Predicting Urban Medical Services Demand in China: An Improved Grey Markov Chain Model by Taylor Approximation
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Traditional GM (1,1) Model
2.2. Grey Markov Chain Prediction Model
2.2.1. The Partition of Transferring
2.2.2. The Establishment of the State Transition Matrix
2.2.3. Prediction of the Grey Markov Chain Model
2.3. The Development of Grey Markov Chain Model with Taylor Approximation
2.4. Data
2.5. Procedure
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Deb, P.; Trivedi, P.K. Demand for medical care by the elderly: A finite mixture approach. J. Appl. Econ. 1997, 12, 313–336. [Google Scholar]
- Parker, M.G.; Thorslund, M. Health trends in the elderly population: Getting better and getting worse. Gerontologist 2007, 47, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Lehnert, T.; Heider, D.; Leicht, H.; Heinrich, S.; Corrieri, S.; Luppa, M.; König, H.H. Review: Health care utilization and costs of elderly persons with multiple chronic conditions. Med. Care Res. Rev. 2011, 68, 387–420. [Google Scholar] [PubMed]
- Umberson, D.; Montez, J.K. Social relationships and health a flashpoint for health policy. J. Health Soc. Behav. 2010, 51 (Suppl. 1), S54–S66. [Google Scholar] [CrossRef] [PubMed]
- Grossman, M. On the concept of health capital and the demand for health. J. Political Econ. 1972, 80, 223–255. [Google Scholar] [CrossRef]
- Hupert, N.; Wattson, D.; Cuomo, J.; Benson, S. Anticipating Demand for Emergency Health Services due to Medication-related Adverse Events after Rapid Mass Prophylaxis Campaigns. Acad. Emerg. Med. 2007, 14, 268–274. [Google Scholar] [PubMed]
- McCarthy, M.L.; Zeger, S.L.; Ding, R.; Aronsky, D.; Hoot, N.R.; Kelen, G.D. The challenge of predicting demand for emergency department services. Acad. Emerg. Med. 2008, 15, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Lowthian, J.A.; Curtis, A.J.; Jolley, D.J.; Stoelwinder, J.U.; McNeil, J.J.; Cameron, P.A. Demand at the emergency department front door: 10-year trends in presentations. Med. J. Aust. 2012, 196, 128–132. [Google Scholar] [PubMed]
- Hagihara, A.; Hasegawa, M.; Hinohara, Y.; Abe, T.; Motoi, M. The aging population and future demand for emergency ambulances in Japan. Intern. Emerg. Med. 2013, 8, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liang, L.; Liu, E.; Chen, C.; Atkins, D. Patient choice analysis and demand prediction for a health care diagnostics company. Eur. J. Oper. Res. 2016, 251, 198–205. [Google Scholar]
- Liu, J.X.; Goryakin, Y.; Maeda, A.; Bruckner, T.; Scheffler, R. Global Health Workforce Labor Market Projections for 2030. Hum. Resour. Health 2017, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jäger, R.; Berg, N.; Hoffmann, W. Estimating future dental services’ demand and supply: A model for Northern Germany. Community Dent. Oral Epidemiol. 2016, 44, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Gudleski, G.D.; Satchidanand, N.; Dunlap, L.J. Predictors of medical and mental health care use in patients with irritable bowel syndrome in the United States. Behav. Res. Ther. 2017, 88, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Jalalpoura, M.; Gelb, Y.; Levincd, S. Forecasting demand for health services: Development of a publicly available toolbox. Oper. Res. Health Care 2015, 5, 1–9. [Google Scholar] [CrossRef]
- Veser, A.; Sieber, F.; Groß, S.; Prückner, S. The demographic impact on the demand for emergency medical services in the urban and rural regions of Bavaria, 2012–2032. J. Public Health 2015, 23, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Xia, J.L.; Wang, J. Comparison of predictive effect between the single auto regressive integrated moving average (ARIMA) model and the ARIMA-generalized regression neural network (GRNN) combination model on the incidence of scarlet fever. Chin. J. Epidemiol. 2009, 30, 964–968. [Google Scholar]
- Yu, S.J.; Zhu, C.H.; Li, J. Cardiovascular Hospital Medical Service Demand Estimation. Chin. Hosp. Archit. Equip. 2014, 15, 99–103. [Google Scholar]
- Li, Y.Z.; Zhang, T.; Wan, L.Z. Estimation of Demand Volume for Basic Public Health Services Based on Age-gender Population Structure. Chin. Gen. Pract. 2016, 19, 400–403. [Google Scholar]
- Landry, M.D.; Hack, L.M.; Coulson, E.; Freburger, J.; Johnson, M.P.; Katz, R.; Kerwin, J.; Smith, M.H.; Venskus, D.G.; Sinnott, P.L.; et al. Workforce Projections 2010–2020: Annual Supply and Demand Forecasting Models for Physical Therapists Across the United States. Phys. Ther. 2016, 96, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Li, M.; Ge, Y.; Li, L.; Zhang, Y.; Liu, Y.; Zhang, L. Transformation of Potential Medical Demand in China: A System Dynamics Simulation Model. J. Biomed. Inform. 2015, 57, 399–414. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, T.; Oliveira, M.D.; Barbosa-Póvoa, A. Modeling the demand for long-term care services under uncertain information. Health Care Manag. Sci. 2012, 15, 385–412. [Google Scholar] [CrossRef] [PubMed]
- Akita, T.; Tanaka, J.; Ohisa, M. Predicting future blood supply and demand in Japan with a Markov model: Application to the sex- and age-specific probability of blood donation. Transfusion 2016, 56, 2750–2759. [Google Scholar] [CrossRef] [PubMed]
- Kumar, U.; Jain, V.K. Time Series models (Grey-markov, Grey Model with rolling mechanism and Singular Spectrum analysis) to Forecast Energy Consumption in India. Energy 2010, 35, 1709–1716. [Google Scholar] [CrossRef]
- Chen, L.H.; Guo, T.S. Forecasting Financial crises for an enterprise by using the Grey Markov forecasting model. Qual. Quant. 2011, 45, 911–922. [Google Scholar] [CrossRef]
- Lin, L.C.; Wu, S.Y. Analyzing Taiwan IC Assembly Industry by Grey-Markov Forecasting Model. Math. Probl. Eng. 2013, 2013, 1024–1030. [Google Scholar] [CrossRef]
- Kordnoori, S.; Mostafaei, H.; Kordnoon, S. The Application of Fourier Residual Grey Verhulst and Grey Markov Model in Analyzing the Global ICT Development. Hyperion Econ. J. 2014, 2, 50–60. [Google Scholar]
- Edem, I.E.; Oke, S.A.; Adebiyi, K.A. A modified grey-Markov Fire Accident Model Based on Information Turbulence Indices and Restricted Residuals. Int. J. Manag. Sci. Eng. Manag. 2016, 11, 231–242. [Google Scholar] [CrossRef]
- Peng, R. Analysis of Senior Population Nursing Needs Based on Markov Model. Stat. Inf. Forum 2009, 24, 77–80. [Google Scholar]
- Huang, F.; Wu, C. A Study of Long-Term-Care Demand of the Elderly in China: Based on Multistatus Transition Model. Econ. Res. J. 2012, 47, 119–130. [Google Scholar]
- Hu, H.; Li, Y.; Zhang, L. Estimation and Prediction of Demand of Chinese Elederly Long-term Care Services. Chin. J. Popul. Sci. 2015, 13, 79–89. [Google Scholar]
- Argiento, R.; Guglielmi, A.; Lanzarone, E.; Nawajah, I. A Bayesian framework for describing and predicting the stochastic demand of home care patients. Flex. Serv. Manuf. J. 2016, 28, 254–279. [Google Scholar] [CrossRef]
- Deng, J. Introduction to grey system theory. J. Grey Syst. 1989, 1, 1–24. [Google Scholar]
- Lin, Y.; Liu, S.F. A historical introduction to grey systems theory. In Proceedings of the 2004 IEEE International Conference on Systems, Man, and Cybernetics, Hague, The Netherlands, 10–13 October 2004; Volume 3, pp. 2403–2408. [Google Scholar]
- Deng, J. Control problems of grey system. Syst. Control Lett. 1982, 1, 288–294. [Google Scholar]
- Deng, J. Extent Information Cover in Grey System Theory. J. Grey Syst. 1995, 7, 13–25. [Google Scholar]
- Chen, F.Y.; Zhang, L.Y.; Yang, W.X. Analysis and Prediction of The Supply and Demand of Bed Resources in Tianjin City. Chin. J. Health Stat. 2012, 29, 404–405. [Google Scholar]
- Xiang, H.L.; Guo, S.X.; Tang, J.X.; Cao, L.; Liu, X.P.; Liu, J.M.; Guo, H.; Liu, H.T.; Li, S.G. Based on multi-factors grey model to predict demand for community health workforce. Chin. J. Health Stat. 2015, 32, 493–495. [Google Scholar]
- Bao, C.Z.; Mayila, M.; Ye, Z.H.; Wang, J.B.; Jin, M.J.; He, W.J.; Chen, K. Forecasting and Analyzing the Disease Burden of Aged Population in China, Based on the 2010 Global Burden of Disease Study. Int. J. Environ. Res. Public Health 2015, 12, 7172–7184. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.X.; Du, Q.Y.; Ren, F.; Liang, S.; Lin, D.; Tian, Q.; Chen, Y.; Li, J. Spatio-Temporal Variation and Prediction of Ischemic Heart Disease Hospitalizations in Shenzhen, China. Int. J. Environ. Res. Public Health 2014, 11, 4799–4824. [Google Scholar] [CrossRef] [PubMed]
- Li, G.-D.; Yamaguchi, D; Nagai, M. A GM (1,1)–Markov chain combined model with an application to predict the number of Chinese international airlines. Technol. Forecast. Soc. Chang. 2007, 74, 1465–1481. [Google Scholar]
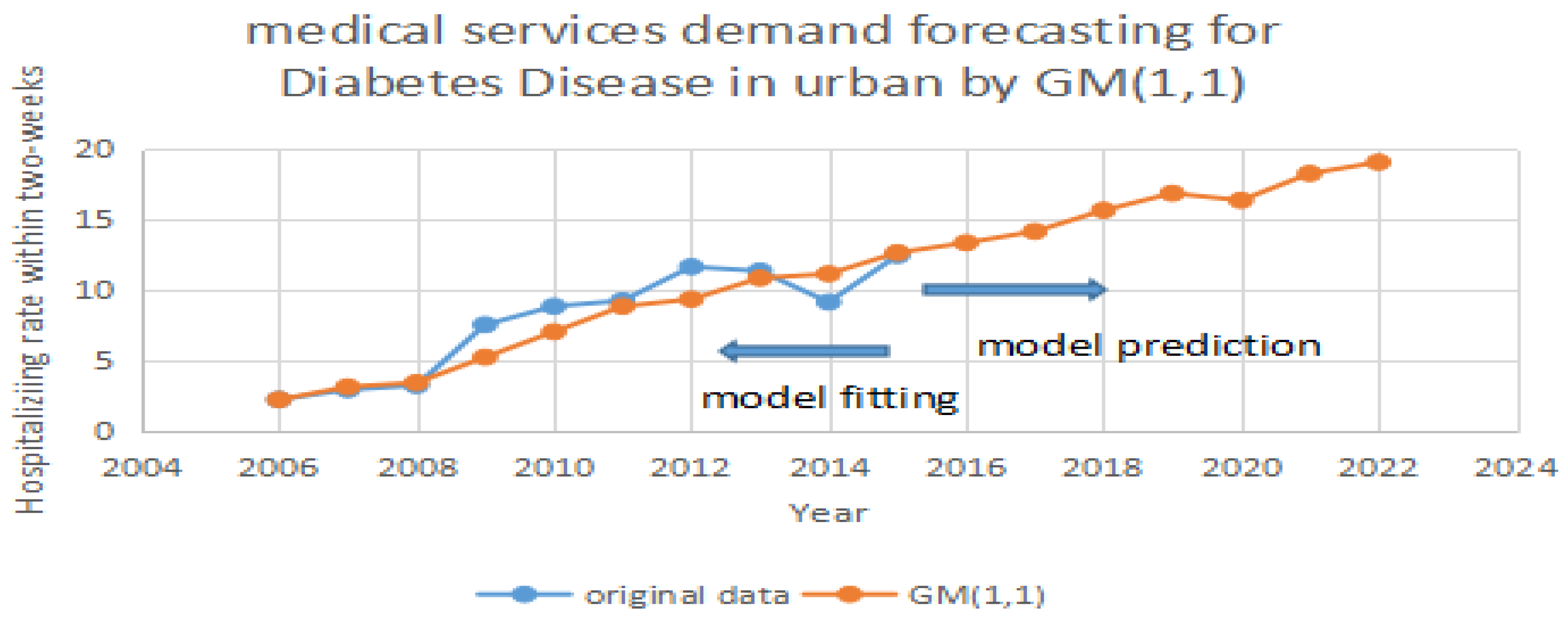




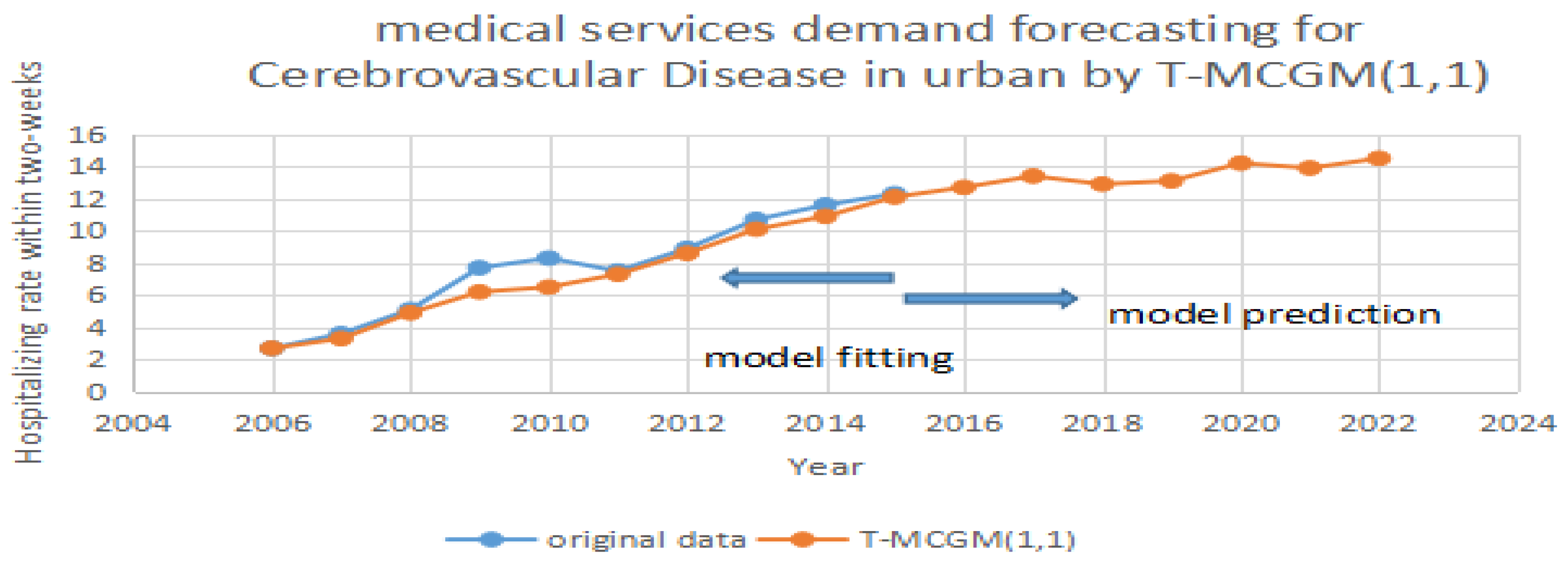

| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| DD | 2.3 | 3 | 3.3 | 7.6 | 8.2 | 9.3 | 10.7 | 11.4 | 10.5 | 12.5 |
| HD | 12.2 | 11.4 | 10.2 | 11.9 | 13.5 | 14.7 | 16.1 | 17.5 | 18.3 | 19.9 |
| CD | 2.7 | 6.7 | 3.6 | 5.1 | 6.9 | 7.5 | 8.9 | 10.7 | 11.6 | 12.3 |
| Model | Diabetes Disease | Heart Disease | Cerebrovascular | |||
|---|---|---|---|---|---|---|
| MAPE | RMSE | MAPE | RMSE | MAPE | RMSE | |
| ARMA | 11.68% | 0.5427 | 13.53% | 0.7011 | 11.32% | 0.4936 |
| BP | 12.77% | 0.6481 | 12.35% | 0.5673 | 11.21% | 0.4922 |
| GM (1,1) | 11.54% | 0.4284 | 10.30% | 0.5453 | 9.59% | 0.3254 |
| T-MCGM (1,1) | 5.66% | 0.2016 | 6.23% | 0.3333 | 6.31% | 0.2577 |
| Year | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|---|
| DD | 13.2 | 14.5 | 16.6 | 16.2 | 17.3 | 18.4 | 19 |
| HD | 22.8 | 22.2 | 23.6 | 24.7 | 25.9 | 24.3 | 24.9 |
| CD | 12.7 | 13.4 | 12.9 | 13.1 | 14.2 | 13.9 | 14.5 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duan, J.; Jiao, F.; Zhang, Q.; Lin, Z. Predicting Urban Medical Services Demand in China: An Improved Grey Markov Chain Model by Taylor Approximation. Int. J. Environ. Res. Public Health 2017, 14, 883. https://doi.org/10.3390/ijerph14080883
Duan J, Jiao F, Zhang Q, Lin Z. Predicting Urban Medical Services Demand in China: An Improved Grey Markov Chain Model by Taylor Approximation. International Journal of Environmental Research and Public Health. 2017; 14(8):883. https://doi.org/10.3390/ijerph14080883
Chicago/Turabian StyleDuan, Jinli, Feng Jiao, Qishan Zhang, and Zhibin Lin. 2017. "Predicting Urban Medical Services Demand in China: An Improved Grey Markov Chain Model by Taylor Approximation" International Journal of Environmental Research and Public Health 14, no. 8: 883. https://doi.org/10.3390/ijerph14080883





