Susceptibility to Smoking among Adolescents and Its Implications for Mexico’s Tobacco Control Programs. Analysis of the Global Youth Tobacco Survey 2003-2004 and 2006-2007
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
Acknowledgments
References
- US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2004. [Google Scholar]
- Mackay, J; Ericksen, M. The Tobacco Atlas,, 1st Ed ed; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Peto, R; Lopez, AD. The future worldwide health effects of current smoking patterns. In Global Health in the 21st Century; Koop, EC, Schwarz, RM, Eds.; Jossey-Bass: New York, USA, 2000. [Google Scholar]
- Ezzati, M; Lopez, AD. Estimates of Global Mortality Attributable to Smoking in 2000. Lancet 2003, 362, 847–852. [Google Scholar]
- US Department of Health and Human Services. Preventing Tobacco Use among Young People: A Report of the Surgeon General; US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, Georgia, USA, 1994. [Google Scholar]
- Mackay, J; Ericksen, M; Shafey, O. The Tobacco Atlas, 2nd Ed ed; American Cancer Society: Atlanta, GA, USA, 2006. [Google Scholar]
- World Health Organization. WHO Framework Convention on Tobacco Control; WHO: Geneva, Switzerland. Available at: www.who.int/tobacco/framework/WHO_FCTC_english.pdf (accessed on November 27, 2008).
- WHO Report on the Global Tobacco Epidemic; World Health Organization: Geneva, Switzerland, 2008. Available at: www.who.int/tobacco/mpower/mpower_report_full_2008.pdf (accessed on April 17, 2008).
- Mayhew, KP; Flay, BR; Mott, JA. Stages in the Development of Adolescent Smoking. Drug Alcohol Dependence 2000, 59, S61–S81. [Google Scholar]
- Butross, LS; Kastner, JW. A Brief Review of Adolescents and Tobacco: What We Know and What We Don’t Know. Am. J. Med. Sci 2003, 326, 235–237. [Google Scholar]
- Backinger, CL; Fagan, P; Nattews, E; Grana, R. Adolescent and Young Adult Tobacco Prevention and Cessation: Current Status and Future Directions. Tob Control 2003, 12, IV46–IV53. [Google Scholar]
- Pierce, JP; Farkas, AJ; Evans, N; Gilpin, EA. An Improved Surveillance Measure for Adolescent Smoking? Tob. Control 1995, 4, S47–S56. [Google Scholar]
- Pierce, JP; Farkas, A; Evans, N; Berry, C; Choi, W; Rosbrook, B; Johnson, M; Bal, DG. Tobacco Use in California 1992: A Focus on Preventing Uptake in Adolescents; California Department of Health Services: Sacramento, USA, 1993. [Google Scholar]
- Pierce, JP; Choi, WS; Gilpin, EA; Farkas, AJ; Merritt, RK. Validation of Susceptibility as a Predictor of Which Adolescents Take Up Smoking in the United States. Health Psychol 1996, 15, 355–361. [Google Scholar]
- Gritz, ER; Prokhorov, AV; Hudmon, KS; Jones, MM; Rosenblum, C; Chang, C; Chamberlain, RM; Taylor, WC; Johnston, D; de Moor, C. Predictors of Susceptibility to Smoking and Ever Smoking: A Longitudinal Study in a Triethnic Sample of Adolescents. Nicotine Tob. Res 2003, 5, 493–506. [Google Scholar]
- Valdés-Salgado, R; Meneses-González, F; Lazcano-Ponce, EC; Hernández-Ramos, MI; Hernández-Ávila, M. Encuesta sobre tabaquismo en Jóvenes, México 2003, Instituto Nacional de Salud Pública: Cuernavaca, Morelos, México, 2004.
- Valdés-Salgado, R; Thrasher, J; Sánchez-Zamorano, LM; Lazcano-Ponce, EC; Reynales-Shigematsu, LM; Meneses-González, F; Hernández-Ávila, M. Los Retos del Convenio Marco para el Control del Tabaco en México: Un Diagnóstico a Partir de la Encuesta sobre Tabaquismo en Jóvenes. Salud Publica Mex 2006, 48, S5–S16. [Google Scholar]
- Valdés-Salgado, R; Reynales-Shiguematsu, LM; Lazcano-Ponce, EC; Hernandez-Avila, M. Before and After the Franework Convention on Tobacco Control in Mexico: A Comparison from the 2003 and 2006 Global Youth Tobacco Survey. Salud Publica Mex 2007, 49, S155–S169. [Google Scholar]
- Arillo-Santillan, E; Thrasher, J; Rodrigues-Bolaños, R; Chavez-Ayala, R; Ruiz-Velazco, S; Lazcano-Ponce, EC. Susceptibility to Use Tobacco Among Non-smoking Students in 10 Mexican Cities. Salud Publica Mex 2007, 49, S170–S181. [Google Scholar]
- Instituto Nacional de Estadisticas, Geografia e Informatica: II Conteo de Población y Vivienda. 2005. Available at: www.inegi.gob.mx/est/contenidos/espanol/sistemas/conteo2005/datos/00 pdf/cpv00_pob_2.pdf (accessed on November 27, 2008).
- STATA (computer program) Release 10.0; STATA Corp: College Station, TX, USA, 2007.
- Valdés-Salgado, R. Tobacco Use Determinants among Mexican Students and its Implications for Tobacco Control Local Programs. Presented as Capstone project to obtain the degree of Master of Public Health at Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA, May 6, 2006. Advisor: Dr Frances A Stillman. (unpublished data).
- Kremers, SPJ; de Vries, H; Mudde, AN; Candel, M. Motivational Stages of Adolescent Smoking Initiation: Predictive Validity and Predictors of Transition. Addict. Behav 2004, 29, 781–789. [Google Scholar]
- Bernat, DH; Erickson, DJ; Widome, R; Perry, CL; Forster, JL. Adolescent Smoking Trajectories: Result from a Population-based Cohort Study. J. Adolescent Health 2008, 43, 334–340. [Google Scholar]
- Barrientos-Gutiérrez, T; Reynales-Shigematsu, LM; Ávila-Tang, E; Wipfli, H; Lazcano-Ponce, EC. Exposición al Humo de Tabaco en Hogares de la Ciudad de México: Análisis de Nicotina Ambiental y en Cabello de Niños y Mujeres. Salud Publica Mex 2007, 49, S224–S232. [Google Scholar]
- Lazcano-Ponce, EC; Sánchez-Zamorano, LM; Benowitz, N; Barbosa-Sánchez, L; Hernández-Ávila, M. Elevada Concentración de Metabolitos de Cotinina en Hijos de Padres Fumadores. Salud Publica Mex 2007, 49, S213–S223. [Google Scholar]
- Hernández-Ávila, JE; Tirado-Ramírez, E; Santos-Luna, R; Reynales-Shigematsu, LM. Use of GIS for Billboards and Points-of-sale Surveillance in Two Mexican Cities. Salud Publica Mex 2007, 49, S241–S246. [Google Scholar]
- Kuri-Morales, PA; Cortés-Ramírez, M; Cravioto-Quintana, P; Hoy, MJ; González-Roldán, JF. Políticas, Vigilancia y Acceso de los Menores de Edad a los Cigarros en la Ciudad de México. Salud Publica Mex 2006, 48, S99–S106. [Google Scholar]
- Valdés-Salgado, R; Lazcano-Ponce, EC; Hernández-Ávila, M. Current panorama of tobacco consumption and control measures in Mexico. Prevent. Control 2005, 1, 319–327. [Google Scholar]
- Dirección General de Epidemiología, Secretaría de Salud. In Encuesta Nacional de Adicciones 2002. Tabaco, Alcohol y otras Drogas; Dirección General de Epidemiología, Secretaría de Salud: México, D.F., Mexico, 2003.
- Medina-Mora, ME; Pena-Corona, MP; Cravioto, P; Villatoro, J; Fleiz, C; Kuri, P. Del Tabaco al uso de otras drogas: El uso temprano de tabaco aumenta la posibilidad de usar otras drogas? Salud Publica Mex 2002, 43, S109–S115. [Google Scholar]
- US Department of Health and Human Services. Women and Smoking: A Report of the Surgeon General; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2001. [Google Scholar]
- Samet, JM; Yoon, SY. Women and the Tobacco epidemic: Challenges for the 21st Century; World Health Organization in collaboration with the Institute for Global Tobacco Control at The Johns Hopkins Bloomberg School of Public Health: Geneva, Switzerland, 2001. [Google Scholar]
- Global Youth Tobacco Survey Collaborative Group. Tobacco Use among youth: A cross country comparison. Tob. Control 2002, 11, 252–270. [Google Scholar]
- Warren, W; Jones, NR; Eriksen, MP; Asma, S; The Global Tobacco Surveillance System Collaborating Group. Patterns of Global Tobacco Use in Young People and Implications for Future Chronic Disease Burden in Adults. Lancet 2006, 367, 749–753. [Google Scholar]
- Global Youth Tobacco Survey Collaborating Group. Differences in Worldwide Tobacco Use by Gender: Findings from the Global Youth Tobacco Survey. J. School Health 2003, 73, 207–215. [Google Scholar]
- Programa Escuela Saludable y Segura, Libre del Humo de Tabaco: Ministry of Health, press release No. 291 November 5, 2004. Available at: www.ssa.gob.mx (accessed on May 10, 2005) and Ministry of Education, press release No. 444 November 5, 2004. Available at: www.sep.gob.mx/wb2/sep/sep_Bol4441104 (accessed on May 10, 2005).
- Lantz, PM; Jacobson, PD; Warner, KE; Wasserman, J; Pollack, HA; Berson, J; Ahlstrom, A. Investing in Youth Tobacco Control: A Review of Smoking Prevention and Control Strategies. Tob. Control 2000, 9, 47–63. [Google Scholar]
- WHO Tobacco Free Initiative. In Building Blocks for Tobacco Control: A Handbook; World Health Organization: Geneva, Switzerland, 2004.
- Ley del Impuesto Especial sobre Producción y Servicios, Diario Oficial de la Federación, miércoles 27 de diciembre de 2006. Cuarta sección. México. 2006; 80.
- Ley General para el Control del Tabaco, Publicada en el Diario Oficial de la Federación el 30 de mayo de. 2008.
- Jha, P; Chaloupka, FJ. Tobacco Control in Developing Countries; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Saffer, H; Chaloupka, F. The Effect of Tobacco Advertising Bans on Tobacco Consumption. J. Health Econo 2000, 19, 1117–1137. [Google Scholar]
- Fichtenberg, CM; Glantz, SA. Effect of Smoke-free Workplaces on Smoking Behavior: Systematic Review. BMJ 2002, 325, 188. [Google Scholar]
- Albers, AB; Biener, L; Siegel, M; Cheng, DM; Rigotti, N. Household Smoking Bans and Adolescent Antismoking Attitudes and Smoking Initiation: Findings from a Longitudinal Study of a Massachusetts Youth Cohort. Am. J. Public Health 2008, 98, 1886–1893. [Google Scholar]
- Pechmann, C; Reibling, ET. Antismoking Advertisements for Youths: An Independent Evaluation of Health, Counter-Industry, and Industry Approaches. Am. J. Public Health 2006, 96, 906–913. [Google Scholar]
- Jason, LA; Berk, M; Schnopp-Wyatt, DL; Talbot, B. Effects of Enforcement of Youth Access Laws on Smoking Prevalence. Am. J. Commun. Psychol 1999, 27, 143–160. [Google Scholar]
- Forster, JL; Widome, R; Bernart, DH. Policy Interventions and Surveillance as Strategies to Prevent Tobacco Use in Adolescents and Young Adults. Am. J. Prev. Med 2007, 33, S335–S339. [Google Scholar]
- Centers for Diseases Control and Prevention. Global Youth Tobacco Survey (GYTS) Data Results by Country and Year. CDC: Atlanta, GA, USA. Available at: www.cdc.gov/tobacco/global/gyts/factsheets/paho/factsheets.htm (accessed on February 16, 2009).
- Global Tobacco Surveillance System Collaborating Group. Global Tobacco Surveillance System (GTSS): Purpose, Production, and Potential. J. School Health 2005, 75, 15–24. [Google Scholar]
| Academic Year | City | Schools sampled | Students surveyed | % Females |
|---|---|---|---|---|
| 2003–04 | Mexico City | 25 | 2,099 | 49.7 |
| 2003–04 | Juarez | 25 | 2,210 | 50.4 |
| 2003–04 | Nuevo Laredo | 21 | 1,416 | 51.2 |
| 2003–04 | Tijuana | 25 | 2,000 | 50.9 |
| 2003–04 | Cuernavaca | 25 | 2,075 | 54.8 |
| 2003–04 | Guadalajara | 24 | 2,059 | 53.5 |
| 2003–04 | Puebla | 23 | 1,888 | 49.8 |
| 2003–04 | Chetumal | 9 | 1,415 | 52.9 |
| 2003–04 | Tapachula | 24 | 2,155 | 50.0 |
| 2006–07 | Mexico City | 24 | 1,826 | 50.2 |
| 2006–07 | Juarez | 22 | 1,546 | 51.0 |
| 2006–07 | Nuevo Laredo | 24 | 1,414 | 51.2 |
| 2006–07 | Tijuana | 23 | 1,785 | 51.3 |
| 2006–07 | Cuernavaca | 23 | 2,001 | 54.7 |
| 2006–07 | Guadalajara | 24 | 2,093 | 53.5 |
| 2006–07 | Puebla | 22 | 1,767 | 49.7 |
| 2006–07 | Chetumal | 11 | 1,456 | 53.1 |
| 2006–07 | Tapachula | 25 | 2,092 | 50.1 |
| Total | 399 | 33,297 | 51.5 | |
| City | Prevalence of smoking during past 30 days (95% CI)
| |
|---|---|---|
| 2003–2004 | 2006–2007 | |
| Mexico City | 20.2 (16.3 – 24.1) | 27.8 (24.0 – 31.9) |
| Juarez | 22.6 (18.7 – 26.5) | 17.7 (15.8 – 19.9) |
| Nuevo Laredo | 16.5 (13.3 – 19.7) | 14.2 (11.9 – 17.0) |
| Tijuana | 11.5 (9.3 – 13.7) | 13.0 (11.2 – 15.2) |
| Cuernavaca | 20.8 (18.1 – 23.5) | 21.7 (18.9 – 24.8) |
| Guadalajara | 19.9 (15.2 – 24.6) | 17.3 (14.8 – 20.2) |
| Puebla | 25.4 (20.0 – 30.8) | 27.5 (24.9 – 30.2) |
| Chetumal | 17.9 (14.9 – 20.9) | 14.6 (12.1 – 17.6) |
| Tapachula | 13.8 (11.2 – 16.4) | 16.3 (14.3 – 18.6) |
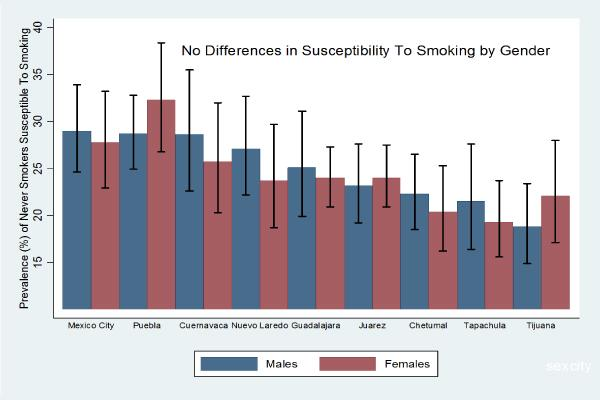
| Academic Year | City | Males % susceptible to smoke (95% CI) | Females % susceptible to smoke (95% CI) |
|---|---|---|---|
| 2003–04 | Mexico City | 22.0 (18.8 – 25.2) | 27.5 (22.9 – 32.1) |
| 2003–04 | Juarez | 21.5 (18.1 – 24.9) | 23.8 (18.9 – 28.7) |
| 2003–04 | Nuevo Laredo | 20.6 (17.7 – 23.5) | 26.6 (21.1 – 32.1) |
| 2003–04 | Tijuana | 22.8 (19.2 – 26.4) | 21.3 (18.5 – 24.1) |
| 2003–04 | Cuernavaca | 27.0 (22.2 – 31.8) | 27.7 (22.2 – 33.2) |
| 2003–04 | Guadalajara | 25.4 (21.8 – 29.0) | 30.2 (25.6 – 34.8) |
| 2003–04 | Puebla | 27.7 (23.6 – 31.8) | 31.1 (25.2 – 37.0) |
| 2003–04 | Chetumal | 24.5 (19.5 – 29.5) | 27.1 (21.6 – 32.6) |
| 2003–04 | Tapachula | 20.4 (16.0 – 24.8) | 17.5 (14.3 – 20.7) |
| 2006–07 | Mexico City | 29.0 (24.6 – 33.9) | 27.8 (22.9 – 33.2) |
| 2006–07 | Juarez | 23.2 (19.2 – 27.6) | 24.0 (20.9 – 27.5) |
| 2006–07 | Nuevo Laredo | 27.1 (22.2 – 32.7) | 23.7 (18.7 – 29.7) |
| 2006–07 | Tijuana | 18.8 (14.9 – 23.4) | 22.1 (17.1 – 28.0) |
| 2006–07 | Cuernavaca | 28.6 (22.6 – 35.5) | 25.7 (20.3 – 32.0) |
| 2006–07 | Guadalajara | 25.1 (19.9 – 31.1) | 24.0 (20.9 – 27.3) |
| 2006–07 | Puebla | 28.7 (24.9 – 32.8) | 32.3 (26.8 – 38.4) |
| 2006–07 | Chetumal | 22.3 (18.5 – 26.5) | 20.4 (16.2 – 25.3) |
| 2006–07 | Tapachula | 21.5 (16.4 – 27.6) | 19.3 (15.6 – 23.7) |
| City | Proportion of non smokers susceptible to smoke (95% CI)
| |
|---|---|---|
| 2003–2004 | 2006–2007 | |
| Mexico City | 25.1 (22.1 – 28.1) | 29.4 (26.2 – 32.9) |
| Juarez | 22.8 (20.1 – 25.5) | 24.3 (21.3 – 27.6) |
| Nuevo Laredo | 24.2 (20.8 – 27.6) | 25.3 (21.8 – 29.1) |
| Tijuana | 22.2 (20.2 – 24.2) | 20.4 (16.9 – 24.5) |
| Cuernavaca | 27.5 (23.8 – 31.2) | 27.6 (24.0 – 31.5) |
| Guadalajara | 28.1 (25.2 – 31.0) | 24.5 (21.8 – 27.4) |
| Puebla | 30.4 (26.7 – 34.1) | 31.0 (27.4 – 34.9) |
| Chetumal | 26.2 (22.5 – 29.9) | 21.9 (19.0 – 25.1) |
| Tapachula | 18.8 (16.0 – 21.6) | 20.3 (17.3 – 23.6) |
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Valdés-Salgado, R.; Reynales-Shiguematsu, L.M.; Lazcano-Ponce, E.C.; Hernández-Avila, M. Susceptibility to Smoking among Adolescents and Its Implications for Mexico’s Tobacco Control Programs. Analysis of the Global Youth Tobacco Survey 2003-2004 and 2006-2007. Int. J. Environ. Res. Public Health 2009, 6, 1254-1267. https://doi.org/10.3390/ijerph6031254
Valdés-Salgado R, Reynales-Shiguematsu LM, Lazcano-Ponce EC, Hernández-Avila M. Susceptibility to Smoking among Adolescents and Its Implications for Mexico’s Tobacco Control Programs. Analysis of the Global Youth Tobacco Survey 2003-2004 and 2006-2007. International Journal of Environmental Research and Public Health. 2009; 6(3):1254-1267. https://doi.org/10.3390/ijerph6031254
Chicago/Turabian StyleValdés-Salgado, Raydel, Luz Myriam Reynales-Shiguematsu, Eduardo C Lazcano-Ponce, and Mauricio Hernández-Avila. 2009. "Susceptibility to Smoking among Adolescents and Its Implications for Mexico’s Tobacco Control Programs. Analysis of the Global Youth Tobacco Survey 2003-2004 and 2006-2007" International Journal of Environmental Research and Public Health 6, no. 3: 1254-1267. https://doi.org/10.3390/ijerph6031254