Colorimetric Immunoassay for Detection of Tumor Markers
Abstract
:1. Introduction
2. Materials
2.1. ELISA-Based Colorimetric Immunoassays
2.1.1. Chemicals
2.1.2. Buffer Reagents
2.2. Nanomaterial-Based Colorimetric Immunoassays
3. Methods
3.1. ELISA-Based Colorimetric Immunoassays
3.1.1. Coating with Capture Antibody
3.1.2. Blocking and Adding Samples
3.1.3. Incubation with Detection Antibody
3.1.4. Colorimetric Detection
3.2. Nanomaterial-based Colorimetric Immunoassays
3.2.1. Synthesis and Modification of Nanomaterials
3.2.1.1. Synthesis of 13 nm Au-NPs
3.2.1.2. Modification of Au-NPs
3.2.1.2.1. Modification of Au-NPs with Thiol-oligonucleotides
3.2.1.2.2. Modification of Au-NPs with Antibodies
3.2.1.3. Modification of MPs
3.2.1.3.1. Modification of Amino-Functionalized MPs
3.2.1.3.2. Modification of Streptavidin-Functionalized MPs
3.2.2. Magnetic Collection and Separation of Target Tumor Markers
3.2.3. Application of Au-NPs in Colorimetric Immunoassays of Tumor Markers
3.2.3.1. Colorimetric Assay Using Homogenous Growth of Au-NPs
3.2.3.2. Colorimetric Assay Using Aggregation of Au-NPs
3.2.3.2.1. scFv-Functionalized Au-NPs Based Assay
3.2.3.2.2. Colorimetric Bio-Barcode Assay
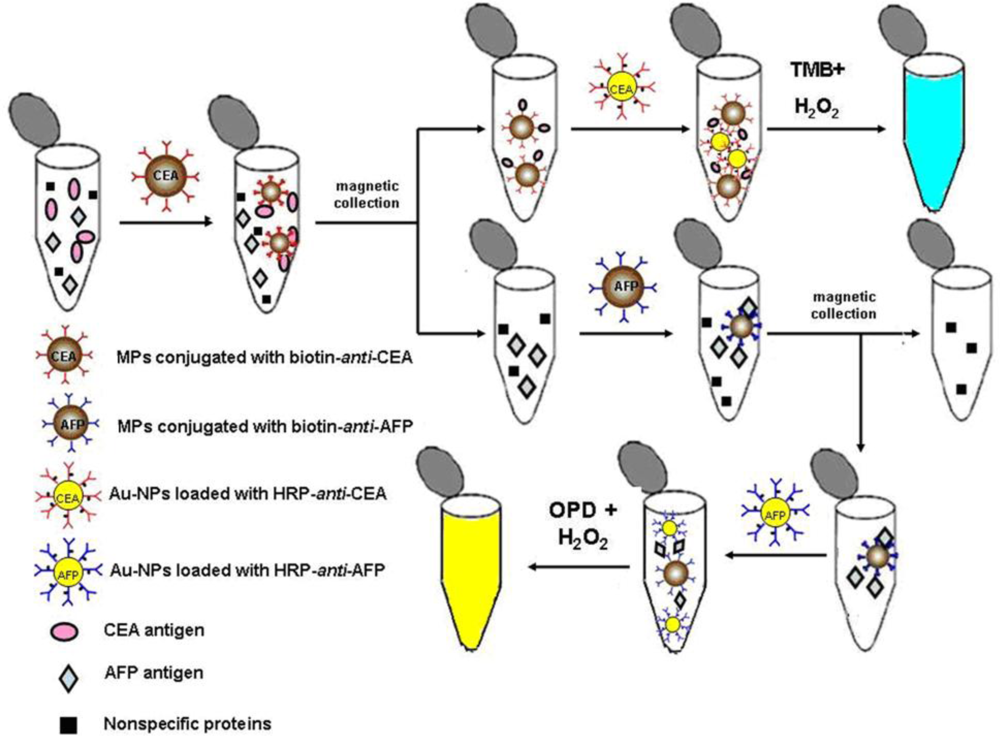
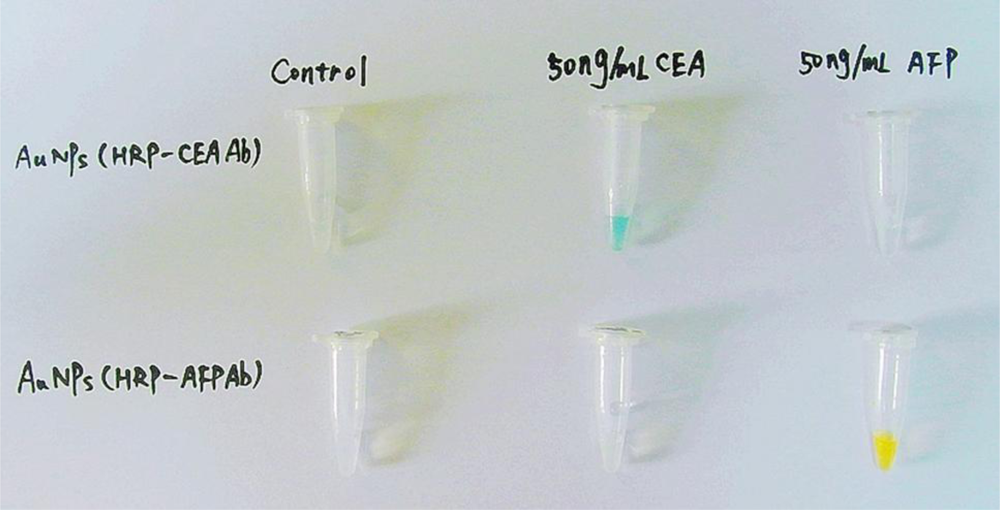
3.2.3.3. Colorimetric Assay using Enzymes Labeled Au-NPs
4. Results and Discussion
References
- World Healther Organization. Cancer. Available online: http://www.who.int/mediacentre/factsheets/fs297/en/ (accessed on 25 November 2007).
- Reid, BJ; Weinstein, WM; Lewin, KJ; Haggitt, RC; van Deventer, G; DenBesten, L; Rubin, CE. Endoscopic biopsy can detect high-grade dysplasia or early adenocarcinoma in Barrett’s esophagus without grossly recognizable neoplastic lesions. Gastroenterology 1988, 6, 81–90. [Google Scholar]
- Wahl, RL; Quint, LE; Greenough, RL; Meyer, CR; White, RI; Orringer, MB. Staging of mediastinal non-small cell lung cancer with FDG PET, CT, and fusion images: Preliminary prospective evaluation. Radiology 1994, 191, 371–377. [Google Scholar]
- Beyer, T; Townsend, DW; Brun, T; Kinahan, PE; Charron, M; Roddy, R; Jerin, J; Young, J; Byars, L; Nutt, R. A combined PET/CT scanner for clinical oncology. J. Nucl. Med 2000, 41, 1369–1379. [Google Scholar]
- Kircher, MF; Mahmood, U; King, RS; Weissleder, R; Josephson, L. A multimodal nanoparticle for preoperative magnetic resonance imaging and intraoperative optical brain tumor delineation. Cancer Res 2003, 63, 8122–8125. [Google Scholar]
- Choi, YE; Kwak, JW; Park, JW. Nanotechnology for early cancer detection. Sensors 2010, 10, 428–455. [Google Scholar]
- Safi, F; Kohler, I; Rottinger, E; Beger, H. The value of the tumor marker CA15-3 in diagnosing and monitoring breast cancer. Cancer 1991, 68, 574–582. [Google Scholar]
- Harris, L; Fritsche, H; Mennel, R; Norton, L; Ravdin, P; Taube, S; Somerfield, MR; Hayes, DF; Bast, RC, Jr. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J. Clin. Oncol 2007, 25, 5287–5312. [Google Scholar]
- Kumar, S; Mohan, A; Guleria, R. Biomarkers in cancer screening, research and detection: Present and future: A review. Biomarkers 2006, 11, 385–405. [Google Scholar]
- Hanash, S; Pitteri, S; Faca, V. Mining the plasma proteome for cancer biomarkers. Nature 2008, 452, 571–579. [Google Scholar]
- Chen, DS; Sung, JL. Serum alpha-fetoprotein in hepatocellular carcinoma. Cancer 1977, 40, 779–783. [Google Scholar]
- Canney, PA; Moore, M; Wilkinson, PM; James, RD. Ovarian cancer antigen CA125: A prospective clinical assessment of its role as a tumour marker. Br. J. Cancer 1984, 50, 765–769. [Google Scholar]
- Benchimol, S; Fuks, A; Jothy, S; Beauchemin, N; Shirota, K; Stanners, CP. Carcinoembryonic antigen, a human tumor marker, functions as an intercellular adhesion molecule. Cell 1989, 57, 327–334. [Google Scholar]
- Osborne, CK; Yochmowitz, MG; Knight, WA, 3rd; McGuire, WL. The value of estrogen and progesterone receptors in the treatment of breast cancer. Cancer 1980, 46, 2884–2888. [Google Scholar]
- Jacobsen, GK; Jacobsen, M. Alpha-fetoprotein (AFP) and human chorionic gonadotropin (HCG) in testicular germ cell tumours: A prospective immunohistochemical study. Acta Pathol. Microbiol. Immunol. Scand. A 1983, 91, 165–176. [Google Scholar]
- Horton, J. Her2 and Trastuzumab in breast cancer. Cancer Control 2001, 8, 103–110. [Google Scholar]
- Lilja, H; Ulmert, D; Vickers, AJ. Prostate-specific antigen and prostate cancer: Prediction, detection and monitoring. Nat. Rev. Cancer 2008, 8, 497–511. [Google Scholar]
- Stamey, TA; Yang, N; Hay, AR; McNeal, JE; Freiha, FS; Redwine, E. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N. Engl. J. Med 1987, 317, 909–916. [Google Scholar]
- Catalona, WJ; Smith, DS; Ratliff, TL; Dodds, KM; Coplen, DE; Yuan, JJ; Petros, JA; Andriole, GL. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N. Engl. J. Med 1991, 324, 1156–1161. [Google Scholar]
- Dhanasekaran, SM; Barrette, TR; Ghosh, D; Shah, R; Varambally, S; Kurachi, K; Pienta, KJ; Rubin, MA; Chinnaiyan, AM. Delineation of prognostic biomarkers in prostate cancer. Nature 2001, 412, 822–826. [Google Scholar]
- Bates, SE. Clinical applications of serum tumor markers. Ann. Int. Med 1991, 115, 623–638. [Google Scholar]
- Carter, P; Presta, L; Gorman, CM; Ridgway, JB; Henner, D; Wong, WL; Rowland, AM; Kotts, C; Carver, ME; Shepard, HM. Humanization of an anti-p185HER2 antibody for human cancer therapy. Proc. Natl. Acad. Sci. USA 1992, 89, 4285–4289. [Google Scholar]
- Bast, RC; Bates, S; Bredt, AB; Desch, CE; Fritsche, H; Fues, L; Hayes, DF; Kemeny, NE; Kragen, M; Jessup, J; Locker, GY; Macdonald, JS; Mennel, RG; Norton, L; Ravdin, P; Smith, TJ; Taube, S; Winn, RJ. Clinical practice guidelines for the use of tumor markers in breast and colorectal cancer. J. Clin. Oncol 1996, 14, 2843–2877. [Google Scholar]
- Sok, D; Clarizia, L; Farris, L; McDonald, M. Novel fluoroimmunoassay for ovarian cancer biomarker CA-125. Anal. Bioanal. Chem 2009, 393, 1521–1523. [Google Scholar]
- Wilson, MS; Nie, W. Multiplex measurement of seven tumor markers using an electrochemical protein chip. Anal. Chem 2006, 78, 6476–6483. [Google Scholar]
- Li, C; Curreli, M; Lin, H; Lei, B; Ishikawa, FN; Datar, R; Cote, RJ; Thompson, ME; Zhou, C. Complementary detection of prostate-specific antigen using In2O3 nanowires and carbon nanotubes. J. Am. Chem. Soc 2005, 127, 12484–12485. [Google Scholar]
- Nam, JM; Thaxton, CS; Mirkin, CA. Nanoparticle-based bio–barcodes for the ultrasensitive detection of proteins. Science 2003, 301, 1884–1886. [Google Scholar]
- Zheng, G; Patolsky, F; Cui, Y; Wang, WU; Lieber, CM. Multiplexed electrical detection of cancer markers with nanowire sensor arrays. Nat. Biotechnol 2005, 23, 1294–1301. [Google Scholar]
- Nam, JM; Wise, AR; Groves, JT. Colorimetric bio-barcode amplification assay for cytokines. Anal. Chem 2005, 77, 6985–6988. [Google Scholar]
- Zhao, Y; Zhao, X; Hu, J; Xu, M; Zhao, W; Sun, L; Zhu, C; Xu, H; Gu, Z. Encoded porous beads for label-free multiplex detection of tumor markers. Adv. Mater 2008, 20, 1–4. [Google Scholar]
- Liu, X; Dai, Q; Austin, L; Coutts, J; Knowles, G; Zou, J; Chen, H; Huo, Q. A One-step homogeneous immunoassay for cancer biomarker detection using gold nanoparticle probes coupled with dynamic light scattering. J. Am. Chem. Soc 2008, 130, 2780–2782. [Google Scholar]
- Stoeva, SI; Lee, JS; Smith, JE; Rosen, ST; Mirkin, CA. Multiplexed detection of protein cancer markers with biobarcoded nanoparticle probes. J. Am. Chem. Soc 2006, 128, 8378–8379. [Google Scholar]
- Oh, BK; Nam, JM; Lee, SW; Mirkin, CA. A fluorophore-based bio-barcode amplification assay for proteins. Small 2006, 2, 103–108. [Google Scholar]
- Wu, G; Datar, RH; Hansen, KM; Thundat, T; Cote, RJ; Majumdar, A. Bioassay of prostate-specific antigen (PSA) using microcantilevers. Nat. Biotechnol 2001, 19, 856–860. [Google Scholar]
- Mani, V; Chikkaveeraiah, BV; Patel, V; Gutkind, JS; Rusling, JF. Ultrasensitive immunosensor for cancer biomarker proteins using gold nanoparticle film electrodes and multienzyme-particle amplification. ACS Nano 2009, 3, 585–594. [Google Scholar]
- Yu, X; Munge, B; Patel, V; Jensen, G; Bhirde, A; Gong, JD; Kim, SN; Gillespie, J; Gutkind, JS; Papadimitrakopoulos, F; Rusling, JF. Carbon nanotube amplification strategies for highly sensitive immunodetection of cancer biomarkers. J. Am. Chem. Soc 2006, 128, 11199–11205. [Google Scholar]
- Grubisha, DS; Lipert, RJ; Park, HY; Driskell, J; Porter, MD. Femtomolar detection of prostate-specific antigen: An immunoassay based on surface-enhanced Raman scattering and immunogold labels. Anal. Chem 2003, 75, 5936–5943. [Google Scholar]
- Cao, C; Li, X; Lee, J; Sim, SJ. Homogenous growth of gold nanocrystals for quantification of PSA protein biomarker. Biosens. Bioelectron 2009, 24, 1292–1297. [Google Scholar]
- Ao, L; Gao, F; Pan, B; He, R; Cui, D. Fluoroimmunoassay for antigen based on fluorescence quenching signal of gold nanoparticles. Anal. Chem 2006, 78, 1104–1106. [Google Scholar]
- Lee, JR; Lee, J; Kim, SK; Kim, KP; Park, HS; Yeo, WS. Mass spectrometry signal amplification method for attomolar detection of antigens using small-molecule-tagged gold microparticles. Angew. Chem. Int. Ed 2008, 47, 9518–9521. [Google Scholar]
- Li, N; Yuan, R; Chai, Y; Chen, S; An, H; Li, W. New antibody immobilization strategy based on gold nanoparticles and azure I/multi-walled carbon nanotube composite membranes for an amperometric enzyme immunosensor. J. Phys. Chem. C 2007, 111, 8443–8450. [Google Scholar]
- Bi, S; Zhou, H; Zhang, S. Multilayers enzyme-coated carbon nanotubes as biolabel for ultrasensitive chemiluminescence immunoassay of cancer biomarker. Biosens. Bioelectron 2009, 24, 2961–2966. [Google Scholar]
- Lee, YM; Jeong, Y; Kang, HJ; Chung, SJ; Chung, BH. Cascade enzyme-linked immunosorbent assay (CELISA). Biosens. Bioelectron 2009, 25, 332–337. [Google Scholar]
- Zhou, WH; Zhu, CL; Lu, CH; Guo, X; Chen, F; Yang, HH; Wang, X. Amplified detection of protein cancer biomarkers using DNAzyme functionalized nanoprobes. Chem. Commun 2009, 44, 6845–6847. [Google Scholar]
- Wang, J; Cao, Y; Xu, Y; Li, G. Colorimetric multiplexed immunoassay for sequential detection of tumor markers. Biosens. Bioelectron 2009, 25, 532–536. [Google Scholar]
- Fu, Z; Liu, H; Ju, H. Flow-through multianalyte chemiluminescent immunosensing system with designed substrate zone-resolved technique for sequential detection of tumor markers. Anal. Chem 2006, 78, 6999–7005. [Google Scholar]
- Ou, C; Yuan, R; Chai, Y; Tang, M; Chai, R; He, X. A novel amperometric immunosensor based on layer-by-layer assembly of gold nanoparticlesmulti-walled carbon nanotubes-thionine multilayer films on polyelectrolyte surface. Anal. Chim. Acta 2007, 603, 205–213. [Google Scholar]
- Chon, H; Lee, S; Son, SW; Oh, CH; Choo, J. Highly sensitive immunoassay of lung cancer marker carcinoembryonic antigen using surface-enhanced raman scattering of hollow gold nanosperes. Anal. Chem 2009, 81, 3029–3034. [Google Scholar]
- Liu, M; Jia, C; Huang, Y; Lou, X; Yao, S; Jin, Q; Zhao, J; Xiang, J. Highly sensitive protein detection using enzyme-labeled gold nanoparticle probes. Analyst 2010, 135, 327–331. [Google Scholar]
- Knecht, MR; Sethi, M. Bio-inspired colorimetric detection of Hg2+ and Pb2+ heavy metal ions using Au nanoparticles. Anal. Bioanal. Chem 2009, 394, 33–46. [Google Scholar]
- Ohno, Y. CIE fundamentals for color measurements. IS&T NIP16 Intl. Conf. on Digital Printing Technologies: Vancouver, Canada, 2000; pp. 540–545. [Google Scholar]
- Zangar, RC; Daly, DS; White, AM. ELISA microarray technology as a high-throught system for cancer biomarker validation. Expert Rev. Proteomics 2006, 3, 37–44. [Google Scholar]
- Lequin, RM. Enzyme immunoassay (EIA)/enzyme-linked immunosorbent assay (ELISA). Clin. Chem 2005, 51, 2415–2418. [Google Scholar]
- Leng, S; McElhaney, J; Walston, J; Xie, D; Fedarko, N; Kuchel, G. Elisa and multiplex technologies for cytokine measurement in inflammation and aging research. J. Gerontol. A Biol. Sci. Med. Sci 2008, 63, 879–884. [Google Scholar]
- Cook, DB; Bustamam, AA; Brotherick, I; Shenton, BK; Self, CH. Lectin ELISA for the c-erb-B2 tumor marker protein p185 in patients with breast cancer and controls. Clin. Chem 1999, 45, 292–295. [Google Scholar]
- Zehentner, BK; Persing, DH; Deme, A; Toure, P; Hawes, SE; Brooks, L; Feng, Q; Hayes, DC; Critichlow, CW; Houghton, RL; Kiviat, NB. Mammaglobin as a novel breast cancer biomarker: Multigene reverse transcription-PCR assay and sandwich ELISA. Clin. Chem 2004, 50, 2069–2076. [Google Scholar]
- Prasad, PV; Chaube, SK; Shrivastav, TG; Kumari, GL. Development of colorimetric enzyme-linked immunosorbent assay for human chorionic gonadotropin. J. Immunoassay Immunochem 2006, 27, 15–30. [Google Scholar]
- Ambrosi, A; Airò, F; Merkoçi, A. Enhanced gold nanoparticle based ELISA for a breast cancer biomarker. Anal. Chem 2010, 82, 1151–1156. [Google Scholar]
- Liu, Y; Wang, H; Huang, J; Yang, J; Liu, B; Yang, P. Microchip-based ELISA strategy for the detection of low-level disease biomarker in serum. Anal. Chim. Acta 2009, 650, 77–82. [Google Scholar]
- Ferrari, M. Cancer nanotechnology: Opportunities and challenges. Nat. Rev. Cancer 2005, 5, 161–171. [Google Scholar]
- Chen, H; Jiang, C; Yu, C; Zhang, S; Liu, B; Kong, J. Protein chips and nanomaterials for application in tumor marker immunoassays. Biosens. Bioelectron 2009, 24, 3399–3411. [Google Scholar]
- Gomez-Hens, A; Fernandez-Romero, JM; Aguilar-Caballos, MP. Control of tumor markers using nanotechnology. Mini-Rev. Med. Chem 2009, 9, 1064–1074. [Google Scholar]
- Kim, D; Daniel, WL; Mirkin, CA. Microarray-based multiplexed scanometric immunoassay for protein cancer markers using gold nanoparticle probes. Anal. Chem 2009, 81, 9183–9187. [Google Scholar]
- Ling, J; Li, YF; Huang, CZ. Visual sandwich immunoassay system on the basis of plasmon resonance scattering signals of silver nanoparticles. Anal. Chem 2009, 81, 1707–1714. [Google Scholar]
- Piao, Y; Lee, D; Kim, J; Kim, J; Hyeon, T; Kim, HS. High performance immunoassay using immobilized enzyme in nanoporous carbon. Analyst 2009, 134, 926–932. [Google Scholar]
- Lu, W; Arumugam, SR; Senapati, D; Singh, AK; Arbneshi, T; Khan, SA; Yu, H; Ray, PC. Multifunctional oval-shaped gold nanoparticle-based selective detection of breast cancer cells using simple colorimetric and highly sensitive two photon scattering assay. ACS Nano 2010, 4, 1739–1749. [Google Scholar]
- Tan, YN; Su, X; Liu, ET; Thomsen, JS. Gold-nanoparticle-based assay for instantaneous detection of nuclear hormone receptor-response elements interactions. Anal. Chem 2010, 82, 2759–2765. [Google Scholar]
- Nam, JM; Jang, KJ; Groves, JT. Detection of proteins using a colorimetric bio-barcode assay. Nat. Protoc 2007, 2, 1438–1444. [Google Scholar]
- Liu, Y; Liu, Y; Mernaugh, RL; Zeng, X. Single chain fragment variable recombinant antibody functionalized gold nanoparticles for a highly sensitive colorimetric immunoassay. Biosens. Bioelectron 2009, 24, 2853–2857. [Google Scholar]
- Liu, M; Jia, C; Jin, Q; Lou, X; Yao, S; Xiang, J; Zhao, J. Novel colorimetric enzyme immunoassay for the detection of carcinoembryonic antigen. Talanta 2010, 81, 1625–1629. [Google Scholar]
- de Dios, AS; Díaz-García, ME. Multifunctional nanoparticles: Analytical prospects. Anal. Chim. Acta 2010, 666, 1–22. [Google Scholar]
- Stanciu, L; Won, YH; Ganesana, M; Andreescu, S. Magnetic Particle-Based Hybrid Platforms for Bioanalytical Sensors. Sensors 2009, 9, 2976–2999. [Google Scholar]
- Hsing, IM; Xu, Y; Zhao, WT. Micro- and nano-magnetic particles for applications in biosensing. Electroanalysis 2007, 19, 755–768. [Google Scholar]
- Sandwich ELISA Protocol. General procedure and tips for Sandwich ELISA including details of how to find matched pair antibodies. Abcam: Hong Kong, China. Available at: http://www.abcam.cn/index.html?pageconfig=resource&rid=11422 (accessed on 25 November 2010).
- Huang, CC; Huang, YF; Cao, Z; Tan, W; Chang, HT. Aptamer-modified gold nanoparticles for colorimetric determination of platelet-derived growth factors and their receptors. Anal. Chem 2005, 77, 5735–5741. [Google Scholar]
- Faulk, WP; Taylor, GM. An immunocolloid method for the electron microscope. Immunochemistry 1971, 8, 1081–1083. [Google Scholar]
- Qian, X; Peng, XH; Ansari, DO; Yin-Goen, Q; Chen, GZ; Shin, DM; Yang, L; Young, AN; Wang, MD; Nie, S. In vivo tumor targeting and spectroscopic detection with surface-enhanced Raman nanoparticle tags. Nat. Biotechnol 2008, 26, 83–90. [Google Scholar]
- Niemeyer, CM; Ceyhan, B. DNA-directed functionalization of colloidal gold with proteins. Angew. Chem. Int. Ed 2001, 40, 3685–3688. [Google Scholar]
- Chen, YH; Tsai, CY; Huang, PY; Chang, MY; Cheng, PC; Chou, CH; Chen, DH; Wang, CR; Shiau, AL; Wu, CL. Methotrexate conjugated to gold nanoparticles inhibits tumor growth in a syngeneic lung tumor model. Mol. Pharm 2007, 4, 713–722. [Google Scholar]
- Ferreira, CS; Papamichael, K; Guilbault, G; Schwarzacher, T; Gariepy, J; Missailidis, S. DNA aptamers against the MUC1 tumour marker: Design of aptamer-antibody sandwich ELISA for the early diagnosis of epithelial tumours. Anal. Bioanal. Chem 2008, 390, 1039–1050. [Google Scholar]
- Lupold, SE; Hicke, BJ; Lin, Y; Coffey, DS. Identification and characterization of nuclease-stabilized RNA molecules that bind human prostate cancer cells via the prostate-specific membrane antigen. Cancer Res 2002, 62, 4029–4033. [Google Scholar]
- Kim, E; Seo, S; Seo, ML; Jung, JH. Functionalized monolayers on mesoporous silica and on titania nanoparticles for mercuric sensing. Analyst 2010, 135, 149–156. [Google Scholar]
- Song, Y; Wang, X; Zhao, C; Qu, K; Ren, J; Qu, X. Label-free colorimetric detection of single nucleotide polymorphism by using single-walled carbon nanotube intrinsic peroxidase-like activity. Chem. Eur. J 2010, 16, 3617–3621. [Google Scholar]
- Chen, Z; He, Y; Luo, S; Lin, H; Chen, Y; Sheng, P; Li, J; Chen, B; Liu, C; Cai, Q. Label-free colorimetric assay for biological thiols based on ssDNA/silver nanoparticle system by salt amplification. Analyst 2010, 135, 1066–1069. [Google Scholar]
- Wu, J; Fu, Z; Yan, F; Ju, H. Biomedical and clinical applications of immunoassays and immunosensors for tumor markers. Trends Anal. Chem 2007, 26, 679–688. [Google Scholar]
| Tumor Markers | Related Cancers | Usual Sample | Refs. |
|---|---|---|---|
| AFP (Alpha-fetoprotein) | Liver, germ cell cancer of ovaries or testes | Blood | [11] |
| CA 15-3 (Cancer antigen 15-3) | Breast | Blood | [7] |
| CA-125 (Cancer antigen 125) | Ovarian | Blood | [12] |
| CEA (Carcinoembryonic antigen) | Colorectal, breast, thyroid et al. | Blood | [13] |
| Estrogen receptors | Breast | Tissue | [14] |
| hCG (Human chorionic gonadotropin) | Testicular and trophoblastic disease | Blood, urine | [15] |
| Her-2/neu | Breast | Tissue | [16] |
| Progesterone receptors | Breast | Tissue | [14] |
| PSA (Prostate specific antigen) | Prostate | Blood | [17,18] |
| Tumor markers | Biosensor principle | Assay principle | Limit of detection | Refs. |
|---|---|---|---|---|
| PSA | Fluorescence | Fluorophore-based bio-barcode amplification method | 30 nM | [33] |
| PSA | Microcantilever | Microcantilever | 2 nM | [34] |
| PSA | Electrochemistry | Using gold nanoparticle film electrodes and multienzyme-particle amplification | 5 fM | [35] |
| PSA | Electrochemistry | Carbon nanotube amplification strategies | 40 fM | [36] |
| PSA | Surface-Enhanced Raman Scattering | Immunoassay based on Surface-Enhanced Raman Scattering and immunogold labels | 30 fM | [37] |
| PSA | Colorimetry | Homogenous growth of gold nanocrystals | 10 fM | [38] |
| AFP | Fluorescence | Fluorescence quenching signal of gold nanoparticles | 0.17 nM | [39] |
| AFP | Mass spectrometry | Mass spectrometry signal amplification using small-molecule tagged gold microparticles | 1 nM | [40] |
| AFP | Electrochemistry | Amperometric enzyme immunosensor based on gold nanoparticles and multi-walled carbon nanotube composite membranes | 0.6 pM | [41] |
| AFP | Chemiluminescence | Multilayers enzyme-coated carbon nanotubes as label | 0.1 pM | [42] |
| AFP | Colorimetry | Cascade enzyme-linked immunosorbent assay | 0.1 pM | [43] |
| AFP | Colorimetry | DNAzyme functionalized nano-probes | 1.4 pM | [44] |
| CEA, AFP | Colorimetry | Colorimetric multiplexed immunoassay based on gold nanoparticles | 0.02 ng/mL; 0.1 pM | [45] |
| CEA | Chemiluminescence | Flow-through multianalyte system with substrate zone-resolved technique | 0.6 ng/mL | [46] |
| CEA | Electrochemistry | Layer-by-layer assembly of gold nanoparticles-multi-walled carbon nanotubes-thionine multilayer films | 0.01 ng/mL | [47] |
| CEA | Surface-Enhanced Raman Scattering | Surface-Enhanced Raman Scattering of hollow gold nanospheres | 0.01 ng/mL | [48] |
| CEA | Colorimetry | Enzyme-labeled gold nanoparticle probes | 0.012 ng/mL | [49] |
© 2010 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Yin, Y.; Cao, Y.; Xu, Y.; Li, G. Colorimetric Immunoassay for Detection of Tumor Markers. Int. J. Mol. Sci. 2010, 11, 5077-5094. https://doi.org/10.3390/ijms11125077
Yin Y, Cao Y, Xu Y, Li G. Colorimetric Immunoassay for Detection of Tumor Markers. International Journal of Molecular Sciences. 2010; 11(12):5077-5094. https://doi.org/10.3390/ijms11125077
Chicago/Turabian StyleYin, Yongmei, Ya Cao, Yuanyuan Xu, and Genxi Li. 2010. "Colorimetric Immunoassay for Detection of Tumor Markers" International Journal of Molecular Sciences 11, no. 12: 5077-5094. https://doi.org/10.3390/ijms11125077




