Update and Review on the Surgical Management of Primary Cutaneous Melanoma
Abstract
:1. Introduction
2. Brief History, Staging Overview, and Current Guidelines
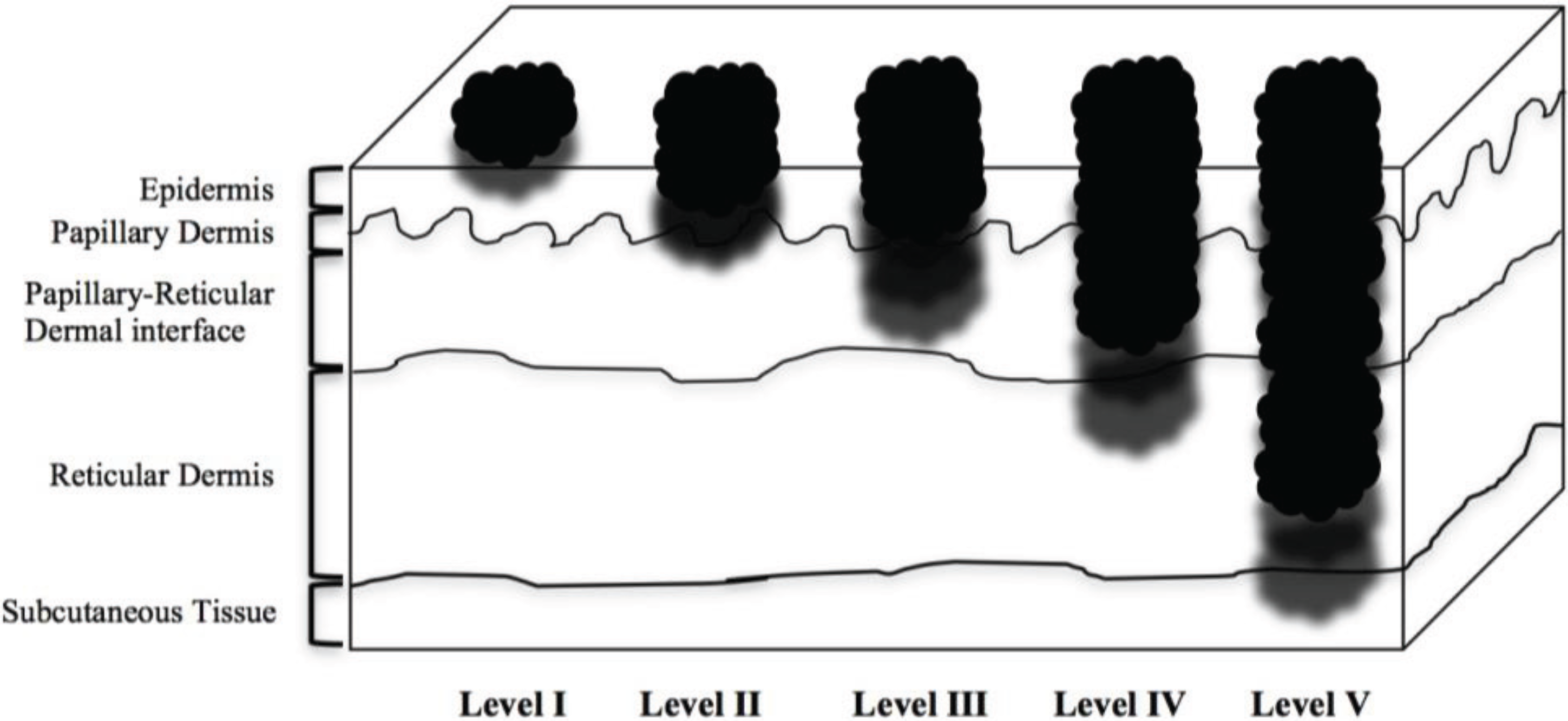
| Level I | Involving only the epidermis, in situ |
| Level II | Invasion of papillary dermis, does NOT reach papillary-reticular dermal interface |
| Level III | Invasion through papillary dermis, does NOT penetrate reticular dermis |
| Level IV | Invasion into reticular dermis |
| Level V | Invasion into subcutaneous tissue |
| Tumor microstage | Thickness | Margin |
|---|---|---|
| Melanoma in situ (Tis) | 0.5 cm | |
| Thin (T1) | ≤1.0 mm | 1.0 cm |
| Intermediate (T2) | 1.01–2 mm | 1.0–2.0 cm |
| Intermediate (T3) | 2.01–4 mm | 2.0 cm |
| Thick (T4) | >4 mm | 2.0 cm |
| TX | Tumor cannot be assessed |
| T0 | No evidence of tumor |
| Tis | Tumor remains on epidermis |
| T1a | Tumor ≤1.0 mm thick, without ulceration and mitosis <1/mm2 |
| T1b | Tumor ≤1.0 mm thick, with ulceration or mitoses ≥1/mm2 |
| T2a | Tumor is between 1.01 and 2.0 mm, without ulceration |
| T2b | Tumor is between 1.01 and 2.0 mm, with ulceration |
| T3a | Tumor is between 2.01 and 4.0 mm, without ulceration |
| T3b | Tumor is between 2.01 and 4.0 mm, with ulceration |
| T4a | Tumor >4.0 mm, without ulceration |
| T4b | Tumor >4.0 mm, with ulceration |
| NX | Lymph nodes cannot be assessed |
| N0 | No spread to lymph nodes |
| N1a | Microscopic spread to 1 lymph node |
| N1b | Macroscopic spread to 1 lymph node |
| N2a | Microscopic spread to 2–3 lymph nodes |
| N2b | Macroscopic spread to 2–3 lymph nodes |
| N2c | In transit met(s)/satellite(s) without metastatic nodes |
| N3 | 4 or more metastatic nodes, or matted nodes, or in transit met(s)/satellite(s) with metastatic node(s) |
| M0 | No metastasis |
| M1a | Metastasis to distant skin, subcutaneous tissue, or distant lymph nodes |
| M1b | Metastasis to lungs |
| M1c | Metastasis to all other visceral sites, or any distant metastasis combined with elevated blood LDH level |
| Stage 0 | Tis, N0, M0 |
| Stage IA | T1a, N0, M0 |
| Stage IB | T1b or T2a, N0, M0 |
| Stage IIA | T2b or T3a, N0, M0 |
| Stage IIB | T3b or T4a, N0, M0 |
| Stage IIC | T4b, N0, M0 |
| Stage IIIA | T1-T4a, N1a or N2a, M0 |
| Stage IIIB | T1-T4b, N1a or N2a, M0 T1-T4a, N1b or N2b, M0 T1-T4a, N2c, M0 |
| Stage IIIC | T1-T4b, N1b or N2b, M0 T1-T4b, N2c, M0 Any T, N3, M0 |
| Stage IV | Any T, any N, any M |
3. Surgical Diagnosis of Melanoma: Types of Biopsy
4. Surgical Margins for Melanoma in-Situ (MIS)
5. Surgical Margins for Thin Melanomas
6. Surgical Margins for Intermediate-Thickness Melanomas
7. Surgical Margins for Thick Melanomas
8. Management of Regional Lymph Nodes: Sentinel Lymph Node Biopsy and Lymphadenectomy
8.1. Introduction
8.2. Utility of Sentinel Lymph Node Biopsy
8.3. Utility of Completion Lymph Node Dissection
8.4. Arguments against Sentinel Lymph Node Biopsy and Completion Lymph Node Dissection
9. Conclusions
Author Contributions
Conflicts of Interest
References
- Lee, C.; Collichio, F.; Ollila, D.; Moschos, S. Historical review of melanoma treatment and outcomes. Clin. Dermatol. 2013, 31, 141–147. [Google Scholar] [CrossRef]
- Handley, W.S. The pathology of melanotic growths in relation to their operative treatment. Lancet 1907, 1, 927–996. [Google Scholar]
- Kaufmann, R. Surgical management of primary melanoma. Clin. Exp. Dermatol. 2000, 25, 476–481. [Google Scholar]
- AJCC Cancer Staging Manual, 7th ed.; Edge, S.B.; Byrd, D.R.; Compton, C.C.; Fritz, A.G.; Greene, F.L.; Trotti, A. (Eds.) Springer: New York, NY, USA, 2010.
- Levine, S.; Shapiro, R. Surgical treatment of malignant melanoma practical guidelines. Dermatol. Clin. 2012, 30, 487–501. [Google Scholar] [CrossRef]
- Balch, C.M.; Soong, S.; Ross, M.I.; Urist, M.M.; Karakousis, C.P.; Temple, W.J.; Mihm, M.C.; Barnhill, R.L.; Jewell, W.R.; Wanebo, H.J.; et al. Long-term results of a multi-institutional randomized trial comparing prognostic factors and surgical results for intermediate thickness melanomas (1.0 to 4.0 mm). Intergroup Melanoma Surgical Trial. Ann. Surg. Oncol. 2000, 7, 87–97. [Google Scholar] [CrossRef]
- Veronesi, U.; Cascinelli, N.; Adamus, J.; Balch, C.; Bandiera, D.; Barchuk, A.; Bufalino, R.; Craig, P.; de Marsillac, J.; Durand, J.C.; et al. Thin stage I primary cutaneous malignant melanoma. Comparison of excision with margins of 1 or 3 cm. N. Engl. J. Med. 1988, 318, 1159–1162. [Google Scholar] [CrossRef]
- Coit, D.G.; Andtbacka, R.A.; Anker, C.J.; Bichakjian, C.K.; Carson, W.E., III; Daud, A.; Dilawari, R.A.; DiMaio, D.; Guild, V.; Halpern, A.C.; et al. Melanoma: Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2012, 10, 366–400. [Google Scholar]
- Balch, C.M.; Gershenwald, J.E.; Soong, S.; Thompson, J.F.; Atkins, M.B.; Byrd, D.R.; Buzaid, A.C.; Cochran, A.J.; Coit, D.G.; Ding, S.; et al. Final version of 2009 AJCC melanoma staging and classification. J. Clin. Oncol. 2009, 27, 6199–6206. [Google Scholar] [CrossRef]
- Ho, V.C.; Milton, G.W.; Sober, A.J. Biopsy of melanoma. In Cutaneous Melanoma, 2nd ed.; Balch, C., Ed.; JB Lippincott: Philadelphia, PA, USA, 1992; pp. 264–268. [Google Scholar]
- Australian Cancer Network Melanoma Guidelines Revision Working Party. Biopsy. In Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand; Sydney and New Zealand Guidelines Group, The Cancer Council Australia, Australian Cancer Network: Wellington, New Zealand, 2008; pp. 35–39. [Google Scholar]
- Coit, D.G.; Thompson, J.A.; Andtbacka, R.; Anker, C.J.; Bichakjian, C.K.; Carson, W.E., III; Daniels, G.A.; Daud, A.; DiMaio, D.; Fleming, M.D.; et al. Melanoma, Version 2.2014. Available online: http://www.nccn.org/ (accessed on 17 April 2014).
- Erickson, C.; Miller, S.J. Treatment options in melanoma in situ: Topical and radiation therapy, excision and Mohs surgery. Int. J. Derm. 2010, 49, 482–491. [Google Scholar] [CrossRef]
- Chin-Lenn, L.; Murynka, T.; McKinnon, J.G.; Arlette, J.P. Comparison of outcomes for malignant melanoma of the face treated using mohs micrographic surgery and wide local excision. Dermatol. Surg. 2013, 39, 1637–1645. [Google Scholar] [CrossRef]
- Whalen, J.; Leone, D. Mohs micrographic surgery for the treatment of malignant melanoma. Clin. Derm. 2009, 27, 597–602. [Google Scholar]
- Zitelli, J.A.; Brown, C.; Hanusa, B.H. Mohs Micrographic surgery for the treatment of primary cutaneous melanoma. J. Am. Acad. Dermatol. 1997, 37, 236–245. [Google Scholar] [CrossRef]
- Hui, A.M.; Jacobson, M.; Markowitz, O.; Brooks, N.A.; Siegel, D.M. Mohs micrographic surgery for the treatment of melanoma. Dermatol. Clin. 2012, 30, 503–515. [Google Scholar]
- Kunishige, J.; Brodland, D.; Zitelli, J. Surgical margins for melanoma in situ. J. Am. Acad. Dermatol. 2012, 66, 438–444. [Google Scholar] [CrossRef]
- National Institutes of Health. Diagnosis and Treatment of Early Melanoma. National Institutes of Health Consensus Development Conference Statement, January 27–29, 1992. NIH Consens. Statement 1992, 10, 1–26. [Google Scholar]
- Thomas, J.M.; Newton-Bishop, J.; A’Hern, R.; Coombes, G.; Timmons, M.; Evans, J.; Cook, M.; Theaker, J.; Fallowfield, M.; O’Neill, T.; et al. Excision margins in high-risk malignant melanoma. N. Engl. J. Med. 2004, 350, 757–766. [Google Scholar] [CrossRef]
- Gillgren, P.; Drzewiecki, K.T.; Niin, M.; Gullestad, H.P.; Hellborg, H.; Mansson-Brahme, E.; Ingvar, C.; Ringborg, U. 2-cm versus 4-cm surgical excision margins for primary cutaneous melanoma thicker than 2 mm: A randomized, multicenter trial. Lancet 2011, 378, 1635–1641. [Google Scholar] [CrossRef]
- Heaton, K.M.; Sussman, J.J.; Gershenwald, J.E.; Lee, J.E.; Reintgen, D.S.; Mansfield, P.F.; Ross, M.I. Surgical margins and prognostic factors in patients with thick (>4 mm) primary melanoma. Ann. Surg. Oncol. 1998, 5, 322–328. [Google Scholar] [CrossRef]
- Pasquali, S.; Haydu, L.E.; Scolyer, R.A.; Winstanley, J.B.; Spillane, A.J.; Quinn, M.J.; Saw, R.P.; Shannon, K.F.; Stretch, J.R.; Thompson, J.F. The importance of adequate primary tumor excision margins and sentinel node biopsy in achieving optimal locoregional control for patients with thick primary melanomas. Ann. Surg. 2013, 258, 152–157. [Google Scholar] [CrossRef]
- Phan, G.Q.; Messina, J.L.; Sondak, V.K.; Zager, J.S. Sentinel lymph node biopsy for melanoma: Indications and rationale. Cancer Control. 2009, 16, 234–239. [Google Scholar]
- Cochran, A.J.; Essner, R.; Rose, D.M.; Glass, E.C. Principles of sentinel lymph node identification: Background and clinical implications. Langenbecks Arch. Surg. 2000, 385, 252–260. [Google Scholar]
- Wong, S.L.; Balch, C.M.; Hurley, P.; Agarwala, S.S.; Akhurst, T.J.; Cochran, A.; Cormier, J.N.; Gorman, M.; Kim, T.Y.; McMasters, K.M.; et al. Sentinel lymph node biopsy for melanoma: American Society of Clinical Oncology and Society of Surgical Oncology joint clinical practice guidelines. J. Clin. Oncol. 2012, 30, 2912–2918. [Google Scholar] [CrossRef]
- Wong, S.L.; Balch, C.M.; Hurley, P.; Agarwala, S.S.; Akhurst, T.J.; Cochran, A.; Cormier, J.N.; Gorman, M.; Kim, T.Y.; McMasters, K.M.; et al. Sentinel lymph node biopsy for melanoma: American Society of Clinical Oncology and Society of Surgical Oncology joint clinical practice guidelines. Ann. Surg. Oncol. 2012, 19, 3313–3324. [Google Scholar] [CrossRef]
- Morton, D.L. Overview and update of the phase III Multicenter Selective Lymphadenectomy Trials (MSLT-I and MSLT-II) in melanoma. Clin. Exp. Metastasis 2012, 29, 699–706. [Google Scholar] [CrossRef]
- Hardin, R.E.; Lange, J.R. Surgical treatment of melanoma patients with early sentinel node involvement. Curr. Treat. Options Oncol. 2012, 13, 318–326. [Google Scholar] [CrossRef]
- Rutkowski, P.; Nowecki, Z.I.; Zurawski, Z.; Dziewirski, W.; Nasierowska-Guttmejer, A.; Switaj, T.; Ruka, W. In transit/local recurrences in melanoma patients after sentinel node biopsy and therapeutic lymph node dissection. Eur. J. Cancer. 2006, 42, 159–164. [Google Scholar] [CrossRef]
- Landi, G.; Polverelli, M.; Moscatelli, G.; Morelli, R.; Landi, C.; Fiscelli, O.; Erbazzi, A. Sentinel lymph node biopsy in patients with primary cutaneous melanoma: Study of 455 cases. J. Eur. Acad. Dermatol. Venereol. 2000, 14, 35–45. [Google Scholar]
- Mays, M.P.; Martin, R.C.; Burton, A.; Ginter, B.; Edwards, M.J.; Reintgen, D.S.; Ross, M.I.; Urist, M.M.; Stromberg, A.J.; McMasters, K.M.; et al. Should all patients with melanoma between 1 and 2 mm Breslow thickness undergo sentinel lymph node biopsy? Cancer 2010, 116, 1535–1544. [Google Scholar] [CrossRef]
- Gershenwald, J.E.; Thompson, W.; Mansfield, P.F.; Lee, J.E.; Colome, M.I.; Tseng, C.H.; Lee, J.J.; Balch, C.M.; Reintgen, D.S.; Ross, M.I. Multi-institutional melanoma lymphatic mapping experience: The prognostic value of sentinel lymph node status in 612 stage I or II melanoma patients. J. Clin. Oncol. 1999, 17, 976–983. [Google Scholar]
- Coit, D.G.; Olszanski, A.J. Progress in the management of melanoma in 2013. J. Natl. Compr. Cancer Netw. 2013, 11, 645–648. [Google Scholar]
- Mozzillo, N.; Pennacchioli, E.; Gandini, S.; Caraco, C.; Crispo, A.; Botti, G.; Lastoria, S.; Barberis, M.; Verrecchia, F.; Testori, A. Sentinel node biopsy in thin and thick melanoma. Ann. Surg. Oncol. 2013, 20, 2780–2786. [Google Scholar] [CrossRef]
- Karakousis, G.C.; Gimotty, P.A.; Botbyl, J.D.; Kesmodel, S.B.; Elder, D.E.; Elenitsas, R.; Ming, M.E.; Guerry, D.; Fraker, D.L.; Czerniecki, B.J.; et al. Predictors of regional nodal disease in patients with thin melanomas. Ann. Surg. Oncol. 2006, 13, 533–541. [Google Scholar] [CrossRef]
- Kalady, M.F.; White, R.R.; Johnson, J.L.; Tyler, D.S.; Seigler, H.F. Thin melanomas: Predictive lethal characteristics from a 30-year clinical experience. Ann. Surg. 2003, 238, 528–535. [Google Scholar]
- Kesmodel, S.B.; Karakousis, G.C.; Botbyl, J.D.; Canter, R.J.; Lewis, R.T.; Wahl, P.M.; Terhune, K.P.; Alavi, A.; Elder, D.E.; Ming, M.E.; et al. Mitotic rate as a predictor of sentinel lymph node positivity in patients with thin melanomas. Ann. Surg. Oncol. 2005, 12, 449–458. [Google Scholar] [CrossRef]
- Ranieri, J.M.; Wagner, J.D.; Wenck, S.; Johnson, C.S.; Coleman, J.J., 3rd. The prognostic importance of sentinel lymph node biopsy in thin melanoma. Ann. Surg. Oncol. 2006, 13, 927–932. [Google Scholar] [CrossRef]
- Morton, D.L.; Thompson, J.F.; Essner, R.; Elashoff, R.; Stern, S.L.; Nieweg, O.E.; Roses, D.F.; Karakousis, C.P.; Mozzillo, N.; Reintgen, D.; et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: A multicenter trial. Multicenter Selective Lymphadenectomy Trial Group. Ann. Surg. 1999, 230, 453–463. [Google Scholar]
- Reintgen, D.; Cruse, C.W.; Wells, K.; Berman, C.; Fenske, N.; Glass, F.; Schroer, K.; Heller, R.; Ross, M.; Lyman, G.; et al. The orderly progression of melanoma nodal metastases. Ann. Surg. 1994, 220, 759–767. [Google Scholar] [CrossRef]
- Morton, D.L.; Wen, D.R.; Wong, J.H.; Economou, J.S.; Cagle, L.A.; Storm, F.K.; Foshag, L.J.; Cochran, A.J. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch. Surg. 1992, 127, 392–399. [Google Scholar] [CrossRef]
- Thompson, J.F.; McCarthy, W.H.; Bosch, C.M.; O’Brien, C.J.; Quinn, M.J.; Paramaesvaran, S.; Crotty, K.; McCarthy, S.W.; Uren, R.F.; Howman-Giles, R. Sentinel lymph node status as an indicator of the presence of metastatic melanoma in regional lymph nodes. Melanoma Res. 1995, 5, 255–260. [Google Scholar] [CrossRef]
- De Rosa, N.; Lyman, G.H.; Silbermins, D.; Valsecchi, M.E.; Pruitt, S.K.; Tyler, D.M.; Lee, W.T. Sentinel node biopsy for head and neck melanoma: A systematic review. Otolaryngol. Head Neck Surg. 2011, 145, 375–382. [Google Scholar] [CrossRef]
- Coit, D.G.; Andtbacka, R.; Anker, C.; Bichakjian, C.K.; Carson, W.E., III; Daud, A.; DiMaio, D.; Fleming, M.D.; Guild, V.; Halpern, A.C.; et al. Melanoma, version 2.2013, featured updates to the NCCN guidelines. J. Natl. Compr. Cancer Netw. 2013, 11, 395–407. [Google Scholar]
- Lens, M.B.; Dawes, M.; Newton-Bishop, J.A.; Goodacre, T. Tumor thickness as a predictor of occult lymph node metastases in patients with stage I and II melanoma undergoing sentinel lymph node biopsy. Br. J. Surg. 2002, 89, 1223–1227. [Google Scholar] [CrossRef]
- Cherpelis, B.S.; Haddad, F.; Messina, J.; Cantor, A.B.; Fitzmorris, K.; Reintgen, D.S.; Fenske, N.A.; Glass, L.F. Sentinel lymph node micrometastasis and other histologic factors that predict outcome in patients with thicker melanomas. J. Am. Acad. Dermatol. 2001, 44, 762–766. [Google Scholar] [CrossRef]
- Oliveira Filho, R.S.; Silva, A.M.; Oliveira, D.A.; Oliveira, G.G.; Nahas, F.X. Sentinel node biopsy should not be recommended for patients with thick melanoma. Rev. Col. Bras. Cir. 2013, 40, 127–129. [Google Scholar] [CrossRef]
- Nowecki, Z.I.; Rutkowski, P.; Michej, W. The survival benefit to patients with positive sentinel node melanoma after completion lymph node dissection may be limited to the subgroup with a primary lesion Breslow thickness greater than 1.0 and less than or equal to 4 mm (pT2-pT3). Ann. Surg. Oncol. 2008, 15, 2223–2234. [Google Scholar] [CrossRef]
- Gershenwald, J.E.; Mansfield, P.F.; Lee, J.E.; Ross, M.I. Role for lymphatic mapping and sentinel lymph node biopsy in patients with thick (> or = 4 mm) primary melanoma. Ann. Surg. Oncol. 2000, 7, 160–165. [Google Scholar] [CrossRef]
- Satzger, I.; Volker, B.; Meier, A.; Kapp, A.; Gutzmer, R. Criteria in sentinel lymph nodes of melanoma patients that predict involvement of nonsentinel lymph nodes. Ann. Surg. Oncol. 2008, 15, 1723–1732. [Google Scholar]
- Roka, F.; Mastan, P.; Binder, M.; Okamoto, I.; Mittlboeck, M.; Horvat, R.; Pehamberger, H.; Diem, E. Prediction of non-sentinel node status and outcome in sentinel node-positive melanoma patients. Eur. J. Surg. Oncol. 2008, 34, 82–88. [Google Scholar]
- Cochran, A.J.; Wen, D.R.; Huang, R.R.; Wang, H.J.; Elashoff, R.; Morton, D.L. Prediction of metastatic melanoma in nonsentinel nodes and clinical outcome based on the primary melanoma and the sentinel node. Mod. Pathol. 2004, 17, 747–755. [Google Scholar] [CrossRef]
- Scolyer, R.A.; Li, L.X.; McCarthy, S.W.; Shaw, H.M.; Stretch, J.R.; Sharma, R.; Thompson, J.F. Immunohistochemical stains fail to increase the detection rate of micrometastatic melanoma in completion regional lymph node dissection specimens. Melanoma Res. 2004, 14, 263–268. [Google Scholar] [CrossRef]
- Gershenwald, J.E.; Andtbacka, R.H.; Prieto, V.G.; Johnson, M.M.; Diwan, A.H.; Lee, J.E.; Mansfield, P.F.; Cormier, J.N.; Schacherer, C.W.; Ross, M.I. Microscopic tumor burden in sentinel lymph nodes predicts synchronous nonsentinel lymph node involvement in patients with melanoma. J. Clin. Oncol. 2008, 26, 4296–303. [Google Scholar] [CrossRef]
- Kretschmer, L.; Hilgers, R.; Mohrle, M.; Balda, B.R.; Breuninger, H.; Konz, B.; Kunte, C.; Marsch, W.C.; Neumann, C.; Starz, H. Patients with lymphatic metastasis of cutaneous malignant melanoma benefit from sentinel lymphonodectomy and early excision of their nodal disease. Eur. J. Cancer 2004, 40, 212–218. [Google Scholar] [CrossRef]
- Morton, D.L.; Hoon, D.S.; Cochran, A.J.; Turner, R.R.; Essner, R.; Takeuchi, H.; Wanek, L.A.; Glass, E.; Foshag, L.J.; Hsueh, E.C.; et al. Lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: Therapeutic utility and implications of nodal microanatomy and molecular staging for improving the accuracy of detection of nodal micrometastases. Ann. Surg. 2003, 238, 538–549. [Google Scholar]
- Pasquali, S.; Mocellin, S.; Campana, L.G.; Bonandini, E.; Montesco, M.C.; Tregnaghi, A.; del Fiore, P.; Nitti, D.; Rossi, C.R. Early (sentinel lymph node biopsy-guided) versus delayed lymphadenectomy in melanoma patients with lymph node metastases: Personal experience and literature meta-analysis. Cancer 2010, 116, 1201–1209. [Google Scholar] [CrossRef]
- Rutkowski, P.; Nowecki, Z.I.; Nasierowska-Guttmejer, A.; Ruka, W. Lymph node status and survival in cutaneous malignant melanoma—Sentinel lymph node biopsy impact. Eur. J. Surg. Oncol. 2003, 29, 611–618. [Google Scholar] [CrossRef]
- Morton, D.L.; Thompson, J.F.; Cochran, A.J.; Mozzillo, N.; Nieweg, O.E.; Roses, D.F.; Hoekstra, H.J.; Karakousis, C.P.; Puleo, C.A.; Coventry, B.J.; et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N. Engl. J. Med. 2014, 370, 599–609. [Google Scholar] [CrossRef]
- Pilko, G.; Besic, N.; Zgajnar, J.; Hocevar, M. Prognostic heterogeneity after the excision of lymph node metastases in patients with cutaneous melanoma. Surg. Oncol. 2011, 20, 26–34. [Google Scholar] [CrossRef]
- Twomey, P. Sentinel node biopsy for early-stage melanoma: Accuracy and morbidity in MSLT-1, an international multicenter trial. Ann. Surg. 2007, 245, 156–157. [Google Scholar] [CrossRef]
- McMasters, K.M.; Noyes, R.D.; Reintgen, D.S.; Goydos, J.S.; Beitsch, P.D.; Davidson, B.S.; Sussman, J.J.; Gershenwald, J.E.; Ross, M.I. Lessons learned from the Sunbelt melanoma trial. J. Surg. Oncol. 2004, 86, 212–223. [Google Scholar] [CrossRef]
- Torjesen, I. Sentinel node biopsy for melanoma: Unnecessary treatment? Br. Med. J. 2013, 346, E8645. [Google Scholar] [CrossRef]
- Printz, C. Physicians differ on the use of Sentinel lymph node biopsy for melanoma: Published data receive various interpretations. Cancer 2013, 119, 2515–2516. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Leilabadi, S.N.; Chen, A.; Tsai, S.; Soundararajan, V.; Silberman, H.; Wong, A.K. Update and Review on the Surgical Management of Primary Cutaneous Melanoma. Healthcare 2014, 2, 234-249. https://doi.org/10.3390/healthcare2020234
Leilabadi SN, Chen A, Tsai S, Soundararajan V, Silberman H, Wong AK. Update and Review on the Surgical Management of Primary Cutaneous Melanoma. Healthcare. 2014; 2(2):234-249. https://doi.org/10.3390/healthcare2020234
Chicago/Turabian StyleLeilabadi, Solmaz Niknam, Amie Chen, Stacy Tsai, Vinaya Soundararajan, Howard Silberman, and Alex K. Wong. 2014. "Update and Review on the Surgical Management of Primary Cutaneous Melanoma" Healthcare 2, no. 2: 234-249. https://doi.org/10.3390/healthcare2020234





