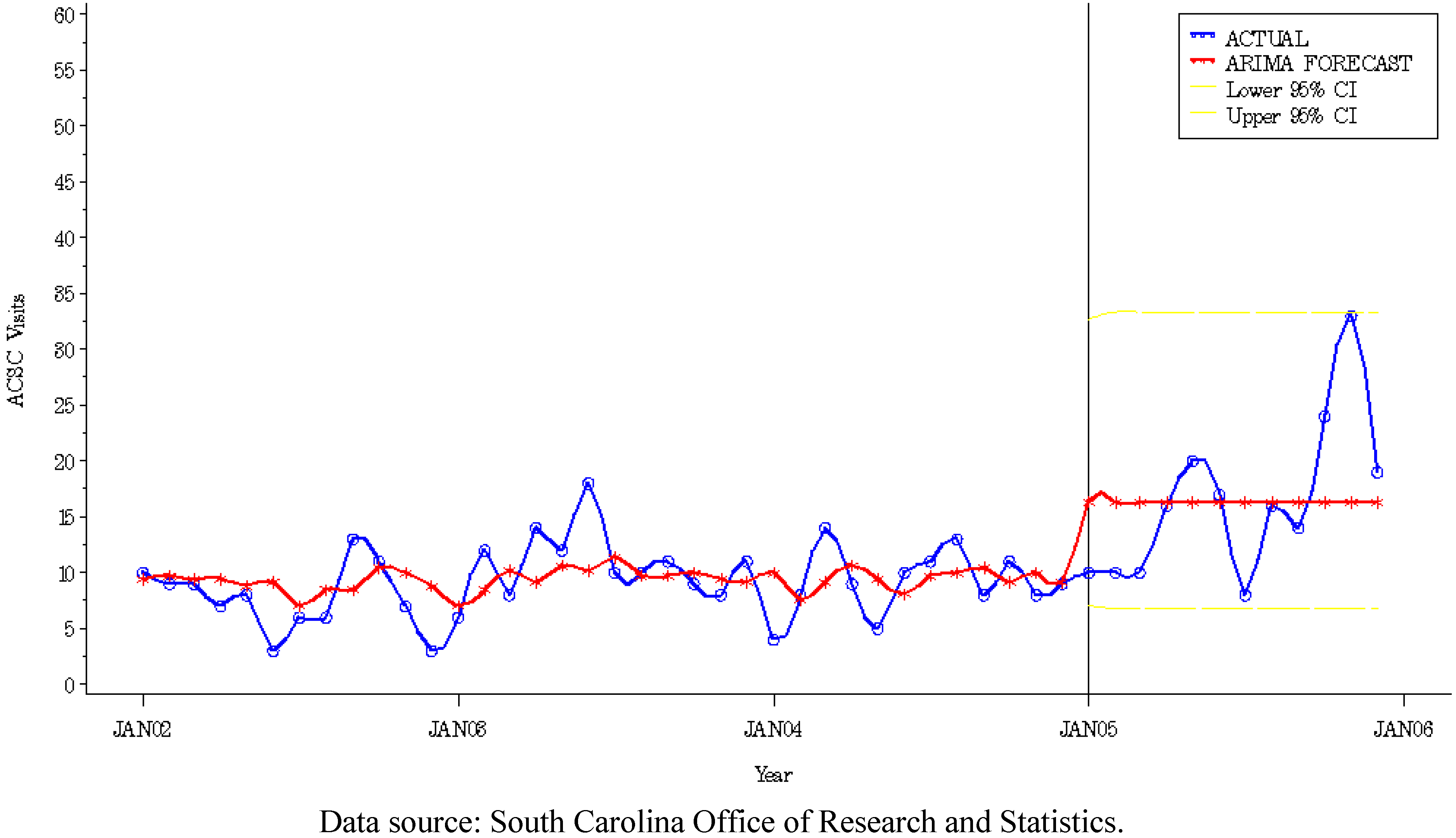
3.4. Primary Care Visits to FQHC
4. Discussion
4.1. Strength and Limitations
4.2. Directions for Future Research
5. Conclusions
Conflict of Interest
Acknowledgements
References
- Aronoff, M.; Gunter, V. Defining disaster: Local constructions for recovery in the aftermath of chemical contamination. Soc. Probl. 1992, 39, 345–365. [Google Scholar] [CrossRef]
- Baum, A.; Fleming, I. Implications of psychological research on stress and technological accidents. Am. Psychol. 1993, 48, 665–672. [Google Scholar] [CrossRef]
- Edwards, M.L.K. An interdisciplinary perspective on disasters and stress: The promise of an ecological framework. Sociol. Forum 1998, 13, 115–132. [Google Scholar] [CrossRef]
- Hospital Staffing and Surge Capacity during a Disaster Event. Available online: http://www.naph.org/Main-Menu-Category/Publications/Emergency-Preparedness/hospitalstaffingandsurgecapacityduringadisasterevent.aspx?FT=.pdf (accessed on 11 November 2011).
- DeLia, D.; Wood, E. The dwindling supply of empty beds: Implications for. hospital surge capacity. Health Affairs 2008, 27, 1688–1694. [Google Scholar] [CrossRef]
- Manley, W.G.; Furbee, P.M.; Coben, J.H.; Smyth, S.K.; Summers, D.E.; Althouse, R.C.; Kimble, R.L.; Kocsis, A.T.; Helmkamp, J.C. Realities of disaster preparedness in rural hospitals. Disaster Manage. Resp. 2006, 4, 80–87. [Google Scholar] [CrossRef]
- Altevogt, B.M.; Pope, A.M.; Hill, M.N.; Shine, K.I. Reference. In Research Priorities in Emergency Preparedness and Response for Public Health Systems: A Letter Report; The National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- Handler, J.A.; Gillam, M.; Kirsch, T.D.; Feied, C.F. Metrics in the science of surge. Acad. Emerg. Med. 2006, 13, 1173–1178. [Google Scholar] [CrossRef]
- WHO, The New Emergency Health Kit: Emergency Supplies for 10,000 Persons for 30 Days; Report Number: 10.000 (1st Edition). World Health Organization: Geneva, Switzerland, 1990.
- Chmatal, P.; Bohonek, M.; Dobiasova, M.; Hasek, R.; Cernohous, M. A humanitarian mission in southern Iraq: Utlization of the 7th Field Hospital of the Army of the Czech Republic: A report on its medical activities and working conditions. Milit. Med. 2005, 170, 473–476. [Google Scholar]
- Sharp, T.W.; Yip, R.; Malong, J.S. U.S. military forces and emergency international humanitarian assistance: Observations and recommendations from three recent missions. J. Amer. Med. Assn. 1994, 272, 386–390. [Google Scholar] [CrossRef]
- Weddle, M.; Prado-Monje, H. The use of deployable military hospitals after hurricanes: Lessons from the Hurricane Marilyn response. Milit. Med. 2000, 154, 411–417. [Google Scholar]
- D’Amore, A.R.; Hardin, C.K. Air Force expedititionary medical support unit at the Houston floods: Use of military model in civilian disaster response. Milit. Med. 2005, 170, 103–106. [Google Scholar]
- Centers for Disease Control and Prevention. Update on CDC’s Response to Hurricane Katrina. Available online: http://www.cdc.gov/od/katrina/ (accessed on 12 March 2011).
- Survey of Hurricane Katrina Evacuees. Available online: http://www.kff.org/newsmedia/7401.cfm (accessed on 21 October 2011).
- Ford, E.S.; Mokdad, A.H.; Link, M.W.; Garvin, W.S.; McGuire, L.C.; Jiles, R.B.; Balluz, L.S. Chronic disease in health emergencies: In the eye of the hurricane. Prev. Chron. Dis. Public Health Res. Pract. Policy 2006, 3, 1–7. [Google Scholar]
- Krol, D.M.; Redlener, M.; Shapiro, A.; Wajnberg, A. A mobile medical care approach targeting underserved populations in post-Hurricane Katrina Mississippi. J. Health Care Poor Underserve 2007, 18, 331–340. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Mensah, G.A.; Posner, S.F.; Reed, E.; Simoes, E.J.; Engelgau, M.M. When Chronic Conditions Become Acute: Prevention and Control of Chronic Diseases and Adverse Health Outcomes during Natural Disasters. Available online: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1459465/ (accessed on 19 December 2011).
- Axelrod, C.; Killam, P.P.; Gaston, M.H.; Stinson, N. Primary health care and the midwest flood disaster. Public Health Rep. 1994, 109, 601–605. [Google Scholar]
- Bayard, D. Haiti earthquake relief, phase two—Long-term needs and local resources. N. Engl. J. Med. 2010, 362, 1858–1861. [Google Scholar] [CrossRef]
- Brodie, M.; Weltzien, E.; Altman, D.; Blendon, R.J.; Benson, J.M. Experiences of hurricane Katrina evacuees in Houston shelters: Implications for future planning. Am. J. Public Health 2006, 96, 1402–1408. [Google Scholar] [CrossRef]
- Dorn, T.; Yzermans, C.J.; Kerseens, J.J.; Spreeuwenberg, P.M.; van der Zee, J. Disaster and subsequent healthcare utilization: A longitudinal study among victims, their family members, and control subjects. Med. Care 2006, 44, 581–589. [Google Scholar] [CrossRef]
- Medically Underserved Areas and Populations (MUA/Ps): Guidelines for MUA and MUP Designation. Shortage Designations 2011. Available online: http://bhpr.hrsa.gov/shortage/muaps/index.html. (accessed on 12 June 2011).
- Burkle, F.M., Jr. Mass casualty management of a large-scale bioterrorist event: An epidemiological approach that shapes triage decisions. Emerg. Med. Clin. North Am. 2002, 20, 409–436. [Google Scholar] [CrossRef]
- Noji, E.K. The public health consequences of disasters. Prehosp. Disaster Med. 2000, 15, 147–157. [Google Scholar]
- Wetterhall, S.F.; Noji, E.K. Surveillance and Epidemiology. In Public Health Consequences of Disasters; Oxford University Press: New York, NY, USA, 1997; pp. 37–64. [Google Scholar]
- Billings, J.; Parikh, N.; Miljanovich, T. Emergency Room Use: The New York Story. Available online: http://www.commonwealthfund.org/usr_doc/billings_nystory.pdf (accessed on 7 May 2011).
- Billings, J.; Zeitel, L.; Lukomnik, J.; Carey, T.S.; Blank, A.E.; Newman, L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993, 12, 162–173. [Google Scholar]
- Agency for Healthand Quality, AHRQ Quality Indicators—Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Available online: www.qualityindicators.ahrq.gov/Downloads/Modules/PQI/V31?pqi_guide_v31.pdf (accessed on 29 October 2011).
- Ansari, Z.; Laditka, J.N.; Laditka, S.B. Access to health care and hospitalization for ambulatory care sensitive conditions. Med. Care Res. Rev. 2006, 63, 719–741. [Google Scholar] [CrossRef]
- Caminal, J.; Caminal, J.; Starfield, B.; Sanchez, E.; Casanova, C.; Morales, M. The role of primary care in preventing ambulatory care sensitive conditions. Eur. J. Public Health 2004, 14, 246–251. [Google Scholar] [CrossRef]
- Falik, M.; Needleman, J.; Wells, B.L.; Korb, J. Ambulatory care sensitive hospitalizations and emergency visits: Experiences of medicaid patients using federally qualified health centers. Med. Care 2001, 39, 551–561. [Google Scholar] [CrossRef]
- Cook, T.D.; Campbell, D.T. Reference. In Quasi-Experimentation Design and Analysis Issues for Field Settings; Houghton Mifflin Company: Boston, MA, USA, 1979. [Google Scholar]
- Box, G.E.P.; Jenkins, G.M.; Reinesl, G.C. Reference. In Time Series Analysis: Forecasting and Control; Prentice Hall: Upper Saddle River, NJ, USA, 1994. [Google Scholar]
- Dickey, D.A.; Fuller, W.A. Distribution of the estimators for autoregressive time series with a unit root. J. Amer. Stat. Assn. 1979, 74, 427–431. [Google Scholar]
- Brocklebank, J.C.; Dickey, D.A. Chapter 7: The ARIMA Procedure. In SAS System for Forecasting Time Series, 2nd ed; SAS Institute Inc.: Cary, NC, USA, 2003; pp. 323–358. [Google Scholar]
- Svendsen, E.R.; Whittle, N.C.; Sanders, L.; McKeown, R.E.; Sprayberry, K.; Heim, M.; Caldwell, R.; Gibson, J.J.; Vena, J. GRACE: Public health recovery methods following an environmental disaster. Arch. Environ. Occup. Health 2010, 65, 77–85. [Google Scholar] [CrossRef]
- Ginsberg, J.P.; Holbrook, J.R.; Chanda, D.; Bao, H.; Svendsen, E.R. Posttraumatic stress and tendency to panic in the aftermath of the chlorine gas disaster in Graniteville, South. Carolina. Soc. Psychiatr. Epidemiol. 2012, 47, 1441–1448. [Google Scholar] [CrossRef]
- Epstein, A.J. The role of public clinics in preventable hospitalizations among vulnerable populations. Health Serv. Res. 2001, 26, 405–420. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Runkle, J.D.; Zhang, H.; Karmaus, W.; Martin, A.B.; Svendsen, E.R. Prediction of Unmet Primary Care Needs for the Medically Vulnerable Post-Disaster: An Interrupted Time-Series Analysis of Health System Responses. Int. J. Environ. Res. Public Health 2012, 9, 3384-3397. https://doi.org/10.3390/ijerph9103384
Runkle JD, Zhang H, Karmaus W, Martin AB, Svendsen ER. Prediction of Unmet Primary Care Needs for the Medically Vulnerable Post-Disaster: An Interrupted Time-Series Analysis of Health System Responses. International Journal of Environmental Research and Public Health. 2012; 9(10):3384-3397. https://doi.org/10.3390/ijerph9103384
Chicago/Turabian StyleRunkle, Jennifer D., Hongmei Zhang, Wilfried Karmaus, Amy B. Martin, and Erik R. Svendsen. 2012. "Prediction of Unmet Primary Care Needs for the Medically Vulnerable Post-Disaster: An Interrupted Time-Series Analysis of Health System Responses" International Journal of Environmental Research and Public Health 9, no. 10: 3384-3397. https://doi.org/10.3390/ijerph9103384