Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications
Abstract
:1. Introduction
1.1. Definition of Hypoglycemia
1.2. Symptoms of Hypoglycemia
1.3. Risk Factors for Hypoglycemia
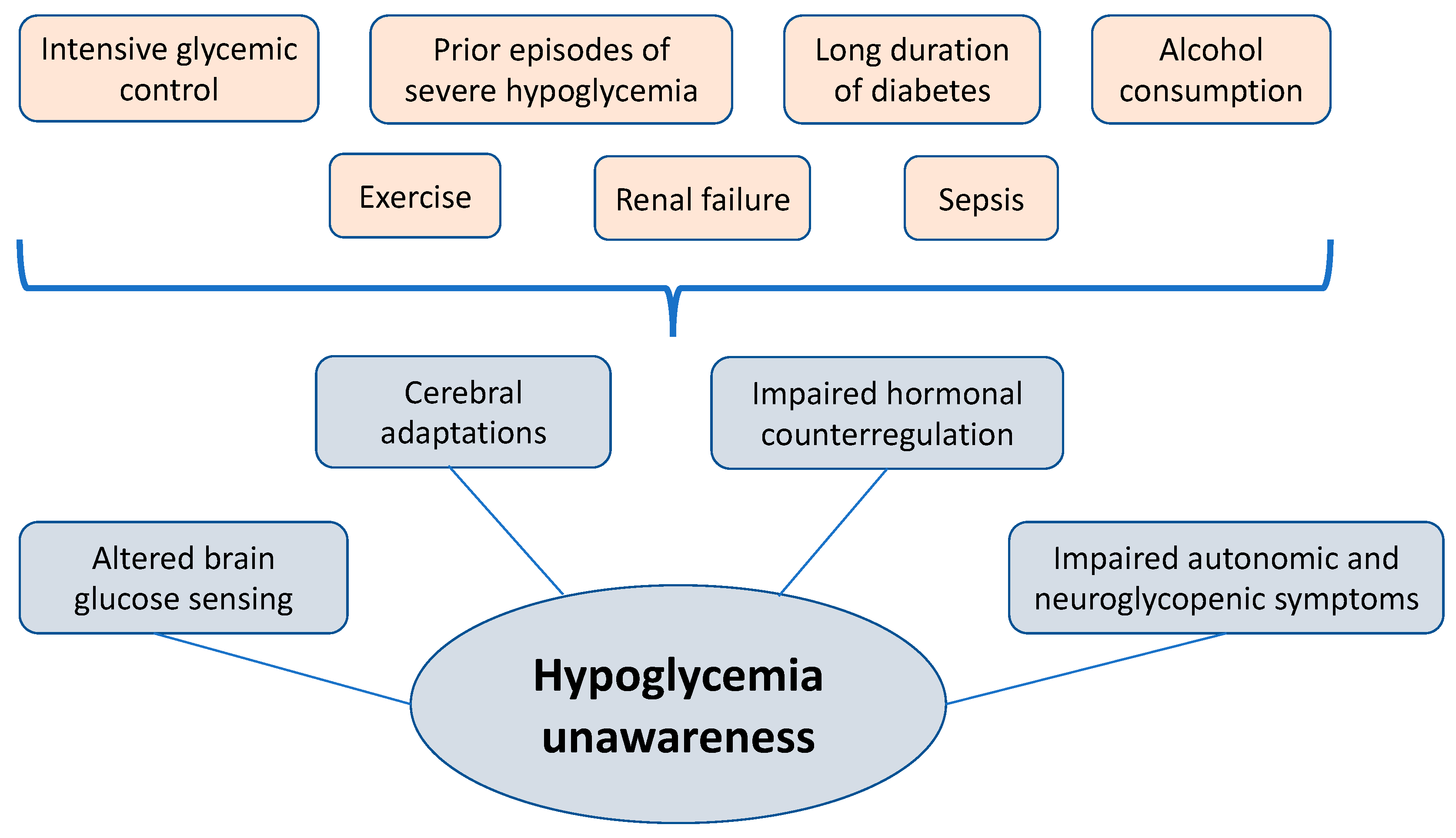
2. Pathophysiology of Hypoglycemia Unawareness Syndrome
2.1. Autonomic Failure
2.2. Altered Brain Glucose Sensing
2.3. Cerebral Adaptations
2.4. Hormonal Regulation
2.5. Sleep
2.6. Consequences
3. Therapeutic Strategies
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: A report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care 2005, 28, 1245–1249. [Google Scholar] [CrossRef] [PubMed]
- Agiostratidou, G.; Anhalt, H.; Ball, D.; Blonde, L.; Gourgari, E.; Harriman, K.N.; Kowalski, A.J.; Madden, P.; McAuliffe-Fogarty, A.H.; McElwee-Malloy, M.; et al. Standardizing Clinically Meaningful Outcome Measures beyond HbA1c for Type 1 Diabetes: A Consensus Report of the American Association of Clinical Endocrinologists, the American Association of Diabetes Educators, the American Diabetes Association, the Endocrine Society, JDRF International, The Leona M. and Harry B. Helmsley Charitable Trust, the Pediatric Endocrine Society, and the T1D Exchange. Diabetes Care 2017, 40, 1622–1630. [Google Scholar] [CrossRef] [PubMed]
- McAulay, V.; Deary, I.J.; Frier, B.M. Symptoms of hypoglycaemia in people with diabetes. Diabet. Med. 2001, 18, 690–705. [Google Scholar] [CrossRef] [PubMed]
- Deary, I.J.; Hepburn, D.A.; MacLeod, K.M.; Frier, B.M. Partitioning the symptoms of hypoglycaemia using multi-sample confirmatory factor analysis. Diabetologia 1993, 36, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Oh, T.J.; Lee, Y.A.; Bae, J.H.; Kim, H.J.; Jung, H.S.; Cho, Y.M.; Park, K.S.; Lim, S.; Jang, H.C.; et al. Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea. Diabetes Metab. J. 2011, 35, 166. [Google Scholar] [CrossRef] [PubMed]
- Allen, C.; LeCaire, T.; Palta, M.; Daniels, K.; Meredith, M.; D’Alessio, D.J.; Wisconsin Diabetes Registry Project. Risk Factors for Frequent and Severe Hypoglycemia in Type 1 Diabetes. Diabetes Care 2001, 24, 1878–1881. [Google Scholar] [CrossRef]
- Weinstock, R.S.; DuBose, S.N.; Bergenstal, R.M.; Chaytor, N.S.; Peterson, C.; Olson, B.A.; Munshi, M.N.; Perrin, A.J.; Miller, K.M.; Beck, R.W.; et al. Risk Factors Associated with Severe Hypoglycemia in Older Adults with Type 1 Diabetes. Diabetes Care 2016, 39, 603–610. [Google Scholar] [CrossRef]
- Matyka, K.A. Sweet dreams?—Nocturnal hypoglycemia in children with type 1 diabetes: Nocturnal hypoglycemia in type 1 diabetes. Pediatr. Diabetes 2002, 3, 74–81. [Google Scholar] [CrossRef]
- Kalra, S.; Mukherjee, J.; Venkataraman, S.; Bantwal, G.; Shaikh, S.; Saboo, B.; Das, A.K.; Ramachandran, A. Hypoglycemia: The neglected complication. Indian J. Endocr. Metab. 2013, 17, 819. [Google Scholar] [CrossRef]
- Cryer, P.E.; Davis, S.N.; Shamoon, H. Hypoglycemia in Diabetes. Diabetes Care 2003, 26, 1902–1912. [Google Scholar] [CrossRef]
- Lee, C.J.; Brown, T.T.; Schweitzer, M.; Magnuson, T.; Clark, J.M. The incidence and risk factors associated with developing symptoms of hypoglycemia after bariatric surgery. Surg. Obes. Relat. Dis. 2018, 14, 797–802. [Google Scholar] [CrossRef]
- Tack, J.; Arts, J.; Caenepeel, P.; De Wulf, D.; Bisschops, R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 583–590. [Google Scholar] [CrossRef]
- Van Beek, A.P.; Emous, M.; Laville, M.; Tack, J. Dumping syndrome after esophageal, gastric or bariatric surgery: Pathophysiology, diagnosis, and management. Obes. Rev. 2017, 18, 68–85. [Google Scholar] [CrossRef] [PubMed]
- Toft-Nielsen, M.; Madsbad, S.; Holst, J.J. Exaggerated secretion of glucagon-like peptide-1 (GLP-1) could cause reactive hypoglycaemia. Diabetologia 1998, 41, 1180–1186. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, N.; Engström, B.E.; Sundbom, M.; Karlsson, F.A. GLP1 analogs as treatment of postprandial hypoglycemia following gastric bypass surgery: A potential new indication? Eur. J. Endocrinol. 2013, 169, 885–889. [Google Scholar] [CrossRef] [PubMed]
- Danowitz, M.; De Leon, D.D. The Role of GLP-1 Signaling in Hypoglycemia due to Hyperinsulinism. Front. Endocrinol. 2022, 13, 863184. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E. Mechanisms of Hypoglycemia-Associated Autonomic Failure in Diabetes. N. Engl. J. Med. 2013, 369, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E. Hypoglycemia-associated autonomic failure in diabetes. Am. J. Physiol. Endocrinol. Metab. 2001, 281, E1115–E1121. [Google Scholar] [CrossRef] [PubMed]
- Meyhöfer, S.; Dembinski, K.; Schultes, B.; Born, J.; Wilms, B.; Lehnert, H.; Hallschmid, M.; Meyhöfer, S.M. Sleep deprivation prevents counterregulatory adaptation to recurrent hypoglycaemia. Diabetologia 2022, 65, 1212–1221. [Google Scholar] [CrossRef]
- Magistretti, P.J.; Allaman, I. Lactate in the brain: From metabolic end-product to signalling molecule. Nat. Rev. Neurosci. 2018, 19, 235–249. [Google Scholar] [CrossRef]
- Martín-Timón, I. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J. Diabetes 2015, 6, 912. [Google Scholar] [CrossRef] [PubMed]
- Tesfaye, N.; Seaquist, E.R. Neuroendocrine responses to hypoglycemia: Neuroendocrine responses to hypoglycemia. Ann. N. Y. Acad. Sci. 2010, 1212, 12–28. [Google Scholar] [CrossRef] [PubMed]
- McNeilly, A.D.; McCrimmon, R.J. Impaired hypoglycaemia awareness in type 1 diabetes: Lessons from the lab. Diabetologia 2018, 61, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Gerich, J.E.; Langlois, M.; Noacco, C.; Karam, J.H.; Forsham, P.H. Lack of glucagon response to hypoglycemia in diabetes: Evidence for an intrinsic pancreatic alpha cell defect. Science 1973, 182, 171–173. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E. Minireview: Glucagon in the pathogenesis of hypoglycemia and hyperglycemia in diabetes. Endocrinology 2012, 153, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Zhang, T.; Harmon, J.S.; Bryan, J.; Robertson, R.P. Zinc, Not Insulin, Regulates the Rat α-Cell Response to Hypoglycemia In Vivo. Diabetes 2007, 56, 1107–1112. [Google Scholar] [CrossRef] [PubMed]
- De Feo, P.; Perriello, G.; Torlone, E.; Ventura, M.M.; Santeusanio, F.; Brunetti, P.; Gerich, J.E.; Bolli, G.B. Demonstration of a role for growth hormone in glucose counterregulation. Am. J. Physiol. 1989, 256 Pt 1, E835–E843. [Google Scholar] [CrossRef]
- Rizza, R.A.; Cryer, P.E.; Gerich, J.E. Role of glucagon, catecholamines, and growth hormone in human glucose counterregulation. Effects of somatostatin and combined alpha- and beta-adrenergic blockade on plasma glucose recovery and glucose flux rates after insulin-induced hypoglycemia. J. Clin. Invest. 1979, 64, 62–71. [Google Scholar] [CrossRef]
- Boyle, P.J.; Cryer, P.E. Growth hormone, cortisol, or both are involved in defense against, but are not critical to recovery from, hypoglycemia. Am. J. Physiol. 1991, 260 Pt 1, E395–E402. [Google Scholar] [CrossRef]
- Davis, S.N.; Shavers, C.; Costa, F.; Mosqueda-Garcia, R. Role of cortisol in the pathogenesis of deficient counterregulation after antecedent hypoglycemia in normal humans. J. Clin. Invest. 1996, 98, 680–691. [Google Scholar] [CrossRef]
- Meyhöfer, S.; Wilms, B.; Oster, H.; Schmid, S.M. Importance of sleep and circadian rhythm for energy metabolism. Internist 2019, 60, 122–127. [Google Scholar] [CrossRef]
- Meyhöfer, S.; Chamorro, R.; Hallschmid, M.; Spyra, D.; Klinsmann, N.; Schultes, B.; Lehnert, H.; Meyhöfer, S.M.; Wilms, B. Late, but Not Early, Night Sleep Loss Compromises Neuroendocrine Appetite Regulation and the Desire for Food. Nutrients 2023, 15, 2035. [Google Scholar] [CrossRef] [PubMed]
- Schmid, S.M.; Hallschmid, M.; Schultes, B. The metabolic burden of sleep loss. Lancet Diabetes Endocrinol. 2015, 3, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Nofzinger, E.A.; Buysse, D.J.; Miewald, J.M.; Meltzer, C.C.; Price, J.C.; Sembrat, R.C.; Ombao, H.; Reynolds, C.F.; Monk, T.H.; Hall, M.; et al. Human regional cerebral glucose metabolism during non-rapid eye movement sleep in relation to waking. Brain 2002, 125, 1105–1115. [Google Scholar] [CrossRef] [PubMed]
- Robinson, R.T.C.E.; Harris, N.D.; Ireland, R.H.; Macdonald, I.A.; Heller, S.R. Changes in cardiac repolarization during clinical episodes of nocturnal hypoglycaemia in adults with Type 1 diabetes. Diabetologia 2004, 47, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Amin, R.; Ross, K.; Acerini, C.L.; Edge, J.A.; Warner, J.; Dunger, D.B. Hypoglycemia prevalence in prepubertal children with type 1 diabetes on standard insulin regimen: Use of continuous glucose monitoring system. Diabetes Care 2003, 26, 662–667. [Google Scholar] [CrossRef]
- Jauch-Chara, K.; Hallschmid, M.; Gais, S.; Oltmanns, K.M.; Peters, A.; Born, J.; Schultes, B. Awakening and Counterregulatory Response to Hypoglycemia during Early and Late Sleep. Diabetes 2007, 56, 1938–1942. [Google Scholar] [CrossRef] [PubMed]
- Merl, V.; Kern, W.; Peters, A.; Oltmanns, K.M.; Gais, S.; Born, J.; Fehm, H.L.; Schultes, B. Differences between nighttime and daytime hypoglycemia counterregulation in healthy humans. Metabolism 2004, 53, 894–898. [Google Scholar] [CrossRef] [PubMed]
- Schultes, B.; Jauch-Chara, K.; Gais, S.; Hallschmid, M.; Reiprich, E.; Kern, W.; Oltmanns, K.M.; Peters, A.; Fehm, H.L.; Born, J. Defective Awakening Response to Nocturnal Hypoglycemia in Patients with Type 1 Diabetes Mellitus. PLoS Med. 2007, 4, e69. [Google Scholar] [CrossRef] [PubMed]
- Diekelmann, S.; Born, J. The memory function of sleep. Nat. Rev. Neurosci. 2010, 11, 114–126. [Google Scholar] [CrossRef]
- Gold, A.E.; MacLeod, K.M.; Deary, I.J.; Frier, B.M. Hypoglycemia-induced cognitive dysfunction in diabetes mellitus: Effect of hypoglycemia unawareness. Physiol. Behav. 1995, 58, 501–511. [Google Scholar] [CrossRef]
- Bolo, N.R.; Musen, G.; Jacobson, A.M.; Weinger, K.; McCartney, R.L.; Flores, V.; Renshaw, P.F.; Simonson, D.C. Brain activation during working memory is altered in patients with type 1 diabetes during hypoglycemia. Diabetes 2011, 60, 3256–3264. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group; Jacobson, A.M.; Musen, G.; Ryan, C.M.; Silvers, N.; Cleary, P.; Waberski, B.; Burwood, A.; Weinger, K.; Bayless, M.; et al. Long-term effect of diabetes and its treatment on cognitive function. N. Engl. J. Med. 2007, 356, 1842–1852. [Google Scholar] [CrossRef] [PubMed]
- Reichard, P.; Pihl, M. Mortality and treatment side-effects during long-term intensified conventional insulin treatment in the Stockholm Diabetes Intervention Study. Diabetes 1994, 43, 313–317. [Google Scholar] [CrossRef]
- Whitmer, R.A. Hypoglycemic Episodes and Risk of Dementia in Older Patients with Type 2 Diabetes Mellitus. JAMA 2009, 301, 1565. [Google Scholar] [CrossRef]
- Gogitidze Joy, N.; Hedrington, M.S.; Briscoe, V.J.; Tate, D.B.; Ertl, A.C.; Davis, S.N. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. Diabetes Care 2010, 33, 1529–1535. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.; Gibbons, L.W.; Mitchell, T.L.; Kampert, J.B.; Stern, M.P.; Blair, S.N. Low fasting plasma glucose level as a predictor of cardiovascular disease and all-cause mortality. Circulation 2000, 101, 2047–2052. [Google Scholar] [CrossRef]
- Desouza, C.; Salazar, H.; Cheong, B.; Murgo, J.; Fonseca, V. Association of hypoglycemia and cardiac ischemia: A study based on continuous monitoring. Diabetes Care 2003, 26, 1485–1489. [Google Scholar] [CrossRef] [PubMed]
- Evers, I.M.; Ter Braak, E.W.M.T.; De Valk, H.W.; Van Der Schoot, B.; Janssen, N.; Visser, G.H.A. Risk Indicators Predictive for Severe Hypoglycemia during the First Trimester of Type 1 Diabetic Pregnancy. Diabetes Care 2002, 25, 554–559. [Google Scholar] [CrossRef]
- Ter Braak, E.W.M.T.; Evers, I.M.; Willem Erkelens, D.; Visser, G.H.A. Maternal hypoglycemia during pregnancy in type 1 diabetes: Maternal and fetal consequences. Diabetes Metab. Res. Rev. 2002, 18, 96–105. [Google Scholar] [CrossRef]
- Fanelli, C.G.; Epifano, L.; Rambotti, A.M.; Pampanelli, S.; Di Vincenzo, A.; Modarelli, F.; Lepore, M.; Annibale, B.; Ciofetta, M.; Bottini, P.; et al. Meticulous prevention of hypoglycemia normalizes the glycemic thresholds magnitude of most of neuroendocrine responses to symptoms of cognitive function during hypoglycemia in intensively treated patients with short-term, IDDM. Diabetes 1993, 42, 1683–1689. [Google Scholar] [CrossRef] [PubMed]
- Hermanns, N.; Kulzer, B.; Kubiak, T.; Krichbaum, M.; Haak, T. The effect of an education programme (HyPOS) to treat hypoglycaemia problems in patients with type 1 diabetes. Diabetes Metab. Res. Rev. 2007, 23, 528–538. [Google Scholar] [CrossRef] [PubMed]
- Leelarathna, L.; Little, S.A.; Walkinshaw, E.; Tan, H.K.; Lubina-Solomon, A.; Kumareswaran, K.; Lane, A.P.; Chadwick, T.; Marshall, S.M.; Speight, J.; et al. Restoration of self-awareness of hypoglycemia in adults with long-standing type 1 diabetes: Hyperinsulinemic-hypoglycemic clamp substudy results from the HypoCOMPaSS trial. Diabetes Care 2013, 36, 4063–4070. [Google Scholar] [CrossRef] [PubMed]
- Bundesärztekammer (BÄK); Kassenärztliche Bundesvereinigung (KBV); Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). S2k-Leitlinie Diagnostik, Therapie und Verlaufskontrolle des Diabetes mellitus im Alter, 2. Auflage. Diabetol. Und Stoffwechs. 2018, 13, 426–489. [Google Scholar]
- Hirsch, I.B. Insulin analogues. N. Engl. J. Med. 2005, 352, 174–183. [Google Scholar] [CrossRef]
- Lucidi, P.; Porcellati, F.; Bolli, G.B.; Fanelli, C.G. Prevention and Management of Severe Hypoglycemia and Hypoglycemia Unawareness: Incorporating Sensor Technology. Curr. Diab. Rep. 2018, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Lane, W.; Bailey, T.S.; Gerety, G.; Gumprecht, J.; Philis-Tsimikas, A.; Hansen, C.T.; Nielsen, T.S.S.; Warren, M. Effect of Insulin Degludec vs Insulin Glargine U100 on Hypoglycemia in Patients with Type 1 Diabetes: The SWITCH 1 Randomized Clinical Trial. JAMA 2017, 318, 33–44. [Google Scholar] [CrossRef]
- Van Staa, T.; Abenhaim, L.; Monette, J. Rates of hypoglycemia in users of sulfonylureas. J. Clin. Epidemiol. 1997, 50, 735–741. [Google Scholar] [CrossRef]
- Miller, K.M.; Beck, R.W.; Bergenstal, R.M.; Goland, R.S.; Haller, M.J.; McGill, J.B.; Rodriguez, H.; Simmons, J.H.; Hirsch, I.B. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care 2013, 36, 2009–2014. [Google Scholar] [CrossRef]
- Lanzinger, S.; Best, F.; Bergmann, T.; Laimer, M.; Lipovsky, B.; Danne, T.; Zimny, S.; Bramlage, P.; Meyhöfer, S.; Holl, R.W. Dynamics of Hemoglobin A1c, Body Mass Index, and Rates of Severe Hypoglycemia in 4434 Adults with Type 1 or Type 2 Diabetes after Initiation of Continuous Glucose Monitoring. Diabetes Technol. Ther. 2022, 24, 763–769. [Google Scholar] [CrossRef]
- Van den Boom, L.; Karges, B.; Auzanneau, M.; Rami-Merhar, B.; Lilienthal, E.; von Sengbusch, S.; Datz, N.; Schröder, C.; Kapellen, T.; Laimer, M.; et al. Temporal Trends and Contemporary Use of Insulin Pump Therapy and Glucose Monitoring Among Children, Adolescents, and Adults with Type 1 Diabetes Between 1995 and 2017. Diabetes Care 2019, 42, 2050–2056. [Google Scholar] [CrossRef] [PubMed]
- Karges, B.; Schwandt, A.; Heidtmann, B.; Kordonouri, O.; Binder, E.; Schierloh, U.; Boettcher, C.; Kapellen, T.; Rosenbauer, J.; Holl, R.W. Association of Insulin Pump Therapy vs. Insulin Injection Therapy with Severe Hypoglycemia, Ketoacidosis, and Glycemic Control among Children, Adolescents, and Young Adults with Type 1 Diabetes. JAMA 2017, 318, 1358–1366. [Google Scholar] [CrossRef] [PubMed]
- Weisman, A.; Bai, J.-W.; Cardinez, M.; Kramer, C.K.; Perkins, B.A. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: A systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 2017, 5, 501–512. [Google Scholar] [CrossRef] [PubMed]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 7. Diabetes Technology: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46 (Suppl. 1), S111–S127. [Google Scholar] [CrossRef]
- Ekhlaspour, L.; Forlenza, G.P.; Chernavvsky, D.; Maahs, D.M.; Wadwa, R.P.; Deboer, M.D.; Messer, L.H.; Town, M.; Pinnata, J.; Kruse, G.; et al. Closed loop control in adolescents and children during winter sports: Use of the Tandem Control-IQ AP system. Pediatr. Diabetes 2019, 20, 12867. [Google Scholar] [CrossRef]
- Garg, S.K.; Weinzimer, S.A.; Tamborlane, W.V.; Buckingham, B.A.; Bode, B.W.; Bailey, T.S.; Brazg, R.L.; Ilany, J.; Slover, R.H.; Anderson, S.M.; et al. Glucose Outcomes with the In-Home Use of a Hybrid Closed-Loop Insulin Delivery System in Adolescents and Adults with Type 1 Diabetes. Diabetes Technol. Ther. 2017, 19, 155–163. [Google Scholar] [CrossRef]

| Level | Criteria |
|---|---|
| Level 1 | Plasma glucose concentration < 70 mg/dL (<3.9 mmol/L); ≥54 mg/dL (≥3.0 mmol/L) |
| Level 2 | Plasma glucose concentration < 54 mg/dL (<3.0 mmol/L) |
| Level 3 | A severe event characterized by altered mental and/or physical status requiring assistance |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hölzen, L.; Schultes, B.; Meyhöfer, S.M.; Meyhöfer, S. Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications. Biomedicines 2024, 12, 391. https://doi.org/10.3390/biomedicines12020391
Hölzen L, Schultes B, Meyhöfer SM, Meyhöfer S. Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications. Biomedicines. 2024; 12(2):391. https://doi.org/10.3390/biomedicines12020391
Chicago/Turabian StyleHölzen, Laura, Bernd Schultes, Sebastian M. Meyhöfer, and Svenja Meyhöfer. 2024. "Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications" Biomedicines 12, no. 2: 391. https://doi.org/10.3390/biomedicines12020391







