Effectiveness of a Video-Versus Text-Based Computer-Tailored Intervention for Obesity Prevention after One Year: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Computer-Tailored Intervention for Obesity Prevention
2.2. Design and Participants
2.3. Procedure
2.4. Measurements
2.5. Statistical Analysis
2.5.1. Handling of Missing Values
2.5.2. Mixed-Effects Modelling
2.5.3. Model Selection
3. Results
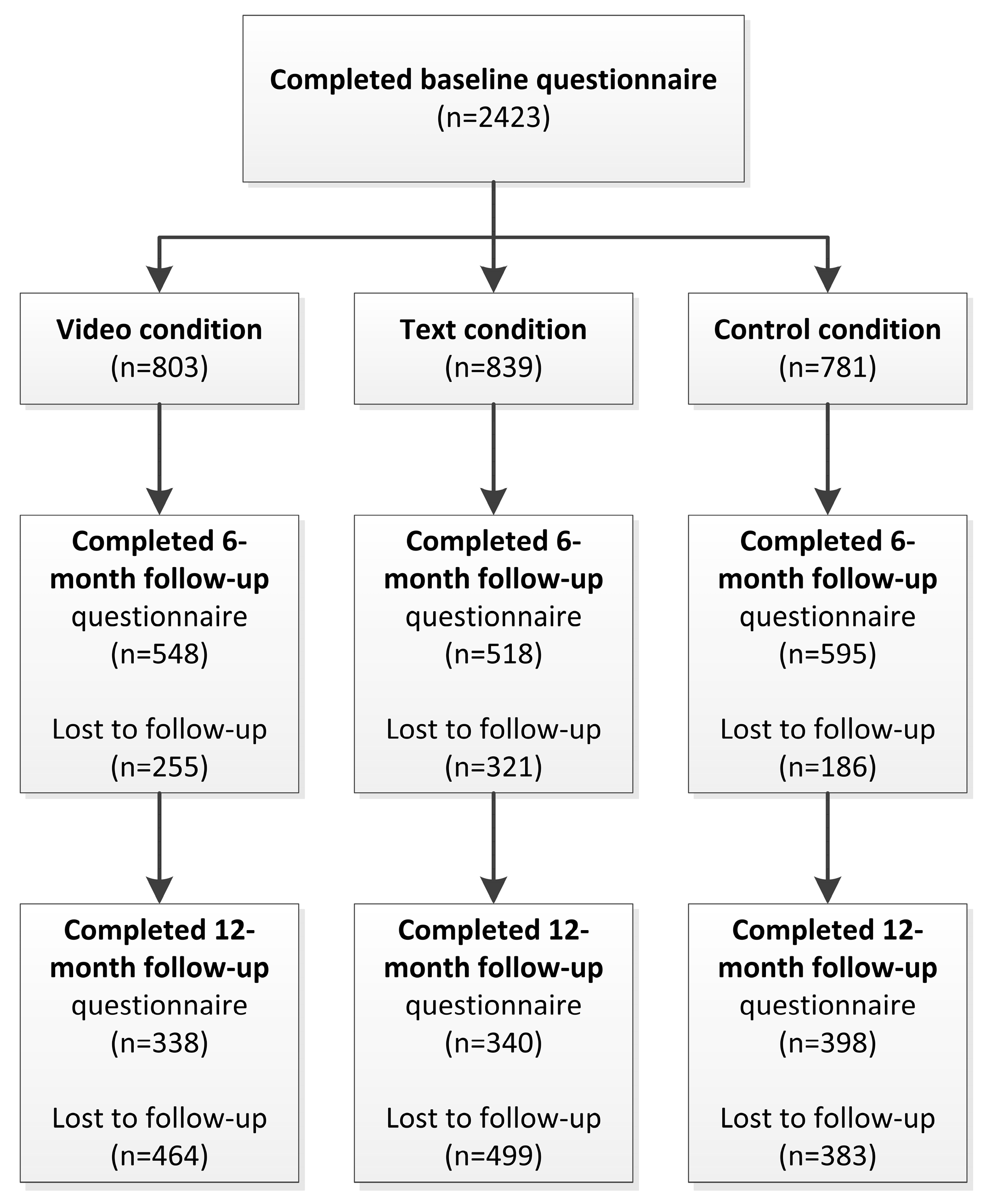
3.1. Study Sample and Attrition Analysis
3.2. Descriptive Statistics
3.3. Final Model
3.4. Intervention Effects on BMI and Physical Activity
3.5. Intervention Effects on Energy Intake
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Havelock, R.G. The utilisation of educational research and development. Br. J. Educ. Technol. 1971, 2, 84–98. [Google Scholar] [CrossRef]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F. 2013 aha/acc/tos guideline for the management of overweight and obesity in adults. Circulation 2014, 129, S102–S138. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. The Economics of Tobacco and Tobacco Control. 2016. Available online: Https://cancercontrol.Cancer.Gov/brp/tcrb/monographs/21/docs/m21_exec_sum.Pdf (accessed on 27 January 2017).
- Trimbos Instituut. Nationale Drug Monitor. 2016. Available online: Https://assets.Trimbos.Nl/docs/3fdeab39-f34e-4aa0–97af-5dbf111c05a0.Pdf (accessed on 27 January 2017).
- Civljak, M.; Sheikh, A.; Stead, L.F.; Car, J. Internet-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2013, 10, CD007078. [Google Scholar]
- Devaux, M.; Sassi, F. Social inequalities in obesity and overweight in 11 Oecd countries. Eur. J. Public Health 2013, 23, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Roskam, A.-J.R.; Kunst, A.E.; Van Oyen, H.; Demarest, S.; Klumbiene, J.; Regidor, E.; Helmert, U.; Jusot, F.; Dzurova, D.; Mackenbach, J.P. Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. Int. J. Epidemiol. 2010, 39, 392–404. [Google Scholar] [CrossRef] [PubMed]
- Wieland, L.S.; Falzon, L.; Sciamanna, C.N.; Trudeau, K.J.; Brodney, S.; Schwartz, J.E.; Davidson, K.W. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst. Rev. 2012, 8, CD007675. [Google Scholar]
- Hutchesson, M.; Rollo, M.; Krukowski, R.; Ells, L.; Harvey, J.; Morgan, P.; Callister, R.; Plotnikoff, R.; Collins, C. Ehealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 2015, 16, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, A.; De Vries, H. The development of computer-generated tailored interventions. Patient Educ. Couns. 1999, 36, 193–203. [Google Scholar] [CrossRef]
- Krebs, P.; Prochaska, J.O.; Rossi, J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev. Med. 2010, 51, 214–221. [Google Scholar] [CrossRef] [PubMed]
- De Vries, H.; Brug, J. Computer-tailored interventions motivating people to adopt health promoting behaviours: Introduction to a new approach. Patient Educ. Couns. 1999, 36, 99–105. [Google Scholar] [PubMed]
- Swartz, L.; Noell, J.; Schroeder, S.; Ary, D. A randomised control study of a fully automated internet based smoking cessation programme. Tob. Control 2006, 15, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Reinwand, D.A.; Schulz, D.N.; Crutzen, R.; Kremers, S.P.; de Vries, H. Who follows ehealth interventions as recommended? A study of participants’ personal characteristics from the experimental arm of a randomized controlled trial. J. Med. Internet Res. 2015, 17, e115. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, W.; Kroeze, W.; Crutzen, R.; de Nooijer, J.; de Vries, N.K.; Brug, J.; Oenema, A. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J. Med. Internet Res. 2011, 13, e2. [Google Scholar] [CrossRef] [PubMed]
- Walthouwer, M.J.L.; Oenema, A.; Soetens, K.; Lechner, L.; De Vries, H. Systematic development of a text-driven and a video-driven web-based computer-tailored obesity prevention intervention. BMC Public Health 2013, 13, 978. [Google Scholar] [CrossRef] [PubMed]
- Magnée, T.; Burdorf, A.; Brug, J.; Kremers, S.P.; Oenema, A.; van Assema, P.; Ezendam, N.P.; van Genugten, L.; Hendriksen, I.J.; Hopman-Rock, M. Equity-specific effects of 26 dutch obesity-related lifestyle interventions. Am. J. Prev. Med. 2013, 44, e61–e70. [Google Scholar] [CrossRef] [PubMed]
- Petty, R.; Cacioppo, J. Communication and Persuasion: Central and Peripheral Routes to Attitude Change; Springer Science and Business Media: Berlin, Germany, 2012. [Google Scholar]
- Sweller, J. Cognitive load theory, learning difficulty, and instructional design. Learn. Instr. 1994, 4, 295–312. [Google Scholar] [CrossRef]
- Walthouwer, M.J.; Oenema, A.; Lechner, L.; de Vries, H. Comparing a video and text version of a web-based computer-tailored intervention for obesity prevention: A randomized controlled trial. J. Med. Internet Res. 2015, 17, e236. [Google Scholar] [CrossRef] [PubMed]
- Eldredge, L.K.B.; Markham, C.M.; Ruiter, R.A.; Kok, G.; Parcel, G.S. Planning Health Promotion Programs: An Intervention Mapping Approach; John Wiley and Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Zimmerman, B.J.; Boekarts, M.; Pintrich, P.; Zeidner, M. A Social Cognitive Perspective. In Handbook of Self-Regulation; Elsevier: Amsterdam, The Netherlands, 2000; Volume 13, pp. 695–716. [Google Scholar]
- Leventhal, H.; Leventhal, E.A.; Contrada, R.J. Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychol. Health 1998, 13, 717–733. [Google Scholar] [CrossRef]
- De Vries, H. An integrated approach for understanding health behavior; The i-change model as an example. Psychol. Behav. Sci. Int. J. 2017, 2, 555–585. [Google Scholar]
- Robroek, S.J.; van Lenthe, F.J.; van Empelen, P.; Burdorf, A. Determinants of participation in worksite health promotion programmes: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 26. [Google Scholar] [CrossRef] [PubMed]
- Van Assema, P.; Brug, J.; Ronda, G.; Steenhuis, I. The relative validity of a short dutch questionnaire as a means to categorize adults and adolescents to total and saturated fat intake. J. Hum. Nutr. Diet. 2001, 14, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Wendel-Vos, W.; Schuit, J. Squash: Short Questionnaire to Asses Health Enhancing Physical Activity; Rijksinstituut voor Volksgezondheid en Milieu (Netherlands Institute for Public Health and Environment): Bilthoven, The Netherlands, 2002; pp. 1–55. [Google Scholar]
- Team, R.D.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2008. [Google Scholar]
- Schwabe, I.; Boomsma, D.I.; Zeeuw, E.L.; Berg, S.M. A new approach to handle missing covariate data in twin research : With an application to educational achievement data. Behav. Genet. 2016, 46, 583–595. [Google Scholar] [CrossRef] [PubMed]
- Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011. [Google Scholar] [CrossRef]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis; John Wiley and Sons: Hoboken, NJ, USA, 2012; Volume 998. [Google Scholar]
- Nlme: Linear and Nonlinear Mixed Effects Models, R package Version 3.1-131. Available online: https://CRAN.R-project.org/package=nlme (accessed on 20 August 2017).
- Bollen, K.A.; Curran, P.J. Latent Curve Models: A Structural Equation Perspective; John Wiley and Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Lenth, R.V. Least-squares means: The R package lsmeans. J. Stat. Softw. 2016, 69, 1–33. [Google Scholar] [CrossRef]
- Murray, D.M.; Pirie, P.; Luepker, R.V.; Pallonen, U. Five-and six-year follow-up results from four seventh-grade smoking prevention strategies. J. Behav. Med. 1989, 12, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Soetens, K.C.; Vandelanotte, C.; de Vries, H.; Mummery, K.W. Using online computer tailoring to promote physical activity: A randomized trial of text, video, and combined intervention delivery modes. J. Health Commun. 2014, 19, 1377–1392. [Google Scholar] [CrossRef] [PubMed]
- Stanczyk, N.; de Vries, H.; Candel, M.; Muris, J.; Bolman, C. Effectiveness of video-versus text-based computer-tailored smoking cessation interventions among smokers after one year. Prev. Med. 2016, 82, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Kruger, J.; Blanck, H.M.; Gillespie, C. Dietary and physical activity behaviors among adults successful at weight loss maintenance. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Schulz, D.N.; Kremers, S.P.; Vandelanotte, C.; van Adrichem, M.J.; Schneider, F.; Candel, M.J.; de Vries, H. Effects of a web-based tailored multiple-lifestyle intervention for adults: A two-year randomized controlled trial comparing sequential and simultaneous delivery modes. J. Med. Internet Res. 2014, 16, e26. [Google Scholar] [CrossRef] [PubMed]
- Prentice, D.A.; Miller, D.T. When small effects are impressive. Psychol. Bull. 1992, 112, 160–164. [Google Scholar] [CrossRef]
- Hill, J.O. Can a small-changes approach help address the obesity epidemic? A report of the Joint Task Force of the American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. Am. J. Clin. Nutr. 2009, 89, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Lehnert, T.; Sonntag, D.; Konnopka, A.; Riedel-Heller, S.; König, H.H. The long-term cost-effectiveness of obesity prevention interventions: Systematic literature review. Obes. Rev. 2012, 13, 537–553. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, N. Self-reports: How the questions shape the answers. Am. Psychol. 1999, 54, 93. [Google Scholar] [CrossRef]
- Matthews, C.E.; Welk, G. Use of Self-Report Instruments to Assess Physical Activity. In Physical Activity Assessments for Health-Related Research; Human Kinetics: Champaign, IL, USA, 2002; pp. 107–123. [Google Scholar]
- Reinwand, D.A.; Crutzen, R.; Elfeddali, I.; Schneider, F.; Schulz, D.N.; Smit, E.S.; Stanczyk, N.E.; Tange, H.; Voncken-Brewster, V.; Walthouwer, M.J.L. Impact of educational level on study attrition and evaluation of web-based computer-tailored interventions: Results from seven randomized controlled trials. J. Med. Internet Res. 2015, 17, e228. [Google Scholar] [CrossRef] [PubMed]
| Variable | Video (n = 803) | Missing | Text (n = 839) | Missing | Control (n = 781) | Missing |
| Gender (male), n (%) | 338 (42.1%) | 0 | 360 (42.9%) | 0 | 316 (40.5%) | 0 |
| Educational level, n (%) | ||||||
| Low | 166 (20.7%) | 0 | 167 (19.9%) | 0 | 158 (20.2%) | 0 |
| Middle | 257 (32.0%) | 0 | 290 (34.6%) | 0 | 296 (37.9%) | 0 |
| High | 380 (47.3%) | 0 | 382 (45.5%) | 0 | 327 (41.9%) | 0 |
| Age, M (SE) | 48.27 (11.57) | 0 | 47.95 (11.36) | 1 | 48.63 (11.31) | 4 |
| Baseline | ||||||
| BMI, M (SE) | 29.77 (5.19) | 17 | 29.74 (5.12) | 16 | 29.32 (4.95) | 41 |
| Energy intake, M (SE) | 1384.11 (557.70) | 9 | 1351.46 (538.28) | 11 | 1320.59 (585.82) | 22 |
| Physical activity, M (SE) | 75.65 (81.96) | 0 | 76.23 (83.39) | 0 | 81.23 (91.22) | 0 |
| Six-month follow-up | ||||||
| BMI, M (SE) | 28.79 (5.09) | 262 | 28.70 (4.91) | 333 | 28.58 (4.75) | 205 |
| Energy intake, M (SE) | 1014.88 (445.03) | 621 | 990.25 (487.60) | 654 | 1189.77 (548.16) | 431 |
| Physical activity, M (SE) | 109.15 (101.32) | 621 | 115.32 (101.71) | 657 | 114.99 (116.51) | 439 |
| Twelve-month follow-up | ||||||
| BMI, M (SE) | 28.47 (5.17) | 466 | 28.22 (4.60) | 504 | 28.72 (5.09) | 388 |
| Energy intake, M (SE) | 1073.94 (414.50) | 598 | 1101.00 (424.41) | 622 | 1158.61 (435.78) | 488 |
| Physical activity, M (SE) | 91.89 (88.36) | 614 | 89.69 (84.61) | 632 | 102.24 (103.59) | 505 |
| Variable | B | SE | 95% CI (Lower) | 95% CI (Higher) | p-Value |
|---|---|---|---|---|---|
| Intercept | 2103.45 | 165.50 | 1777.59 | 2429.31 | 0.00 |
| Study condition | 136.18 | 70.95 | −3.33 | 275.68 | 0.06 |
| Time | −29.05 | 3.75 | −36.43 | −21.67 | 0.00 |
| Educational level | −49.46 | 27.42 | −103.38 | 4.45 | 0.07 |
| Gender | −271.71 | 44.82 | −359.93 | −183.49 | 0.00 |
| Age | −1.96 | 1.90 | −5.70 | 1.77 | 0.30 |
| Goal setting | −33.46 | 10.49 | −54.19 | −12.73 | 0.00 |
| BMI category | 79.03 | 76.97 | −72.14 | 230.20 | 0.31 |
| Condition * time | 3.88 | 1.64 | 0.66 | 7.10 | 0.02 |
| Condition * educational level | −8.63 | 12.19 | −32.58 | 15.32 | 0.48 |
| Condition * gender | −25.01 | 19.84 | −64.01 | 14.00 | 0.21 |
| Condition * age | −1.82 | 0.83 | −3.45 | −0.19 | 0.03 |
| Condition * BMI category | −68.37 | 74.73 | −215.12 | 78.39 | 0.36 |
| Contrast | LSM-diff | SE | p-Value |
|---|---|---|---|
| Baseline | |||
| Video vs. Control | 39.69 | 44.49 | 0.57 |
| Text vs. Control | 19.72 | 27.70 | 0.69 |
| 6-month follow-up | |||
| Video vs. Control | −205.40 | 52.38 | 0.00 |
| Text vs. Control | −198.44 | 40.54 | 0.00 |
| 12-month follow-up | |||
| Video vs. Control | −128.14 | 53.17 | 0.03 |
| Text vs. Control | −57.10 | 40.18 | 0.27 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheung, K.L.; Schwabe, I.; Walthouwer, M.J.L.; Oenema, A.; Lechner, L.; De Vries, H. Effectiveness of a Video-Versus Text-Based Computer-Tailored Intervention for Obesity Prevention after One Year: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2017, 14, 1275. https://doi.org/10.3390/ijerph14101275
Cheung KL, Schwabe I, Walthouwer MJL, Oenema A, Lechner L, De Vries H. Effectiveness of a Video-Versus Text-Based Computer-Tailored Intervention for Obesity Prevention after One Year: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2017; 14(10):1275. https://doi.org/10.3390/ijerph14101275
Chicago/Turabian StyleCheung, Kei Long, Inga Schwabe, Michel J. L. Walthouwer, Anke Oenema, Lilian Lechner, and Hein De Vries. 2017. "Effectiveness of a Video-Versus Text-Based Computer-Tailored Intervention for Obesity Prevention after One Year: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 14, no. 10: 1275. https://doi.org/10.3390/ijerph14101275





