In-situ Real-Time Monitoring of Volatile Organic Compound Exposure and Heart Rate Variability for Patients with Multiple Chemical Sensitivity
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Design
2.2. Subjects
2.3. VOC Monitoring
2.4. HRV Analysis
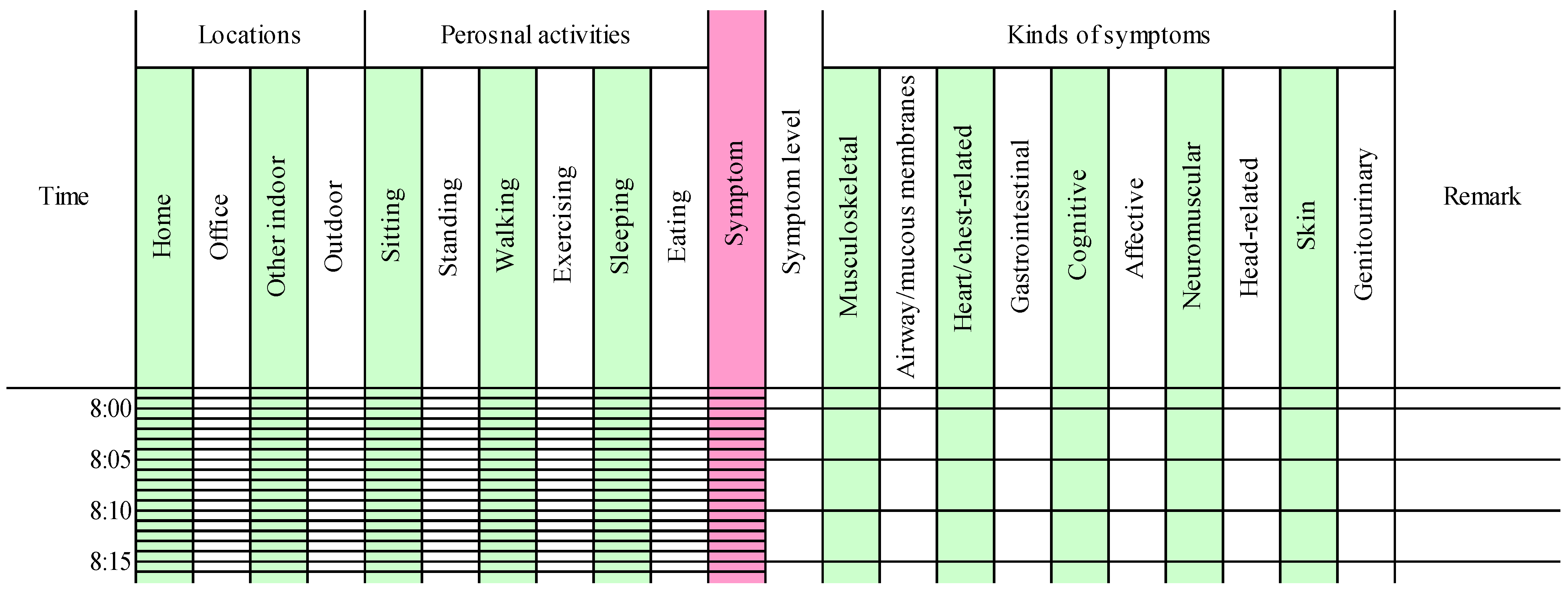
2.5. Time-Activity Pattern
2.6 Statistical Analysis
3. Results
3.1. Statistical Summary
| Parameters | Patients | Controls c | p d | ||
|---|---|---|---|---|---|
| n a | Mean ± SD b | n | Mean ± SD | ||
| VOC exposure concentration (µg·m−3) | |||||
| Total | 8 | 306 ± 148 | 7 | 176 ± 130 | 0.12 |
| Home | 8 | 262 ± 204 | 7 | 299 ± 267 | 1.00 |
| HRV parameters | |||||
| Log10HF (m·sec2) | 8 | 1.5 ± 0.2 | 7 | 1.7 ± 0.4 | 0.34 |
| LF/HF | 8 | 3.8 ± 1.9 | 7 | 3.8 ± 2.2 e | 1.00 |
3.2. Bivariate Analysis
| Parameters | Subject | − d | + e | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | |||
| Sex (M: male, F: female) | M | F | F | F | M | M | F | F | ||
| Age (years) | 39 | 62 | 33 | 46 | 31 | 49 | 35 | 54 | ||
| VOC vs. HF | −0.35 ** a | 0.19 * | −0.03 | −0.00 | −0.34 ** | −0.04 | 0.06 | −0.13 | 6 (2) | 2 (1) |
| ΔVOC vs. HF | −0.38 ** | 0.01 | 0.11 | −0.32 ** | 0.07 | −0.03 | −0.24 * | −0.30 ** | 5 (4) | 3 (0) |
| d+VOC vs. HF | −0.46 ** | −0.17 | 0.13 | −0.37 * | 0.02 | 0.04 | −0.38 * | −0.45 ** | 5 (4) | 3 (0) |
| d−VOC vs. HF | 0.31 * b | −0.08 | 0.09 | 0.45 ** | 0.30 ** | 0.39 ** | 0.15 | 0.34 ** | 1 (0) | 7 (5) |
| VOC vs. LF/HF | 0.06 | −0.22 * | 0.01 | −0.16 | 0.26 ** | −0.04 | −0.06 | 0.01 | 4 (1) | 4 (1) |
| ΔVOC vs. LF/HF | 0.08 | 0.11 | 0.02 | 0.28 ** | −0.09 | −0.08 | 0.29 ** | 0.04 | 2 (0) | 6 (2) |
| d+VOC vs. LF/HF | 0.04 | 0.10 | 0.27 | 0.45 ** | 0.04 | −0.18 | 0.27 | 0.12 | 1 (0) | 7 (1) |
| d−VOC vs. LF/HF | 0.13 | −0.21 | −0.13 | −0.33 * | −0.27 ** | −0.30 * | −0.21 | −0.08 | 7 (3) | 1 (0) |
| Temp vs. HF | −0.01 | 0.38 ** | −0.07 | 0.13 | - c | 0.15 | 0.21 * | −0.40 ** | 3 (1) | 4 (2) |
| RH vs. HF | 0.10 | −0.61 ** | 0.15 | 0.18 | - | −0.21 * | 0.16 | 0.38 ** | 2 (2) | 5 (1) |
| Temp vs. LF/HF | 0.20 * | −0.12 | −0.02 | −0.03 | - | −0.04 | −0.12 | 0.09 | 5 (0) | 2 (1) |
| RH vs. LF/HF | −0.08 | −0.15 | −0.14 | −0.22 * | - | 0.18 | −0.20 * | −0.10 | 6 (2) | 1 (0) |
3.3. Characteristics of Subjective Symptoms
| Symptoms | Subject | |||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | |
| Symptom time | 2.7 | 9.8 | 4.8 | 0.8 | 2.8 | 0.3 | 2.4 | 2.1 |
| Musculoskeletal | 0 | 8 | 0 | 0 | 52 | 0 | 0 | 4 |
| Airway/mucous membranes | 94 | 84 | 7 | 22 | 3 | 75 | 97 | 84 |
| Heart/chest-related | 0 | 84 | 24 | 44 | 0 | 25 | 17 | 92 |
| Gastrointestinal | 0 | 5 | 40 | 22 | 3 | 0 | 0 | 4 |
| Cognitive | 0 | 81 | 5 | 0 | 0 | 0 | 31 | 84 |
| Affective | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 4 |
| Neuromuscular | 91 | 92 | 10 | 0 | 0 | 0 | 0 | 12 |
| Head-related | 94 | 92 | 43 | 0 | 18 | 0 | 0 | 0 |
| Skin | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 64 |
| Genitourinary | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 |

3.4. Comparison between Subjective Symptom Time and Normal Time
| Parameters | Subject | ↓ f | ↑ g | ||||||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | G | H | |||
| VOC | ↓ a | ↑ ** | ↓ | ↑ | ↑ * | ↑ | ↑ | 2 (0) | 5 (2) |
| ΔVOC | ↑ b | ↑ | ↑ | ↓ | ↑ * | ↑ | ↓ | 2 (0) | 5 (1) |
| HF | ↓ ** c | ↓ ** | ↓ ** | ↓ | ↑ ** | ↑ | ↓ | 5 (3) | 2 (1) |
| LF/HF | ↑ * d | ↓ | ↑ ** | ↑ | ↓ | ↓ | ↓ | 4 (0) | 3 (2) |
| Temp | ↓ | ↓ | ↑ * | ↓ | - e | ↓ ** | ↓ ** | 5 (2) | 1 (1) |
| RH | ↑ ** | ↑ ** | ↑ | ↑ | - | ↑ * | ↑ * | 0 (0) | 6 (4) |
4. Discussion
4.1. Comparisons of VOC Exposure and HRV Parameters between Patients and Controls
4.2. Correlations between VOC Exposure and HRV Parameters
4.3. Comparison between Subjective Symptom Time and Normal Time
4.4. Case Studies
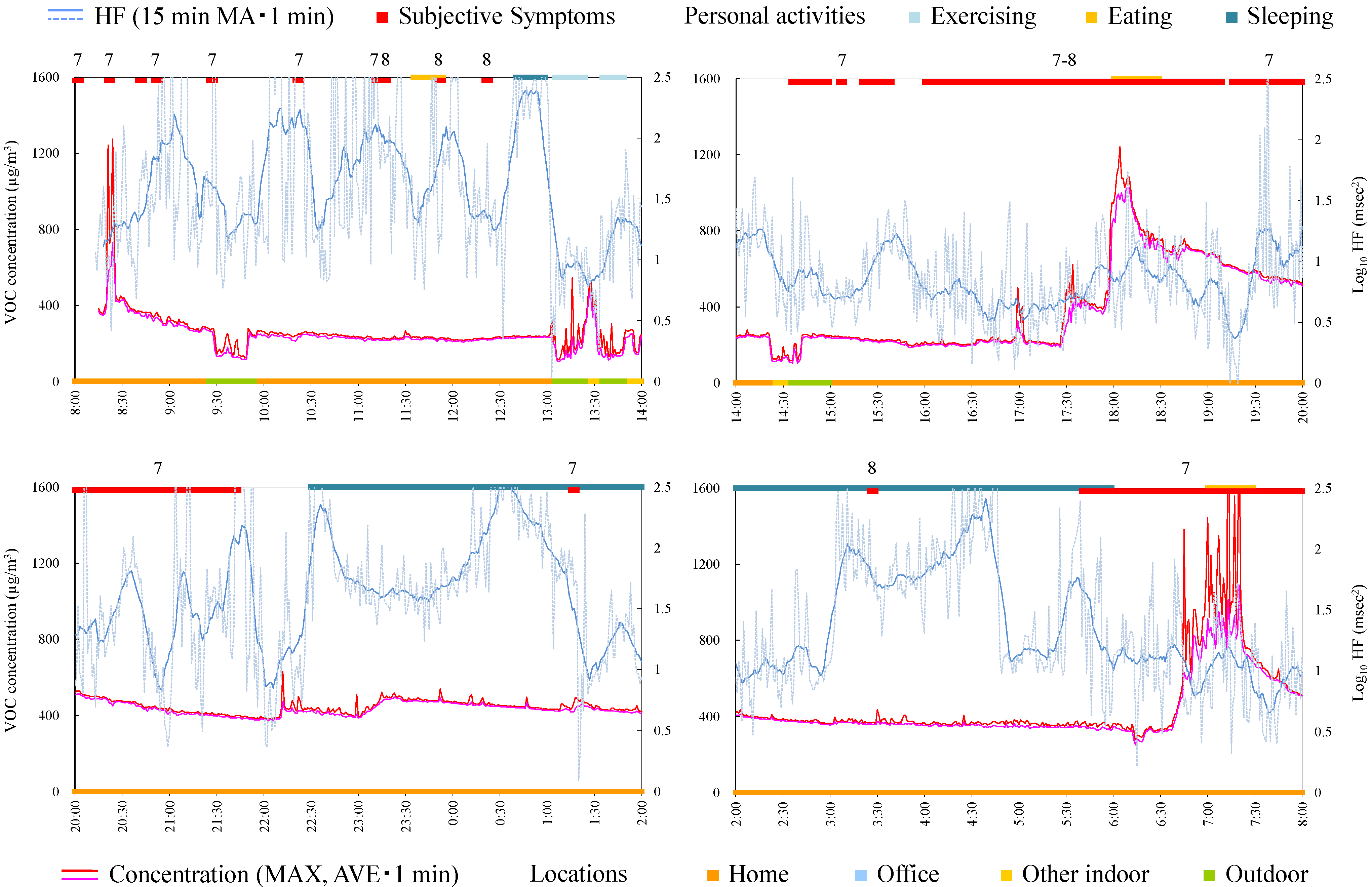
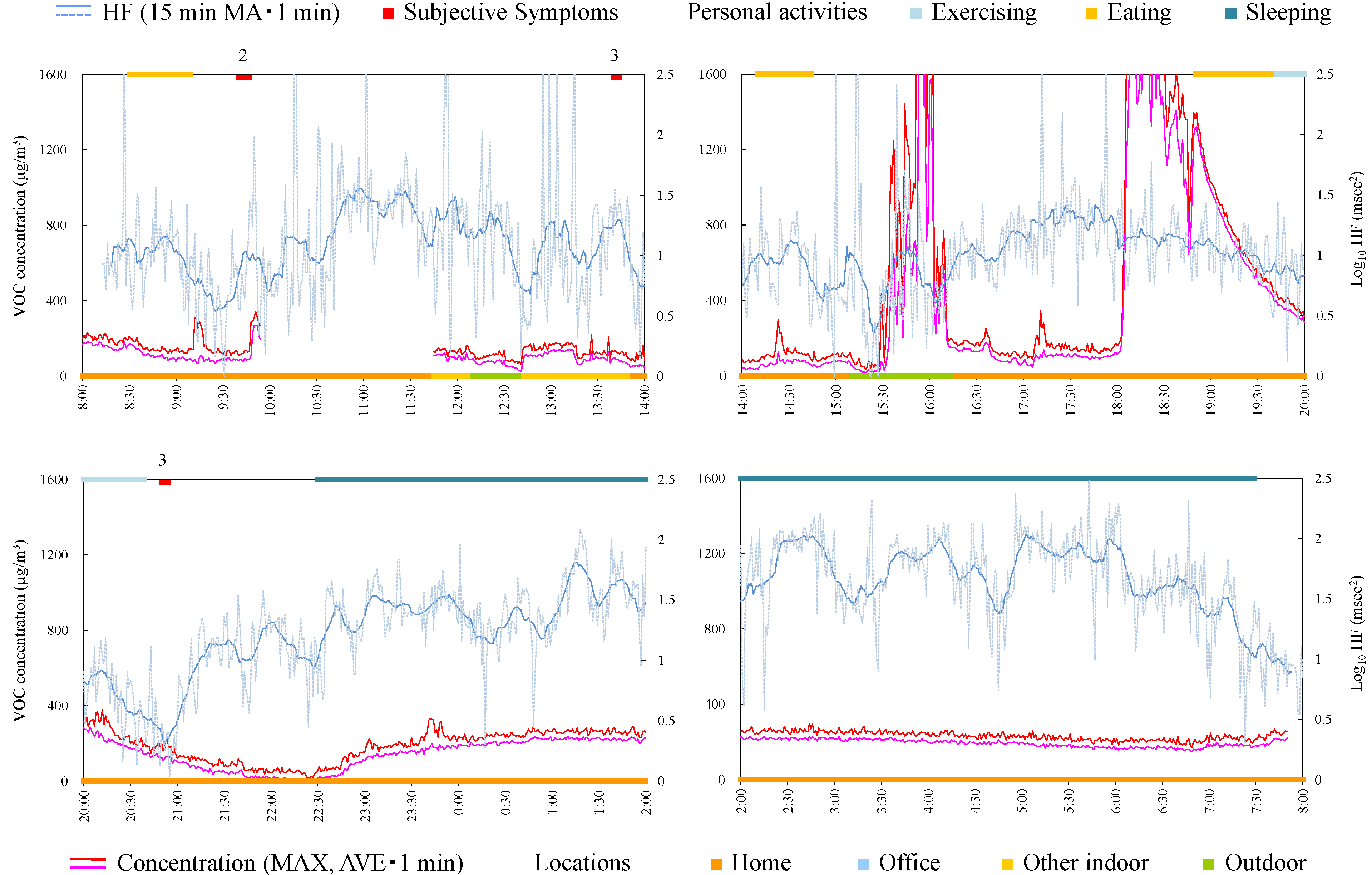
4.4.1. Subject A

4.4.2. Subject B
4.4.3. Subject C

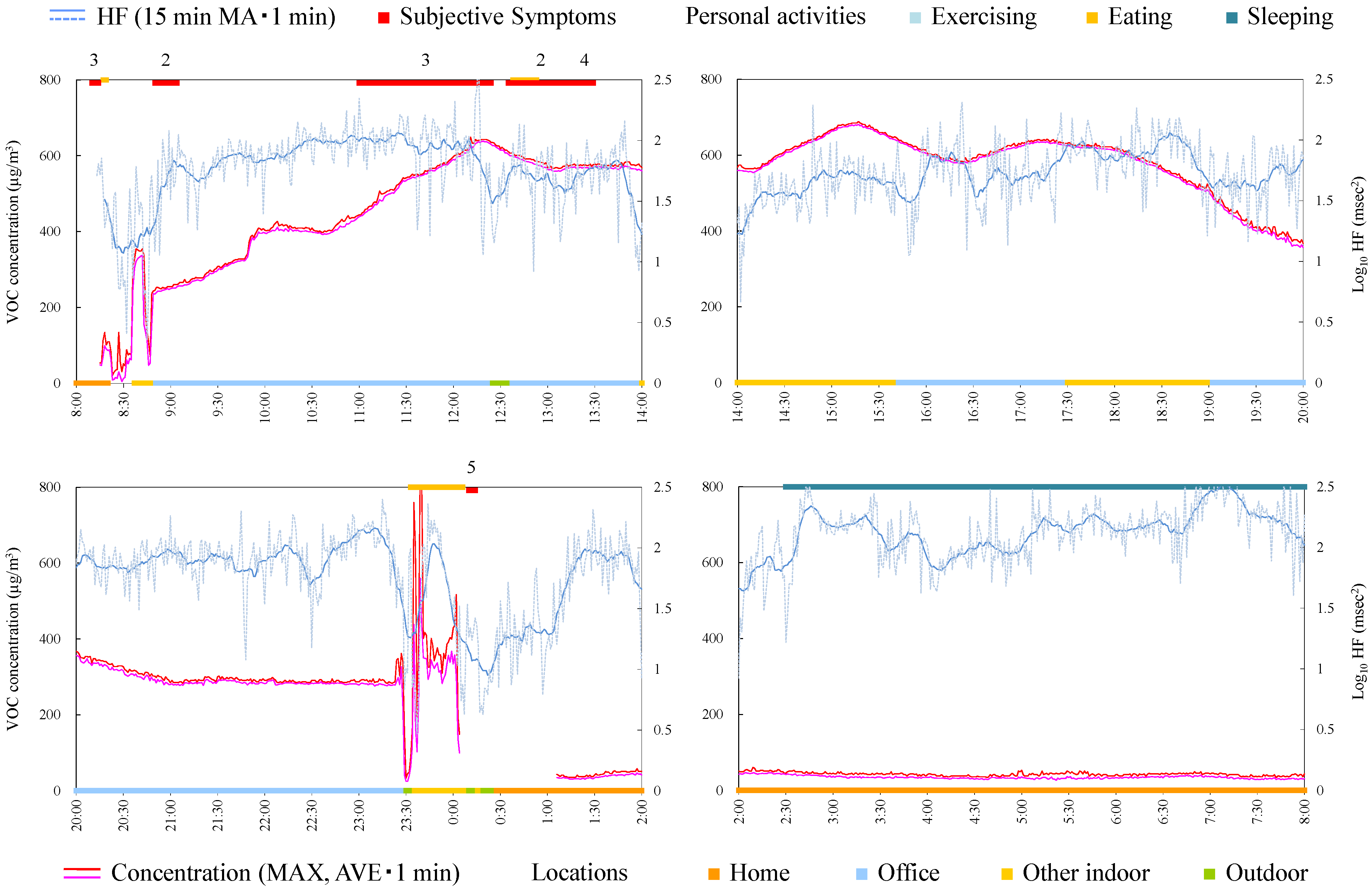
4.4.4. Subject D
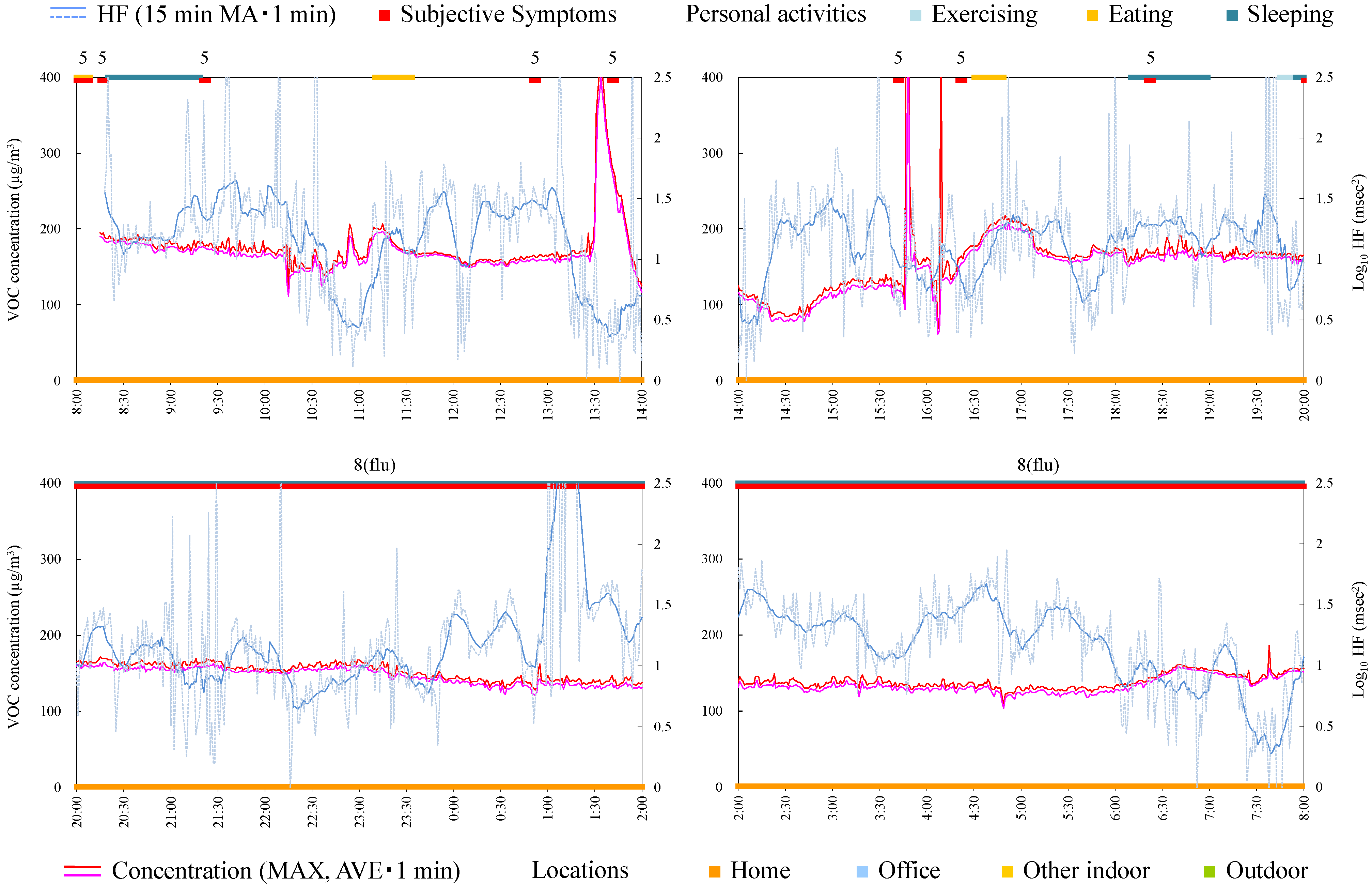
4.4.5. Subject E
4.4.6. Subject F
4.4.7. Subject G

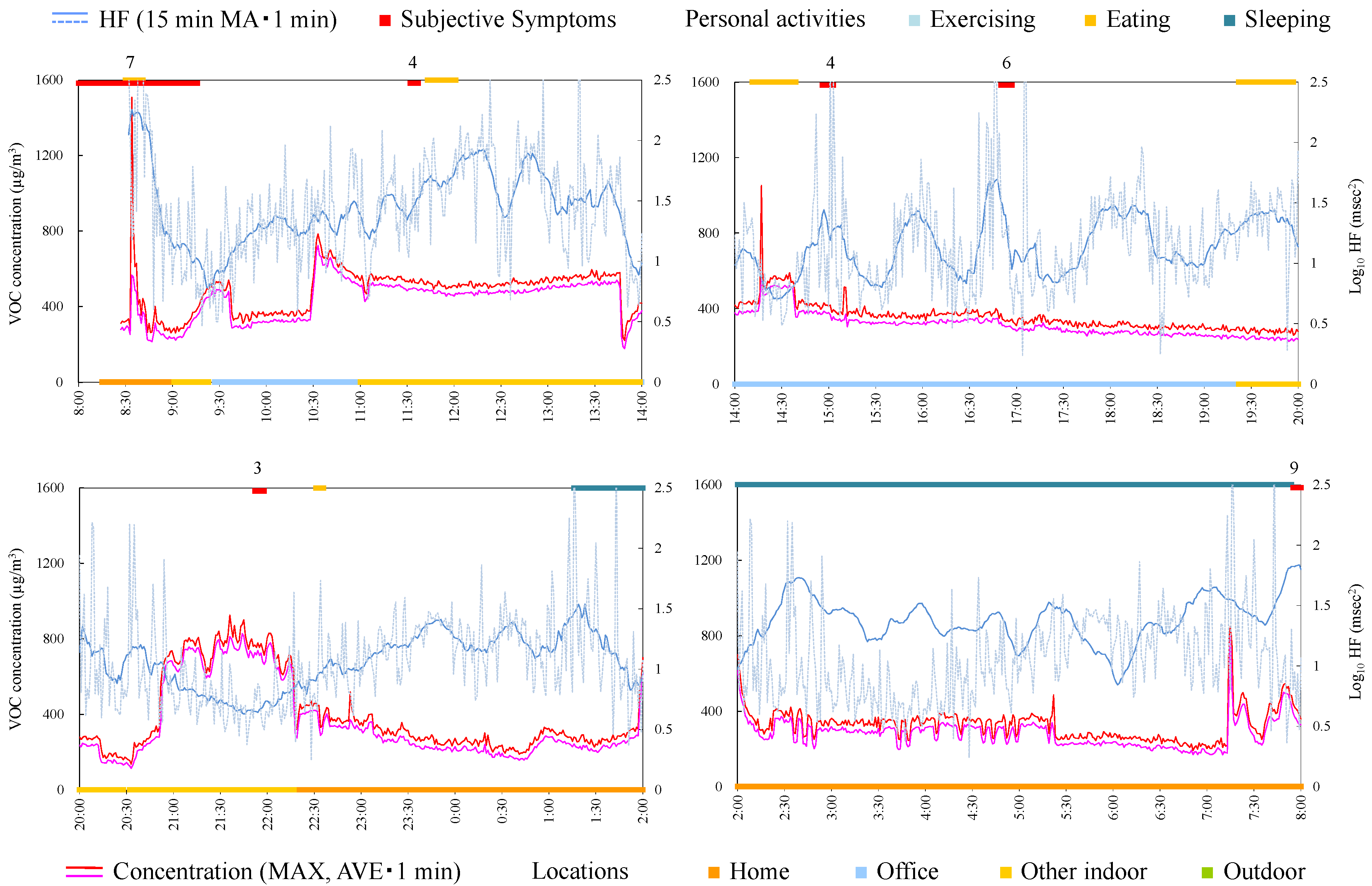
4.4.8. Subject H
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Cullen, M.R. The worker with multiple chemical sensitivities: An overview. Occup. Med. 1987, 2, 655–661. [Google Scholar] [PubMed]
- McCready, P. Multiple chemical sensitivity: A 1999 consensus. Arch. Environ. Health 1999, 54, 147–149. [Google Scholar]
- Das-Munshi, J.; Rubin, G.J.; Wessely, S. Multiple chemical sensitivities: A systematic review of provocation studies. J. Allergy Clin. Immunol. 2006, 118, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.S. Chemical sensitivity: Symptom, syndrome or mechanism for disease? Toxicology 1996, 111, 69–86. [Google Scholar] [CrossRef]
- Shinohara, N.; Mizukoshi, A.; Yanagisawa, Y. Identification of responsible volatile chemicals that induce hypersensitive reactions to multiple chemical sensitivity patients. J. Expo. Anal. Environ. Epidemiol. 2004, 14, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Kumano, H.; Yoshiuchi, K.; Kokubo, N.; Ohashi, K.; Yamamoto, Y.; Shinohara, N.; Yanagisawa, Y.; Sakabe, K.; Miyata, M.; et al. Symptom profile of multiple chemical sensitivity in actual life. Psychosom. Med. 2005, 67, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Coy, J.D.; Bigelow, P.L.; Buchan, R.M.; Tessari, J.D.; Parnell, J.O. Field evaluation of a portable photoionization detector for assessing exposure to solvent mixtures. AIHAJ 2000, 61, 268–274. [Google Scholar] [CrossRef]
- Oka, K.; Iizuka, A.; Inoue, Y.; Mizukoshi, A.; Noguchi, M.; Yamasaki, A.; Yanagisawa, Y. Development of a combined real time monitoring and integration analysis system for volatile organic compounds (VOCs). Int. J. Environ. Res. Public Health 2010, 7, 4100–4110. [Google Scholar] [CrossRef] [PubMed]
- Hori, H.; Ishimatsu, S.; Fueta, Y.; Ishidao, T. Evaluation of a real-time method for monitoring volatile organic compounds in indoor air in a Japanese university. Environ. Health Prev. Med. 2013, 18, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Liao, D.; Creason, J.; Shy, C.; Williams, R.; Watts, R.; Zweidinger, R. Daily variation of particulate air pollution and poor cardiac autonomic control in the elderly. Environ. Health Perspect. 1999, 107, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.C.; Chuang, K.J.; Shiao, G.M.; Lin, L.Y. Personal exposure to submicrometer particles and heart rate variability in human subjects. Environ. Health Perspect. 2004, 112, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Chuang, K.J.; Chan, C.C.; Chen, N.T.; Su, T.C.; Lin, L.Y. Effects of particle size fractions on reducing heart rate variability in cardiac and hypertensive patients. Environ. Health Perspect. 2005, 113, 1693–1697. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A., 3rd; Eatough, D.J.; Gold, D.R.; Pang, Y.; Nielsen, K.R.; Nath, P.; Verrier, R.L.; Kanner, R.E. Acute exposure to environmental tobacco smoke and heart rate variability. Environ. Health Perspect. 2001, 109, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Riojas-Rodriguez, H.; Escamilla-Cejudo, J.A.; Gonzalez-Hermosillo, J.A.; Tellez-Rojo, M.M.; Vallejo, M.; Santos-Burgoa, C.; Rojas-Bracho, L. Personal PM2.5 and CO exposures and heart rate variability in subjects with known ischemic heart disease in Mexico City. J. Expo. Sci. Environ. Epidemiol. 2006, 16, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Sandstrom, M.; Lyskov, E.; Hornsten, R.; Hansson Mild, K.; Wiklund, U.; Rask, P.; Klucharev, V.; Stenberg, B.; Bjerle, P. Holter ECG monitoring in patients with perceived electrical hypersensitivity. Int. J. Psychophysiol. 2003, 49, 227–235. [Google Scholar] [CrossRef]
- Weichenthal, S.; Kulka, R.; Belisle, P.; Joseph, L.; Dubeau, A.; Martin, C.; Wang, D.; Dales, R. Personal exposure to specific volatile organic compounds and acute changes in lung function and heart rate variability among urban cyclists. Environ. Res. 2012, 118, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Mehta, A.J.; Adam, M.; Schaffner, E.; Barthelemy, J.C.; Carballo, D.; Gaspoz, J.M.; Rochat, T.; Schindler, C.; Schwartz, J.; Zock, J.P.; et al. Heart rate variability in association with frequent use of household sprays and scented products in SAPALDIA. Environ. Health Perspect. 2012, 120, 958–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizukoshi, A.; Kumagai, K.; Yamamoto, N.; Noguchi, M.; Yoshiuchi, K.; Kumano, H.; Yanagisawa, Y. A novel methodology to evaluate health impacts caused by VOC exposures using real-time VOC and Holter monitors. Int. J. Environ. Res. Public Health 2010, 7, 4127–4138. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, S.; Miyata, M. Multiple Chemical Sensitivity: Criteria and test methods for diagnosis. Allergol. Immuol. 1999, 6, 990–998. [Google Scholar]
- Heart Rate Variability. Standards of Measurement, Physiological Interpretation, and Clinical Use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Available online: http://www.escardio.org/static_file/Escardio/Guidelines/Scientific-Statements/guidelines-Heart-Rate-Variability-FT-1996.pdf (accessed on 25 August 2015).
- Malliani, A.; Lombardi, F.; Pagani, M. Power spectrum analysis of heart rate variability: A tool to explore neural regulatory mechanisms. Br. Heart J. 1994, 71, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.S.; Prihoda, T.J. The Environmental Exposure and Sensitivity Inventory (EESI): A standardized approach for measuring chemical intolerances for research and clinical applications. Toxicol. Ind. Health 1999, 15, 370–385. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.S.; Prihoda, T.J. A controlled comparison of symptoms and chemical intolerances reported by Gulf War veterans, implant recipients and persons with multiple chemical sensitivity. Toxicol. Ind. Health 1999, 15, 386–397. [Google Scholar] [CrossRef] [PubMed]
- Caress, S.M.; Steinemann, A.C. A review of a two-phase population study of multiple chemical sensitivities. Environ. Health Perspect. 2003, 111, 1490–1497. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.R.; Elms, A.N.; Ruding, L.A. Perceived treatment efficacy for conventional and alternative therapies reported by persons with multiple chemical sensitivity. Environ. Health Perspect. 2003, 111, 1498–1504. [Google Scholar] [CrossRef] [PubMed]
- Sampalli, T.; Berlasso, E.; Fox, R.; Petter, M. A controlled study of the effect of a mindfulness-based stress reduction technique in women with multiple chemical sensitivity, chronic fatigue syndrome, and fibromyalgia. J. Multidiscip. Healthc. 2009, 2, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Hauge, C.R.; Bonde, P.J.; Rasmussen, A.; Skovbjerg, S. Mindfulness-based cognitive therapy for multiple chemical sensitivity: A study protocol for a randomized controlled trial. Trials 2012, 13. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.R.; Vogel, V.M. Sickness-related dysfunction in persons with self-reported multiple chemical sensitivity at four levels of severity. J. Clin. Nurs. 2009, 18, 72–81. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizukoshi, A.; Kumagai, K.; Yamamoto, N.; Noguchi, M.; Yoshiuchi, K.; Kumano, H.; Sakabe, K.; Yanagisawa, Y. In-situ Real-Time Monitoring of Volatile Organic Compound Exposure and Heart Rate Variability for Patients with Multiple Chemical Sensitivity. Int. J. Environ. Res. Public Health 2015, 12, 12446-12465. https://doi.org/10.3390/ijerph121012446
Mizukoshi A, Kumagai K, Yamamoto N, Noguchi M, Yoshiuchi K, Kumano H, Sakabe K, Yanagisawa Y. In-situ Real-Time Monitoring of Volatile Organic Compound Exposure and Heart Rate Variability for Patients with Multiple Chemical Sensitivity. International Journal of Environmental Research and Public Health. 2015; 12(10):12446-12465. https://doi.org/10.3390/ijerph121012446
Chicago/Turabian StyleMizukoshi, Atsushi, Kazukiyo Kumagai, Naomichi Yamamoto, Miyuki Noguchi, Kazuhiro Yoshiuchi, Hiroaki Kumano, Kou Sakabe, and Yukio Yanagisawa. 2015. "In-situ Real-Time Monitoring of Volatile Organic Compound Exposure and Heart Rate Variability for Patients with Multiple Chemical Sensitivity" International Journal of Environmental Research and Public Health 12, no. 10: 12446-12465. https://doi.org/10.3390/ijerph121012446





