Journal Description
Journal of Cardiovascular Development and Disease
Journal of Cardiovascular Development and Disease
is an international, scientific, peer-reviewed, open access journal on cardiovascular medicine published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, PMC, Embase, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q2 (Cardiac and Cardiovascular Systems) / CiteScore - Q2 (General Pharmacology, Toxicology and Pharmaceutics )
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 25.7 days after submission; acceptance to publication is undertaken in 2.8 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
2.4 (2023);
5-Year Impact Factor:
2.6 (2023)
Latest Articles
Non-Traditional Cardiovascular Risk Factors: Tailored Assessment and Clinical Implications
J. Cardiovasc. Dev. Dis. 2025, 12(5), 171; https://doi.org/10.3390/jcdd12050171 - 28 Apr 2025
Abstract
Non-traditional cardiovascular risk factors (RFs) are increasingly emerging as important modifiers of cardiovascular risk (CVR), offering insights beyond traditional metrics like hypertension, diabetes, and dyslipidemia. These include novel biomarkers, chronic conditions (e.g., chronic kidney disease and chronic obstructive pulmonary disease), environmental exposures, chronic
[...] Read more.
Non-traditional cardiovascular risk factors (RFs) are increasingly emerging as important modifiers of cardiovascular risk (CVR), offering insights beyond traditional metrics like hypertension, diabetes, and dyslipidemia. These include novel biomarkers, chronic conditions (e.g., chronic kidney disease and chronic obstructive pulmonary disease), environmental exposures, chronic inflammation, infections, psychosocial factors, and sex-specific conditions, all of which influence the prediction, management, and outcomes of cardiovascular disease (CVD). These additional RFs may impact on CVD prediction and add valid information during tailored patient assessment and management. Therefore, a careful assessment of both traditional and non-traditional cardiovascular RFs, with a personalized treatment, could dramatically reduce the total CVD burden. Nevertheless, further research is needed to precisely estimate the magnitude of their impact as risk and prognosis modifiers in order to be included in future risk charts. This review provides a critical analysis of non-traditional RFs, their pathophysiological mechanisms, and their implications for personalized care. Integrating these factors into CVR assessment can reclassify patient risk categories, optimize therapeutic strategies, and improve prognosis. However, further research is needed to refine their inclusion in risk charts and evaluate their impact on public health outcomes. A tailored, multidisciplinary approach is essential to reduce the burden of CVD and associated mortality.
Full article
(This article belongs to the Special Issue Cardiovascular Risk Factors: Focus on Epidemiology and Clinical Consequences)
►
Show Figures
Open AccessReview
Treatment Options in Isolated Atherosclerotic Popliteal Artery Disease
by
Stephanie Rassam and Raphaël Coscas
J. Cardiovasc. Dev. Dis. 2025, 12(5), 170; https://doi.org/10.3390/jcdd12050170 - 27 Apr 2025
Abstract
Isolated popliteal artery (PA) lesions account for around 1% of lower limb revascularisations. Whatever treatment modality is chosen, the effects on the artery during knee flexion must be considered. The decision between a less invasive endovascular treatment (EVT) and traditional open interventions remains
[...] Read more.
Isolated popliteal artery (PA) lesions account for around 1% of lower limb revascularisations. Whatever treatment modality is chosen, the effects on the artery during knee flexion must be considered. The decision between a less invasive endovascular treatment (EVT) and traditional open interventions remains complex due to anatomical, biomechanical, and pathophysiological considerations and the varying aetiology of PA lesions. Available data remain limited, making it more challenging to decide on the most effective and durable treatment approach. Nowadays, when EVT is planned, several non-stenting techniques are available, making a “leave-nothing-behind strategy” possible after adequate vessel preparation. If stent implantation is required, self-expanding vasculomimetic stents are preferred due to their ability to provide flexibility and resist compression during motion. This narrative review discusses the available treatment options, challenges, and specific considerations for isolated PA disease, highlighting the need for large-scale, high-quality studies to provide more robust evidence on the optimal treatment approach.
Full article
(This article belongs to the Special Issue Management and Challenges in Peripheral Arterial Disease)
►▼
Show Figures
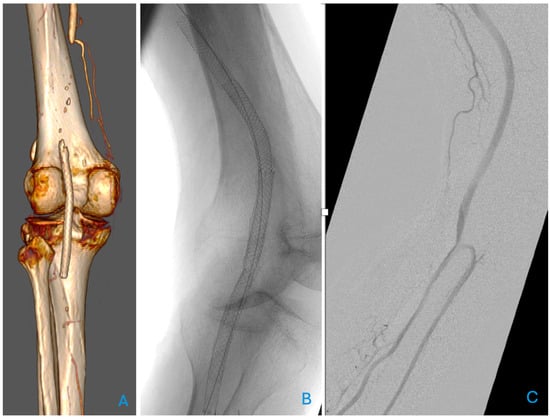
Figure 1
Open AccessReview
Lipoprotein(a): Assessing the Current Knowledge and Gaps in Screening and Treatment—A Narrative Review
by
Octavian Amaritei, Oana Laura Mierlan, Cristian Gutu and Gabriela Gurau
J. Cardiovasc. Dev. Dis. 2025, 12(5), 169; https://doi.org/10.3390/jcdd12050169 - 26 Apr 2025
Abstract
Atherosclerotic cardiovascular disease (ASCVD) has long been screened using the traditional lipid profile, mainly focusing on LDL cholesterol. However, despite growing evidence supporting lipoprotein(a) [Lp(a)] as an independent risk factor involved in atherosclerosis, its clinical use remains limited. This review examines the reasons
[...] Read more.
Atherosclerotic cardiovascular disease (ASCVD) has long been screened using the traditional lipid profile, mainly focusing on LDL cholesterol. However, despite growing evidence supporting lipoprotein(a) [Lp(a)] as an independent risk factor involved in atherosclerosis, its clinical use remains limited. This review examines the reasons behind the limited use of Lp(a) screening in clinical practice, assessing its role in cardiovascular risk, comparing it to traditional lipid markers and evaluating current assessment methods. It also explores existing and emerging treatments, including gene-silencing therapies, for managing elevated Lp(a) levels. One in four clinicians does not routinely check Lp(a) levels, which proves a lack of awareness amongst them. The reasons for that are implied to be that the cost is too high and that available treatments are scarce. The traditional lipid profile, including LDL, high-density lipoprotein (HDL) and triglycerides, continues to be the gold standard for CV risk assessment. One limitation of using Lp(a) in clinical practice is the significant variability in apo(a) sizes, which results from the presence of multiple isoforms determined by the number of kringle domains. This structural diversity poses challenges in standardizing measurement methods, affecting the accuracy and comparability of results. While statins have a minimal impact on Lp(a), PCSK9-i lowers its levels by 20–25%, although this class is not prescribed primarily for this reason. Lastly, gene-silencing therapies, which achieve the greatest reduction in Lp(a) levels, are still in phase III trials, and there is still a need to examine whether this reduction translates into CV benefits. These limitations should not discourage further research, because ASCVD’s complexity requires a more tailored approach. Current lipid-lowering therapy still fails in a minority of cases, as evidenced by new-onset cardiovascular events in patients with well-controlled LDL levels. There is a need for future interventional studies to assess whether a reduction in Lp(a) by PCSK9-i really translates into CV benefits, independent of LDL.
Full article
(This article belongs to the Topic Biomarkers in Cardiovascular Disease—Chances and Risks, 2nd Volume)
►▼
Show Figures
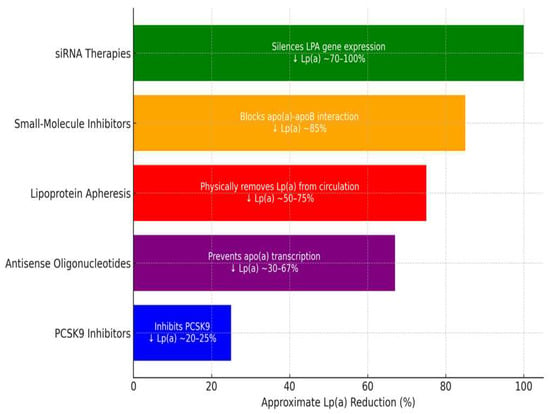
Figure 1
Open AccessReview
Predicting the Outcomes of External Direct Current Cardioversion for Atrial Fibrillation: A Narrative Review of Current Evidence
by
Ibrahim Antoun, Georgia R. Layton, Ahmed Abdelrazik, Mahmoud Eldesouky, Sherif Altoukhy, Mustafa Zakkar, Riyaz Somani and G. André Ng
J. Cardiovasc. Dev. Dis. 2025, 12(5), 168; https://doi.org/10.3390/jcdd12050168 - 25 Apr 2025
Abstract
Atrial fibrillation (AF) is the most common sustained arrhythmia associated with significant morbidity and mortality. External direct current cardioversion (DCCV) is a cornerstone intervention for rhythm control in AF; however, its success is influenced by various patient-specific and procedural factors. This review examines
[...] Read more.
Atrial fibrillation (AF) is the most common sustained arrhythmia associated with significant morbidity and mortality. External direct current cardioversion (DCCV) is a cornerstone intervention for rhythm control in AF; however, its success is influenced by various patient-specific and procedural factors. This review examines the predictors of DCCV success and AF recurrence with specific focus upon demographics, biochemical, cardiovascular imaging, and P-wave parameters and their likely ability to predict procedural outcomes. Demographic factors such as age, sex, and comorbidities influence DCCV outcomes, with prolonged AF duration, obesity, and heart failure being associated with higher failure rates. Elevated biochemical markers of inflammation and fibrosis, including C-reactive protein, galectin-3, and Type III procollagen-N-peptide, were predictive of poor outcomes. Imaging parameters, particularly left atrial (LA) volume and strain, emerged as critical indicators of atrial remodelling and DCCV failure. Increased P-wave duration and dispersion on electrocardiography were associated with an increased risk of recurrence. Biphasic waveforms and antiarrhythmic drugs, such as amiodarone and flecainide, improved cardioversion success. The predictors of DCCV success and recurrence reflect the interplay of structural, biochemical, and electrical remodelling in AF. Integrating these parameters into clinical practice can guide individualised patient management and improve outcomes. Further research is needed to validate these predictors and enhance precision medicine approaches in DCCV.
Full article
(This article belongs to the Special Issue Extensive Approach to Atrial Fibrillation: Background and Future Perspectives)
►▼
Show Figures
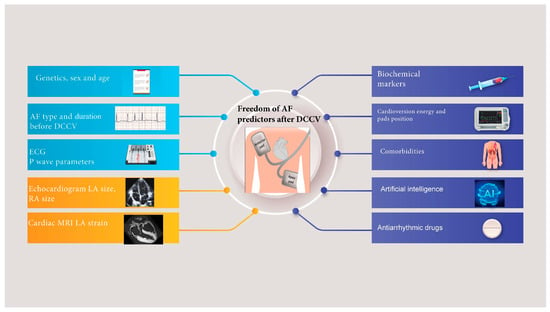
Figure 1
Open AccessArticle
Beyond the Echo: Is Comprehensive Vascular Exploration Valuable in Cases of Non-Syndromic Thoracic Aortic Aneurysms or Bicuspid Aortic Valve?
by
Austin Saugstad, Srekar Ravi, George Bcharah, Christine E. Firth, Hend Bcharah, Hussein Abdul Nabi, Hoang Nhat Pham, Ramzi Ibrahim, Sant J. Kumar, Mahmoud Abdelnabi, Linnea M. Baudhuin, Yuxiang Wang, Mayowa A. Osundiji and Fadi Shamoun
J. Cardiovasc. Dev. Dis. 2025, 12(5), 167; https://doi.org/10.3390/jcdd12050167 - 24 Apr 2025
Abstract
Bicuspid aortic valve (BAV) and thoracic aortic aneurysms and dissections (TAAD) are recognized in syndromic connective tissue diseases (CTD), but most cases occur sporadically. The extent to which non-syndromic BAV or TAAD predisposes to additional arteriopathies, particularly in younger individuals, remains unclear. We
[...] Read more.
Bicuspid aortic valve (BAV) and thoracic aortic aneurysms and dissections (TAAD) are recognized in syndromic connective tissue diseases (CTD), but most cases occur sporadically. The extent to which non-syndromic BAV or TAAD predisposes to additional arteriopathies, particularly in younger individuals, remains unclear. We retrospectively analyzed 1438 patients (mean age = 48.0, 67.7% female), excluding those with CTDs. Participants were ≤60 years old and categorized by the presence of BAV and/or TAAD. We examined co-existing arterial pathologies, including fibromuscular dysplasia, spontaneous coronary artery dissection, abdominal aortic aneurysms (AAA), mesenteric, peripheral extremity, and carotid/cerebral arteriopathies. Overall, 44.6% had either BAV or TAAD, and 27.2% had multiple arteriopathies. While vascular diseases were frequently noted, odds ratios demonstrated no significantly increased risk of extra-aortic arteriopathies in the BAV or TAAD cohorts. AAA exhibited a non-significant trend toward higher prevalence in TAAD patients. These findings support current guidelines recommending targeted imaging (transthoracic echocardiography of the aortic root and ascending aorta) over comprehensive “head-to-pelvis” screening for non-syndromic BAV or TAAD patients without additional risk factors. Ongoing genetic analyses may elucidate whether particular variants predispose to multi-site aneurysms or dissections. Consequently, targeted surveillance remains appropriate, with broader imaging reserved for patients with genetic or clinical indicators of higher risk.
Full article
(This article belongs to the Special Issue Models and Methods for Computational Cardiology: 2nd Edition)
►▼
Show Figures
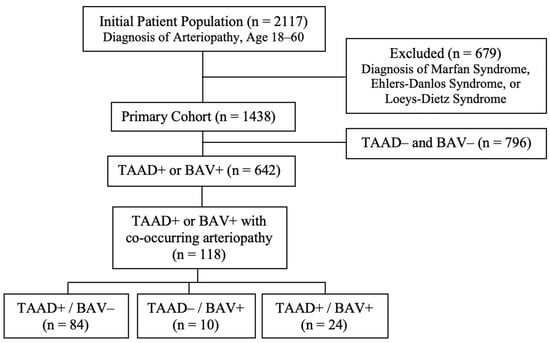
Figure 1
Open AccessArticle
Impact of the Pre-Operative Standardized Nutritional Protocol in Infants with Congenital Heart Disease (CHD)
by
Patrick Zacharias, Jenna Blinci, Ruthie Shenoy, Jesse Lee and Yogen Singh
J. Cardiovasc. Dev. Dis. 2025, 12(5), 166; https://doi.org/10.3390/jcdd12050166 - 23 Apr 2025
Abstract
Neonates with congenital heart disease (CHD) are at increased risk of growth failure and necrotizing enterocolitis (NEC), making nutritional management crucial for their outcomes. This study aimed to evaluate the impact of a standardized feeding protocol on growth and NEC incidence in CHD
[...] Read more.
Neonates with congenital heart disease (CHD) are at increased risk of growth failure and necrotizing enterocolitis (NEC), making nutritional management crucial for their outcomes. This study aimed to evaluate the impact of a standardized feeding protocol on growth and NEC incidence in CHD infants. A retrospective study was conducted at a tertiary care center, including neonates diagnosed with CHDs from January 2020 to March 2023. Patients were divided into two groups: those receiving the standardized feeding protocol (protocol group, n = 12) and those who did not (non-protocol group, n = 39). Key metrics such as growth velocity at discharge, anthropometric z score changes at discharge since birth, days to full enteral feeds, NEC incidence, and length of stay were analyzed. Statistical comparisons were made using two-tailed Mann-Whitney test and chi-squared tests. The NEC incidence was 10% in the non-protocol group and 0% in the protocol group (p = 0.25), with no significant difference. All anthropometric growth markers at the time of discharge differed between the groups, with the protocol group demonstrating favorable outcomes across all measured variables; however, these differences did not reach statistical significance. The time to reach full enteral feeds was shorter (8.5 days vs. 11 days; p = 0.22), and length of stay was shorter in the protocol group (17 days vs. 23 days; p = 0.14), although neither was statistically significant. Although the protocol group showed trends towards reduced NEC and improved growth, this was not statistically significant, which could have been because of the small sample size. Our findings suggest that a standardized feeding protocol may reduce the time to full enteral feeds and hospital stay, but further large-scale studies are needed to confirm these results.
Full article
(This article belongs to the Section Pediatric Cardiology and Congenital Heart Disease)
►▼
Show Figures
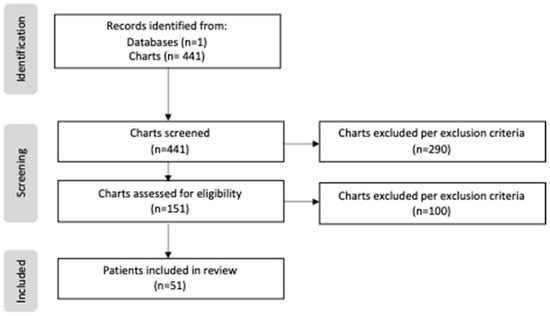
Figure 1
Open AccessArticle
Early Experience with Acuson AcuNav 4D-ICE to Guide Transcatheter Tricuspid Edge-to-Edge Repair: 4D Intracardiac Echocardiography Compared to Transesophageal Echocardiography
by
Matteo Biroli, Fabio Fazzari, Francesco Cannata, Vincenzo De Peppo, Cristina Ferrari, Carlo Maria Giacari, Marco Gennari, Paolo Olivares, Manuela Muratori, Mauro Pepi, Gianluca Pontone and Federico De Marco
J. Cardiovasc. Dev. Dis. 2025, 12(5), 165; https://doi.org/10.3390/jcdd12050165 - 23 Apr 2025
Abstract
Tricuspid regurgitation is a common valvular disease associated with high morbidity and mortality if left untreated. While surgery has been the standard intervention, transcatheter tricuspid edge-to-edge repair (T-TEER) has emerged as an alternative for high-risk surgical candidates. Transesophageal echocardiography (TEE) is the gold-standard
[...] Read more.
Tricuspid regurgitation is a common valvular disease associated with high morbidity and mortality if left untreated. While surgery has been the standard intervention, transcatheter tricuspid edge-to-edge repair (T-TEER) has emerged as an alternative for high-risk surgical candidates. Transesophageal echocardiography (TEE) is the gold-standard imaging modality for guiding T-TEER due to its high spatial and temporal resolution. However, it requires general anesthesia and esophageal intubation, limiting its use in certain patients. Additionally, TEE image quality may be compromised by anterior structure shadowing, which is common in T-TEER. The development of 4D intracardiac echocardiography (ICE) offers real-time, three-dimensional imaging, potentially overcoming these limitations. This study compared TEE and Acuson AcuNav 4D-ICE in guiding T-TEER in ten high-risk patients across eight crucial procedural steps. ICE showed optimal feasibility in key procedural steps, including valve steering and leaflet grasping, due to its proximity to target structures, minimizing shadowing artifacts. Both modalities performed equally in lesion identification and residual regurgitation assessment and achieved non-statistically different results in most quantitative measurements. This study supports the integration of 4D-ICE into T-TEER procedures, particularly for patients unsuited for TEE or with complex TEE windows. Its real-time imaging, reduced invasiveness, and feasibility in critical steps highlight its potential as a viable alternative or complement to TEE. Further multicenter studies are needed to validate its role, optimize protocols, and evaluate long-term outcomes in 4D-ICE-guided T-TEER.
Full article
(This article belongs to the Section Imaging)
►▼
Show Figures
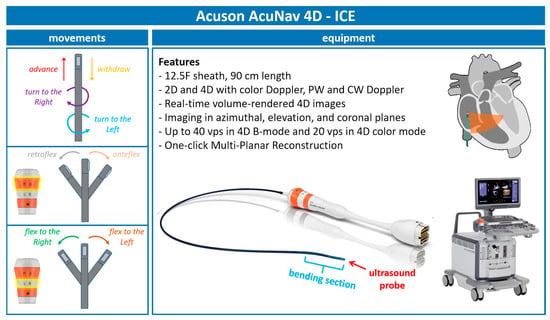
Figure 1
Open AccessArticle
Riding the Highs and Lows of the Conduction System Pacing Wave—Our Experience
by
Hooi Khee Teo, Yi Yi Chua, Julian Cheong Kiat Tay, Xuanming Pung, Jonathan Wei Sheng Ong, Germaine Jie Min Loo, Eric Tien Siang Lim, Kah Leng Ho, Daniel Thuan Tee Chong and Chi Keong Ching
J. Cardiovasc. Dev. Dis. 2025, 12(5), 164; https://doi.org/10.3390/jcdd12050164 - 22 Apr 2025
Abstract
Conduction system pacing started with His bundle pacing (HBP) and then rapidly switched gears into left bundle branch pacing (LBBP). We describe our center’s experience with LBBP using either lumenless leads (LLLs) or stylet-driven leads (SDLs). Patients who were admitted to two tertiary
[...] Read more.
Conduction system pacing started with His bundle pacing (HBP) and then rapidly switched gears into left bundle branch pacing (LBBP). We describe our center’s experience with LBBP using either lumenless leads (LLLs) or stylet-driven leads (SDLs). Patients who were admitted to two tertiary centers between 1 April 2021 and 30 June 2024 and met the guidelines for pacing were recruited and prospectively followed up. A total of 124 patients underwent permanent pacemaker (PPM) implantation using the LBBP technique with a mean follow-up of 19.7 ± 13.3 months. In total, 90 patients were implanted with LLLs and 34 with SDLs. There was no significant difference in the procedural time and final paced QRS duration, but fluoroscopy time was significantly longer in the SDLs (26.2 ± 17.7 min vs. 17.5 ± 13.0 min, respectively, p = 0.026). The on-table impedance values were also significantly higher in the LLLs, and this persisted throughout the follow-up. There were no differences in the rates of complications. The success of conduction system pacing implantation with SDLs and LLLs is comparable with reasonable safety and reliable outcomes. Good pre-implant patient selection will contribute to improved outcomes.
Full article
(This article belongs to the Special Issue Advances in Cardiac Pacing and Cardiac Resynchronisation Therapy)
►▼
Show Figures

Figure 1
Open AccessArticle
Impact of Simulated Vascular Aging and Heart Rate on Myocardial Efficiency: A Tale of Two Paradigms from In Silico Modelling
by
Lawrence J. Mulligan, Julian Thrash, Ludmil Mitrev, Daniel Ewert and Jeffrey C. Hill
J. Cardiovasc. Dev. Dis. 2025, 12(5), 163; https://doi.org/10.3390/jcdd12050163 - 22 Apr 2025
Abstract
Introduction: Vascular aging is associated with a loss of aortic compliance (CA), which results in increased left ventricular pressure–volume area (PVA), stroke work (SW) and myocardial oxygen consumption (MVO2). Myocardial efficiency (MyoEff) is derived from the PVA and MVO
[...] Read more.
Introduction: Vascular aging is associated with a loss of aortic compliance (CA), which results in increased left ventricular pressure–volume area (PVA), stroke work (SW) and myocardial oxygen consumption (MVO2). Myocardial efficiency (MyoEff) is derived from the PVA and MVO2 construct, which includes potential energy (PE). However, the SW/MVO2 ratio does not include PE and provides a more accurate physiologic measure. Methods: We used a modified computational model (CM) to assess PVA and SW and calculate MVO2 using a pressure-work index (e MVO2), to derive MyoEff–PVA and MyoEff–SW metrics. Phase I evaluated five levels of human CA from normal (N) to stiff (S) at 80 bpm, and Phase II evaluated two levels of CA (N and S) at three heart rates (60, 100, and 140 bpm). Results: During Phase I, MyoEff–PVA increased from 20.7 to 31.2%, and MyoEff–SW increased from 14.8 to 18.9%. In Phase II, during the N setting coupled with increases in the heart rate, the MyoEff–PVA decreased from 29.4 to 14.8 to 9.5%; the MyoEff–SW also decreased from 22.5 to 10.3 to 5.9%. As expected, during the S setting, MyoEff–PVA decreased from 45.5 to 22.9 to 14.8; a similar effect occurred with the MyoEff–SW, demonstrating a decrease from 29.9 to 13.9 to 7.9%, respectively. Conclusions: The CM provided insights into a simple and clinically relevant calculation for assessing MyoEff. The agreement on the CM metrics aligns with studies conducted previously in the clinical setting.
Full article
(This article belongs to the Special Issue Models and Methods for Computational Cardiology: 2nd Edition)
►▼
Show Figures

Figure 1
Open AccessArticle
Sarcopenia in Patients with Chronic Thromboembolic Pulmonary Hypertension
by
Steven Hopkins, Jillian Hall, Hollie Saunders, Riyaz Bashir, Vladimir Lakhter, Anjali Vaidya, Ahmed Sadek, Paul Forfia and Estefania Oliveros
J. Cardiovasc. Dev. Dis. 2025, 12(5), 162; https://doi.org/10.3390/jcdd12050162 - 22 Apr 2025
Abstract
►▼
Show Figures
Background: Sarcopenia, or loss of skeletal muscle mass, has been associated with poor outcomes (e.g., functional decline, increased mortality, and low quality of life), but its role in CTEPH remains unclear. The psoas muscle index (PMI) is a validated measure of sarcopenia. We
[...] Read more.
Background: Sarcopenia, or loss of skeletal muscle mass, has been associated with poor outcomes (e.g., functional decline, increased mortality, and low quality of life), but its role in CTEPH remains unclear. The psoas muscle index (PMI) is a validated measure of sarcopenia. We investigated the incidence of sarcopenia using PMI in CTEPH. Methods: Retrospective analysis of a single-center cohort of patients with CTEPH with an available computed tomography of the abdomen and pelvis (CTAP). PMI was measured at the L3 level of the CTAP and was then calculated using the formula (left psoas area + right psoas area/height2). Patients in the first quartile of PMI were classified as sarcopenic. Results: We reviewed 558 patients with CTEPH, and 97 patients had an available CTAP before intervention. Sarcopenia was identified in 26 (24.8%) of the patients and was associated with worse baseline functional status (p = 0.008), higher mean pulmonary artery pressure (48 vs. 39 mmHg; p = 0.002), and higher pulmonary vascular resistance (9.9 vs. 6.8 WU; p = 0.013). Post-PTE, patients with sarcopenia exhibited longer intensive care unit (ICU) (9 vs. 4 days, p < 0.001) and overall hospital stays (24 vs. 11 days, p < 0.001), despite similar post-operative hemodynamics achieved compared to non-sarcopenic patients. Conclusions: CTEPH patients with sarcopenia have worse baseline functional class and hemodynamics. For those with sarcopenia requiring surgery, there is longer ICU and total hospitalization stays, but they achieve significant functional improvements and hemodynamics comparable to that of non-sarcopenic patients. Hence, the risk of longer perioperative hospitalization days is justified by the longer-term benefit of hemodynamic improvement. The use of PMI as part of routine pre-operative assessments could improve clinical decision-making in CTEPH patients undergoing surgical or medical intervention.
Full article

Graphical abstract
Open AccessArticle
Intravascular Imaging-Guided Versus Angiography-Guided Percutaneous Coronary Intervention in Patients with Non-ST-Segment Elevation Myocardial Infarction in the United States: Results from Big Data Analysis
by
Chayakrit Krittanawong, Song Peng Ang, Neil Sagar Maitra, Zhen Wang, Mahboob Alam, Hani Jneid and Samin Sharma
J. Cardiovasc. Dev. Dis. 2025, 12(4), 161; https://doi.org/10.3390/jcdd12040161 - 17 Apr 2025
Abstract
►▼
Show Figures
Non-ST-segment elevation myocardial infarction (NSTEMI) can be managed by ischemia guide strategies or early invasive strategies. Here, we present the findings of an updated contemporary analysis regarding the use of intracoronary imaging (ICI)-guided PCI versus angiography-guided PCI and in-hospital mortality in patients with
[...] Read more.
Non-ST-segment elevation myocardial infarction (NSTEMI) can be managed by ischemia guide strategies or early invasive strategies. Here, we present the findings of an updated contemporary analysis regarding the use of intracoronary imaging (ICI)-guided PCI versus angiography-guided PCI and in-hospital mortality in patients with NSTEMI in the United States using the NIS database from 2016 to 2021. ICI use increased by nearly threefold between 2016 and 2021, without a significant difference in in-hospital mortality, though interestingly, mortality rates compared with angiography guidance were similar and relatively low. In this study, the use of ICI was associated with lower adjusted odds of in-hospital mortality, cardiogenic shock, and cardiac arrest, but with a longer length of stay and cost of hospitalization.
Full article
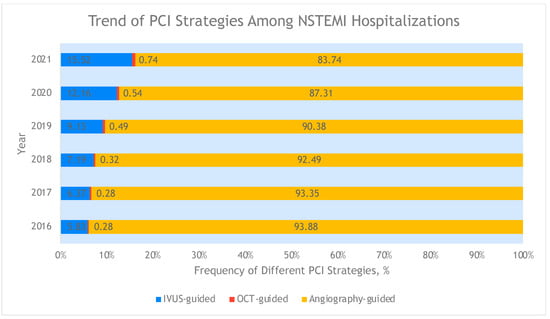
Figure 1
Open AccessArticle
Echocardiographic Predictors of Postoperative Atrial Fibrillation After Cardiac Surgery: Assessing Atrial Mechanics for Risk Stratification
by
Velimir Perić, Mlađan Golubović, Marija Stošić, Dragan Milić, Lela Lazović, Dalibor Stojanović, Milan Lazarević, Dejan Marković and Dragana Unić-Stojanović
J. Cardiovasc. Dev. Dis. 2025, 12(4), 160; https://doi.org/10.3390/jcdd12040160 - 17 Apr 2025
Abstract
Postoperative atrial fibrillation (POAF) is a common complication after cardiac surgery, increasing morbidity and healthcare costs. This study aimed to identify echocardiographic predictors of POAF to improve risk stratification. A total of 131 patients undergoing cardiac surgery were analyzed and divided into two
[...] Read more.
Postoperative atrial fibrillation (POAF) is a common complication after cardiac surgery, increasing morbidity and healthcare costs. This study aimed to identify echocardiographic predictors of POAF to improve risk stratification. A total of 131 patients undergoing cardiac surgery were analyzed and divided into two groups based on POAF occurrence. Echocardiographic analysis showed that patients with POAF had larger left and right atrial dimensions and impaired atrial function. Prolonged total atrial conduction time (TACT), reduced atrial emptying volumes, and contractile function were more common in the POAF group. Univariable analysis identified LAEF (χ2 = 71.8, p < 0.001), LAKE (χ2 = 70.1, p < 0.001), RATEF (χ2 = 65.7, p < 0.001), and RAAEF (χ2 = 66.8, p < 0.001) as significant predictors of POAF, each with an area under the curve (AUC) greater than 0.89. In multivariable analysis, LAKE (OR = 0.27, p < 0.001), hypertension (OR = 11.87, p = 0.035), left ventricular ejection fraction (OR = 1.08, p = 0.020), and peripheral vascular disease (OR = 40.28, p = 0.002) were independent predictors. The final model showed a significant discriminatory ability (AUC = 0.94). LAKE and clinical factors remained independent predictors after adjustment.
Full article
(This article belongs to the Special Issue Heart Rhythm Disorders: Diagnosis, Treatment, and Management)
►▼
Show Figures

Figure 1
Open AccessReview
Coronary Computed Angiography and Coronary Artery Calcium Score for Preoperative Cardiovascular Risk Stratification in Patients Undergoing Noncardiac Surgery
by
Ioannis Kyriakoulis, Sriram S. Kumar, Georgios D. Lianos, Dimitrios Schizas and Damianos G. Kokkinidis
J. Cardiovasc. Dev. Dis. 2025, 12(4), 159; https://doi.org/10.3390/jcdd12040159 - 17 Apr 2025
Abstract
Perioperative and long-term postoperative major adverse cardiovascular events (MACE) are a leading cause of morbidity and mortality in patients undergoing noncardiac surgery. In selected high-risk patients, when information about cardiovascular status may influence surgical decisions, preoperative risk stratification is reasonable, with stress imaging
[...] Read more.
Perioperative and long-term postoperative major adverse cardiovascular events (MACE) are a leading cause of morbidity and mortality in patients undergoing noncardiac surgery. In selected high-risk patients, when information about cardiovascular status may influence surgical decisions, preoperative risk stratification is reasonable, with stress imaging being the preferred method. Coronary computed angiography (CCTA) and coronary artery calcium score (CACS) offer direct anatomical assessment of atherosclerotic coronary arteries and help gauge the extent and severity of coronary artery disease. Strong evidence supports that CCTA and CACS, either alone or in combination, are reliable methods for assessing the risk of both perioperative and long-term postoperative MACE, often demonstrating equal or superior prognostic performance compared to traditional imaging tools. Moreover, integrating CCTA or CACS into standard preoperative imaging protocols further enhances perioperative risk prediction and improves the ability to accurately stratify patients. Future research is needed to better define the role of CCTA and CACS in preoperative cardiovascular risk evaluation of patients undergoing noncardiac surgery.
Full article
(This article belongs to the Special Issue Clinical Applications of Cardiovascular Computed Tomography (CT))
►▼
Show Figures
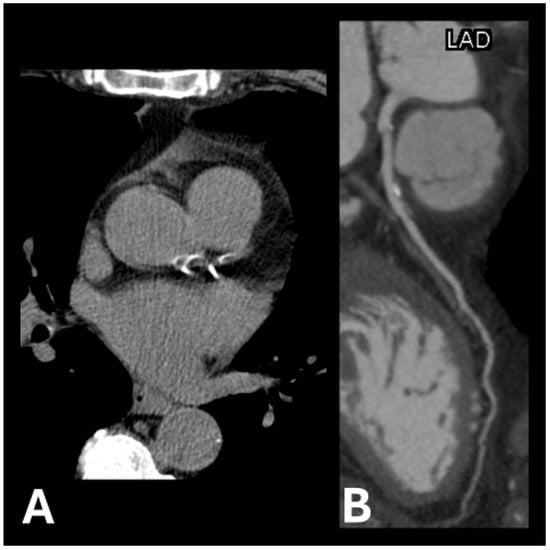
Figure 1
Open AccessReview
Narrative Review of High-Intensity Interval Training: Positive Impacts on Cardiovascular Health and Disease Prevention
by
Jae-Myun Ko, Wi-Young So and Sung-Eun Park
J. Cardiovasc. Dev. Dis. 2025, 12(4), 158; https://doi.org/10.3390/jcdd12040158 - 17 Apr 2025
Abstract
Background: High-intensity interval training (HIIT) has gained recognition for its positive impacts on cardiovascular (CV) health, metabolic outcomes, mental health, and quality of life (QoL). This narrative review aims to comprehensively evaluate the efficacy of HIIT in enhancing CV health and preventing CV
[...] Read more.
Background: High-intensity interval training (HIIT) has gained recognition for its positive impacts on cardiovascular (CV) health, metabolic outcomes, mental health, and quality of life (QoL). This narrative review aims to comprehensively evaluate the efficacy of HIIT in enhancing CV health and preventing CV disease (CVD). Methods: A comprehensive search of PubMed identified 257 articles, of which 39 studies met predefined inclusion and exclusion criteria for quality assessment. Key metrics evaluated included blood pressure, vascular function, lipid profiles, body composition, and CRF. Results: HIIT significantly improved vascular function, evidenced by reductions in systolic and diastolic blood pressure and enhanced flow-mediated dilation. Improvements in cardiac function were observed through increased cardiac output and heart rate variability. Additionally, HIIT positively influenced lipid profiles, decreasing low-density lipoprotein and triglycerides while increasing high-density lipoprotein. Significant reductions in body fat and improvements in VO2peak were noted, contributing to enhanced CRF. HIIT also positively impacted mental health and QoL, reducing anxiety and depressive symptoms. Importantly, HIIT was safely and effectively applied to high-risk populations—individuals with obesity, metabolic syndrome, CVD, and cancer survivors—with a low incidence of adverse effects. Conclusions: This review highlights HIIT as an effective and safe exercise modality for improving CV health, metabolic indicators, mental health, and QoL. Future research should focus on developing tailored HIIT protocols to optimize adherence and efficacy across diverse populations, considering variations in age, sex, health status, and underlying medical conditions.
Full article
(This article belongs to the Special Issue Sports Cardiology: From Diagnosis to Clinical Management, 2nd Edition)
►▼
Show Figures
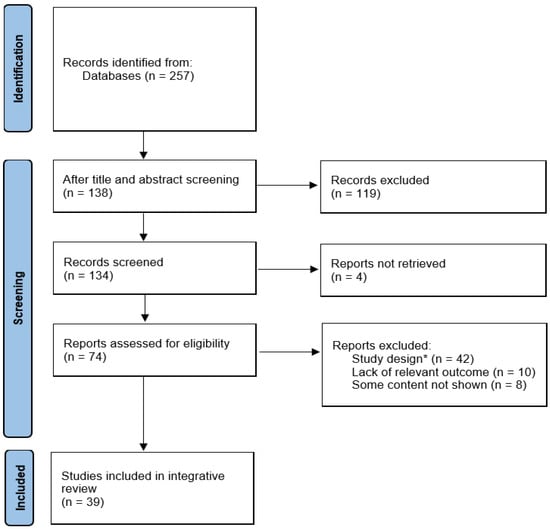
Figure 1
Open AccessCase Report
Non-ST-Elevation Myocardial Infarction as the Initial Manifestation of Calreticulin-Positive Essential Thrombocythemia: A Case Report
by
Jared B. Hinton, Jalal S. Jwayyed, Sonum Jagetia, Hunter J. Landwehr and John D. Scrocco
J. Cardiovasc. Dev. Dis. 2025, 12(4), 157; https://doi.org/10.3390/jcdd12040157 - 16 Apr 2025
Abstract
►▼
Show Figures
Essential thrombocythemia (ET) is a rare myeloproliferative neoplasm characterized by excessive platelet production and a predisposition to thrombotic or hemorrhagic complications. We report a case of a 62-year-old male with no conventional cardiovascular risk factors who presented with a non-ST-segment elevation myocardial infarction
[...] Read more.
Essential thrombocythemia (ET) is a rare myeloproliferative neoplasm characterized by excessive platelet production and a predisposition to thrombotic or hemorrhagic complications. We report a case of a 62-year-old male with no conventional cardiovascular risk factors who presented with a non-ST-segment elevation myocardial infarction (NSTEMI). Initial coronary angiography showed isolated proximal LAD stenosis. Laboratory tests revealed marked thrombocytosis (>1,000,000/μL) and a CALR mutation, confirming a diagnosis of ET. The patient was treated with percutaneous coronary intervention (PCI), dual antiplatelet therapy, and cytoreductive therapy with hydroxyurea, leading to a favorable outcome. This case illustrates how ET, particularly CALR-mutated subtypes, can manifest as acute coronary syndrome in the absence of atherosclerosis and underscores the need to consider hematologic malignancies in atypical presentations of myocardial infarction.
Full article
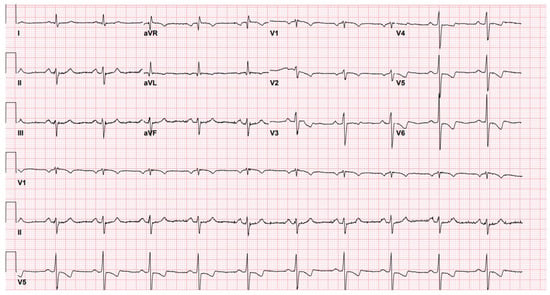
Figure 1
Open AccessReview
The Prenatal Diagnosis and Perinatal Management of Congenital Long QT Syndrome: A Comprehensive Literature Review and Recent Updates
by
Stefani Samples, Sara Cherny, Nitin Madan, Jeff Hong, Sheena A. Mansukhani, Janette F. Strasburger, Michael R. Carr and Sheetal R. Patel
J. Cardiovasc. Dev. Dis. 2025, 12(4), 156; https://doi.org/10.3390/jcdd12040156 - 14 Apr 2025
Abstract
Congenital long QT syndrome (LQTS) is a group of heritable conditions that are associated with cardiac repolarization abnormalities characterized by QT prolongation on electrocardiogram and the risk of life-threatening arrhythmias. The prenatal detection of LQTS presents significant challenges for clinicians, and a multidisciplinary
[...] Read more.
Congenital long QT syndrome (LQTS) is a group of heritable conditions that are associated with cardiac repolarization abnormalities characterized by QT prolongation on electrocardiogram and the risk of life-threatening arrhythmias. The prenatal detection of LQTS presents significant challenges for clinicians, and a multidisciplinary approach is required for optimal prenatal and postnatal management. In this comprehensive literature review, we describe strategies for the fetal diagnosis of LQTS with variable initial presentation, genetic testing in suspected fetal LQTS, the utility of fetal magnetocardiography as an additional diagnostic tool, prenatal management, and postnatal treatment. We focus on a multidisciplinary team approach including fetal cardiology, adult and pediatric electrophysiology, neonatology, maternal–fetal medicine, and genetic counselors, all playing vital roles in the comprehensive prenatal management and orchestration of postnatal treatment to optimize neonatal outcomes.
Full article
(This article belongs to the Special Issue Recent Advances in Fetal Cardiology)
►▼
Show Figures

Graphical abstract
Open AccessReview
Advances in Hypertension Management: Insights from the Latest European Guidelines
by
Marco Zuin, Chiara Tognola, Alessandro Maloberti, Gianfranco Parati, Stefania Angela Di Fusco, Vered Gil Ad, Donatella Armata, Chiara Dalla Valle, Furio Colivicchi, Claudio Bilato, Massimo Grimaldi, Fabrizio Oliva and Pier Luigi Temporelli
J. Cardiovasc. Dev. Dis. 2025, 12(4), 155; https://doi.org/10.3390/jcdd12040155 - 14 Apr 2025
Abstract
►▼
Show Figures
Arterial hypertension is one of the most common and preventable risk factors for cardiovascular disease and its related mortality. Currently, the prevalence of hypertension in different European countries appears to be around 30–45% of the general population, with a steep increase with ageing.
[...] Read more.
Arterial hypertension is one of the most common and preventable risk factors for cardiovascular disease and its related mortality. Currently, the prevalence of hypertension in different European countries appears to be around 30–45% of the general population, with a steep increase with ageing. Recent European guidelines have introduced novel recommendations for the management and treatment of hypertensive patients, with direct implications in daily clinical practice. Therefore, in this focused review, we will provide answers to the most common questions regarding the diagnosis, management and treatment of arterial hypertension according to the latest available European guidelines.
Full article
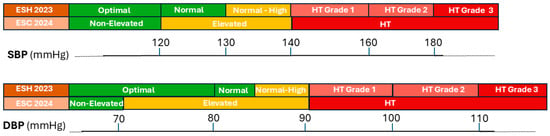
Figure 1
Open AccessReview
Cardiac Magnetic Resonance Imaging in the Evaluation and Prognosis of Infiltrative Cardiomyopathies
by
Merna Hussien, Francisca Bermudez, Patrick T. Bering, Gaby Weissman, Allison G. Hays and Farooq H. Sheikh
J. Cardiovasc. Dev. Dis. 2025, 12(4), 154; https://doi.org/10.3390/jcdd12040154 - 12 Apr 2025
Abstract
Advancements in cardiac magnetic resonance (CMR) imaging quality and availability have made it an essential tool in the care of individuals living with cardiomyopathies. CMR complements clinical suspicion, electrocardiogram patterns, and echocardiographic findings to help elucidate the etiology of cardiomyopathies and can also
[...] Read more.
Advancements in cardiac magnetic resonance (CMR) imaging quality and availability have made it an essential tool in the care of individuals living with cardiomyopathies. CMR complements clinical suspicion, electrocardiogram patterns, and echocardiographic findings to help elucidate the etiology of cardiomyopathies and can also be used to prognosticate and follow treatment responses. In this review, we highlight the common CMR findings in cardiac amyloidosis, cardiac sarcoidosis, iron overload cardiomyopathy, and Fabry disease. We also summarize prognostic findings and additional potential roles for CMR in the management of infiltrative cardiomyopathies.
Full article
(This article belongs to the Special Issue Cardiovascular Magnetic Resonance in Cardiology Practice: 2nd Edition)
►▼
Show Figures
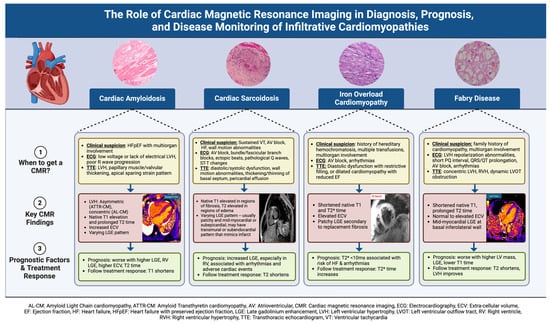
Figure 1
Open AccessArticle
The Dilemma of Surgical Timing in Acute Aortic Valve Endocarditis: Does Early Surgery Improve Risks or Prognosis?
by
Michele D’Alonzo, Lorenzo Di Bacco, Antonio Fiore, Massimo Baudo, Francesca Zanin, Chiara Baldelli, Cyrus Moini, Thierry Folliguet and Claudio Muneretto
J. Cardiovasc. Dev. Dis. 2025, 12(4), 153; https://doi.org/10.3390/jcdd12040153 - 11 Apr 2025
Abstract
Background: Acute aortic valve infective endocarditis (IE) presents a critical surgical timing dilemma. This study investigates whether early surgical intervention (within seven days of targeted antibiotic therapy initiation) affects mortality and clinical outcomes compared to delayed/conventional surgery. Methods: A retrospective, multicenter analysis of
[...] Read more.
Background: Acute aortic valve infective endocarditis (IE) presents a critical surgical timing dilemma. This study investigates whether early surgical intervention (within seven days of targeted antibiotic therapy initiation) affects mortality and clinical outcomes compared to delayed/conventional surgery. Methods: A retrospective, multicenter analysis of 204 patients with aortic IE was conducted, excluding emergency cases requiring immediate intervention. Patients were stratified into EARLY (≤7 days) and LATE (>7 days) surgical groups. Primary endpoints included in-hospital mortality and major adverse events, while secondary endpoints assessed long-term survival, recurrence, and reintervention rates. Results: No significant differences in in-hospital mortality were observed between groups (16% in both). The LATE group exhibited a trend toward increased permanent pacemaker implantation (16% vs. 8.2%; p = 0.100) and a higher incidence of postoperative atrial fibrillation (36% vs. 24%, p = 0.048). Infective endocarditis recurrence and long-term survival did not significantly differ between groups. Predictors of one-year mortality included chronic kidney disease, annular abscess, extracorporeal membrane oxygenation (ECMO) use, and prolonged mechanical ventilation. Conclusions: These findings suggest that early surgery, following a short course of antibiotics, does not compromise outcomes nor increase recurrence risk, challenging the conventional preference for delayed intervention in non-emergency IE cases.
Full article
(This article belongs to the Section Cardiac Surgery)
►▼
Show Figures
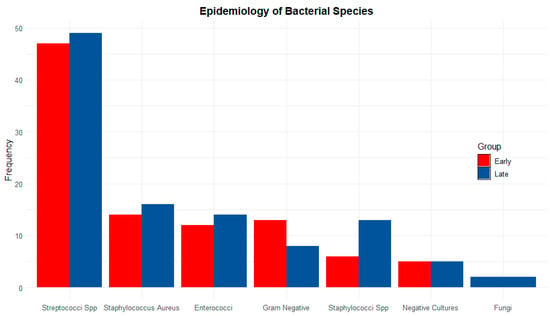
Figure 1
Open AccessArticle
Right Ventricular and Left Atrial Strain Predict Volumetric Response to Cardiac Resynchronization Therapy
by
Shing Ching, Jeffrey Ji-Peng Li, Stefanie Maria Werhahn, Rebecca Elisabeth Beyer, Misael Estepa, Christian Stehning, Djawid Hashemi, Natalia Solowjowa, Christoph Klein, Henryk Dreger, Sebastian Kelle and Patrick Doeblin
J. Cardiovasc. Dev. Dis. 2025, 12(4), 152; https://doi.org/10.3390/jcdd12040152 - 11 Apr 2025
Abstract
Background: While left-bundle-branch-block-related contraction patterns as well as echocardiography-derived strain are variably associated with the volumetric response to cardiac resynchronization therapy (CRT), the role of CMR-derived strain parameters is unexplored. Methods: A total of 50 patients receiving CRT implantation were retrospectively analyzed, all
[...] Read more.
Background: While left-bundle-branch-block-related contraction patterns as well as echocardiography-derived strain are variably associated with the volumetric response to cardiac resynchronization therapy (CRT), the role of CMR-derived strain parameters is unexplored. Methods: A total of 50 patients receiving CRT implantation were retrospectively analyzed, all of whom had undergone CMR imaging within one year before, and echocardiography within 6 months before and 6–12 months after CRT implantation. We assessed CMR-derived morphological and functional parameters with regard to the echocardiographic response, defined as a reduction in the left ventricular end-systolic volume of ≥15%. Results: Among the standard CMR parameters, the indexed right ventricular volumes in end-diastole (RVEDVi) (74.5 ± 19.5 vs. 94.8 ± 30.2 mL/m2, p = 0.006) and end-systole (RVESVi) (43.2 ± 13.3 vs. 61.6 ± 28.8 mL/m2, p = 0.003), as well as the left atrial (LA) area (24.8 ± 3.5 vs. 30.4 ± 9.5 cm2, p = 0.020), differed significantly between CRT responders and non-responders. In strain analysis, CRT responders showed a significantly better LA global longitudinal strain (GLS) (25.1 ± 10.4 vs. 15.3 ± 10.5, p = 0.002), LA global circumferential strain (GCS) (27.9 ± 14.7 vs. 17.1 ± 13.1%, p = 0.012), RV GLS (−25.0 ± 6.5 vs. −18.9 ± 7.6%, p = 0.004) and RV free wall strain (−31.1 ± 7.9 vs. −24.9 ± 9.5, p = 0.017). Conclusions: CMR-derived peak septal circumferential strain and RVEDVi correlated with the echocardiographic volumetric response to CRT at 6–12 months.
Full article
(This article belongs to the Section Imaging)
►▼
Show Figures
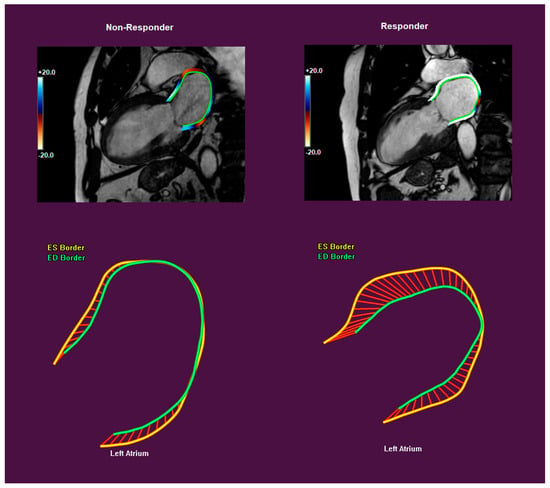
Figure 1

Journal Menu
► ▼ Journal Menu-
- JCDD Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Antioxidants, Biomolecules, JCDD, Metabolites, Neurology International, Pharmaceutics
Tissue-Specific, Disease-Signatured Macrophages in Control of Redox and Antioxidation in Metabolic Diseases
Topic Editors: Xiangwei Xiao, Yingmei Feng, Zhiyong LeiDeadline: 5 July 2025
Topic in
Cardiogenetics, Hearts, JCDD, JCM, Medicina
Biomarkers in Cardiovascular Disease—Chances and Risks, 2nd Volume
Topic Editors: Alexander E. Berezin, Michael LichtenauerDeadline: 31 December 2025
Topic in
Diagnostics, Geriatrics, JCDD, Medicina
New Research on Atrial Fibrillation
Topic Editors: Michele Magnocavallo, Domenico G. Della Rocca, Stefano Bianchi, Pietro Rossi, Antonio BisignaniDeadline: 31 March 2026
Topic in
Cardiogenetics, Hearts, JCDD, JCM
Adult Congenital Heart Disease: Advances in Diagnosis, Surgery, and Lifelong Care
Topic Editors: Satoshi Akagi, Jin Young SongDeadline: 30 June 2026

Conferences
Special Issues
Special Issue in
JCDD
Feature Review Papers in Stroke and Cerebrovascular Disease
Guest Editor: Narayanaswamy VenketasubramanianDeadline: 30 April 2025
Special Issue in
JCDD
Bicuspid Aortic Valve Management for Cardiologists and Cardiac Surgeons
Guest Editor: Francesco NappiDeadline: 30 April 2025
Special Issue in
JCDD
Stroke in the Young
Guest Editor: Narayanaswamy VenketasubramanianDeadline: 15 May 2025
Special Issue in
JCDD
Pulmonary Hypertension: Current Status of Diagnosis and Treatment
Guest Editors: Roxana Sulica, Himanshu DeshwalDeadline: 25 May 2025
Topical Collections
Topical Collection in
JCDD
Current Challenges in Heart Failure and Cardiac Transplantation
Collection Editors: Rasmus Rivinius, Daniel Oehler, Andreas J. Rieth, Andreas Doesch








