Disseminating Childhood Home Injury Risk Reduction Information in Pakistan: Results from a Community-Based Pilot Study
Abstract
:1. Background
2. Methods
2.1. Tool Development
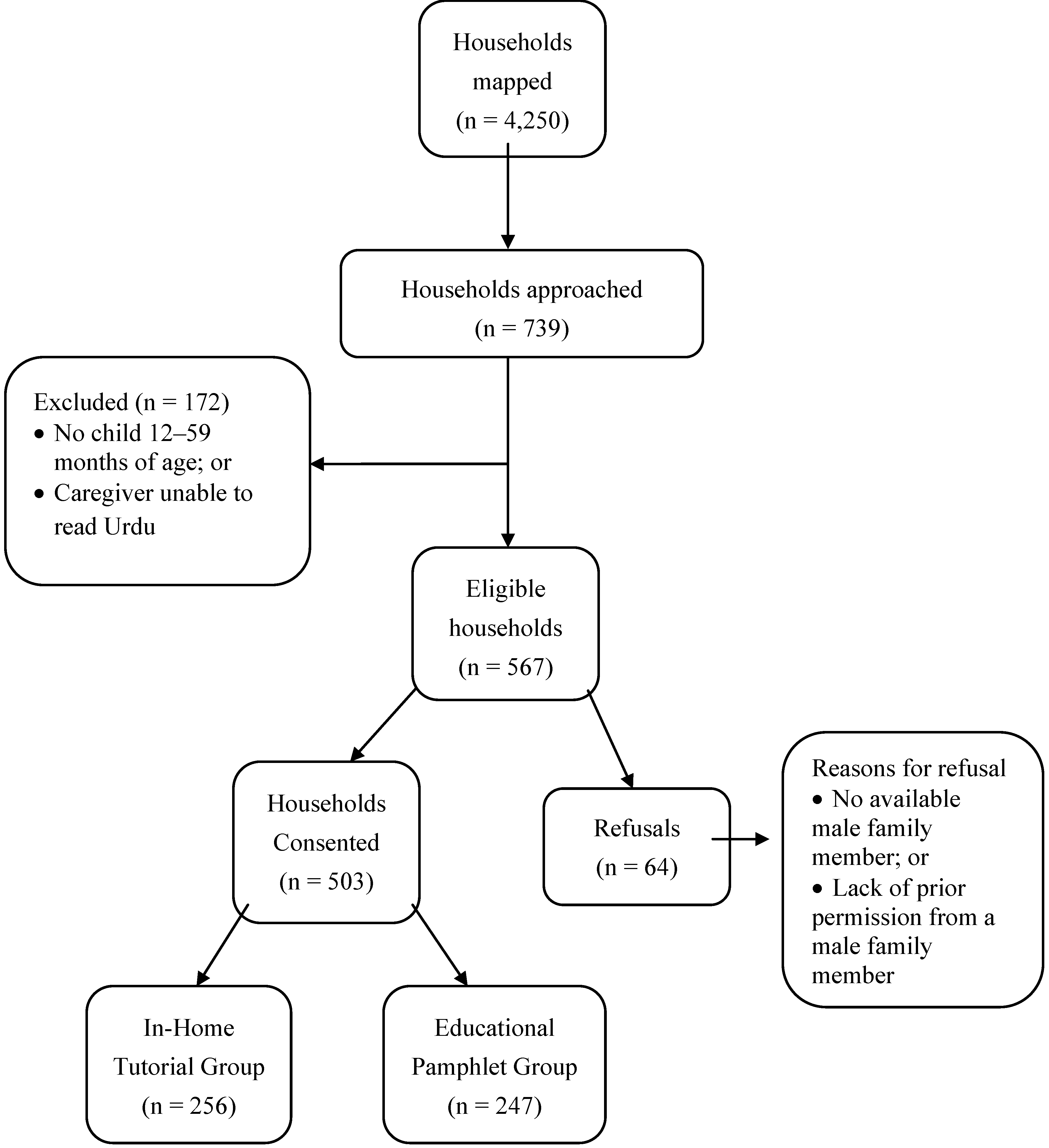
2.2. Study Design
2.3. Statistical Analysis
3. Results
| Characteristics | In-Home Tutorial Group; | Educational Pamphlet Group; | Comparison |
|---|---|---|---|
| N = 256 (%) | N = 247 (%) | (p value) | |
| Respondent Characteristics | |||
| Gender | |||
| Female | 254 (99.2) | 243 (98.4) | p = 0.39 |
| Male | 2 (0.8) | 4 (1.6) | |
| Age Group | |||
| <20 years | 6 (2.3) | 8 (3.2) | p = 0.12 |
| 20–29 years | 124 (48.4) | 144 (58.3) | |
| 30–39 years | 95 (37.1) | 78 (31.6) | |
| 40–49 years | 19 (7.4) | 11 (4.5) | |
| 50+ years | 12 (4.7) | 6 (2.4) | |
| Education Level | |||
| <Grade 9 | 104 (40.6) | 59 (23.9) | p < 0.01 |
| ≥Grade 9 | 152 (59.4) | 188 (76.1) | |
| Occupation of Mother | |||
| Housewife | 235 (91.8) | 233 (94.3) | p = 0.53 |
| Other | 21 (8.2) | 14 (5.7) | |
| Child Characteristics | |||
| Mean Age (months) | 34.3 | 35.2 | p = 0.42 |
| Gender | |||
| Male | 131 (51.2) | 124 (50.2) | p = 0.83 |
| Female | 125 (48.8) | 123 (49.8) | |
| Child’s Primary Caregiver | |||
| Mother | 218 (85.2) | 233 (94.3) | p < 0.01 |
| Father | 9 (3.5) | 2 (0.8) | |
| Other | 29 (11.3) | 12 (4.9) | |
| In Home-Tutorial Group | Educational Pamphlet Group | |||||
|---|---|---|---|---|---|---|
| Pre-Intervention | Post-Intervention | Comparison | Pre-Intervention | Post Intervention | Comparison | |
| N = 256 (%) | N = 215 (%) | (p value) | N = 247 (%) | N = 219 (%) | (p value) | |
| Falls | ||||||
| Walker present/used | 43 (16.8) | 10 (4.6) | <0.01 | 34 (13.8) | 9 (4.1) | <0.01 |
| Accessible rooftop without railing | 54/110 * (49.1) | 33/78 * (42.3) | 0.36 | 42/77 * (54.6) | 35/66 * (53.0) | 0.86 |
| Drowning | ||||||
| Open buckets of water | 134 (52.3) | 63 (29.2) | <0.01 | 106 (42.9) | 43/217 * (19.8) | <0.01 |
| Uncovered large vat of water | 74 (28.9) | 23 (10.7) | <0.01 | 35 (14.2) | 17 (7.8) | 0.03 |
| Burns | ||||||
| Water heater within reach | 72 (28.1) | 9 (4.2) | <0.01 | 65 (26.3) | 4/218 * (1.8) | <0.01 |
| Stove within reach | 165 (64.5) | 82 (38.1) | <0.01 | 114 (46.2) | 47 (21.5) | <0.01 |
| Matches within reach | 127 (49.6) | 68 (31.5) | <0.01 | 94 (38.1) | 39 (17.8) | <0.01 |
| Open fire within reach | 65 (25.4) | 37 (17.1) | 0.03 | 19 (7.7) | 30 (13.7) | 0.04 |
| Iron within reach | 146 (57.0) | 87 (40.5) | <0.01 | 81 (32.8) | 92 (42.0) | 0.04 |
| Overloaded outlets | 47 (18.4) | 42 (19.4) | 0.76 | 47 (19.0) | 38 (17.4) | 0.64 |
| Frayed/loose cords within reach | 44 (17.2) | 24 (11.1) | 0.06 | 42 (17.0) | 18 (8.2) | <0.01 |
| Poisoning | ||||||
| Cooking fluids labeled inappropriately | 81 (31.6) | 67 (31.0) | 0.89 | 35 (14.2) | 38 (17.4) | 0.35 |
| Cleaning supplies within reach | 86 (33.6) | 45 (20.9) | <0.01 | 84 (34.0) | 27 (12.3) | <0.01 |
| Shampoos/soaps within reach | 99 (38.7) | 28 (13.0) | <0.01 | 58 (23.5) | 26 (11.9) | <0.01 |
| Medicines within reach | 47 (18.4) | 12 (5.6) | <0.01 | 30 (12.2) | 17 (7.8) | 0.12 |
| Lacerations | ||||||
| Breakable objects within reach | 88 (34.4) | 21 (9.7) | <0.01 | 65 (26.3) | 24/218 * (11.0) | <0.01 |
| Knives within reach | 110 (43.0) | 47 (21.8) | <0.01 | 76 (30.8) | 22 (10.1) | <0.01 |
| Fan/sharp object within reach | 129 (50.4) | 89 (41.4) | 0.05 | 113 (45.8) | 82 (37.4) | 0.07 |
| Hazard Description | Odds Ratio (OR) * | 95% CI |
|---|---|---|
| Falls | ||
| Walker present/used | 1.48 | 0.84, 2.62 |
| Accessible rooftop without railing | 1.04 | 0.61, 1.79 |
| Drowning | ||
| Open bucket of water | 1.27 | 0.83, 1.95 |
| Uncovered vat/pool of water | 2.14 | 1.28, 3.58 |
| Burns | ||
| Water heater within reach | 1.20 | 0.76, 1.88 |
| Stove within reach | 1.09 | 0.72, 1.67 |
| Matches within reach | 1.07 | 0.69, 1.66 |
| Open fire within reach | 3.55 | 1.80, 7.00 |
| Iron within reach | 1.95 | 1.21, 3.12 |
| Overloaded outlets | 0.75 | 0.43, 1.30 |
| Frayed/loose cords within reach | 0.84 | 0.48, 1.47 |
| Poisoning | ||
| Cooking fluids labeled inappropriately | 1.86 | 1.07, 3.25 |
| Cleaning supplies within reach | 0.86 | 0.54, 1.37 |
| Medicines within reach | 1.45 | 0.82, 2.55 |
| Shampoos/soaps within reach | 1.78 | 1.12, 2.82 |
| Cuts | ||
| Breakable objects within reach | 1.52 | 0.96, 2.41 |
| Knives within reach | 1.11 | 0.71, 1.72 |
| Fan/sharp objects within reach | 1.17 | 0.73, 1.89 |
4. Discussion
5. Conclusions
Acknowledgements
References
- Mock, C.; Peden, M.; Hyder, A.A.; Butchart, A.; Krug, E. Child injuries and violence: The new challenge for child health. Bull. WHO 2008, 86, 420. [Google Scholar] [CrossRef]
- Peden, M. World report on child injury prevention appeals to “keep kids safe”. Inj. Prev. 2008, 14, 413–414. [Google Scholar] [CrossRef]
- Zia, N.; Khan, U.R.; Razzak, J.A.; Puvanachandra, P.; Hyder, A.A. Understanding unintentional childhood home injuries: Pilot surveillance data from Karachi, Pakistan. BMC Res. Notes 2012, 5, 37. [Google Scholar] [CrossRef]
- Sengoelge, M.; Hasselberg, M.; Laflamme, L. Child home injury mortality in Europe: A 16-country analysis. Eur. J. Public Health 2011, 21, 166–170. [Google Scholar] [CrossRef]
- Mahalakshmy, T.; Dongre, A.R.; Kalaiselvan, G. Epidemiology of childhood injuries in rural Puducherry, South India. Indian J. Pediatr. 2011, 78, 821–825. [Google Scholar] [CrossRef]
- Irving, L. Preventing unintentional injuries in children and young people under 15. Community Pract. 2011, 84, 36–38. [Google Scholar]
- Gururaj, G. Injury prevention and care: An important public health agenda for health, survival and safety of children. Indian J. Pediatr. 2012. [Google Scholar] [CrossRef]
- Phelan, K.J.; Khoury, J.; Xu, Y.; Liddy, S.; Hornung, R.; Lanphear, B.P. A randomized controlled trial of home injury hazard reduction: The home injury study. Arch. Pediatr. Adolesc. Med. 2011, 165, 339–345. [Google Scholar] [CrossRef]
- Kendrick, D.; Coupland, C.; Mulvaney, C.; Simpson, J.; Smith, S.J.; Sutton, A.; Watson, M.; Woods, A. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst. Rev. 2007, CD005014. [Google Scholar] [CrossRef]
- Kendrick, D.; Elkan, R.; Hewitt, M.; Dewey, M.; Blair, M.; Robinson, J.; Williams, D.; Brummell, K. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta analysis. Arch. Dis. Child. 2000, 82, 443–451. [Google Scholar] [CrossRef]
- Elkan, R.; Kendrick, D.; Hewitt, M.; Robinson, J.J.; Tolley, K.; Blair, M.; Dewey, M.; Williams, D.; Brummell, K. The effectiveness of domiciliary health visiting: A systematic review of international studies and a selective review of the British literature. Health Technol. Assess. 2000, 4, 1–339. [Google Scholar]
- Babul, S.; Olsen, L.; Janssen, P.; McIntee, P.; Raina, P. A randomized trial to assess the effectiveness of an infant home safety programme. Int. J. Inj. Contr. Saf. Promot. 2007, 14, 109–117. [Google Scholar] [CrossRef]
- Odendaal, W.; van Niekerk, A.; Jordaan, E.; Seedat, M. The impact of a home visitation programme on household hazards associated with unintentional childhood injuries: A randomised controlled trial. Accid. Anal. Prev. 2009, 41, 183–190. [Google Scholar] [CrossRef]
- Carlsson, A.; Bramhagen, A.C.; Jansson, A.; Dykes, A.K. Precautions taken by mothers to prevent burn and scald injuries to young children at home: An intervention study. Scand. J. Public Health 2011, 39, 471–478. [Google Scholar] [CrossRef]
- Swart, L.; van Niekerk, A.; Seedat, M.; Jordaan, E. Paraprofessional home visitation program to prevent childhood unintentional injuries in low-income communities: A cluster randomized controlled trial. Inj. Prev. 2008, 14, 164–169. [Google Scholar] [CrossRef]
- Nansel, T.R.; Weaver, N.L.; Jacobsen, H.A.; Glasheen, C.; Kreuter, M.W. Preventing unintentional pediatric injuries: A tailored intervention for parents and providers. Health Educ. Res. 2008, 23, 656–669. [Google Scholar]
- Sznajder, M.; Leduc, S.; Janvrin, M.P.; Bonnin, M.H.; Aegerter, P.; Baudier, F.; Chevallier, B. Home delivery of an injury prevention kit for children in four french cities: A controlled randomized trial. Inj. Prev. 2003, 9, 261–265. [Google Scholar] [CrossRef]
- Pakistan: Country at a Glance. Available online: www.worldbank.org/en/country/pakistan (accessed on 15 December 2012).
- Lasi, S.; Rafique, G.; Peermohamed, H. Childhood injuries in Pakistan: Results from two communities. J. Health Popul. Nutr. 2010, 28, 392–398. [Google Scholar]
- Fatmi, Z.; Kazi, A.; Hadden, W.C.; Bhutta, Z.A.; Razzak, J.A.; Pappas, G. Incidence and pattern of unintentional injuries and resulting disability among children under 5 years of age: Results of the national health survey of Pakistan. Paediatr. Perinat. Epidemiol. 2009, 23, 229–238. [Google Scholar] [CrossRef]
- Hyder, A.A.; Wali, S.; Fishman, S.; Schenk, E. The burden of unintentional injuries among the under-five population in South Asia. Acta Paediatr. 2008, 97, 267–275. [Google Scholar] [CrossRef]
- Hyder, A.A.; Sugerman, D.E.; Puvanachandra, P.; Razzak, J.; El-Sayed, H.; Isaza, A.; Rahman, F.; Peden, M. Global childhood unintentional injury surveillance in four cities in developing countries: A pilot study. Bull. WHO 2009, 87, 345–352. [Google Scholar]
- Rehmani, R.; Leblanc, J.C. Home visits reduce the number of hazards for childhood home injuries in Karachi, Pakistan: A randomized controlled trial. Int. J. Emerg. Med. 2010, 3, 333–339. [Google Scholar] [CrossRef]
- Hyder, A.A.; Chandran, A.; Khan, U.R.; Zia, N.; Huang, C.M.; de Ramirez, S.S.; Razzak, J. Childhood unintentional injuries: Need for a community-based home injury risk assessments in Pakistan. Int. J. Pediatr. 2012, 2012. [Google Scholar] [CrossRef]
- Wong, C.X.; Carson, K.V.; Smith, B.J. Home care by outreach nursing for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2012, 4, CD000994. [Google Scholar] [CrossRef]
- Viswanathan, M.; Kraschnewski, J.; Nishikawa, B.; Morgan, L.C.; Thieda, P.; Honeycutt, A.; Lohr, K.N.; Jonas, D. Outcomes of Community Health Worker Interventions; Rockville (MD): Rockville, USA, 2009; pp. 1–144. Evidence Reports/Technology Assessments, No. 181. [Google Scholar]
- Viswanathan, M.; Kraschnewski, J.L.; Nishikawa, B.; Morgan, L.C.; Honeycutt, A.A.; Thieda, P.; Lohr, K.N.; Jonas, D.E. Outcomes and costs of community health worker interventions: A systematic review. Med. Care 2010, 48, 792–808. [Google Scholar]
- Lewin, S.; Munabi-Babigumira, S.; Glenton, C.; Daniels, K.; Bosch-Capblanch, X.; van Wyk, B.E.; Odgaard-Jensen, J.; Johansen, M.; Aja, G.N.; Zwarenstein, M.; et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst. Rev. 2010, CD004015. [Google Scholar] [CrossRef]
- Forst, L.; Lacey, S.; Chen, H.Y.; Jimenez, R.; Bauer, S.; Skinner, S.; Alvarado, R.; Nickels, L.; Zanoni, J.; Petrea, R.; et al. Effectiveness of community health workers for promoting use of safety eyewear by Latino farm workers. Am. J. Ind. Med. 2004, 46, 607–613. [Google Scholar]
- Marsh, P.; Kendrick, D.; Williams, E.I. Health visitors’ knowledge, attitudes and practices in childhood accident prevention. J. Public Health Med. 1995, 17, 193–199. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Chandran, A.; Khan, U.R.; Zia, N.; Feroze, A.; De Ramirez, S.S.; Huang, C.-M.; Razzak, J.A.; Hyder, A.A. Disseminating Childhood Home Injury Risk Reduction Information in Pakistan: Results from a Community-Based Pilot Study. Int. J. Environ. Res. Public Health 2013, 10, 1113-1124. https://doi.org/10.3390/ijerph10031113
Chandran A, Khan UR, Zia N, Feroze A, De Ramirez SS, Huang C-M, Razzak JA, Hyder AA. Disseminating Childhood Home Injury Risk Reduction Information in Pakistan: Results from a Community-Based Pilot Study. International Journal of Environmental Research and Public Health. 2013; 10(3):1113-1124. https://doi.org/10.3390/ijerph10031113
Chicago/Turabian StyleChandran, Aruna, Uzma Rahim Khan, Nukhba Zia, Asher Feroze, Sarah Stewart De Ramirez, Cheng-Ming Huang, Junaid A. Razzak, and Adnan A. Hyder. 2013. "Disseminating Childhood Home Injury Risk Reduction Information in Pakistan: Results from a Community-Based Pilot Study" International Journal of Environmental Research and Public Health 10, no. 3: 1113-1124. https://doi.org/10.3390/ijerph10031113




