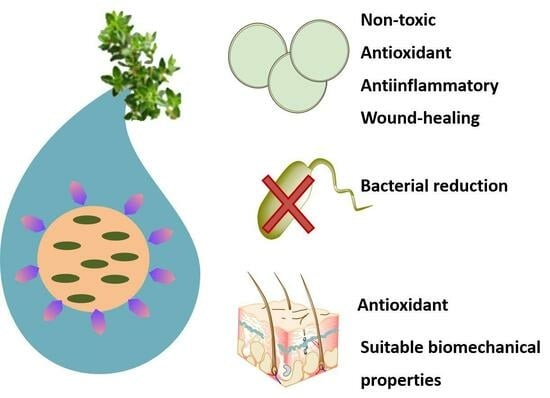
Hydrogel of Thyme-Oil-PLGA Nanoparticles Designed for Skin Inflammation Treatment
Abstract
:1. Introduction
2. Results and Discussion
2.1. Characterization and Optimization of THO-NPs
2.2. In Vitro Bacterial Viability Reduction
2.3. Cytotoxicity in HaCaT Cells
2.4. Antioxidant Activity
2.5. Anti-Inflammatory Activity
2.6. Wound Healing
2.7. Ex Vivo Skin Antioxidant Efficacy
2.8. Characterization and Stability of the Hydrogels
2.9. Rheological Studies
2.10. Extensibility Studies
2.11. In Vivo Skin Biomechanical Properties
2.12. Discussion
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Preparation of THO-NPs
4.3. Characterization and Stability of THO-NPs
4.4. In Vitro Antimicrobial Efficacy
4.5. In Vitro Cytotoxicity
4.6. In Vitro Antioxidant Activity
4.7. In Vitro Anti-Inflammatory Efficacy
4.8. Wound-Healing Activity
4.9. Ex Vivo Skin Antioxidant Efficacy
4.10. Preparation of THO Hydrogels
4.11. Characterization and Stability of the Hydrogels
4.12. Rheology Studies
4.13. Extensibility Studies
4.14. In Vivo Biomechanical Properties on Skin
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Firlej, E.; Kowalska, W.; Szymaszek, K.; Roliński, J.; Bartosińska, J. The Role of Skin Immune System in Acne. J. Clin. Med. 2022, 11, 1579. [Google Scholar] [CrossRef] [PubMed]
- Dréno, B.; Dagnelie, M.A.; Khammari, A.; Corvec, S. The Skin Microbiome: A New Actor in Inflammatory Acne. Am. J. Clin. Dermatol. 2020, 21, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Kardeh, S.; Moein, S.A.; Namazi, M.R.; Kardeh, B. Evidence for the Important Role of Oxidative Stress in the Pathogenesis of Acne. Galen Med. J. 2019, 8, e1291. [Google Scholar] [CrossRef]
- Na-Bangchang, K.; Plengsuriyakarn, T.; Karbwang, J. The Role of Herbal Medicine in Cholangiocarcinoma Control: A Systematic Review. Planta Med. 2023, 89, 3–18. [Google Scholar] [CrossRef]
- Liu, Z.; Lin, D.; Shen, R.; Zhang, R.; Liu, L.; Yang, X. Konjac glucomannan-based edible films loaded with thyme Essential oil: Physical properties and antioxidant-antibacterial activities. Food Packag. Shelf Life 2021, 29, 100700. [Google Scholar] [CrossRef]
- Barakat, H.; Aljabeili, H.S.; Rahman, H.A.A. Synergistic Effect of Thymus vulgaris Essential Oil Oral Administration on Topically Treated Wound with Chitosan, Thyme Essential Oil and their Combination in Rats. J. Nutr. Food Sci. 2018, 08, 1–6. [Google Scholar] [CrossRef]
- Kowalczyk, A.; Przychodna, M.; Sopata, S.; Bodalska, A.; Fecka, I. Thymol and Thyme Essential Oil—New Insights into Selected Therapeutic Applications. Molecules 2020, 25, 4125–4142. [Google Scholar] [CrossRef]
- Volić, M.M.; Obradović, N.S.; Djordjević, V.B.; Luković, N.D.; Knežević-Jugović, Z.D.; Bugarski, B.M. Design of biopolymer carriers enriched with natural emulsifiers for improved controlled release of thyme essential oil. J. Food Sci. 2020, 85, 3833–3842. [Google Scholar] [CrossRef]
- Folle, C.; Marqués, A.M.; Díaz-Garrido, N.; Espina, M.; Sánchez-López, E.; Badia, J.; Baldoma, L.; Calpena, A.C.; García, M.L. Thymol-loaded PLGA nanoparticles: An efficient approach for acne treatment. J. Nanobiotechnol. 2021, 19, 359. [Google Scholar] [CrossRef]
- Folle, C.; Díaz-Garrido, N.; Sánchez-López, E.; Marqués, A.M.; Badia, J.; Baldomà, L.; Espina, M.; Calpena, A.C.; García, M.L. Surface-modified multifunctional thymol-loaded biodegradable nanoparticles for topical acne treatment. Pharmaceutics 2021, 13, 1501. [Google Scholar] [CrossRef]
- Sánchez-López, E.; Egea, M.A.; Cano, A.; Espina, M.; Calpena, A.C.C.; Ettcheto, M.; Camins, A.; Souto, E.B.; Silva, A.M.; García, M.L.L. PEGylated PLGA nanospheres optimized by design of experiments for ocular administration of dexibuprofen—In Vitro, ex vivo and in vivo characterization. Colloids Surfaces B Biointerfaces 2016, 145, 241–250. [Google Scholar] [CrossRef]
- Bernal-Chávez, S.A.; Alcalá-Alcalá, S.; Cerecedo, D.; Ganem-Rondero, A. Platelet lysate-loaded PLGA nanoparticles in a thermo-responsive hydrogel intended for the treatment of wounds. Eur. J. Pharm. Sci. 2020, 146, 105231. [Google Scholar] [CrossRef]
- Yu, Y.Q.; Yang, X.; Wu, X.F.; Fan, Y. Bin Enhancing Permeation of Drug Molecules across the Skin via Delivery in Nanocarriers: Novel Strategies for Effective Transdermal Applications. Front. Bioeng. Biotechnol. 2021, 9, 646554. [Google Scholar] [CrossRef]
- Su, R.; Fan, W.; Yu, Q.; Dong, X.; Qi, J.; Zhu, Q.; Zhao, W.; Wu, W.; Chen, Z.; Li, Y.; et al. Size-dependent penetration of nanoemulsions into epidermis and hair follicles: Implications for transdermal delivery and immunization. Oncotarget 2017, 8, 38214–38226. [Google Scholar] [CrossRef] [PubMed]
- Zeb, A.; Arif, S.T.; Malik, M.; Shah, F.A.; Din, F.U.; Qureshi, O.S.; Lee, E.S.; Lee, G.Y.; Kim, J.K. Potential of Nanoparticulate Carriers for Improved Drug Delivery via Skin; Springer: Singapore, 2019; Volume 49, ISBN 0123456789. [Google Scholar]
- Liu, Y.H.; Lin, Y.S.; Huang, Y.W.; Fang, S.U.; Lin, S.Y.; Hou, W.C. Protective Effects of Minor Components of Curcuminoids on Hydrogen Peroxide-Treated Human HaCaT Keratinocytes. J. Agric. Food Chem. 2016, 64, 3598–3608. [Google Scholar] [CrossRef] [PubMed]
- Ocaña, A.; Reglero, G. Effects of thyme extract oils (from Thymus vulgaris, Thymus zygis, and Thymus hyemalis) on cytokine production and gene expression of oxLDL-stimulated THP-1-macrophages. J. Obes. 2012, 2012, 104706. [Google Scholar] [CrossRef] [PubMed]
- Dey, S.; Rothe, H.; Page, L.; O’Connor, R.; Farahmand, S.; Toner, F.; Marsh, R.; Wehmeyer, K.; Zhou, S. An in vitro skin penetration model for compromised skin: Estimating penetration of polyethylene glycol [14C]-PEG-7 phosphate. Skin Pharmacol. Physiol. 2015, 28, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Constantin, M.-M.; Poenaru, E.; Poenaru, C.; Constantin, T. Skin Hydration Assessment through Modern Non-Invasive Bioengineering Technologies. Maedica 2014, 9, 33–38. [Google Scholar] [PubMed]
- Çalışkan, U.K.; Karakuş, M.M. Essential Oils as Skin Permeation Boosters and Their Predicted Effect Mechanisms. J. Dermatol. Ski. Sci. 2020, 2, 24–30. [Google Scholar]
- Heng, A.H.S.; Chew, F.T. Systematic review of the epidemiology of acne vulgaris. Sci. Rep. 2020, 10, 5754. [Google Scholar] [CrossRef] [PubMed]
- Lampe, M.A.; Burlingame, A.L.; Whitney, J.A.; Williams, M.L.; Brown, B.E.; Roitman, E.; Elias, P.M. Human stratum corneum lipids: Characterization and regional variations. J. Lipid Res. 1983, 24, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Piasecki, B.; Korona-Głowniak, I.; Kiełtyka-Dadasiewicz, A.; Ludwiczuk, A. Composition and Anti-Helicobacter pylori Properties of Essential Oils Obtained from Selected Mentha Cultivars. Molecules 2023, 28, 5690. [Google Scholar] [CrossRef] [PubMed]
- Yap, P.S.X.; Yusoff, K.; Lim, S.H.E.; Chong, C.M.; Lai, K.S. Membrane disruption properties of essential oils-a double-edged sword? Processes 2021, 9, 595. [Google Scholar] [CrossRef]
- Lin, T.K.; Zhong, L.; Santiago, J.L. Anti-inflammatory and skin barrier repair effects of topical application of some plant oils. Int. J. Mol. Sci. 2018, 19, 70. [Google Scholar] [CrossRef]
- Serrano, G.; Almudéver, P.; Serrano, J.M.; Milara, J.; Torrens, A.; Expósito, I.; Cortijo, J. Phosphatidylcholine liposomes as carriers to improve topical ascorbic acid treatment of skin disorders. Clin. Cosmet. Investig. Dermatol. 2015, 8, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Mengoni, T.; Adrian, M.; Pereira, S.; Santos-Carballal, B.; Kaiser, M.; Goycoolea, F.M. A chitosan-based liposome formulation enhances the in vitro wound healing efficacy of substance P neuropeptide. Pharmaceutics 2017, 9, 56. [Google Scholar] [CrossRef] [PubMed]
- Riella, K.R.; Marinho, R.R.; Santos, J.S.; Pereira-Filho, R.N.; Cardoso, J.C.; Albuquerque-Junior, R.L.C.; Thomazzi, S.M. Anti-inflammatory and cicatrizing activities of thymol, a monoterpene of the essential oil from Lippia gracilis, in rodents. J. Ethnopharmacol. 2012, 143, 656–663. [Google Scholar] [CrossRef] [PubMed]
- Fessi, H.; Puisieux, F.; Devissaguet, J.P.; Ammoury, N.; Benita, S. Nanocapsule formation by interfacial polymer deposition following solvent displacement. Int. J. Pharm. 1989, 55, R1–R4. [Google Scholar] [CrossRef]
- Messager, S.; Goddard, P.A.; Dettmar, P.W.; Maillard, J.Y. Determination of the antibacterial efficacy of several antiseptics tested on skin by an “ex-vivo” test. J. Med. Microbiol. 2001, 50, 284–292. [Google Scholar] [CrossRef]
- Liu, H.-M.; Lei, S.-N.; Tang, W.; Xun, M.-H.; Zhao, Z.-W.; Cheng, M.-Y.; Zhang, X.-D.; Wang, W. Optimization of Ultrasound-Assisted Cellulase Extraction from Nymphaea hybrid Flower and Biological Activities: Antioxidant Activity, Protective Effect against ROS Oxidative Damage in HaCaT Cells and Inhibition of Melanin Production in B16 Cells. Molecules 2022, 27, 1914. [Google Scholar] [CrossRef]
- Mazzotta, S.; Governa, P.; Borgonetti, V.; Marcolongo, P.; Nanni, C.; Gamberucci, A.; Manetti, F.; Pessina, F.; Carullo, G.; Brizzi, A.; et al. Pinocembrin and its linolenoyl ester derivative induce wound healing activity in HaCaT cell line potentially involving a GPR120/FFA4 mediated pathway. Bioorg. Chem. 2021, 108, 104657. [Google Scholar] [CrossRef] [PubMed]
- Fernández-García, E.; Heluani-Gahete, H.; Wellinger, R.E. A new colorimetric assay for antioxidant capacity and photostability. Color. Technol. 2016, 132, 195–200. [Google Scholar] [CrossRef]
- Mokdad, R.; Aouabed, A.; Ball, V.; Si Youcef, F.F.; Nasrallah, N.; Heurtault, B.; HadjSadok, A. Formulation and rheological evaluation of liposomes-loaded carbopol hydrogels based on thermal waters. Drug Dev. Ind. Pharm. 2022, 48, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Kolman, M.; Smith, C.; Chakrabarty, D.; Amin, S. Rheological stability of carbomer in hydroalcoholic gels: Influence of alcohol type. Int. J. Cosmet. Sci. 2021, 43, 748–763. [Google Scholar] [CrossRef]
- Strachota, B.; Strachota, A.; Vratović, L.; Pavlova, E.; Šlouf, M.; Kamel, S.; Cimrová, V. Exceptionally Fast Temperature-Responsive, Mechanically Strong and Extensible Monolithic Non-Porous Hydrogels: Poly(N-isopropylacrylamide) Intercalated with Hydroxypropyl Methylcellulose. Gels 2023, 9, 926. [Google Scholar] [CrossRef]
- Carvajal-Vidal, P.; González-Pizarro, R.; Araya, C.; Espina, M.; Halbaut, L.; Gómez de Aranda, I.; García, M.L.; Calpena, A.C. Nanostructured lipid carriers loaded with Halobetasol propionate for topical treatment of inflammation: Development, characterization, biopharmaceutical behavior and therapeutic efficacy of gel dosage forms. Int. J. Pharm. 2020, 585, 119480. [Google Scholar] [CrossRef]






| t (Months) | Zav (nm) | PI | ZP (mV) | |
|---|---|---|---|---|
| THO-NP-L- | 0 | 193.3 ± 1.1 | 0.153 ± 0.029 | −32.1 ± 0.9 |
| 3 | 228.9 ± 19.6 | 0.154 ± 0.061 | −24.3 ± 0.8 | |
| 6 | 254.8 ± 3.6 | 0.173 ± 0.018 | −18.1 ± 0.5 | |
| THO-NP-P- | 0 | 181.2 ± 4.9 | 0.052 ± 0.014 | −22.8 ± 0.2 |
| 3 | 193.2 ± 3.1 | 0.123 ± 0.032 | −17.1 ± 0.3 | |
| 6 | 196.0 ± 4.1 | 0.123 ± 0.056 | −13.9 ± 0.6 | |
| THO-NP-P-C+ | 0 | 237.5 ± 2.9 | 0.168 ± 0.028 | 24.3 ± 0.7 |
| 3 | 326.9 ± 9.6 | 0.167 ± 0.06 | 20.1 ± 0.2 | |
| 6 | 344.4 ± 8.3 | 0.174 ± 0.02 | 16.5 ± 0.4 |
| t (Months) | Zav (nm) | PI | |
|---|---|---|---|
| GC-THO-NP-L- | 0 | 268.0 ± 6.5 | 0.306 ± 0.080 |
| 3 | 293.6 ± 16.5 | 0.374 ± 0.112 | |
| 6 | 297.9 ± 38.4 | 0.364 ± 0.109 |
| Parameters | GC-THO | GC-THO-NP-L- | |
|---|---|---|---|
| Rheology | Viscosity at 100 s−1 (Pa·s) | 1.01 ± 0.00 | 0.37 ± 0.00 |
| Flow | Shear thinning | Shear thinning | |
| Equation | Herschel–Bulkley | Herschel–Bulkley | |
| r (up/down) | 1/1 | 1/1 | |
| Extensibility | Eₘₐₓ | 25.09 ± 2.21 | 45.71 ± 4.12 |
| Km | 37.02 ± 3.81 | 31.44 ± 3.91 | |
| Equation | Hyperbola | Hyperbola | |
| r2 | 0.9347 | 0.9611 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Folle, C.; Díaz-Garrido, N.; Mallandrich, M.; Suñer-Carbó, J.; Sánchez-López, E.; Halbaut, L.; Marqués, A.M.; Espina, M.; Badia, J.; Baldoma, L.; et al. Hydrogel of Thyme-Oil-PLGA Nanoparticles Designed for Skin Inflammation Treatment. Gels 2024, 10, 149. https://doi.org/10.3390/gels10020149
Folle C, Díaz-Garrido N, Mallandrich M, Suñer-Carbó J, Sánchez-López E, Halbaut L, Marqués AM, Espina M, Badia J, Baldoma L, et al. Hydrogel of Thyme-Oil-PLGA Nanoparticles Designed for Skin Inflammation Treatment. Gels. 2024; 10(2):149. https://doi.org/10.3390/gels10020149
Chicago/Turabian StyleFolle, Camila, Natalia Díaz-Garrido, Mireia Mallandrich, Joaquim Suñer-Carbó, Elena Sánchez-López, Lyda Halbaut, Ana M. Marqués, Marta Espina, Josefa Badia, Laura Baldoma, and et al. 2024. "Hydrogel of Thyme-Oil-PLGA Nanoparticles Designed for Skin Inflammation Treatment" Gels 10, no. 2: 149. https://doi.org/10.3390/gels10020149