Review of Positive Psychology Applications in Clinical Medical Populations
Abstract
:1. Introduction
1.1 Correlational Studies of Positive Psychology Variables in Medical Populations
1.2 Development of Positive Psychology Interventions
2. Method
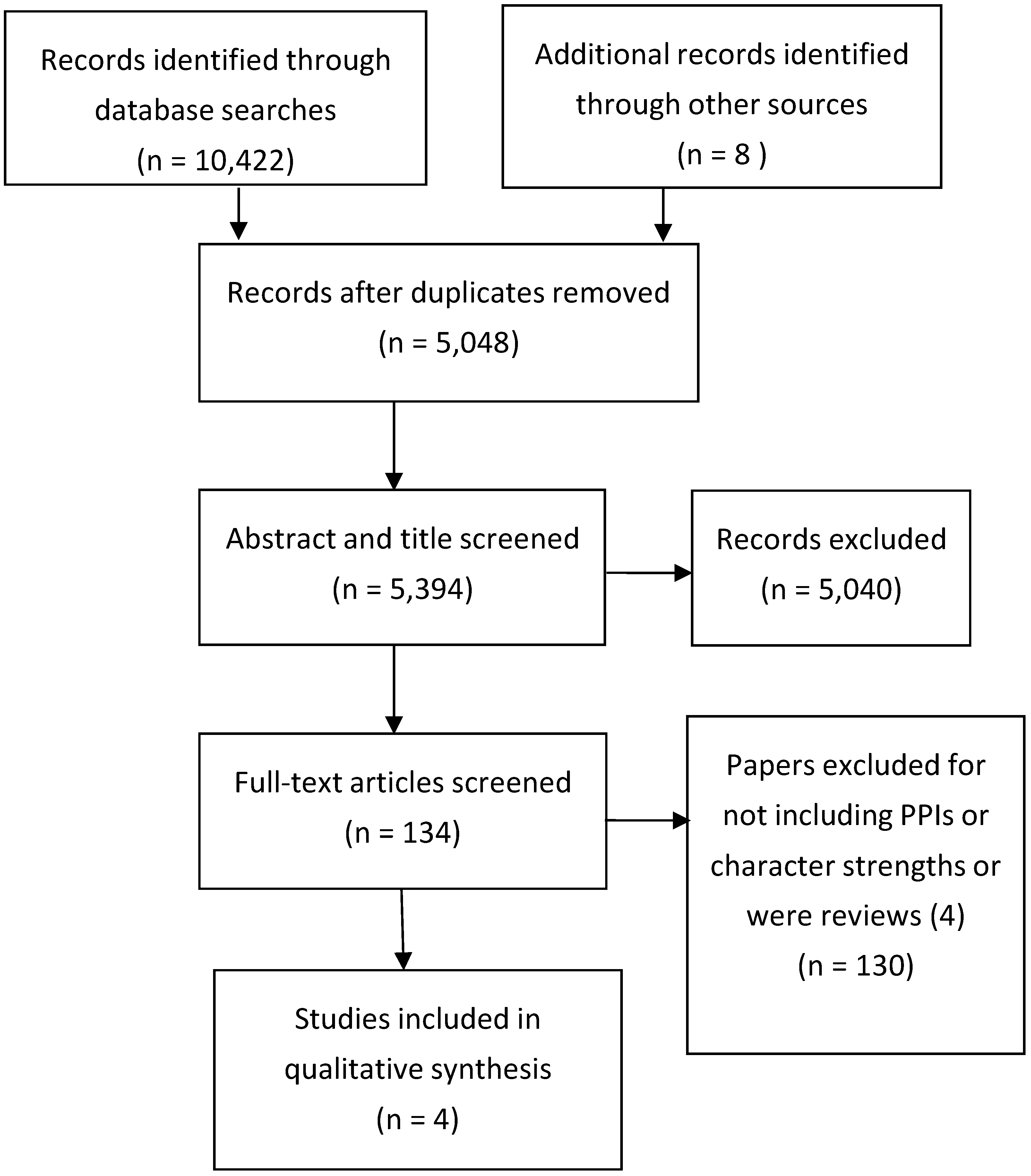
2.1 Literature Search Strategies
2.2. Selection Criteria
2.3. Quality Assessment
3. Results
3.1. Cancer
3.2. Cardiovascular Disease
3.3. Diabetes
3.4. Systematic Review of PPIs
4. Discussion
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Seligman, M.; Csikszentmihalyi, M. Positive psychology: An introduction. Am. Psychol. 2000, 55, 5–14. [Google Scholar] [CrossRef]
- Peterson, C.; Seligman, M.E.P. Character Strengths and Virtues: A Classification and Handbook; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar]
- McGrath, R.E. Scale and item-level factor analyses of the VIA Inventory of Strengths. Assessment 2012, 21, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Park, N.; Peterson, C.; Seligman, M.E.P. Strengths of character and wellbeing. J. Soc. Clin. Psychol. 2004, 23, 603–619. [Google Scholar] [CrossRef]
- Rasmussen, H.N.; Scheier, M.F.; Greenhouse, J.B. Optimism and physical health: A meta-analytic review. Ann. Behav. Med. 2009, 37, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Chida, Y.; Steptoe, A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychsom. Med. 2008, 70, 741–756. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Kubzansky, L.D. The heart's content: the association between positive psychological well-being and cardiovascular health. Psychol. Bull. 2012, 138, 655–691. [Google Scholar] [CrossRef] [PubMed]
- Dubois, C.; Beach, T.; Kashdan, M.; Nyer, E.; Park, C.; Celano, C.; Huffman, J.C. Positive psychology attributes and cardiac outcomes: Associations, mechanisms, and interventions. Psychosomatics 2012, 53, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Richman, L.S.; Kubzansky, L.; Kawachi, I.; Masleko, J. Positive emotion and health: Going beyond the negative. Health Psychol. 2005, 24, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Pressman, S.; Cohen, S. Does positive affect influence health? Psychol. Bull. 2015, 131, 925–971. [Google Scholar] [CrossRef] [PubMed]
- Sin, N.L.; Lyubomirsky, S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. J. Clin. Psychol. 2009, 65, 467–487. [Google Scholar] [CrossRef] [PubMed]
- Seligman, M.E.P.; Steen, T.A.; Park, N.; Peterson, C. Positive psychology progress: Empirical validation of interventions. Am. Psychol. 2005, 60, 410–421. [Google Scholar] [CrossRef] [PubMed]
- Boiler, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Pub. Health 2013, 13, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Seligman, M.E.P.; Rashid, T.; Parks, A.C. Positive psychotherapy. Am. Psychol. 2006, 61, 467–487. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Pisouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and weaknesses. The FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation Database (2015). Available online: http://www.who.int/gho/database/en/ (accessed on 20 August 2016).
- Higgins, J.P.T.; Green, S. The Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Chichester, UK, 2008. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6. [Google Scholar] [CrossRef] [PubMed]
- Casellas-Grau, A.; Font, A.; Vives, J. Positive psychology interventions in breast cancer: A systematic review. Psycho-Oncology 2014, 23, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Rustøen, T.; Bruce, A.; Coope, C.; Miaskowski, A.D. A longitudinal study of the effects of a hope intervention on levels of hope and psychological distress in a community-based sample of oncology patients. Eur. J. Oncol. Nurs. 2011, 15, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.C.; Mastromauro, C.A.; Boehm, J.K.; Seabrook, R.; Fricchione, G.L.; Denninger, J.W.; Lyubormirsky, S.L. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Int. 2011, 6, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.C.; DuBois, C.M.; Millstein, R.A.; Celano, C.M.; Wexler, D. Positive psychological interventions for patients with type 2 diabetes: Rationale, theoretical model, and intervention development. J. Diabetes Res. 2015. [Google Scholar] [CrossRef] [PubMed]
- Cohn, M.A.; Pietrucha, M.E.; Saslow, L.R.; Hult, J.R. An online positive affect skills intervention reduces depression in adults with type 2 diabetes. J. Posit. Psychol. 2014, 9, 523–534. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.E.; Emmons, R.A.; Tsang, J. The grateful disposition: A conceptual and empirical topography. J. Pers. Soc. Psychol. 2002, 82, 112–127. [Google Scholar] [CrossRef]
- Scheier, M.F.; Carver, C.S.; Bridges, M.W. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A re-evaluation of the Life Orientation Test. J. Pers. Soc. Psychol. 1994, 67, 1063–1078. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using self- report assessment methods to explore facets of mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Bergomi, C.; Tschacher, W.; Kupper, Z. The Assessment of Mindfulness with Self-Report Measures: Existing Scales and Open Issues. Mindfulness 2013, 4, 191–202. [Google Scholar] [CrossRef]
- Macaskill, A. A feasibility study of psychological strengths and wellbeing assessment in individuals living with recurrent depression. J. Posit. Psychol. 2012, 7, 372–386. [Google Scholar] [CrossRef]
- Byrne, R. The Secret; Atria Books: New York, NY, USA, 2006. [Google Scholar]
- Holland, J.C.; Lewis, S. The Human Side of Cancer: Living with Hope, Coping with Uncertainty; Harper Collins: New York, NY, USA, 2000. [Google Scholar]
- Seligman, M.E.P. Positive health. Appl. Psychol-Int. Rev. 2008, 57, 3–18. [Google Scholar] [CrossRef]
- Coyne, J.C.; Tennen, H. Positive psychology in cancer care: Bad science, exaggerated claims, and unproven medicine. Ann. Behav. Med. 2010, 39, 16–26. [Google Scholar] [CrossRef] [PubMed]
| References, First Author, Condition | Study Design | Constructs Targeted, Delivery Mode, Duration | Sample | Sampling method | Outcome Measures | Results | Quality Assessment |
|---|---|---|---|---|---|---|---|
| [21] Huffman (2011) Cardiovascular Disease | RCT Pretest -posttest design with a control group and treatment as usual group (relaxation) | Gratitude, (3 good things), letter writing, optimism, (best possible self), kindness. First session (45 min) held in hospital, programme explained and first exercise given. Subsequent exercise delivered weekly via a 15-min telephone call to review previous exercise and set new one. Sessions delivered by social worker over 12 weeks and a written manual provided. | Hospitalised cardiac patients N = 30 3 equal n groups: 1. PPI 2. Relaxation 3. Control undertook an unrelated activity | Self-selecting, randomized to intervention group | Pre-test and post-test scores for happiness *, positive affect *, mental health related quality of life *, anxiety *, depression *. | In PPI group depression, anxiety, happiness, Quality of life showed significantly more improvement from baseline after 8 weeks than in the other two groups. | Medium No direct measure of gratitude, or positive affect. Self-selecting volunteers No longer term follow-up |
| [20] Rustøen (2011) Breast cancer | Single sample with follow up at 3- and 12- months | Hope, Impact of Events (stress) Hope intervention (Hope-in) Programme 8 weekly sessions lasting 2 h delivered by trained nurses to groups of 5–12 patients in health care setting. | N = 195 all diagnosed with breast cancer living at home but requesting professional support via a regional office. | Self-selecting responded to request from health care workers | Pre and post -test scores for hope, Impact of Events scale (stress) | Levels of hope increased Post-intervention and stress levels decreased but these decreases were not maintained at 3- and 12- month follow up. | Medium No control group. No measurement of possible confounding life experience/health variables that may impact on stress levels |
| [22] Huffman (2015) Types 2 diabetes Intervention delivery designed on Huffman (2011) | Single-arm proof of concept study. Pretest -posttest design. | Optimism, gratitude, positive affect. First session (45 min) held in hospital or on phone, programme explained, and first exercise given. Subsequent exercise delivered weekly via a 15 min. telephone call to review previous exercise and set new one. Sessions delivered over 12 weeks and a written manual provided. | N = 15 adults all with diagnosis of diabetes confirmed by a clinician 13 completed | Self-selecting, recruited by researchers at hospital and outpatient diabetic clinics. Had to meet diagnostic criteria and adherence to treatment. | Optimism *, gratitude *, anxiety *, depression *, diabetes distress *, diabetes self-care activities *, health behavior adherence * | Only baseline data reported. Study ongoing. No follow up paper found or response from study team. | Incomplete Good description of intervention but study ongoing. |
| [23] Cohn, (2014) Type 2 diabetes | Pretest -post-test design with randomised control group from the self-selecting volunteer sample. | Positive affect, gratitude, acts of kindness, mindfulness, incorporated into a package. (Developing affective health to improve adherence to diabetes treatment) Delivered online over 5 weeks. Intervention was a weekly exercise on concept and daily exercises. Participants visited the website daily to record emotions and treatment adherence. Received a daily email reminder. New exercise posted each week. Control group only completed online emotion reporting. Paid for participation. | N = 49, all diagnosed with Type 2 diabetes. | Self-selecting, recruited online from a research volunteering site (n = 25) or from a diabetes education centre (n = 28) | Depression, perceived stress, positive & negative affect, diabetes self-efficacy, diabetes distress, diabetes-relevant health behaviours | Post- intervention reductions in depression, No changes in other measures. | Poor as an evaluation of a PPI as no direct measure of gratitude, positive affect, or mindfulness although study aims to develop these strengths. More a feasibility study. |
| Cochrane Criteria | [20] Huffman (2011) Cardiovascular Disease | [16] Rustøen (2011) Breast Cancer | [22] Huffman (2015) Types 2 Diabetes | [23] Cohn, (2014) Type 2 Diabetes |
|---|---|---|---|---|
| 1.Handbook or written guidance on PPI | 1 | 1 | 1 | 1 |
| 2. Randomisation adequate | 1 | 1 | 0 | 1 |
| 3. Comparability of groups | 1 | 0 no control group pre-post design | 0 no control group pre-post design | 0 no control group pre-post design |
| 4. Longer term follow-up | 0 | 1 | 0 | 0 |
| 5. Dropout rate given and acceptable | 1 | 0 | 1 from initial recruitment | 1 |
| 6. Assessed by objective outcomes | yes, but not all relevant for PPI | 1 | 1 in future | yes but not all relevant ones for PPI |
| 7. Intent-to treat analysis applied | 0 | 0 | intended | 0 |
| Total scores | 4 | 4 | Study continuing and only baseline data available. | 3 |
© 2016 by the author; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macaskill, A. Review of Positive Psychology Applications in Clinical Medical Populations. Healthcare 2016, 4, 66. https://doi.org/10.3390/healthcare4030066
Macaskill A. Review of Positive Psychology Applications in Clinical Medical Populations. Healthcare. 2016; 4(3):66. https://doi.org/10.3390/healthcare4030066
Chicago/Turabian StyleMacaskill, Ann. 2016. "Review of Positive Psychology Applications in Clinical Medical Populations" Healthcare 4, no. 3: 66. https://doi.org/10.3390/healthcare4030066
APA StyleMacaskill, A. (2016). Review of Positive Psychology Applications in Clinical Medical Populations. Healthcare, 4(3), 66. https://doi.org/10.3390/healthcare4030066





