Perilla Seed Oil Enhances Cognitive Function and Mental Health in Healthy Elderly Japanese Individuals by Enhancing the Biological Antioxidant Potential
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Anthropometry, Body Composition, and Dietary Intake Analysis
2.3. Blood Sampling
2.4. Evaluation of Cognitive Functions and Mental Health
2.5. Blood Biochemical Analysis, Fatty Acid Profile, and Apolipoprotein E Genotyping
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics of Participants and Assessment of Dietary Intake
3.2. Cognitive Functions and Mental Health Assessment
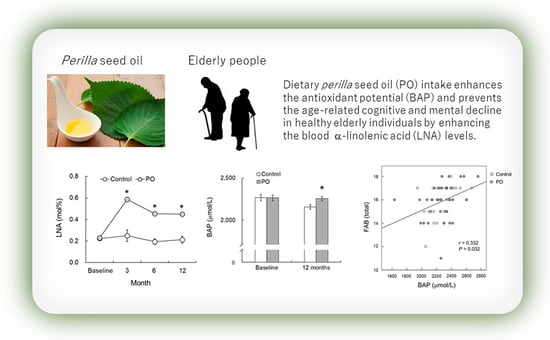
3.3. Fatty Acid Profile of the RBC-PM
3.4. Biological Antioxidant Potential (BAP) and Brain Derived Neurotropic Factor (BDNF) Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Akbaraly, N.T.; Faure, H.; Gourlet, V.; Favier, A.; Berr, C. Plasma carotenoid levels and cognitive performance in an elderly population: Results of the EVA Study. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 308–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, P.Y.; Chiu, C.C.; Huang, S.Y.; Su, K.P. A meta-analytic review of polyunsaturated fatty acid compositions in dementia. J. Clin. Psychiatry 2012, 73, 1245–1254. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Maekawa, M.; Katakura, M.; Hamasaki, K.; Matsuoka, Y. Possibility of polyunsaturated fatty acids for the prevention and treatment of neuropsychiatric illnesses. J. Pharmacol. Sci. 2014, 124, 294–300. [Google Scholar] [CrossRef] [Green Version]
- Freund-Levi, Y.; Eriksdotter-Jönhagen, M.; Cederholm, T.; Basun, H.; Faxén-Irving, G.; Garlind, A.; Vedin, I.; Vessby, B.; Wahlund, L.O.; Palmblad, J. Omega-3 fatty acid treatment in 174 patients with mild to moderate Alzheimer disease: OmegAD study: A randomized double-blind trial. Arch. Neurol. 2006, 63, 1402–1408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashimoto, M.; Yamashita, K.; Kato, S.; Tamai, T.; Tanabe, Y.; Mitarai, M.; Matsumoto, I.; Ohno, M. Beneficial effects of daily dietary omega-3 polyunsaturated fatty acid supplementation on age-related cognitive decline in elderly Japanese with very mild dementia: A 2-year randomized, double-blind, placebo-controlled trial. J. Aging Res. Clin. Pract. 2012, 1, 193–201. [Google Scholar]
- Martí, A.; Fortique, F. Omega-3 fatty acids and cognitive decline: A systematic review. Nutr. Hosp. 2019, 36, 939–949. [Google Scholar]
- Hashimoto, M.; Kato, S.; Tanabe, Y.; Katakura, M.; Mamun, A.A.; Ohno, M.; Yamaguchi, S.; Shido, O. Beneficial effects of dietary docosahexaenoic acid intervention on cognitive function and mental health of the oldest elderly in Japanese care facilities and nursing homes. Geriatr. Gerontol. Int. 2017, 17, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.M. Ethnomedicinal, Phytochemical and Pharmacological Investigations of Perilla frutescens (L.) Britt. Molecules 2018, 24, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burdge, G. Alpha-linolenic acid metabolism in men and women: Nutritional and biological implications. Curr. Opin. Clin. Nutr. Metab. Care 2004, 7, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Campos, H.; Baylin, A.; Willett, W.C. α-Linolenic acid and risk of nonfatal acute myocardial infarction: Campos: α-Linolenic acid myocardial infarction. Circulation 2008, 118, 339–345. [Google Scholar] [CrossRef] [Green Version]
- Albert, C.M.; Oh, K.; Whang, W.; Manson, J.E.; Chae, C.U.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Dietary α-linolenic acid intake and risk of sudden cardiac death and coronary heart disease. Circulation 2005, 112, 3232–3238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, G.; Etherton, T.D.; Martin, K.R.; Gillies, P.J.; West, S.G.; Kris-Etherton, P.M. Dietary alpha-linolenic acid inhibits proinflammatory cytokine production by peripheral blood mononuclear cells in hypercholesterolemic subjects. Am. J. Clin. Nutr. 2007, 85, 385–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguemeni, C.; Delplanque, B.; Rovere, C.; Simon-Rousseau, N.; Gandin, C.; Agnani, G.; Nahon, J.L.; Heurteaux, C.; Blondeau, N. Dietary supplementation of alpha-linolenic acid in an enriched rapeseed oil diet protects from stroke. Pharmacol. Res. 2010, 61, 226–233. [Google Scholar] [CrossRef]
- Lee, J.; Park, S.; Lee, J.Y.; Yeo, Y.K.; Kim, J.S.; Lim, J. Improved spatial learning and memory by perilla diet is correlated with immunoreactivities to neurofilament and α-synuclein in hilus of dentate gyrus. Proteome Sci. 2012, 10, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashimoto, M.; Matsuzaki, K.; Kato, S.; Hossain, S.; Ohno, M.; Shido, O. Twelve-month Studies on Perilla Oil Intake in Japanese Adults-Possible Supplement for Mental Health. Foods 2020, 9, 530–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef]
- Imai, Y.; Hasegawa, K. The revised Hasegawa’s dementia scale (HDS-R)-Evaluation of its usefulness as a screening test for dementia. J. Hong Kong Coll. Psychiatr. 1994, 4, 20–24. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Dubois, B.; Slachevsky, A.; Litvan, I.; Pillon, B. The FAB: A Frontal Assessment Battery at bedside. Neurology 2000, 55, 1621–1626. [Google Scholar] [CrossRef] [Green Version]
- Okada, K.; Kobayashi, S.; Aoki, K.; Suyama, N.; Yamagata, S. Assessment of moti-vational loss in poststroke patients using the Japanese version of Starkstein’s Apathy Scale (in Japanese). Jpn. J. Stroke 1998, 20, 318–327. [Google Scholar] [CrossRef] [Green Version]
- Zung, W.W. A SELF-RATING DEPRESSION SCALE. Arch. Gen. Psychiatr. 1965, 12, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Shinozuka, K.; Gamoh, S.; Tanabe, Y.; Hossain, M.S.; Kwon, Y.H.; Hata, N.; Misawa, Y.; Kunitomo, M.; Masumura, S. The hypotensive effect of docosahexaenoic acid is associated with the enhanced release of ATP from the caudal artery of aged rats. J. Nutr. 1999, 129, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Longvah, T.; Deosthale, Y.G.; Kumar, U.P. Nutritional and short term toxicological evaluation of perilla seed oil. Food Chem. 2000, 70, 13–16. [Google Scholar] [CrossRef]
- Blondeau, N.; Nguemeni, C.; Debruyne, D.N.; Piens, M.; Wu, X.; Pan, H.; Hu, X.; Gandin, C.; Lipsky, R.H.; Plumier, J.C.; et al. Subchronic alpha-linolenic acid treatment enhances brain plasticity and exerts an antidepressant effect: A versatile potential therapy for stroke. Neuropsychopharmacology 2009, 34, 2548–2559. [Google Scholar] [CrossRef] [Green Version]
- Feng, Z.; Zou, X.; Jia, H.; Li, X.; Zhu, Z.; Liu, X.; Bucheli, P.; Ballevre, O.; Hou, Y.; Zhang, W.; et al. Maternal docosahexaenoic acid feeding protects against impairment of learning and memory and oxidative stress in prenatally stressed rats: Possible role of neuronal mitochondria metabolism. Antioxid. Redox Signal. 2012, 16, 275–289. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.B.; Nam, Y.A.; Kim, H.S.; Hayes, A.W.; Lee, B.M. Alpha-linolenic acid: Nutraceutical, pharmacological and toxicological evaluation. Food Chem. Toxicol. 2014, 70, 163–178. [Google Scholar] [CrossRef]
- Kamalashiran, C.; Sriyakul, K.; Pattaraarchachai, J.; Muengtaweepongsa, S. Outcomes of Perilla Seed Oil as an Additional Neuroprotective Therapy in Patients with Mild to Moderate Dementia: A Randomized Control Trial. Curr. Alzheimer Res. 2019, 16, 146–155. [Google Scholar] [CrossRef]
- Jansen, E.; Ruskovska, T. Comparative analysis of plasma (anti)oxidative status parameters in healthy persons. Int. J. Mol. Sci. 2013, 14, 6106–6115. [Google Scholar] [CrossRef] [Green Version]
- Pesce, M.; Tatangelo, R.; La, F.I.; Rizzuto, A.; Campagna, G.; Turli, C.; Ferrone, A.; Franceschelli, S.; Speranza, L.; Patruno, A.; et al. Aging-Related Oxidative Stress: Positive Effect of Memory Training. Neuroscience 2018, 370, 246–255. [Google Scholar] [CrossRef]
- Hetyey, C.S.; Manczur, F.; Dudás-Györki, Z.; Reiczigel, J.; Ribiczey, P.; Vajdovich, P.; Vörös, K. Plasma antioxidant capacity in dogs with naturally occurring heart diseases. J. Vet. Med. A Physiol. Pathol. Clin. Med. 2007, 54, 36–39. [Google Scholar] [CrossRef]
- Zhou, X.J.; Yan, L.L.; Yin, P.P.; Shi, L.L.; Zhang, J.H.; Liu, Y.J.; Ma, C. Structural characterisation and antioxidant activity evaluation of phenolic compounds from cold-pressed Perilla frutescens var. arguta seed flour. Food Chem. 2014, 164, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.; Lee, M.H.; Lee, S.; Cho, E.J. Alpha-Linolenic Acid from Perilla frutescens var. japonica Oil Protects Aβ-Induced Cognitive Impairment through Regulation of APP Processing and Aβ Degradation. J. Agric. Food Chem. 2017, 65, 10719–10729. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Hossain, S.; Al Mamun, A.; Matsuzaki, K.; Arai, H. Docosahexaenoic acid: One molecule diverse functions. Crit. Rev. Biotechnol. 2017, 37, 579–597. [Google Scholar] [CrossRef]
- Crupi, R.; Marino, A.; Cuzzocrea, S. n-3 fatty acids: Role in neurogenesis and neuroplasticity. Curr. Med. Chem. 2013, 20, 2953–2963. [Google Scholar] [CrossRef] [PubMed]
- Francois, C.A.; Connor, S.L.; Bolewicz, L.C.; Connor, W.E. Supplementing lactating women with flaxseed oil does not increase docosahexaenoic acid in their milk. Am. J. Clin. Nutr. 2003, 77, 226–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emmison, N.; Gallagher, P.A.; Coleman, R.A. Linoleic and linolenic acids are selectively secreted in triacylglycerol by hepatocytes from neonatal rats. Am. J. Physiol. 1995, 269, R80–R86. [Google Scholar] [CrossRef] [PubMed]
- Freemantle, E.; Vandal, M.; Tremblay-Mercier, J.; Tremblay, S.; Blachère, J.C.; Bégin, M.E.; Brenna, J.T.; Windust, A.; Cunnane, S.C. Omega-3 fatty acids, energy substrates, and brain function during aging. Prostaglandins Leukot. Essent. Fat. Acids 2006, 75, 213–220. [Google Scholar] [CrossRef]
- Su, K.P.; Lai, H.C.; Yang, H.T.; Su, W.P.; Peng, C.Y.; Chang, J.P.; Chang, H.C.; Pariante, C.M. Omega-3 fatty acids in the prevention of interferon-alpha-induced depression: Results from a randomized, controlled trial. Biol. Psychiatry 2014, 76, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Nettiksimmons, J.; Simonsick, E.M.; Harris, T.; Satterfield, S.; Rosano, C.; Yaffe, K.; for the Health ABC Study. The associations between serum brain-derived neurotrophic factor, potential confounders, and cognitive decline: A longitudinal study. PLoS ONE 2014, 9, e91339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angelucci, F.; Spalletta, G.; di Iulio, F.; Ciaramella, A.; Salani, F.; Colantoni, L.; Varsi, A.E.; Gianni, W.; Sancesario, G.; Caltagirone, C.; et al. Alzheimer’s disease (AD) and Mild Cognitive Impairment (MCI) patients are characterized by increased BDNF serum levels. Curr. Alzheimer Res. 2010, 7, 15–20. [Google Scholar] [CrossRef]
- Håkansson, K.; Ledreux, A.; Daffner, K.; Terjestam, Y.; Bergman, P.; Carlsson, R.; Kivipelto, M.; Winblad, B.; Granholm, A.C.; Mohammed, A.K. BDNF Responses in Healthy Older Persons to 35 Minutes of Physical Exercise, Cognitive Training, and Mindfulness: Associations with Working Memory Function. J. Alzheimers Dis. 2017, 55, 645–657. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Tozawa, R.; Katakura, M.; Shahdat, H.; Haque, A.M.; Tanabe, Y.; Gamoh, S.; Shido, O. Protective effects of prescription n-3 fatty acids against impairment of spatial cognitive learning ability in amyloid β-infused rats. Food Funct. 2011, 2, 386–394. [Google Scholar] [CrossRef]
- Pawełczyk, T.; Grancow-Grabka, M.; Trafalska, E.; Szemraj, J.; Żurner, N.; Pawełczyk, A. An increase in plasma brain derived neurotrophic factor levels is related to n-3 polyunsaturated fatty acid efficacy in first episode schizophrenia: Secondary outcome analysis of the OFFER randomized clinical trial. Psychopharmacology 2019, 236, 2811–2822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamazaki, K.; Itomura, M.; Hamazaki, T.; Sawazaki, S. Effects of cooking plant oils on recurrent aphthous stomatitis: A randomized, placebo-controlled, double-blind trial. Nutrition 2006, 22, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Burdge, G.C.; Wootton, S.A. Conversion of alpha-linolenic acid to palmitic, palmitoleic, stearic and oleic acids in men and women. Prostaglandins. Leukot. Essent. Fat. Acids 2003, 69, 283–290. [Google Scholar] [CrossRef]
- Burdge, G.C. Dietary a-linolenic acid nd health-related outcomes: A metabolic perspective. Nutr. Res. Rev. 2006, 19, 26–52. [Google Scholar] [CrossRef]
- Bourre, J.M.; Piciotti, M.; Dumont, O. ∆6-desaturase in brain and liver during development and aging. Lipids 1990, 25, 354–356. [Google Scholar] [CrossRef]
- Davidson, Y.; Gibbons, L.; Pritchard, A.; Hardicre, J.; Wren, J.; Stopford, C.; Julien, C.; Thompson, J.; Payton, A.; Pickering-Brown, S.M.; et al. Apolipoprotein E epsilon4 allele frequency and age at onset of Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 2007, 23, 60–66. [Google Scholar] [CrossRef]
- Heffernan, A.L.; Chidgey, C.; Peng, P.; Masters, C.L.; Roberts, B.R. The Neurobiology and Age-Related Prevalence of the ε4 Allele of Apolipoprotein E in Alzheimer’s Disease Cohorts. J. Mol. Neurosci. 2016, 60, 316–324. [Google Scholar] [CrossRef] [Green Version]
- Alata, W.; Ye, Y.; St-Amour, I.; Vandal, M.; Calon, F. Human apolipoprotein E ε4 expression impairs cerebral vascularization and blood-brain barrier function in mice. J. Cereb. Blood Flow Metab. 2015, 35, 86–94. [Google Scholar] [CrossRef]
- Theendakara, V.; Peters-Libeu, C.A.; Spilman, P.; Poksay, K.S.; Bredesen, D.E.; Rao, R.V. Direct Transcriptional Effects of Apolipoprotein E. J. Neurosci. 2016, 36, 685–700. [Google Scholar] [CrossRef] [Green Version]
- Fenesi, B.; Fang, H.; Kovacevic, A.; Oremus, M.; Raina, P.; Heisz, J.J. Physical Exercise Moderates the Relationship of Apolipoprotein E (APOE) Genotype and Dementia Risk: A Population-Based Study. J. Alzheimers Dis. 2017, 56, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Ward, A.; Crean, S.; Mercaldi, C.J.; Collins, J.M.; Boyd, D.; Cook, M.N.; Arrighi, H.M. Prevalence of apolipoprotein E4 genotype and homozygotes (APOE e4/4) among patients diagnosed with Alzheimer’s disease: A systematic review and meta-analysis. Neuroepidemiology 2012, 38, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, F.; Liu, J.; Zhang, O.; Lei, P. Inverse Relationship between Baseline Serum Albumin Levels and Risk of Mild Cognitive Impairment in Elderly: A Seven-Year Retrospective Cohort Study. Tohoku J. Exp. Med. 2018, 246, 51–57. [Google Scholar] [CrossRef] [Green Version]
- Zheng, F.; Yan, L.; Yang, Z.; Zhong, B.; Xie, W. HbA1c, diabetes and cognitive decline: The English Longitudinal Study of Ageing. Diabetologia 2018, 61, 839–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Fatty Acids (g/100 g) | Canola Oil | Perilla Seed Oil |
|---|---|---|
| Palmitic acid (C16:0) | 4.3 | 5.6 |
| Stearic acid (C18:0) | 2.09 | 1.7 |
| Oleic acid (C16:0, ω-9) | 61.7 | 12 |
| Linoleic acid (C18:2, ω-6) | 19 | 13.9 |
| α-linolenic acid (C18:3, ω-3) | 9.14 | 62.2 |
| Control (n = 33) | PO (n = 42) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | Min | Max | Mean | Median | Min | Max | p Value | |
| Anthropometry | |||||||||
| Sex (male/female) | 16/17 | 19/23 | |||||||
| Age (years) | 71.0 | 71.3 | 64 | 84 | 71.0 | 70.5 | 65 | 83 | 0.988 |
| Height (cm) | 155.3 | 153.8 | 137.0 | 173.3 | 155.9 | 155.3 | 136.0 | 175.0 | 0.776 |
| Body Weight (kg) | 55.5 | 58.3 | 34.6 | 75.1 | 54.9 | 53.5 | 36.5 | 80.8 | 0.818 |
| BMI (kg/m2) | 22.9 | 22.4 | 15.4 | 28.6 | 22.4 | 22.3 | 16.9 | 32.5 | 0.641 |
| BC (cm) | 84.4 | 84.6 | 64.0 | 100.0 | 82.5 | 82.0 | 63.0 | 116.0 | 0.409 |
| Body fat (%) | 26.5 | 26.2 | 10.9 | 38.5 | 26.5 | 25.3 | 16.8 | 36.3 | 0.993 |
| Blood pressure | |||||||||
| SBP (mmHg) | 148.1 | 147.0 | 116.0 | 198.0 | 148.1 | 147.0 | 106.0 | 198.0 | 0.995 |
| DBP (mmHg) | 81.3 | 81.0 | 57.0 | 102.0 | 84.1 | 83.0 | 49.0 | 107.0 | 0.312 |
| Cognitive index | |||||||||
| HDS-R score | 28.1 | 29.0 | 22.0 | 30.0 | 27.8 | 28.0 | 18.0 | 30.0 | 0.503 |
| MMSE score | 28.4 | 29.0 | 24.0 | 30.0 | 28.3 | 29.0 | 22.0 | 30.0 | 0.412 |
| FAB score | 15.7 | 16.0 | 11.0 | 18.0 | 15.5 | 16.0 | 8.0 | 18.0 | 0.507 |
| Emotional index | |||||||||
| SDS score | 32.6 | 31.0 | 20.0 | 49.0 | 32.9 | 31.5 | 22.0 | 52.0 | 0.869 |
| Apathy score | 10.3 | 11.0 | 1.0 | 24.0 | 10.3 | 10.0 | 2.0 | 23.0 | 0.981 |
| Blood biochemistry | |||||||||
| GOT (U/L) | 25.6 | 25.0 | 17.0 | 43.0 | 26.1 | 26.0 | 16.0 | 40.0 | 0.695 |
| GPT (U/L) | 22.6 | 19.0 | 8.0 | 64.0 | 21.0 | 19.0 | 12.0 | 39.0 | 0.465 |
| γ-GT (IU/L) | 39.7 | 22.0 | 11.0 | 365.0 | 36.6 | 23.0 | 8.0 | 167.0 | 0.787 |
| ALB (g/dL) | 4.3 | 4.3 | 3.4 | 4.9 | 4.4 | 4.4 | 4.1 | 5.1 | 0.002 |
| TC (mg/dL) | 208.0 | 207.0 | 161.0 | 296.0 | 215.8 | 215.0 | 144.0 | 294.0 | 0.305 |
| TG (mg/dL) | 112.7 | 98.0 | 53.0 | 255.0 | 118.6 | 108.0 | 50.0 | 308.0 | 0.636 |
| BUN (mg/dL) | 16.0 | 15.0 | 9.5 | 26.1 | 15.9 | 15.2 | 10.4 | 35.7 | 0.867 |
| CRE (mg/dL) | 0.7 | 0.7 | 0.5 | 1.5 | 0.7 | 0.7 | 0.5 | 1.6 | 0.824 |
| BS (mg/dL) | 113.8 | 99.0 | 84.0 | 252.0 | 97.2 | 94.0 | 69.0 | 191.0 | 0.018 |
| HDL-C (mg/dL) | 60.5 | 59.0 | 32.0 | 99.0 | 65.7 | 62.0 | 40.0 | 113.0 | 0.202 |
| LDL-C (mg/dL) | 124.9 | 112.0 | 68.0 | 210.0 | 126.2 | 129.0 | 73.0 | 184.0 | 0.838 |
| HbA1c (NGSP) (%) | 6.2 | 5.9 | 5.2 | 10.7 | 5.7 | 5.6 | 5.2 | 6.8 | 0.004 |
| Baseline | Month 12 | Month 12—Baseline | ||||||
|---|---|---|---|---|---|---|---|---|
| Unit | Control (n = 33) | PO (n = 42) | Control (n = 24) | PO (n = 35) | Control (n = 24) | PO (n = 35) | p-Value | |
| Energy | KJ/d | 8774 ± 565 | 9302 ± 493 | 8326 ± 454 | 8560 ± 1905 | −448 ± 473 | −742 ± 371 | 0.670 |
| Protein | g/d | 84.4 ± 4.8 | 92.0 ± 6.4 | 79.6 ± 5.6 | 83.6 ± 5.3 | −4.7 ± 5.9 | −8.4 ± 3.5 | 0.452 |
| Fat | g/d | 63.9 ± 4.3 | 65.2 ± 4.6 | 58.5 ± 4.2 | 58.1 ± 3.9 | −5.4 ± 3.7 | −7.1 ± 2.8 | 0.704 |
| Carbohydrate | g/d | 277.3 ± 22.5 | 279.9 ± 15.4 | 266.9 ± 15.9 | 262.9 ± 14.8 | −10.4 ± 18.5 | −17.0 ± 14.7 | 0.779 |
| Total dietary fiber | g/d | 15.0 ± 1.1 | 15.6 ± 1.0 | 14.8 ± 1.3 | 15.7 ± 1.1 | −0.2 ± 1.3 | 0.1 ± 0.9 | 0.842 |
| Saturated fat | g/d | 22.3 ± 1.3 | 17.8 ± 1.3 | 15.3 ± 1.2 | 15.3 ± 1.1 | −2.0 ± 1.0 | −2.5 ± 0.8 | 0.713 |
| Monounsaturated fat | g/d | 15.4 ± 1.6 | 22.8 ± 1.7 | 20.7 ± 1.6 | 20.5 ± 1.5 | −1.6 ± 1.4 | −2.3 ± 1.1 | 0.668 |
| Polyunsaturated fat | g/d | 15.0 ± 0.9 | 15.4 ± 1.1 | 14.7 ± 1.0 | 13.9 ± 0.9 | −0.7 ± 0.9 | −1.4 ± 0.7 | 0.524 |
| ω-6 polyunsaturated fat | g/d | 11.8 ± 0.7 | 11.6 ± 0.8 | 11.5 ± 0.8 | 10.6 ± 0.7 | −0.4 ± 0.6 | −1.0 ± 0.5 | 0.507 |
| ω-3 polyunsaturated fat | g/d | 3.5 ± 0.3 | 3.7 ± 0.3 | 3.2 ± 0.2 | 3.3 ± 0.2 | −0.3 ± 0.3 | −0.5 ± 0.2 | 0.667 |
| LNA (C18:3ω-3) | g/d | 1.84 ± 0.12 | 1.82 ± 0.13 | 1.84 ± 0.14 | 1.69 ± 0.12 | 0.005 ± 0.1 | −0.13 ± 0.09 | 0.353 |
| EPA (C20:5ω-3) | g/d | 0.51 ± 0.06 | 0.59 ± 0.06 | 0.41 ± 0.04 | 0.48 ± 0.04 | −0.098 ± 0.06 | −0.11 ± 0.05 | 0.919 |
| DHA (C22:6ω-3) | g/d | 0.84 ± 0.09 | 0.96 ± 0.10 | 0.68 ± 0.06 | 0.74 ± 0.06 | −0.16 ± 0.10 | −0.16 ± 0.07 | 0.976 |
| Control (n = 24) | PO (n = 35) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | Min | Max | Mean | Median | Min | Max | p-Value | |
| Anthropometry | |||||||||
| Sex (male/female) | 12/12 | 16/19 | |||||||
| Age (years) | 72.0 | 71.3 | 65 | 85 | 72.0 | 70.8 | 66 | 84 | 0.883 |
| Height (cm) | 154.6 | 154.7 | 136.0 | 170.5 | 156.3 | 155.7 | 136.4 | 175.0 | 0.502 |
| Body Weight (kg) | 55.9 | 59.9 | 38.1 | 77.9 | 54.4 | 52.5 | 35.2 | 81.0 | 0.512 |
| BMI (kg/m2) | 23.3 | 23.1 | 17.5 | 29.8 | 22.1 | 21.7 | 16.3 | 32.1 | 0.100 |
| BC (cm) | 85.7 | 86.5 | 65.5 | 103.0 | 82.0 | 82.6 | 63.0 | 115.0 | 0.103 |
| Body fat (%) | 26.1 | 25.4 | 6.7 | 41.4 | 25.4 | 24.4 | 14.6 | 42.2 | 0.578 |
| Blood pressure | |||||||||
| SBP (mmHg) | 143.6 | 136.0 | 104.0 | 188.0 | 135.7 | 139.0 | 99.0 | 174.0 | 0.396 |
| DBP (mmHg) | 79.3 | 76.7 | 56.0 | 106.0 | 76.5 | 76.3 | 55.0 | 99.0 | 0.552 |
| Cognitive index | |||||||||
| HDS-R score | 28.7 | 28.8 | 26.0 | 30.0 | 29.1 | 29.3 | 26.0 | 30.0 | 0.194 |
| MMSE score | 29.0 | 29.0 | 25.0 | 30.0 | 29.2 | 29.4 | 26.0 | 30.0 | 0.865 |
| FAB score | 16.0 | 16.2 | 12.0 | 18.0 | 16.5 | 16.8 | 13.0 | 18.0 | 0.223 |
| Emotional index | |||||||||
| SDS score | 32.3 | 30.3 | 21.0 | 54.0 | 31.9 | 31.0 | 22.0 | 51.0 | 0.547 |
| Apathy score | 9.5 | 9.0 | 0.0 | 19.0 | 8.4 | 8.1 | 0.0 | 26.0 | 0.383 |
| Blood biochemistry | |||||||||
| GOT (U/L) | 24.7 | 24.3 | 18.0 | 46.0 | 26.1 | 24.0 | 16.0 | 60.0 | 0.792 |
| GPT (U/L) | 19.2 | 16.3 | 11.0 | 46.0 | 20.1 | 17.7 | 10.0 | 53.0 | 0.501 |
| γ-GT (IU/L) | 31.6 | 19.3 | 13.0 | 172.0 | 29.6 | 23.5 | 11.0 | 102.0 | 0.677 |
| ALB (g/dL) | 4.2 | 4.2 | 3.4 | 4.6 | 4.3 | 4.3 | 3.9 | 4.9 | 0.134 |
| TC (mg/dL) | 196.0 | 196.0 | 124.0 | 255.0 | 205.1 | 202.0 | 144.0 | 279.0 | 0.342 |
| TG (mg/dL) | 105.1 | 91.0 | 51.0 | 264.0 | 108.1 | 82.0 | 41.0 | 402.0 | 0.605 |
| BUN (mg/dL) | 16.5 | 15.7 | 11.3 | 24.5 | 16.6 | 16.0 | 9.8 | 23.6 | 0.896 |
| CRE (mg/dL) | 0.8 | 0.7 | 0.5 | 1.9 | 0.8 | 0.7 | 0.5 | 1.5 | 0.694 |
| BS (mg/dL) | 105.7 | 98.0 | 88.0 | 166.0 | 100.9 | 97.3 | 73.0 | 216.0 | 0.290 |
| HDL-C (mg/dL) | 57.4 | 56.3 | 31.0 | 80.0 | 64.9 | 64.3 | 40.0 | 94.0 | 0.068 |
| LDL-C (mg/dL) | 117.9 | 112.5 | 70.0 | 167.0 | 119.3 | 124.0 | 49.0 | 191.0 | 0.796 |
| HbA1c (NGSP) (%) | 6.2 | 6.0 | 5.3 | 7.9 | 5.8 | 5.7 | 5.2 | 6.9 | 0.020 |
| Baseline | 12-Months | ||||
|---|---|---|---|---|---|
| Control (n = 33) | PO (n = 42) | Control (n = 24) | PO (n = 35) | p-Value | |
| Fatty acid (mol%) | |||||
| PLA | 25.8 ± 0.2 | 25.6 ± 0.2 | 23.6 ± 0.5 | 24.0 ± 0.4 | 0.557 |
| POA | 0.4 ± 0.0 | 0.4 ± 0.0 | 0.5 ± 0.1 | 0.5 ± 0.0 | 0.591 |
| STA | 17.8 ± 0.2 | 17.7 ± 0.2 | 17.5 ± 0.3 | 18.0 ± 0.3 | 0.284 |
| OLA | 14.7 ± 0.5 | 14.6 ± 0.5 | 15.8 ± 0.3 | 15.9 ± 0.3 | 0.430 |
| LLA | 11.3 ± 0.3 | 11.6 ± 0.3 | 11.7 ± 0.3 | 11.7 ± 0.5 | 0.965 |
| LNA | 0.2 ± 0.0 | 0.2 ± 0.0 | 0.2 ± 0.0 | 0.4 ± 0.0 | <0.0001 |
| AA | 10.5 ± 0.3 | 11.0 ± 0.3 | 10.8 ± 0.5 | 10.3 ± 0.5 | 0.513 |
| EPA | 2.1 ± 0.2 | 2.0 ± 0.1 | 2.1 ± 0.2 | 2.1 ± 0.1 | 0.774 |
| DPA | 2.0 ± 0.1 | 2.0 ± 0.0 | 1.5 ± 0.1 | 1.5 ± 0.1 | 0.681 |
| C24:0 | 3.7 ± 0.1 | 3.6 ± 0.1 | 4.7 ± 0.1 | 4.8 ± 0.1 | 0.702 |
| DHA | 7.5 ± 0.2 | 7.6 ± 0.2 | 7.6 ± 0.4 | 7.0 ± 0.4 | 0.295 |
| C24:1 | 3.8 ± 0.1 | 3.7 ± 0.1 | 3.9 ± 0.1 | 3.8 ± 0.1 | 0.587 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hashimoto, M.; Matsuzaki, K.; Hossain, S.; Ito, T.; Wakatsuki, H.; Tanabe, Y.; Ohno, M.; Kato, S.; Yamashita, K.; Shido, O. Perilla Seed Oil Enhances Cognitive Function and Mental Health in Healthy Elderly Japanese Individuals by Enhancing the Biological Antioxidant Potential. Foods 2021, 10, 1130. https://doi.org/10.3390/foods10051130
Hashimoto M, Matsuzaki K, Hossain S, Ito T, Wakatsuki H, Tanabe Y, Ohno M, Kato S, Yamashita K, Shido O. Perilla Seed Oil Enhances Cognitive Function and Mental Health in Healthy Elderly Japanese Individuals by Enhancing the Biological Antioxidant Potential. Foods. 2021; 10(5):1130. https://doi.org/10.3390/foods10051130
Chicago/Turabian StyleHashimoto, Michio, Kentaro Matsuzaki, Shahdat Hossain, Tomoko Ito, Harumi Wakatsuki, Yoko Tanabe, Miho Ohno, Setsushi Kato, Kazuya Yamashita, and Osamu Shido. 2021. "Perilla Seed Oil Enhances Cognitive Function and Mental Health in Healthy Elderly Japanese Individuals by Enhancing the Biological Antioxidant Potential" Foods 10, no. 5: 1130. https://doi.org/10.3390/foods10051130