Electronic Cigarettes on Hospital Campuses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Development
2.2. Participants
2.3. Demographic Measures
2.4. Data Analysis
3. Results
| Hospital Characteristics | Survey Responders (n = 75) | Non-Responders (n = 46) | p-Value * | |
|---|---|---|---|---|
| % (n) | % (n) | |||
| E-cigarette policy † | Yes | 81.3% (61) | 77.5% (31) | 0.62 |
| No | 18.7% (14) | 22.5% (9) | ||
| Hospital service type | General acute | 94.7% (71) | 93.5% (43) | 0.79 |
| Psychiatric | 5.3% (4) | 6.5% (3) | ||
| Type of ownership | For-profit | 10.7% (8) | 8.7% (4) | 0.72 |
| Not-for-profit | 61.3% (46) | 56.5% (26) | ||
| Federal government | 2.7% (2) | 4.4% (2) | ||
| Non-federal government | 25.3% (19) | 30.4% (14) | ||
| Setting | Urban | 52.0% (39) | 50.0% (23) | 0.83 |
| Rural | 48.0% (36) | 50.0% (23) | ||
| Bed size | Small: <100 beds | 34.7% (26) | 50.0% (23) | 0.14 |
| Medium: 100–299 beds | 42.7% (32) | 39.1% (18) | ||
| Large: >299 beds | 22.7% (17) | 10.9% (5) | ||
| AMA resident status | Teaching | 20.0% (15) | 8.7% (4) | 0.13 |
| Non-teaching | 80.0% (60) | 91.3% (42) | ||
3.1. Tobacco Use and Policies
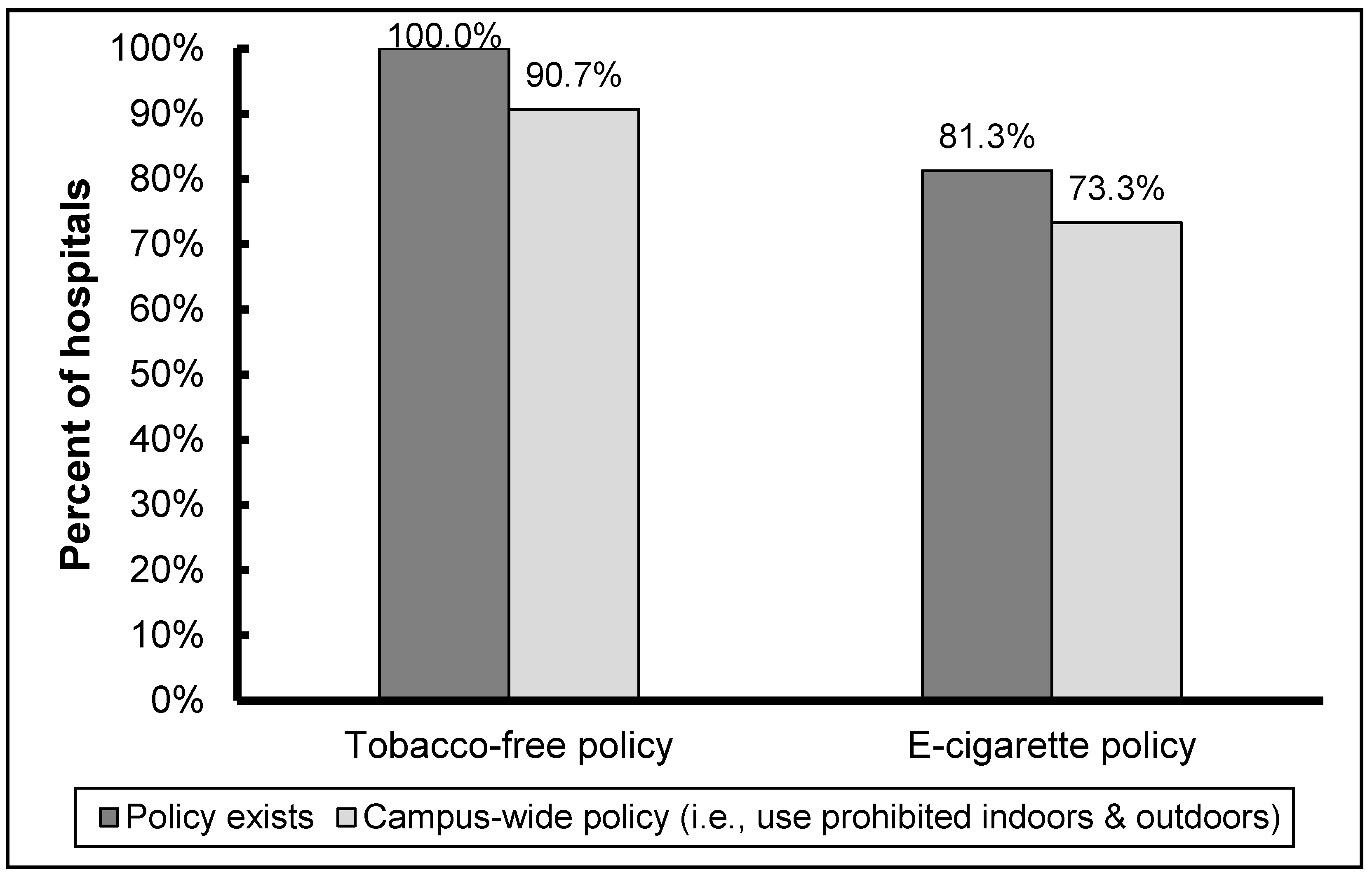
3.2. E-Cigarette Use and Policies
| Hospital Characteristics | Odds Ratio (95% Confidence Interval) | p-Value * | |
|---|---|---|---|
| Hospital service type † | Psychiatric | 4.13 (0.19–91.14) | 0.37 |
| General acute (ref.) | |||
| Type of ownership | Government | 0.52 (0.19–1.45) | 0.78 |
| For-profit | 0.36 (0.092–1.41) | 0.30 | |
| Not-for-profit (ref.) | |||
| Setting | Urban | 3.68 (1.331–0.19) | 0.01 |
| Rural (ref.) | |||
| Bed size | Small: <100 beds | 0.21 (0.03–1.78) | 0.31 |
| Medium: 100–299 beds | 0.17 (0.02–1.38) | 0.11 | |
| Large: >299 beds (ref.) | |||
| AMA resident status | Teaching | 2.21 (0.47–10.39) | 0.32 |
| Non-teaching (ref.) | |||
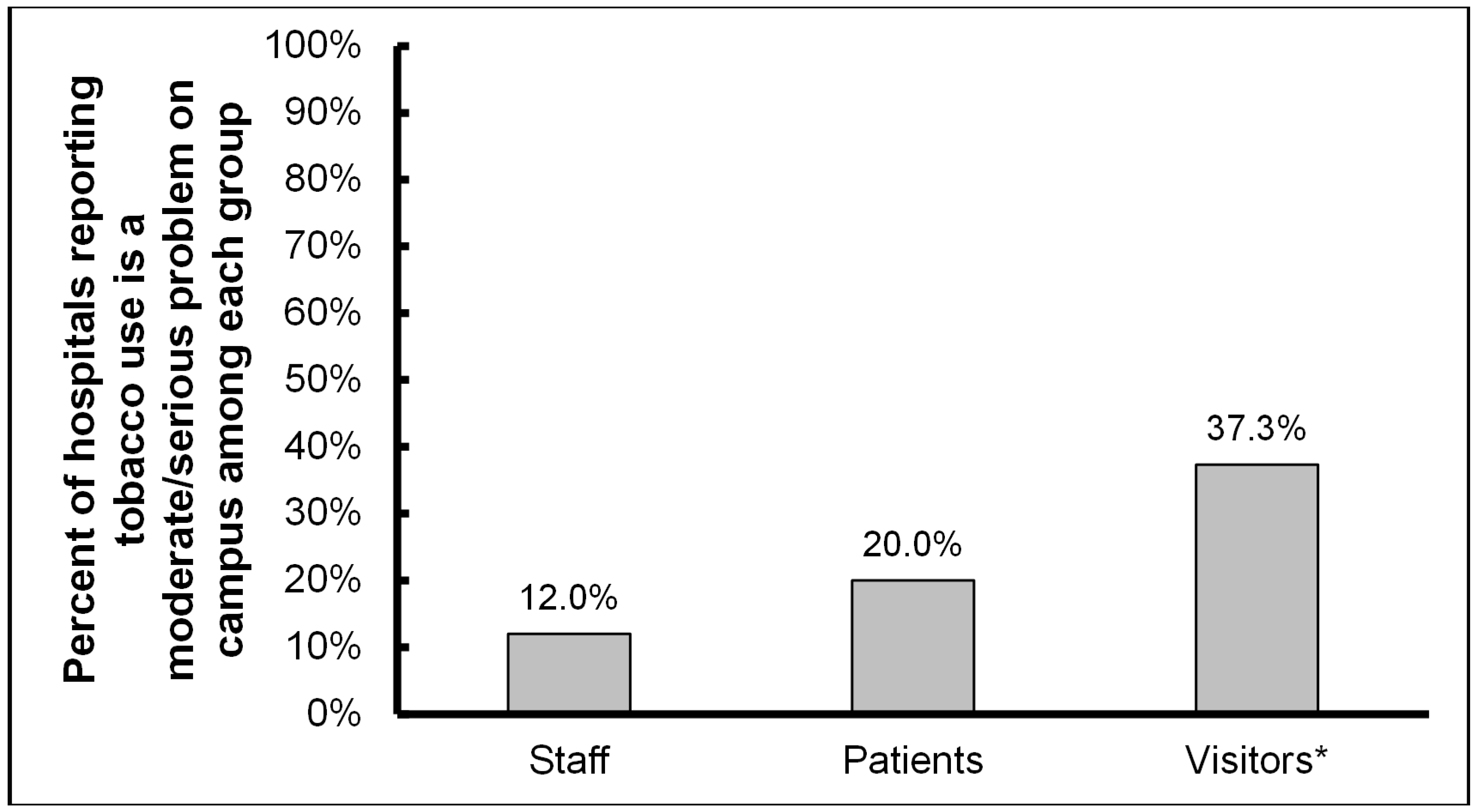
3.3. E-Cigarette Policy Implementation

3.4. E-Cigarette Policy Communication and Enforcement

4. Discussion
Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
References
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2011. Available online: http://www.who.int/tobacco/global_report/2011/en/ (accessed on 18 August 2015).
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General; Office on Smoking and Health, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, U.S. Department of Health and Human Services: Atlanta, GA, USA, 2014. Available online: http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf (accessed on 3 August 2015).
- U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General; Office on Smoking and Health, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, U.S. Department of Health and Human Services: Atlanta, GA, USA, 2006. Available online: http://www.surgeongeneral.gov/library/reports/secondhandsmoke/fullreport.pdf (accessed on 3 August 2015).
- Lee, J.G.L.; Goldstein, A.O.; Kramer, K.D.; Steiner, J.; Ezzell, M.M.; Shah, V. Statewide diffusion of 100% tobacco-free college and university policies. Tob. Control 2010, 19, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Azagba, S. Effect of smoke-free patio policy of restaurants and bars on exposure to second-hand smoke. Prev. Med. 2015, 76, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Ripley-Moffitt, C.; Viera, A.J.; Goldstein, A.O.; Steiner, J.B.; Kramer, K.D. Influence of a tobacco-free hospital campus policy on smoking status of hospital employees. Am. J. Health Promot. 2010, 25, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Osinubi, O.Y.; Sinha, S.; Rovner, E.; Perez-Lugo, M.; Jain, N.J.; Demissie, K.; Goldman, M. Efficacy of tobacco dependence treatment in the context of a “smoke-free grounds” worksite policy: A case study. Am. J. Ind. Med. 2004, 46, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Gajendra, S.; Ossip, D.J.; Panzer, R.J.; McInstosh, S. Implementing a smoke-free campus: A medical center initiative. J. Commun. Health 2011, 36, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Longo, D.R.; Brownson, R.C.; Johnson, J.C.; Hewett, J.E.; Kruse, R.L.; Novotny, T.E.; Logan, R.A. Hospital smoking bans and employee smoking behavior: Results of a national survey. JAMA 1996, 275, 1252–1257. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.O.; Westbrook, W.R.; Howell, R.E.; Fischer, P.M. Hospital efforts in smoking control: Remaining barriers and challenges. J. Fam. Pract. 1992, 34, 729–734. [Google Scholar] [PubMed]
- Brown, A.; Moodie, C.; Hastings, G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine Tob. Res. 2009, 11, 924–932. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M.; Stergachis, A.; Heaney, C. Evaluation of smoking prohibition policy in a health maintenance organization. Am. J. Public Health 1986, 76, 1014–1015. [Google Scholar] [CrossRef]
- Barker, A.F.; Moseley, J.R.; Glidewell, B.L. Components of a smoke-free hospital program. Arch. Intern. Med. 1989, 149, 1357–1359. [Google Scholar] [CrossRef] [PubMed]
- Longo, D.R.; Feldman, M.M.; Kruse, R.L.; Brownson, R.C.; Petroski, G.F.; Hewett, J.E. Implementing smoking bans in American hospitals: Results of a national survey. Tob. Control 1998, 7, 47–55. [Google Scholar] [CrossRef] [PubMed]
- ENSH. European Smoke-Free Hospital Network. Available online: http://www.ensh.org/ (accessed on 18 August 2015).
- Fernandez, E.; Martinez, C.; Alonso, B.; Chalom, D.; Dumont, J.; Gunning, M.; Mihaltan, F.; Riordan, A.; Rustler, C. Tobacco-Free Hospital Campuses in Europe. Available online: http://tobaccocontrol.bmj.com/content/18/6/451/reply#tobaccocontrol_el_3371 (accessed on 18 August 2015).
- Goldstein, A.O.; Steiner, J.; Mccullough, A.; Kramer, K.D.; Okun, M.F. State adoption of 100% smoke-free acute non federal hospital campus policies. Int. J. Environ. Res. Public Health 2009, 6, 2793–2799. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.C.; Hafner, J.M.; Morton, D.J.; Holm, A.L.; Milberger, S.M.; Koss, R.G.; Loeb, J.M. The adoption of smoke-free hospital campuses in the United States. Tob. Control 2009, 18, 451–458. [Google Scholar] [CrossRef] [PubMed]
- American Nonsmokers’ Rights Foundation. 100% Smokefree U.S. Hospitals and Psychiatric Facilities. Available online: http://www.no-smoke.org/pdf/smokefreehealthcare.pdf (accessed on 21 July 2015).
- Prochaska, J.J. Smoking and mental illness—Breaking the link. N. Engl. J. Med. 2011, 365, 196–198. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, G.; Schacht, L.; Lane, G.M. Smoking cessation care in state-operated or state-supported psychiatric hospitals: From policy to practice. Psychiatr. Ser. 2013, 64, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Irish Health Promoting Hospitals Network, Health Service Executive. Best Practice Guidelines for Tobacco Management in the Mental Health Setting, 2008. Available online: http://www.hse.ie/eng/services/publications/Mentalhealth/Tobacco_Management_in_the_Mental_Health_Setting_-_Feb_2008.pdf (accessed on 18 August 2015).
- Mermelstein, R.J. Adapting to a changing tobacco landscape: Research implications for understanding and reducing youth tobacco use. Am. J. Prev. Med. 2014, 47, S87–S89. [Google Scholar] [CrossRef] [PubMed]
- Euromonitor Research. Vapor Devices and e-Cigarettes in the Global Tobacco Market. Available online: http://blog.euromonitor.com/2015/06/vapor-devices-and-e-cigarettes-in-the-global-tobacco-market.html (accessed on 3 August 2015).
- Pepper, J.K.; Brewer, N.T. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: A systematic review. Tob. Control 2014, 23, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Adkison, S.E.; O’Connor, R.J.; Bansal-Travers, M.; Hyland, A.; Borland, R.; Yong, H.H.; Cummings, K.M.; McNeill, A.; Thrasher, J.F.; Hammond, D.; et al. Electronic nicotine delivery systems: International tobacco control four-country survey. Amer. J. Prev. Med. 2013, 44, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Pearson, J.L.; Richardson, A.; Niaura, R.S.; Vallone, D.M.; Abrams, D.B. E-cigarette awareness, use, and harm perceptions in U.S. adults. Am. J. Public Health 2012, 102, 1758–1766. [Google Scholar] [CrossRef] [PubMed]
- King, B.A.; Patel, R.; Nguyen, K.H.; Dube, S.R. Trends in awareness and use of electronic cigarettes among U.S. adults, 2010–2013. Nicotine Tob. Res. 2015, 17, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Kadowaki, J.; Vuolo, M.; Kelly, B.C. A review of the current geographic distribution of and debate surrounding electronic cigarette clean air regulations in the United States. Health Place 2015, 31, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.C.; Pluye, P.; Gore, G.; Granikov, V.; Filion, K.B.; Eisenberg, M.J. Regulation profiles of e-cigarettes in the United States: A critical review with qualitative synthesis. BMC Med. 2015, 13. [Google Scholar] [CrossRef] [PubMed]
- Marynak, K.; Holmes, C.B.; King, B.A.; Promoff, G.; Bunnell, R.; McAfee, T. State laws prohibiting sales to minors and indoor use of electronic nicotine delivery systems—United States, November 2014. MMWR 2014, 63, 1145–1150. [Google Scholar] [PubMed]
- Choi, K.; Fabian, L.; Mottey, N.; Corbett, A.; Forster, J. Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: Findings from a focus group study. Am. J. Public Health 2012, 102, 2088–2093. [Google Scholar] [CrossRef] [PubMed]
- Etter, J.F.; Bullen, C.; Flouris, A.D.; Laugesen, M.; Eissenberg, T. Electronic nicotine delivery systems: A research agenda. Tob. Control 2011, 20, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Bullen, C.; Howe, C.; Laugesen, M.; McRobbie, H.; Parag, V.; Williman, J.; Walker, N. Electronic cigarettes for smoking cessation: A randomised controlled trial. Lancet 2013, 382, 1629–1637. [Google Scholar] [CrossRef]
- Directive 2014/40/EU of the European Parliament and of the Council of 3 April 2014 on the Approximation of the Laws, Regulations and Administrative Provisions of the Member States Concerning the Manufacture, Presentation and Sale of Tobacco and Related Products and Repealing Directive 2001/37/EU. Available online: http://eur-lex.europa.eu/legal-content/EN/TXT/?qid=1399478051133&uri=OJ:JOL_2014_127_R_0001 (accessed on 18 August 2015).
- Gourdet, C.K.; Chriqui, J.F.; Chaloupka, F.J. A baseline understanding of state laws governing e-cigarettes. Tob. Control 2014, 23, 37–40. [Google Scholar]
- Food and Drug Administration. FDA Warns of Health Risks Posed by E-Cigarettes. Available online: http://www.fda.gov/downloads/ForConsumers/ConsumerUpdates/UCM173430.pdf (accessed on 3 August 2015).
- Food and Drug Administration. Deeming Tobacco Products to be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act. Regulations on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products; Proposed Rule, 79 FR 23141. Available online: http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/EconomicAnalyses/UCM394933.pdf (accessed on 3 August 2015).
- American Hospital Association Data Viewer. Available online: http://www.ahadataviewer.com/ (accessed on 15 July 2015).
- Blackwell, D.L.; Lucas, J.W.; Clarke, T.C. Summary health statistics for U.S. adults: National health interview survey, 2012. Vital Health Stat. 2014, 10, 1–161. [Google Scholar]
- Mckee, M. Electronic cigarettes: Proceed with great caution. Int. J. Public Health 2014, 59, 683–685. [Google Scholar] [CrossRef] [PubMed]
- Protano, C.; di Milia, L.M.; Orsi, G.B.; Vitali, M. Electronic cigarette: A threat or an opportunity for public health? State of the art and future perspectives. Clin. Ter. 2015, 166, 32–37. [Google Scholar] [PubMed]
- Schmitt, C.L.; Lee, Y.O.; Curry, L.E.; Farrelly, M.C.; Rogers, T. Research support for effective state and community tobacco control programme response to electronic nicotine delivery systems. Tob. Control 2014, 23, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.; Diehl, K. A public health strategy for e-cigarettes. Wien. Klin. Wochenschr. 2015, 127, 570–576. [Google Scholar] [CrossRef] [PubMed]
- WHO. Electronic Nicotine Delivery Systems. Available online: http://apps.who.int/gb/fctc/PDF/cop6/FCTC_COP6_10-en.pdf?ua=1 (accessed on 17 August 2015).
- Crowley, R.A. Electronic nicotine delivery systems: Executive summary of a policy position paper from the American College of Physicians. Ann. Intern. Med. 2015, 162, 583–584. [Google Scholar] [CrossRef] [PubMed]
- ENSH-Global Network for Tobacco Free Health Care Services and the International Network of Health Promoting Hospitals and Health Services. E-Cigarette Declaration. May 2015. Available online: http://www.ensh.org/news.php?id=191(accessed on 25 December 2015).
- American Nonsmokers’ Rights Foundation. States and Municipalities with Laws Regulating the Use of Electronic Cigarettes. Available online: http://www.no-smoke.org/pdf/ecigslaws.pdf (accessed on 3 August 2015).
- Smoke Free Partnership. SmokeFree Map. Available online: http://www.smokefreepartnership.eu/map/index.html (accessed on 18 August 2015).
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meernik, C.; Baker, H.M.; Paci, K.; Fischer-Brown, I.; Dunlap, D.; Goldstein, A.O. Electronic Cigarettes on Hospital Campuses. Int. J. Environ. Res. Public Health 2016, 13, 87. https://doi.org/10.3390/ijerph13010087
Meernik C, Baker HM, Paci K, Fischer-Brown I, Dunlap D, Goldstein AO. Electronic Cigarettes on Hospital Campuses. International Journal of Environmental Research and Public Health. 2016; 13(1):87. https://doi.org/10.3390/ijerph13010087
Chicago/Turabian StyleMeernik, Clare, Hannah M. Baker, Karina Paci, Isaiah Fischer-Brown, Daniel Dunlap, and Adam O. Goldstein. 2016. "Electronic Cigarettes on Hospital Campuses" International Journal of Environmental Research and Public Health 13, no. 1: 87. https://doi.org/10.3390/ijerph13010087





