A Review of Telehealth Service Implementation Frameworks
Abstract
:1. Introduction
2. Purpose
- (1)
- What are the common themes and formats used in these frameworks?
- (2)
- Which methodologies were followed to develop these frameworks? On which theories are they based? Which research methods were used to develop these frameworks? How are they validated? What are the areas for further research?
3. Methodology
| Search terms and database | Science Direct | IEEE | EBSCO Host | Scopus | ProQuest | PubMed |
|---|---|---|---|---|---|---|
| (telemedicine OR telehealth) AND implementation AND framework | 14 | 19 | 13 | 81 | 6 | 81 |
| (telemedicine OR telehealth) AND implementation AND model | 29 | 43 | 27 | 200 | 18 | 159 |
| (telemedicine OR telehealth) AND implementation AND guidelines | 4 | 5 | 8 | 62 | 4 | 59 |
- Section 5: Frameworks related to the diffusion of telemedicine
- Section 6: Frameworks related to ereadiness
- Section 7: Telehealth applications of the Unified Theory for the Acceptance of Technology
- Section 8: Guidelines that are not based on a particular theory, but retrospectively on the implementation of some telehealth services
- Section 10: Frameworks that incorporate the lifecycle phases of a telehealth service
| Framework | Underlying Theory | Research and Development Methods | Validation Methods | Framework Format | Main Themes | |
|---|---|---|---|---|---|---|
| 5 | Barriers to the diffusion of telemedicine | Diffusion of Innovation [12] | A longitudinal study of three telehealth programs. | No formal validation | Four so-called barriers diffusion of telehealth services. | technological, organizational, behavioral and economic barriers |
| 6 | eHealth readiness assessment tools | Theories on ereadiness and change management | Adaption of existing ereadiness scales based on input from ehealth experts. | Expert interviews, as well as statistical reliability testing of questionnaire results [13] | A set of questionnaires, including 51 statements linked to a Likert scale. | technology, learning, society, economical, policy |
| 7 | Unified Theory of Acceptance and Use of Technology (UTAUT) applied to telehealth [14,15] | Unified Theory of Acceptance and Use of Technology (UTAUT) | UTAUT questionnaire administered with specific reference to telehealth. | UTAUT questionnaire validated through other studies; telehealth application validate by experts. | A list of statements linked to a Likert scale. | technology perceived usefulness, perceived ease of use, behavioral intent, demographic factors |
| 8.1 | Seven Core Principles for the Successful Development of Telemedicine Systems | No particular theory | Literature and personal experience of setting up three telehealth services in Australia. | No formal validation. | Guidelines structured according to seven principles. | ownership, bottom-up support, user-friendliness of technology, training, dissemination of evidence |
| 8.2 | Lessons in telemedicine service innovation | No particular theory | Longitudinal qualitative study; data gathered by means of questionnaires. | No formal validation | Guidelines structured according to 5 lessons. | policy, evidence, perceived benefit, commitment, service design, professional roles and border crossing |
| 8.3 | Framework for Assessing the Health System Challenges to Scaling up mHealth | ICT for health in developing countries Khoja et al. [16] Bukachi and Pakenham-Walsh [17] | Qualitative study, combination of reviews with key informants, site visits to local projects and documented reviews. | No formal validation | Four dimensions, each with a collection of capatiy requirements. | government, organization, technology, finances. |
| 9 | Comprehensive Model for the Evaluation of Telemedicine | Theories of Transactional Economics [18] | Design and integration of three evaluation dimensions. | No formal validation | A three-dimensional framework; each dimension has several categories. | individual, community, society, cost, quality, access. |
| 10.1 | The Layered Telemedicine Implementation Model | Knowledge barriers to the diffusion of telemedicine Tanriverdi and Iacono [19] | Systematic literature review of 45 articles on the implementation of telemedicine services. | No formal validation | 5 lifecycle phases, each of a collection of determinants for success. | technology, acceptance, organization, policy and legislation |
| 10.2 | The Khoja– Durrani–Scott (KDS) Evaluation Framework | Concepts and theories related to the evaluation of ehealth (no mention of which) as well as system lifecycle theories | Systematic literature review and expert opinions. | Validation to be published in another paper | A list of desired outcomes per lifecycle phase per theme; each outcome linked to a Likert-like scale. | evidence, technology, economic, behavioral and sociotechnical, thical, change management, policy |
4. eHealth, Telehealth, Telemedicine, Telecare and mHealth
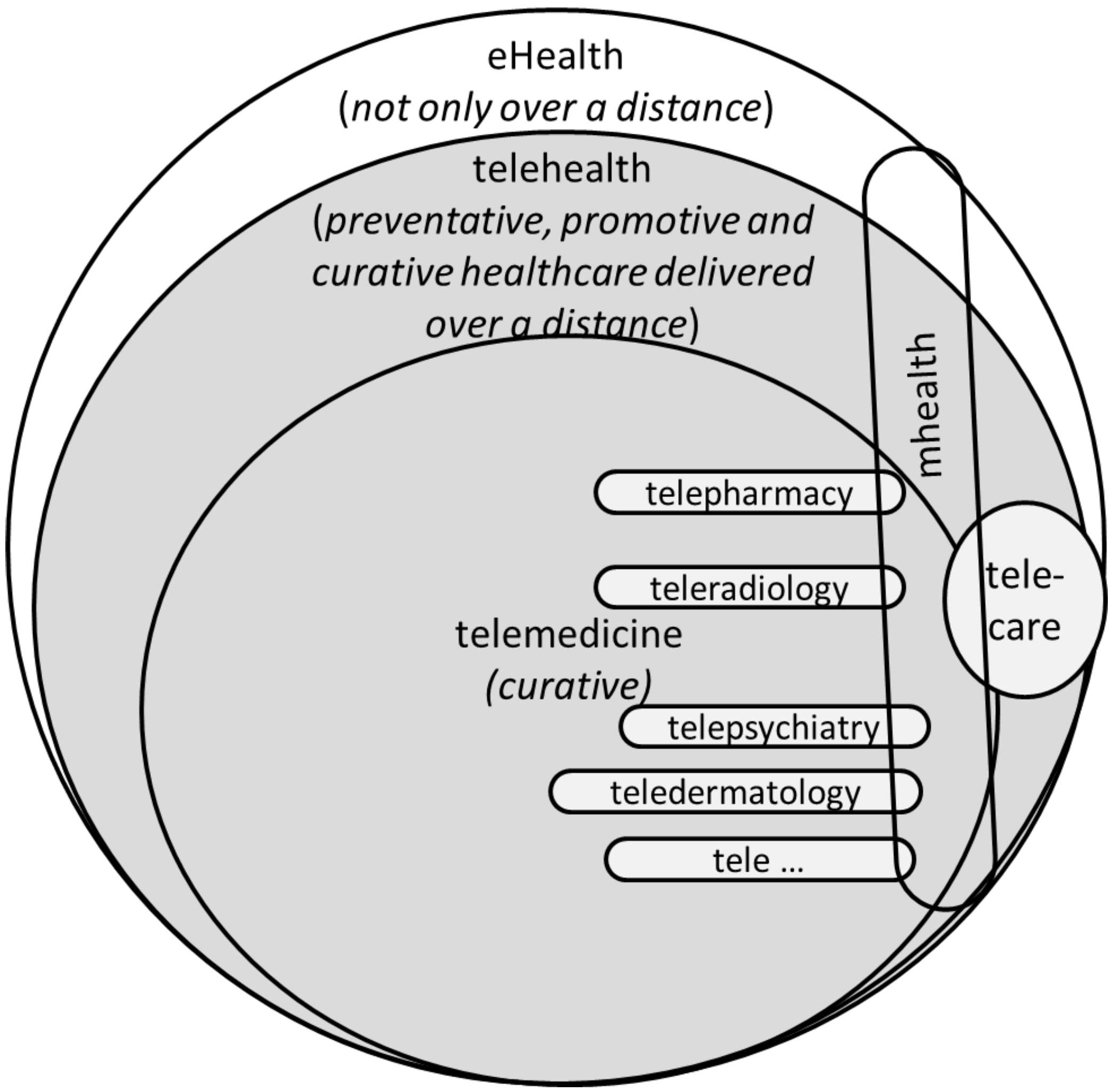
4.1. Telehealth
4.2. Telecare
5. Frameworks Related to the Diffusion of Innovation
- Technical barrier: It is imperative that the appropriate technology is available, as well as knowledge about it.
- Behavioral barrier: This barrier involves change management, especially with respect to resistance to change, power and politics around telehealth. Tanriverdi and Iacono [19] emphasized the importance of so-called proponents of telehealth in accomplishing this change.
- Economical barrier: Two major concerns of Tanriverdi and Iacono [19] were to reimburse healthcare workers for telehealth consultations and to open up new patient markets.
- Organizational barrier: Tanriverdi and Iacono [19] found it crucial to integrate telehealth services into existing organizational structures and to provide institutional support to execute these services.
6. eReadiness Frameworks
- Chipps and Mars [30] assessed the preparedness of health districts and designated hospitals in the KwaZulu-Natal (KZN) province for proposed telepsychiatry services. They concluded that in order for telepsychiatry to succeed in KwaZulu-Natal, a change management awareness would be needed. However, it was not made clear if and how the ehealth readiness assessment tool set could assist with this.
- Durrani and Khoja [31] used this tool set to measure the ehealth readiness of two separate ehealth programs, one in Kabul and the other in Bamyan. The ehealth readiness assessment tool set was found to be useful, firstly, in comparing the ehealth readiness of these two programs, and secondly, in “broadening the vision of the institutions as a whole”.
- (1)
- Core readiness (21 statements) deals with aspects of planning and integration.
- (2)
- Technological readiness (10 statements) considers the availability, reliability, affordability and ICT, as well as the related infrastructure.
- (3)
- Learning readiness (six statements) addresses issues related to the programs and resources available for the provision of training in the use of the technology.
- (4)
- Societal readiness (11 statements) considers the interaction between the institution and other institutions in the region and beyond. Socio-cultural factors are also included.
- (5)
- Policy readiness (12 statements) deals with policies, at the government and institutional level, which are in place to address common issues, such as licensing, liability and reimbursement.
| Barriers [19] | Micro-level | Macro-level |
|---|---|---|
| Technical | Technology (hardware and software) | Technology (ICT infrastructure) |
| Behavioral | Learning (healthcare workers) | Society |
| Economical | Core (budget) | Policy (reimbursement models) |
| Organizational | Core (process integration and prioritization) | Policy (planning and promotion of telehealth) |
7. Unified Theory of Acceptance and Use of Technology (UTAUT)
- I find (the technology under consideration) useful in my daily life.
- Using (the technology under consideration) helps me accomplish things more quickly.
- The (technology under consideration) is reasonably priced.
- The use of (the technology under consideration) has become a habit for me.
8. Retrospective Guidelines
8.1. Seven Core Principles for the Successful Development of Telemedicine Services
- (1)
- Telehealthcare applications as sites should be selected pragmatically, rather than philosophically.
- (2)
- Clinician drivers and telehealth users must own the systems.
- (3)
- Telehealthcare management and support should be from the bottom up rather than from the top down.
- (4)
- The technology should be as user-friendly as possible.
- (5)
- Telehealthcare users must be well trained and supported, both technically and professionally.
- (6)
- Telehealthcare applications should be evaluated in a clinically appropriate and user-friendly manner.
- (7)
- Information about the development of telehealth must be shared.
8.2. Lessons in Telemedicine Service Innovation
- Policy context: Policies should be formulated in such a way that telehealth innovation is encouraged rather than discouraged. It is also important that the policies are translated into resources.
- Evidence gathering, “proving” safety and managing risk: The successful telemedicine services were those whose potential risks were acknowledged and for which safeguards were built into the systems. Furthermore, such services emphasized the close monitoring of effects and outcomes, rather than formal, scientific, evaluation.
- Perceived benefit and related commitment: Finch et al. [34], without consulting theories on the acceptance of technology, concluded that there is a direct link between the willingness of role players to commit to new technology and/or methods and the benefit they are perceived to have.
- Reconfiguring services: The focus should not be on the technology, but on the way in which the service is delivered.
- Professional roles and boundary crossing: Together with changes in work procedures, clinicians need to make changes to their traditionally perceived professional roles.
8.3. Framework for Assessing Health System Challenges to Scaling up mHealth in South Africa
| Government stewardship: is there a policy environment supportive of mhealth? |
| Strategic leadership: policy guidelines, alignment with strategic health goals, funding sources, common ICT standards, collaboration partnerships |
| Learning environment: learning environment, systematic evaluation of projects, central repository of projects |
| Organizational: culture of and capacity for using information technology for management |
| Capacity for implementation: capacity to implement mhealth interventions, assessment of ereadiness, a functional ICT environment and effective mechanisms for implementation, support, monitoring and evaluation. |
| Culture of information use: organizational culture of using health information for management |
| Technological: integrated and sustainable technology |
| Use-ability: ease of use, flexibility and durability, beneficial to end users |
| Interoperability: communication across technological and information platforms, integration with existing work practices, common standards, financial sustainability |
| Privacy and security: privacy and security of data, regulations for protecting electronic data |
| Financial: financial provision being made for the medium to long term |
| Sustainable funding: sustainable funding for large-scale implementation, clear business and funding plans |
| Cost-effectiveness: cost-effectiveness evaluated, mhealth interventions weighed up against other priority and evidence-based interventions; opportunity costs are routinely considered |
9. Comprehensive Model for Evaluating Telemedicine
- Level of analysis: Each of the three broad categories (individual, community and society) is comprised of multiple elements of which some examples are indicated in Figure 2. “Conclusions regarding the acceptability of telehealth may vary substantially across the three levels, since benefits and costs may accrue to entities outside the immediate transaction.” [11]
- Focus of analysis: This dimension considers the often conflicting considerations of cost, quality and access to healthcare.
- Activities of analysis: Telehealthcare services are mostly directed towards clinical examinations, consultations, discussions and other clinical purposes. With this dimension, it is also recognized that telehealth service infrastructure is also used for education, research and administration.
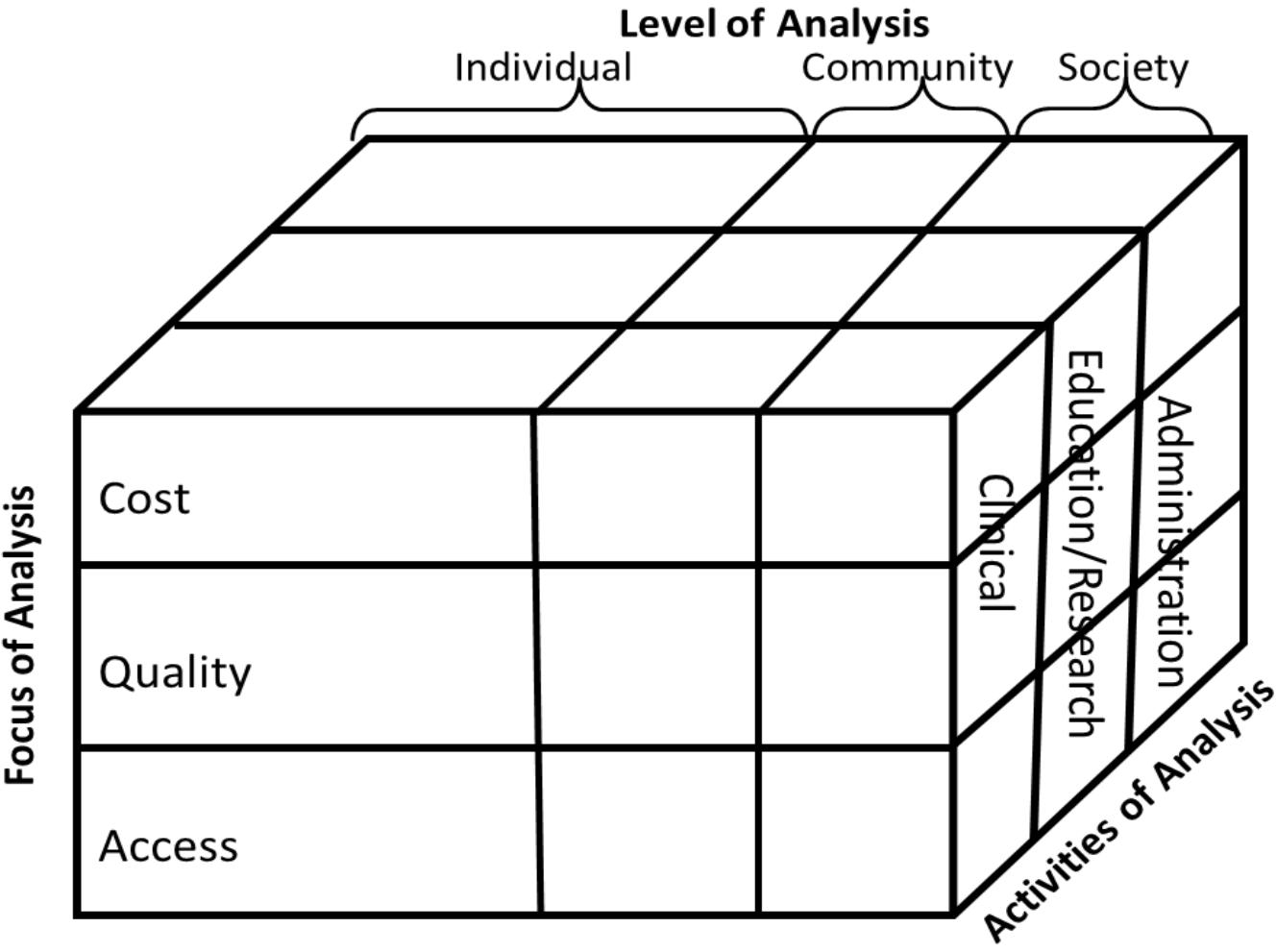
- The cost of education/research concerning the service at the level of an individual;
- The level of community access to clinical services;
- The level of quality of the clinical services to society;
- An individuals level of access to administrative services;
- The quality of education/research concerning the service at the community level;
- The cost of administrative services at the society level.
10. Lifecycle Frameworks
| Layered telemedicine implementation model [3] | Stages of the ehealth lifecycle [26] |
|---|---|
| Prototype | Development |
| Small-scale Pilot | Implementation |
| Large-scale Pilot | Integration |
| Operational Product | Sustained Operation |
10.1. The Layered Telemedicine Implementation Model
| Lifecycle Phase | Category | Determinants for the successful implementation of telemedicine |
|---|---|---|
| Prototype phase | Technology | support, training, usability, quality |
| Small-scale pilots | Acceptance | attitude and usability, evidence-based medicine, diffusion and dissemination |
| Large-scale pilots | Financing and organization | service provider and structure |
| Operational products | Policy and legislation | legislation and policy, standardization, security |
10.2. The Khoja–Durrani–Scott (KDS) Evaluation Framework
| Stages of the ehealth lifecycle | ||||
|---|---|---|---|---|
| Themes of Evaluation | Development | Implementation | Integration | Sustained Operation |
| Health Services | Ongoing assessment of health services status, opportunities and needs | Improved diagnosis and treatment of disease conditions | Health impact leading to change in disease status | Health impact showing change via indicators |
| Technology | Cost of development, availability, affordability | Interoperability | Appropriate in a variety of conditions | Scalability |
| Economic | Affordability | Cost-utility | Cost-utility Cost-benefit | Improved disability-adjusted life years |
| Behavioral andSociotechnical | Factors related to human resources | Strategy for ehealth implementation | Strategy for broader ehealth adoption | Adoption / adaption of technology on a wider scale |
| Ethical | eHealth prioritized over other issues | Sensitive to sociocultural issues | Broader perspective on security, liability, licensure as well as reimbursement | Security |
| Readiness andChange | Change management planning | Training of staff, including clinical and management staff | Effective management of change | modification, improvement, customization |
| Policy | Change management policies | Limited changes in organizational and national policies | Policy changes to facilitate broader adoption | Public policy and organizational practice |
11. Discussion
11.1. Theories
11.2. Development Methods and Framework Formats
- Statements/outcomes associated with Likert-like scales: The ehealth readiness assessment tools [16] as well as the UTAUT, as it is applied to telehealth [14,15], are framed as a list of statements that is linked to a Likert-like scale, ranging from strongly disagree to strongly agree. Both of these tool sets are taken from other domains in which they were already validated.
- Guidelines based on longitudinal studies: The barriers to the diffusion of telemedicine in [19], the Seven Core Principles in [2] and the lessons in telemedicine service innovation in [34] are all based on longitudinal studies, and they are formatted as a list of guidelines. The framework for assessing health system challenges to scaling up mhealth [29] is also included here, since it relies on case studies and consists of a list of so-called capability requirements.
- Lifecycle frameworks: For both the KDS Evaluation Framework [26] and the Layered Implementation Model [3], systematic literature reviews were executed. Khoja et al. [26] also conducted interviews. Both of these are framed along the lifecycle phases of a telehealth service. Within their frame, Broens et al. [3] indicate, what they call, determinants for the successful implementation of telemedicine services. Khoja et al. [26] fill their framework with expected outcomes.
- The Comprehensive Model for the Evaluation of Telemedicine has a unique three-dimensional design. It is not clear which method was followed to arrive at this design.
11.3. Validation
11.4. Themes
12. Conclusions
Acknowledgments
Conflicts of Interest
References
- Bashshur, R.; Reardon, T.; Shannon, G. Telemedicine: A new health care delivery system. Annu. Rev. Public Health 2000, 21, 613–637. [Google Scholar] [CrossRef]
- Yellowlees, P. Successfully developing a telemedicine system. J. Telemed. Telecare 2005, 11, 331–336. [Google Scholar] [CrossRef]
- Broens, T.H.; Vollenbroek-Hutten, M.M.; Hermens, H.J.; van Halteren, A.T.; Nieuwenhuis, L.J. Determinants of successful telemedicine implementations: A literature study. J. Telemed. Telecare 2007, 13, 303–309. [Google Scholar] [CrossRef]
- South African Government. eHealth Strategy for South Africa, 2012–2016. Available online: http://www.doh.gov.za/docs/stratdocs/2012 (accessed on 17 February 2013).
- Handler, T.J. Hype cycle for telemedicine. Gart. Ind. Res. 2007, G00233474, 1–56. [Google Scholar]
- Sood, S.; Mbarika, V.; Jugoo, S.; Dookhy, R.; Doarn, C.R.; Prakash, N. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed. e-Health 2007, 13, 573–590. [Google Scholar] [CrossRef]
- Ekeland, A.G.; Bowes, A.; Flottorp, S. Methodologies for assessing telemedicine: A systematic review of reviews. Int. J. Med. Inform. 2011, 81, 1–11. [Google Scholar] [CrossRef]
- Van der Wetering, R.; Batenburg, R. A framework for the economic evaluation of telemedicine. J. Telemed. Telecare 1997, 28, 132–139. [Google Scholar]
- Ethal, E. Sustainable Telemedicine: Paradigms for Future-Proof Healthcare. Available online: http://armtelemed.org/resources/48-EHTEL_Briefing Paper Sustainable Telemedicine.pdf (accessed on 30 December 2013).
- Kidholm, K.; Ekeland, A.G.; Jensen, L.K.; Rasmussen, J.; Pedersen, C.D.; Bowes, A.; Flottorp, S.A.; Bech, M. A model for assessment of telemedicine applications: MAST. Int. J. Technol. Assess. Health Care 2012, 28, 44–51. [Google Scholar] [CrossRef]
- Hicks, L.L.; Boles, K.E. A comprehensive model for evaluating telemedicine. Stud. Health Technol. Inform. 2004, 106, 3–13. [Google Scholar]
- Attewell, P. Technology diffusion and organizational learning: The case of business computing. Organ. Sci. 1992, 3, 1–19. [Google Scholar] [CrossRef]
- Khoja, S.; Scott, R.; Mohsin, M.; Ishaq, A.F.M.; Casebeer, A.L. Developing a conceptual-framework for e-health readiness assessment tools for developing countries. ICT Develop. 2006, 8, 79–81. [Google Scholar]
- Cilliers, L.; Flowerday, S.V. Health information systems to improve health care: A telemedicine case study. SA J. Inf. Manag. 2013, 15, 5. [Google Scholar] [CrossRef]
- Alikarami, R.; Moghadam, R.A.; Javadi, S.R.S.; Vahdat, D. Evaluation of effecting factors on success of telemedicine systems (using models of TAM and UTAUT). Can. J. Netw. Inf. Secur. 2011, 2, 5–9. [Google Scholar]
- Khoja, S.; Scott, R.; Casebeer, A.; Mohsin, M.; Ishaq, A.; Gilani, S. E-health readiness assessment tools for healthcare institutions in developing countries. Telemed. e-Health 2007, 13, 425–432. [Google Scholar] [CrossRef]
- Buchachi, F.; Pakenham-Walsh, N. Information technology of health in developing countries. Chest 2007, 132, 1624–1630. [Google Scholar] [CrossRef]
- Pelletier-Fleury, N.; Fargeon, V.; Lanoé, J.; Fardeau, M. Transaction costs economics as a conceptual framework for the analysis of barriers to the diffusion of telemedicine. Health Policy 1997, 106, 1–14. [Google Scholar] [CrossRef]
- Tanriverdi, H.; Iacono, C.S. Knowledge Barriers to Diffusion of Telemedicine. In Proceedings of the International Conference of the Association for Information Systems, Helsinki, Finland, 14–16 August 1998; pp. 39–50.
- Bashshur, R.; Shannon, G.; Krupinski, E.; Grigsby, J. The taxonomy of telemedicine. Telemed. e-Health 2011, 17, 484–494. [Google Scholar] [CrossRef] [Green Version]
- Telehealth and Telecare Aware. What is Telecare? Available online: http://telecareaware.com (accessed on 17 July 2013).
- Grigsby, J.; Rigby, M.; Hiemstra, A.; House, M.; Olsson, S.; Whitten, P. The diffusion of telemedicine. Telemed. J. e-Health 2002, 8, 79–94. [Google Scholar] [CrossRef]
- Scott, W.R. Innovation in medical care organizations: A synthetic review. Med. Care Res. Rev. 1990, 47, 165–192. [Google Scholar] [CrossRef]
- Jennett, P.; Gagnon, M.; Brandstadt, H. Preparing for success: Readiness models for rural telehealth. J. Postgrad. Med. 2005, 51, 279. [Google Scholar]
- Legare, E.; Vincent, C.; Lehoux, P.; Anderson, D.; Kairy, D.; Gagnon, M. Telehealth readiness assessment tools. J. Telemed. Telecare 2010, 16, 107. [Google Scholar] [CrossRef]
- Khoja, S.; Durrani, H.; Scott, R.; Sajwani, A.; Piryani, U. Conceptual framework for development of comprehensive e-Health evaluation tool. Telemed. e-Health 2013, 19, 48–53. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Li, J.; Land, L.; Ray, P. A Framework for Assessing ICT Preparedness for e-Health Implementations. In Proceedings of the 10th International Conference on e-Health Networking, Applications and Services, Singapore, 7–9 July 2008; pp. 124–129.
- Tamburis, O.; Mangia, M.; Contenti, M.; Mercurio, G.; Mori, A.R. The LITIS conceptual framework: Measuring eHealth readiness and adoption dynamics across the Healthcare Organizations. Health Technol. 2012, 2, 97–112. [Google Scholar] [CrossRef]
- Leon, N.; Schneider, H.; Daviaud, E. Applying a framework for assessing the health system challenges to scaling up mHealth in South Africa. BMC Med. Inform. Decis. Mak. 2012, 12, 123. [Google Scholar] [CrossRef]
- Chipps, J.; Mars, M. Readiness of healthcare institutions in Kwazulu-Natal to implement telepsychiatry. J. Telemed. Telecare 2012, 18, 133–137. [Google Scholar] [CrossRef]
- Durrani, H.; Khoja, S. Health needs and eHealth readiness assessment of health care organizations in Kabul and Bamyan, Afghanistan. EMHJ 2012, 18, 663–670. [Google Scholar]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar]
- Dünnebeil, S.; Sunyaev, A.; Blohm, I.; Leimeister, J.M.; Krcmar, H. Determinants of physicians technology acceptance for e-health in ambulatory care. Int. J. Med. Inform. 2012, 81, 746–760. [Google Scholar] [CrossRef]
- Finch, T.; Mair, F.; May, C. Teledermatology in the UK: Lessons in service innovation. Br. J. Dermatol. 2006, 156, 521–527. [Google Scholar] [CrossRef]
- Van Dyk, L. The Development of a Telemedicine Maturity Model. Ph.D. Dissertation, Stellenbosch University, Stellenbosch, South Africa, 2013. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Van Dyk, L. A Review of Telehealth Service Implementation Frameworks. Int. J. Environ. Res. Public Health 2014, 11, 1279-1298. https://doi.org/10.3390/ijerph110201279
Van Dyk L. A Review of Telehealth Service Implementation Frameworks. International Journal of Environmental Research and Public Health. 2014; 11(2):1279-1298. https://doi.org/10.3390/ijerph110201279
Chicago/Turabian StyleVan Dyk, Liezl. 2014. "A Review of Telehealth Service Implementation Frameworks" International Journal of Environmental Research and Public Health 11, no. 2: 1279-1298. https://doi.org/10.3390/ijerph110201279
APA StyleVan Dyk, L. (2014). A Review of Telehealth Service Implementation Frameworks. International Journal of Environmental Research and Public Health, 11(2), 1279-1298. https://doi.org/10.3390/ijerph110201279




