Vulnerability Reduction Needed to Maintain Current Burdens of Heat-Related Mortality in a Changing Climate—Magnitude and Determinants
Abstract
:1. Introduction
Hypothesis and Aim
2. Materials and Methods
2.1. Climate Scenarios
2.2. Population Data
2.3. Impact Calculation
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- De’ Donato, F.K.; Leone, M.; Scortichini, M.; De Sario, M.; Katsouyanni, K.; Lanki, T.; Basagana, X.; Ballester, F.; Astrom, C.; Paldy, A.; et al. Changes in the effect of heat on mortality in the last 20 years in nine European cities. Results from the phase project. Int. J. Environ. Res. Public Health 2015, 12, 15567–15583. [Google Scholar] [CrossRef] [PubMed]
- Baccini, M.; Biggeri, A.; Accetta, G.; Kosatsky, T.; Katsouyanni, K.; Analitis, A.; Anderson, H.R.; Bisanti, L.; D’Ippoliti, D.; Danova, J.; et al. Heat effects on mortality in 15 European cities. Epidemiology 2008, 19, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Fouillet, A.; Rey, G.; Laurent, F.; Pavillon, G.; Bellec, S.; Guihenneuc-Jouyaux, C.; Clavel, J.; Jougla, E.; Hemon, D. Excess mortality related to the august 2003 heat wave in France. Int. Arch. Occup. Environ. Health 2006, 80, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, S.C.; Dixon, P.G. Spatiotemporal trends in human vulnerability and adaptation to heat across the United States. Anthropocene 2016. [Google Scholar] [CrossRef]
- Astrom, D.O.; Forsberg, B.; Edvinsson, S.; Rocklov, J. Acute fatal effects of short-lasting extreme temperatures in Stockholm, Sweden: Evidence across a century of change. Epidemiology 2013, 24, 820–829. [Google Scholar] [CrossRef] [PubMed]
- Arbuthnott, K.; Hajat, S.; Heaviside, C.; Vardoulakis, S. Changes in population susceptibility to heat and cold over time: Assessing adaptation to climate change. Environ. Health 2016, 15. [Google Scholar] [CrossRef] [PubMed]
- Field, C.B. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation: Special Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar]
- Nikulin, G.; Kjellstrom, E.; Hansson, U.; Strandberg, G.; Ullerstig, A. Evaluation and future projections of temperature, precipitation and wind extremes over Europe in an ensemble of regional climate simulations. Tellus A 2011, 63, 41–55. [Google Scholar] [CrossRef]
- Jacob, D.; Petersen, J.; Eggert, B.; Alias, A.; Christensen, O.B.; Bouwer, L.M.; Braun, A.; Colette, A.; Deque, M.; Georgievski, G.; et al. Euro-cordex: New high-resolution climate change projections for European impact research. Reg. Environ. Chang. 2014, 14, 563–578. [Google Scholar] [CrossRef]
- Strandberg, G.; Bärring, L.; Hansson, U.; Jansson, C.; Jones, C.; Kjellström, E.; Kolax, M.; Kupiainen, M.; Nikulin, G.; Samuelsson, P. Cordex Scenarios for Europe from the Rossby Centre Regional Climate Model RCA4; Sveriges Meteorologiska och Hydrologiska Institut (SMHI): Norrköping, Sweden, 2015. [Google Scholar]
- Clarke, L.; Edmonds, J.; Jacoby, H.; Pitcher, H.; Reilly, J.; Richels, R. Scenarios of Greenhouse Gas Emissions and Atmospheric Concentrations; US Department of Energy Publications: Lincoln, NE, USA, 2007.
- Moss, R.H.; Edmonds, J.A.; Hibbard, K.A.; Manning, M.R.; Rose, S.K.; van Vuuren, D.P.; Carter, T.R.; Emori, S.; Kainuma, M.; Kram, T.; et al. The next generation of scenarios for climate change research and assessment. Nature 2010, 463, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Van Vuuren, D.P.; Edmonds, J.; Kainuma, M.; Riahi, K.; Thomson, A.; Hibbard, K.; Hurtt, G.C.; Kram, T.; Krey, V.; Lamarque, J.F.; et al. The representative concentration pathways: An overview. Clim. Chang. 2011, 109, 5–31. [Google Scholar] [CrossRef]
- Thomson, A.M.; Calvin, K.V.; Smith, S.J.; Kyle, G.P.; Volke, A.; Patel, P.; Delgado-Arias, S.; Bond-Lamberty, B.; Wise, M.A.; Clarke, L.E.; et al. RCP 4.5: A pathway for stabilization of radiative forcing by 2100. Clim. Chang. 2011, 109, 77–94. [Google Scholar] [CrossRef]
- Riahi, K.; Rao, S.; Krey, V.; Cho, C.H.; Chirkov, V.; Fischer, G.; Kindermann, G.; Nakicenovic, N.; Rafaj, P. RCP 8.5-A scenario of comparatively high greenhouse gas emissions. Clim. Chang. 2011, 109, 33–57. [Google Scholar] [CrossRef]
- Pachauri, R.K.; Allen, M.R.; Barros, V.R.; Broome, J.; Cramer, W.; Christ, R.; Church, J.A.; Clarke, L.; Dahe, Q.; Dasgupta, P. Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Intergovenmental Panel on Climate Change (IPCC): Geneva, Switzerland, 2014. [Google Scholar]
- Kjellström, E.; Bärring, L.; Nikulin, G.; Nilsson, C.; Persson, G.; Strandberg, G. Production and use of regional climate model projections—A Swedish perspective on building climate services. Clim. Serv. 2016, 2–3, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Dee, D.P.; Uppala, S.M.; Simmons, A.J.; Berrisford, P.; Poli, P.; Kobayashi, S.; Andrae, U.; Balmaseda, M.A.; Balsamo, G.; Bauer, P.; et al. The era-interim reanalysis: Configuration and performance of the data assimilation system. Q. J. R. Meteorol. Soc. 2011, 137, 553–597. [Google Scholar] [CrossRef]
- Kuhn, A.; Vinneau, D.; Yang, A.; Roos, J. Population Data for the Common Case Study in INTARESE and HEIMTSA. Available online: http://en.opasnet.org/en-opwiki/images/e/ed/Population_data_documentation.pdf (accessed on 3 July 2017).
- Statistical Services Branch, United Nations Statistics Division. Standard Country or Area Codes for Statistical Use. Available online: https://unstats.un.org/unsd/publication/SeriesM/Series_M49_Rev4(1999)_en.pdf (accessed on 3 July 2017).
- Li, T.T.; Horton, R.M.; Kinney, P.L. Projections of seasonal patterns in temperature-related deaths for Manhattan, New York. Nat. Clim. Chang. 2013, 3, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Peng, R.D.; Bobb, J.F.; Tebaldi, C.; McDaniel, L.; Bell, M.L.; Dominici, F. Toward a quantitative estimate of future heat wave mortality under global climate change. Environ. Health Perspect. 2011, 119, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Knowlton, K.; Lynn, B.; Goldberg, R.A.; Rosenzweig, C.; Hogrefe, C.; Rosenthal, J.K.; Kinney, P.L. Projecting heat-related mortality impacts under a changing climate in the new york city region. Am. J. Public Health 2007, 97, 2028–2034. [Google Scholar] [CrossRef] [PubMed]
- Baccini, M.; Kosatsky, T.; Analitis, A.; Anderson, H.R.; D’Ovidio, M.; Menne, B.; Michelozzi, P.; Biggeri, A.; Grp, P.C. Impact of heat on mortality in 15 European cities: Attributable deaths under different weather scenarios. J. Epidemiol. Commun. Health 2011, 65, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Guariguata, L.; Whiting, D.R.; Hambleton, I.; Beagley, J.; Linnenkamp, U.; Shaw, J.E. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res. Clin. Pract. 2014, 103, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Oudin Astrom, D.; Schifano, P.; Asta, F.; Lallo, A.; Michelozzi, P.; Rocklov, J.; Forsberg, B. The effect of heat waves on mortality in susceptible groups: A cohort study of a mediterranean and a northern European city. Environ. Health 2015, 14, 30. [Google Scholar] [CrossRef] [PubMed]
- Andersson, T.; Ahlbom, A.; Carlsson, S. Diabetes prevalence in Sweden at present and projections for year 2050. PLoS ONE 2015, 10, e0143084. [Google Scholar] [CrossRef] [PubMed]
- Barnes, P.J. Chronic obstructive pulmonary disease: A growing but neglected global epidemic. PLoS Med. 2007, 4, e112. [Google Scholar] [CrossRef] [PubMed]
- Kainu, A.; Pallasaho, P.; Pietinalho, A. No change in prevalence of symptoms of COPD between 1996 and 2006 in Finnish adults—A report from the Finess Helsinki Study. Eur. Clin. Respir. J. 2016, 3, 31780. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklov, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
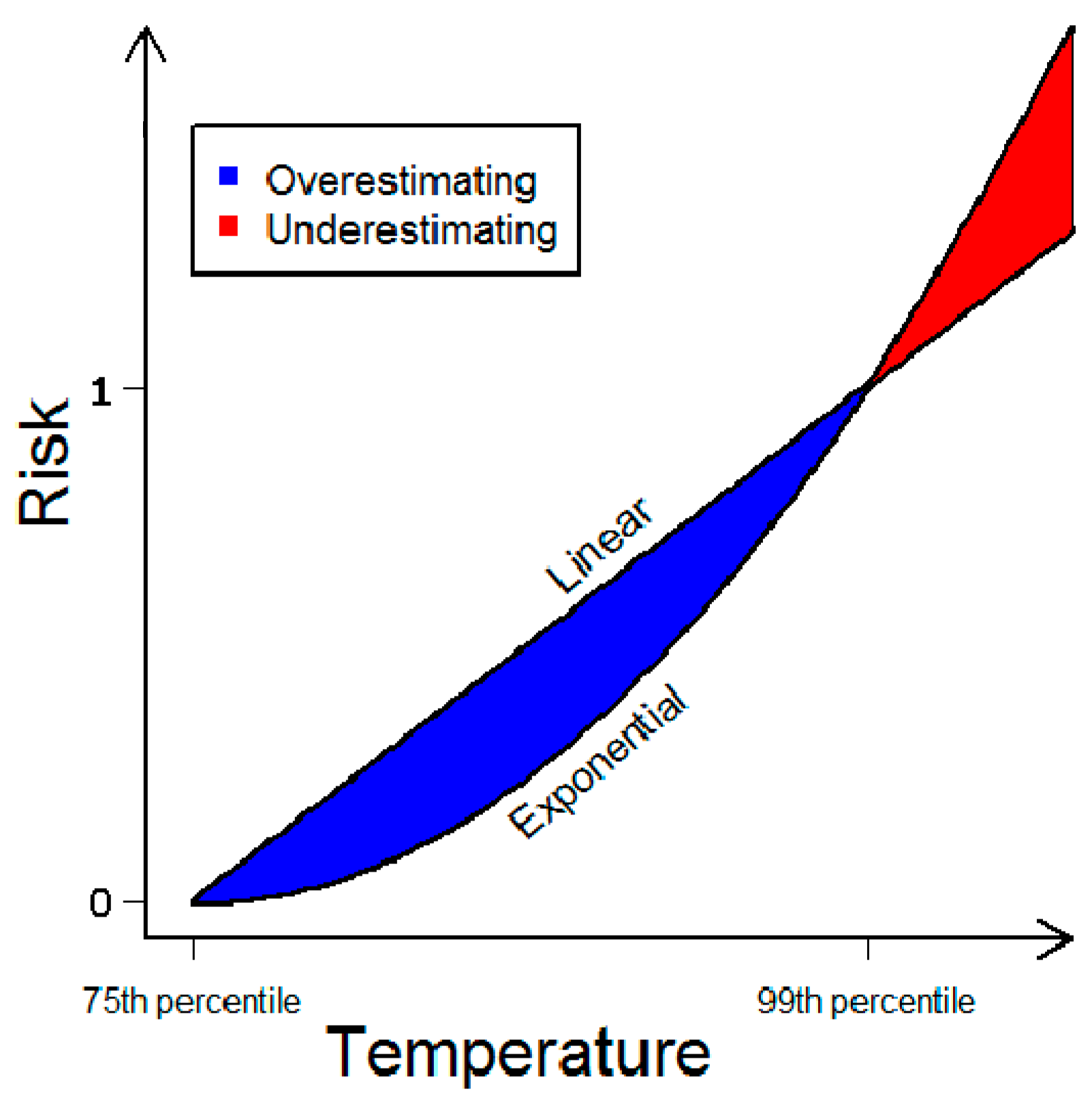
- Rocklov, J.; Ebi, K.L. High dose extrapolation in climate change projections of heat-related mortality. J. Agric. Biol. Environ. Stat. 2012, 17, 461–475. [Google Scholar] [CrossRef]
- Benmarhnia, T.; Deguen, S.; Kaufman, J.S.; Smargiassi, A. Vulnerability to heat-related mortality: A systematic review, meta-analysis, and meta-regression analysis. Epidemiology 2015, 26, 781–793. [Google Scholar] [CrossRef] [PubMed]
- Benmarhnia, T.; Oulhote, Y.; Petit, C.; Lapostolle, A.; Chauvin, P.; Zmirou-Navier, D.; Deguen, S. Chronic air pollution and social deprivation as modifiers of the association between high temperature and daily mortality. Environ. Health 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Ishigami, A.; Hajat, S.; Kovats, R.S.; Bisanti, L.; Rognoni, M.; Russo, A.; Paldy, A. An ecological time-series study of heat-related mortality in three European cities. Environ. Health 2008, 7, 5. [Google Scholar] [CrossRef] [PubMed]
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk? Occup. Environ. Med. 2007, 64, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Rocklov, J.; Forsberg, B.; Ebi, K.; Bellander, T. Susceptibility to mortality related to temperature and heat and cold wave duration in the population of Stockholm county, Sweden. Glob. Health Action 2014, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Caranci, N.; De’Donato, F.; Demaria, M.; Michelozzi, P.; Miglio, R.; Rognoni, M.; Russo, A.; et al. Factors affecting in-hospital heat-related mortality: A multi-city case-crossover analysis. J. Epidemiol. Commun. Health 2008, 62, 209–215. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Public Health Advice on Preventing Health Effects of Heat. Available online: http://www.euro.who.int/__data/assets/pdf_file/0007/147265/Heat_information_sheet.pdf?ua=1 (accessed on 3 July 2017).
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Disparities by race in heat-related mortality in four US cities: The role of air conditioning prevalence. J. Urban Health 2005, 82, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Fouillet, A.; Rey, G.; Wagner, V.; Laaidi, K.; Empereur-Bissonnet, P.; Le Tertre, A.; Frayssinet, P.; Bessemoulin, P.; Laurent, F.; De Crouy-Chanel, P.; et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int. J. Epidemiol. 2008, 37, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Palecki, M.A.; Changnon, S.A.; Kunkel, K.E. The nature and impacts of the July 1999 heat wave in the midwestern United States: Learning from the lessons of 1995. Bull. Am. Meteorol. Soc. 2001, 82, 1353–1367. [Google Scholar] [CrossRef]
- Ebi, K.; Teisberg, T.; Kalkstein, L.; Robinson, L.; Weiher, R. Heat watch/warning systems save lives: Estimated costs and benefits for Philadelphia 1995–1998. Epidemiology 2003, 14, S35. [Google Scholar] [CrossRef]
- Weisskopf, M.G.; Anderson, H.A.; Foldy, S.; Hanrahan, L.P.; Blair, K.; Torok, T.J.; Rumm, P.D. Heat wave morbidity and mortality, Milwaukee, WIS, 1999 vs 1995: An improved response? Am. J. Public Health 2002, 92, 830–833. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.G.; Zheng, Y.F.; Song, G.X.; Kalkstein, L.S.; Kalkstein, A.J.; Tang, X. Heat wave impacts on mortality in Shanghai, 1998 and 2003. Int. J. Biometeorol. 2007, 51, 193–200. [Google Scholar] [CrossRef] [PubMed]
| All Ages | Above Age 65 | |||
|---|---|---|---|---|
| Region | Present Population | Future Population | Future Population | |
| Present climate | All study area | −0.2 (−0.2, −0.2) | 38.9 (38.9, 38.9) | |
| Northern Europe | 2.2 (2.1, 2.2) | 34.7 (34.7, 34.7) | ||
| Western Europe | 7.0 (7.0, 7.0) | 41.3 (41.3, 41.3) | ||
| Eastern Europe | −17.2 (−17.2, −17.2) | 38.0 (38.0, 38.0) | ||
| Southern Europe | 3.4 (3.4, 3.4) | 45.9 (45.9, 45.9) | ||
| RCP 4.5 | All study area | 47.0 (33.7, 54.9) | 46.8 (33.3, 54.4) | 67.5 (59.4, 72.3) |
| Northern Europe | 45.0 (31.7, 54.6) | 46.1 (32.4, 55.2) | 64.1 (54.9, 70.1) | |
| Western Europe | 45.1 (29.7, 53.3) | 48.9 (34.5, 56.4) | 67.8 (58.7, 72.5) | |
| Eastern Europe | 45.6 (29.5, 52.1) | 36.6 (18, 44.1) | 66.6 (56.8, 70.6) | |
| Southern Europe | 53.5 (44.4, 61.2) | 54.8 (46, 62.3) | 74.7 (69.7, 78.9) | |
| RCP 8.5 | All study area | 53.4 (34.6, 63.7) | 52.9 (34, 63.2) | 71.4 (59.8, 77.7) |
| Northern Europe | 53.6 (44, 62.9) | 54.3 (44.9, 62.9) | 69.5 (63.2, 75.1) | |
| Western Europe | 50.1 (24.6, 61.4) | 53.4 (29.8, 64) | 70.7 (55.8, 77.3) | |
| Eastern Europe | 49.8 (32.1, 58.4) | 41.7 (21.6, 51.7) | 69.3 (58.6, 74.6) | |
| Southern Europe | 60.8 (46.7, 68.7) | 61.7 (47.9, 69.5) | 78.5 (70.7, 82.9) | |
| Population change | ||
|---|---|---|
| Region | All Ages | Above 65 |
| All study area | −0.2% | 63.3% |
| Northern Europe | 13.8% | 61.9% |
| Western Europe | −1.7% | 54.0% |
| Eastern Europe | −14.8% | 68.4% |
| Southern Europe | 1.8% | 74.8% |
| Drivers | SSP2 | SSP1 | SSP3 |
|---|---|---|---|
| Population | Medium | Low | Low |
| Age-structure | Larger proportion of elderly | Smaller proportion of elderly | |
| Chronic disease prevalence | Higher, better care | Higher, poor care | |
| Urbanization | Medium | High | Low |
| Access to indoor cooling | Medium | High | Low |
| Urban planning | Continuation of historical patterns | Well managed | Poorly managed |
| Heatwave Early Warning System | Medium | High | Low |
| Societal participation | Medium | High | Low |
| Equity | Medium | High | Medium |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Åström, C.; Åström, D.O.; Andersson, C.; Ebi, K.L.; Forsberg, B. Vulnerability Reduction Needed to Maintain Current Burdens of Heat-Related Mortality in a Changing Climate—Magnitude and Determinants. Int. J. Environ. Res. Public Health 2017, 14, 741. https://doi.org/10.3390/ijerph14070741
Åström C, Åström DO, Andersson C, Ebi KL, Forsberg B. Vulnerability Reduction Needed to Maintain Current Burdens of Heat-Related Mortality in a Changing Climate—Magnitude and Determinants. International Journal of Environmental Research and Public Health. 2017; 14(7):741. https://doi.org/10.3390/ijerph14070741
Chicago/Turabian StyleÅström, Christofer, Daniel Oudin Åström, Camilla Andersson, Kristie L. Ebi, and Bertil Forsberg. 2017. "Vulnerability Reduction Needed to Maintain Current Burdens of Heat-Related Mortality in a Changing Climate—Magnitude and Determinants" International Journal of Environmental Research and Public Health 14, no. 7: 741. https://doi.org/10.3390/ijerph14070741





