Ischemic Postconditioning Alleviates Neuronal Injury Caused by Relief of Carotid Stenosis in a Rat Model of Cerebral Hypoperfusion
Abstract
:1. Introduction
2. Results and Discussion
2.1. Ischemic Postconditioning Increased Cerebral Blood Flow
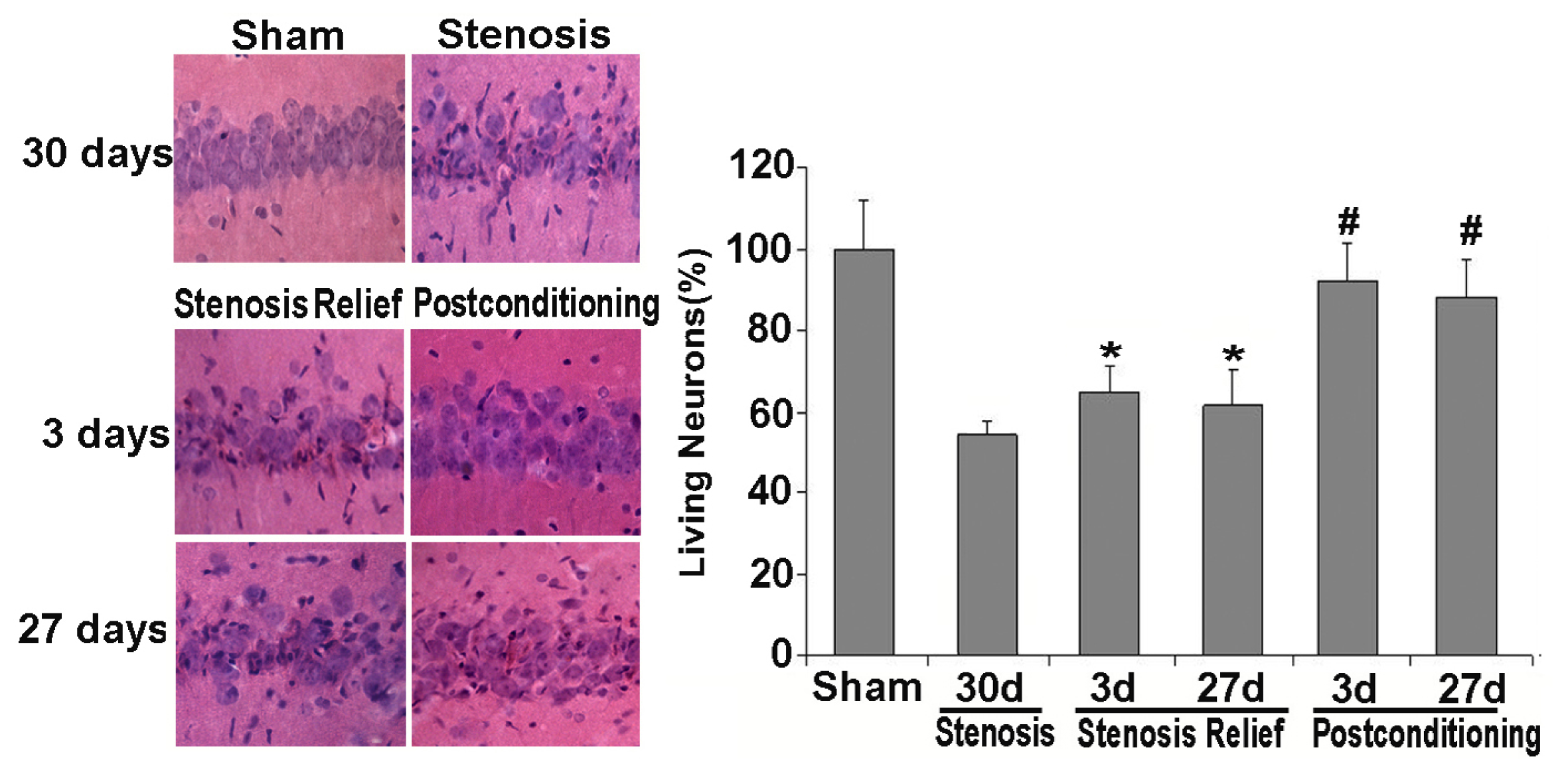
2.2. Ischemic Postconditioning Rescued Neuronal Death Caused by Stenosis Relief
2.3. Ischemic Postconditioning Inhibited Oxidative Stress Caused by Stenosis Relief
2.4. Ischemic Postconditioning Alleviated Inflammatory Response Caused by Stenosis Relief
2.5. Discussion
3. Experimental Section
3.1. Animals
3.2. Surgical Procedure and Postconditioning Protocol
3.3. Cerebral Blood Flow (CBF) Measurement
3.4. Brain Tissue Fixation
3.5. Hematoxylin and Eosin Staining and Histological Examination
3.6. Measurement of the Activities of Anti-Oxidative Enzymes
3.7. Measurement of Oxidative Product Level
3.8. Measurement of Inflammatory Factor Level
3.9. Data Analysis
4. Conclusions
Acknowledgements
- Conflict of InterestThe authors declare no conflict of interests.
References
- Taussky, P.; Hanel, R.A.; Meyer, F.B. Clinical considerations in the management of asymptomatic carotid artery stenosis. Neurosurg. Focus 2011, 31, E7. [Google Scholar]
- Young, K.C.; Jain, A.; Jain, M.; Replogle, R.E.; Benesch, C.G.; Jahromi, B.S. Evidence-based treatment of carotid artery stenosis. Neurosurg. Focus 2011, 30, E2. [Google Scholar]
- Landgraff, N.C.; Whitney, S.L.; Rubinstein, E.N.; Yonas, H. Cognitive and physical performance in patients with asymptomatic carotid artery disease. J. Neurol 2010, 257, 982–991. [Google Scholar]
- Silvestrini, M.; Paolino, I.; Vernieri, F.; Pedone, C.; Baruffaldi, R.; Gobbi, B.; Cagnetti, C.; Provinciali, L.; Bartolini, M. Cerebral hemodynamics and cognitive performance in patients with asymptomatic carotid stenosis. Neurology 2009, 72, 1062–1068. [Google Scholar]
- Zhou, Z.; Zhang, Y.; Zhu, C.; Sui, J.; Wu, G.; Meng, Z.; Huang, H.; Chen, K. Cognitive functions of carotid artery stenosis in the aged rat. Neuroscience 2012, 219, 137–144. [Google Scholar]
- Chen, Y.H.; Lin, M.S.; Lee, J.K.; Chao, C.L.; Tang, S.C.; Chao, C.C.; Chiu, M.J.; Wu, Y.W.; Chen, Y.F.; Shih, T.F.; et al. Carotid stenting improves cognitive function in asymptomatic cerebral ischemia. Int. J. Cardiol 2012, 157, 104–107. [Google Scholar]
- Duan, W.; Chun-Qing, Z.; Zheng, J.; Gui, L.; Huang, H.Q.; Chen, K.N. Relief of carotid stenosis improves impaired cognition in a rat model of chronic cerebral hypoperfusion. Acta Neurobiol. Exp(Wars) 2011, 71, 233–243. [Google Scholar]
- Marnane, M.; Ni, C.D.; Callaly, E.; Sheehan, O.C.; Merwick, A.; Hannon, N.; Horgan, G.; Kyne, L.; Moroney, J.; McCormack, P.M.; et al. Stroke recurrence within the time window recommended for carotid endarterectomy. Neurology 2011, 77, 738–743. [Google Scholar]
- Annambhotla, S.; Park, M.S.; Keldahl, M.L.; Morasch, M.D.; Rodriguez, H.E.; Pearce, W.H.; Kibbe, M.R.; Eskandari, M.K. Early vs. delayed carotid endarterectomy in symptomatic patients. J. Vasc. Surg 2012. [Google Scholar] [CrossRef]
- Wu, T.Y.; Anderson, N.E.; Barber, P.A. Neurological complications of carotid revascularisation. J. Neurol. Neurosurg. Psychiatry 2012, 83, 543–550. [Google Scholar]
- Liu, H.; Zhang, J.; Yang, Y.; Zhang, L.; Zeng, X. Decreased cerebral perfusion and oxidative stress result in acute and delayed cognitive impairment. Curr. Neurovasc. Res 2012, 9, 152–158. [Google Scholar]
- Zhao, H.; Sapolsky, R.M.; Steinberg, G.K. Interrupting reperfusion as a stroke therapy: Ischemic postconditioning reduces infarct size after focal ischemia in rats. J. Cereb. Blood Flow Metab 2006, 26, 1114–1121. [Google Scholar]
- Xing, B.; Chen, H.; Zhang, M.; Zhao, D.; Jiang, R.; Liu, X.; Zhang, S. Ischemic postconditioning inhibits apoptosis after focal cerebral ischemia/reperfusion injury in the rat. Stroke 2008, 39, 2362–2369. [Google Scholar]
- Wang, J.Y.; Shen, J.; Gao, Q.; Ye, Z.G.; Yang, S.Y.; Liang, H.W.; Bruce, I.C.; Luo, B.Y.; Xia, Q. Ischemic postconditioning protects against global cerebral ischemia/reperfusion-induced injury in rats. Stroke 2008, 39, 983–990. [Google Scholar]
- Penna, C.; Mancardi, D.; Rastaldo, R.; Pagliaro, P. Cardioprotection: A radical view Free radicals in pre and postconditioning. Biochim. Biophys. Acta 2009, 1787, 781–793. [Google Scholar]
- Guo, J.Y.; Yang, T.; Sun, X.G.; Zhou, N.Y.; Li, F.S.; Long, D.; Lin, T.; Li, P.Y.; Feng, L. Ischemic postconditioning attenuates liver warm ischemia-reperfusion injury through Akt-eNOS-NO-HIF pathway. J. Biomed. Sci 2011, 18, 79. [Google Scholar]
- Liu, K.X.; Li, Y.S.; Huang, W.Q.; Li, C.; Liu, J.X.; Li, Y. Immediate postconditioning during reperfusion attenuates intestinal injury. Intensive Care Med 2009, 35, 933–942. [Google Scholar]
- Liu, X.; Chen, H.; Zhan, B.; Xing, B.; Zhou, J.; Zhu, H.; Chen, Z. Attenuation of reperfusion injury by renal ischemic postconditioning: The role of NO. Biochem. Biophys. Res. Commun 2007, 359, 628–634. [Google Scholar]
- Loukogeorgakis, S.P.; Panagiotidou, A.T.; Yellon, D.M.; Deanfield, J.E.; MacAllister, R.J. Postconditioning protects against endothelial ischemia-reperfusion injury in the human forearm. Circulation 2006, 113, 1015–1019. [Google Scholar]
- Ma, X.J.; Zhang, X.H.; Li, C.M.; Luo, M. Effect of postconditioning on coronary blood flow velocity and endothelial function in patients with acute myocardial infarction. Scand. Cardiovasc. J 2006, 40, 327–333. [Google Scholar]
- Zhou, C.; Tu, J.; Zhang, Q.; Zhu, Y.; Zhang, W.; Yang, F.; Brann, D.W.; Wang, R. Delayed ischemic postconditioning protects hippocampal CA1 neurons by preserving mitochondrial integrity via Akt/GSK3β signaling. Neurochem. Int 2011, 59, 749–758. [Google Scholar]
- Li, Z.Y.; Liu, B.; Yu, J.; Yang, F.W.; Luo, Y.N.; Ge, P.F. Ischemic postconditioning rescues brain injury caused by focal ischemia reperfusion via attenuating proteins oxidization. J. Int. Med. Res 2012, 40, 954–966. [Google Scholar]
- Wang, Q.; Zhang, X.; Ding, Q.; Hu, B.; Xie, Y.; Li, X.; Yang, Q.; Xiong, L. Limb remote postconditioning alleviates cerebral reperfusion injury through reactive oxygen species-mediated inhibition of delta protein kinase C in rats. Anesth. Analg 2011, 113, 1180–1187. [Google Scholar]
- Zhang, W.; Miao, Y.; Zhou, S.; Jiang, J.; Luo, Q.; Qiu, Y. Neuroprotective effects of ischemic postconditioning on global brain ischemia in rats through upregulation of hippocampal glutamine synthetase. J. Clin. Neurosci 2011, 18, 685–689. [Google Scholar]
- Yuan, Y.; Guo, Q.; Ye, Z.; Pingping, X.; Wang, N.; Song, Z. Ischemic postconditioning protects brain from ischemia/reperfusion injury by attenuating endoplasmic reticulum stress-induced apoptosis through PI3K-Akt pathway. Brain Res 2011, 1367, 85–93. [Google Scholar]
- Ge, P.F.; Luo, T.F.; Zhang, J.Z.; Chen, D.W.; Luan, Y.X.; Fu, S.L. Ischemic preconditioning induces chaperone hsp70 expression and inhibits protein aggregation in the CA1 neurons of rats. Neurosci. Bull 2008, 24, 288–296. [Google Scholar]
- Kim, V.B.; Brown, P.M.; Brown, P.M., Jr; Sun, Y.S.; Lust, R.M.; Chitwood, W.R., Jr. A carotid stenosis model in canines. J. Invest. Surg 2001, 14, 241–247. [Google Scholar]
- Gao, X.; Ren, C.; Zhao, H. Protective effects of ischemic postconditioning compared with gradual reperfusion or preconditioning. J. Neurosci. Res 2008, 86, 2505–2511. [Google Scholar]
- Zhao, H.; Ren, C.; Chen, X.; Shen, J. From rapid to delayed and remote postconditioning: The evolving concept of ischemic postconditioning in brain ischemia. Curr. Drug Targets 2012, 13, 173–187. [Google Scholar]
- Ren, C.; Gao, X.; Niu, G.; Yan, Z.; Chen, X.; Zhao, H. Delayed postconditioning protects against focal ischemic brain injury in rats. PLoS One 2008, 3, e3851. [Google Scholar]
- Ren, C.; Yan, Z.; Wei, D.; Gao, X.; Chen, X.; Zhao, H. Limb remote ischemic postconditioning protects against focal ischemia in rats. Brain Res 2009, 1288, 88–94. [Google Scholar]
- Nanetti, L.; Taffi, R.; Vignini, A.; Moroni, C.; Raffaelli, F.; Bacchetti, T.; Silvestrini, M.; Provinciali, L.; Mazzanti, L. Reactive oxygen species plasmatic levels in ischemic stroke. Mol. Cell. Biochem 2007, 303, 19–25. [Google Scholar]
- Taffi, R.; Nanetti, L.; Mazzanti, L.; Bartolini, M.; Vignini, A.; Raffaelli, F.; Pasqualetti, P.; Vernieri, F.; Provinciali, L.; Silvestrini, M. Plasma levels of nitric oxide and stroke outcome. J. Neurol 2008, 255, 94–98. [Google Scholar]
- Nanetti, L.; Raffaelli, F.; Vignini, A.; Perozzi, C.; Silvestrini, M.; Bartolini, M.; Provinciali, L.; Mazzanti, L. Oxidative stress in ischaemic stroke. Eur. J. Clin. Invest 2011, 41, 1318–1322. [Google Scholar]
- Sugawara, T.; Chan, P.H. Reactive oxygen radicals and pathogenesis of neuronal death after cerebral ischemia. Antioxid. Redox Signal 2003, 5, 597–607. [Google Scholar]
- Amantea, D.; Marrone, M.C.; Nisticò, R.; Federici, M.; Bagetta, G.; Bernardi, G.; Mercuri, N.B. Oxidative stress in stroke pathophysiology validation of hydrogen peroxide metabolism as a pharmacological target to afford neuroprotection. Int. Rev. Neurobiol 2009, 85, 363–374. [Google Scholar]
- Ikonomidou, C.; Kaindl, A.M. Neuronal death and oxidative stress in the developing brain. Antioxid. Redox Signal 2011, 14, 1535–1550. [Google Scholar]
- Barone, F.C.; Feuerstein, G.Z. Inflammatory mediators and stroke: New opportunities for novel therapeutics. J. Cereb. Blood Flow Metab 1999, 19, 819–834. [Google Scholar]
- Kadhim, H.J.; Duchateau, J.; Sebire, G. Cytokines and brain injury: Invited review. J. Intensive Care Med 2008, 23, 236–249. [Google Scholar]





© 2012 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Feng, C.; Luo, T.; Qi, L.; Wang, B.; Luo, Y.; Ge, P. Ischemic Postconditioning Alleviates Neuronal Injury Caused by Relief of Carotid Stenosis in a Rat Model of Cerebral Hypoperfusion. Int. J. Mol. Sci. 2012, 13, 13338-13351. https://doi.org/10.3390/ijms131013338
Feng C, Luo T, Qi L, Wang B, Luo Y, Ge P. Ischemic Postconditioning Alleviates Neuronal Injury Caused by Relief of Carotid Stenosis in a Rat Model of Cerebral Hypoperfusion. International Journal of Molecular Sciences. 2012; 13(10):13338-13351. https://doi.org/10.3390/ijms131013338
Chicago/Turabian StyleFeng, Chunsheng, Tianfei Luo, Li Qi, Boyu Wang, Yinan Luo, and Pengfei Ge. 2012. "Ischemic Postconditioning Alleviates Neuronal Injury Caused by Relief of Carotid Stenosis in a Rat Model of Cerebral Hypoperfusion" International Journal of Molecular Sciences 13, no. 10: 13338-13351. https://doi.org/10.3390/ijms131013338



