Abstract
Lyme disease is a most common vector-borne disease in the US. Although the majority of Lyme patients can be cured with the standard two- to four-week antibiotic treatment, at least 10%–20% of patients continue to suffer from prolonged post-treatment Lyme disease syndrome (PTLDS). While the cause for this is unclear, one possibility is that persisting organisms are not killed by current Lyme antibiotics. In our previous studies, we screened an FDA drug library and an NCI compound library on B. burgdorferi and found some drug hits including sulfa drugs as having good activity against B. burgdorferi stationary phase cells. In this study, we evaluated the relative activity of three commonly used sulfa drugs, sulfamethoxazole (Smx), dapsone (Dps), sulfachlorpyridazine (Scp), and also trimethoprim (Tmp), and assessed their combinations with the commonly prescribed Lyme antibiotics for activities against B. burgdorferi stationary phase cells. Using the same molarity concentration, dapsone, sulfachlorpyridazine and trimethoprim showed very similar activity against stationary phase B. burgdorferi enriched in persisters; however, sulfamethoxazole was the least active drug among the three sulfa drugs tested. Interestingly, contrary to other bacterial systems, Tmp did not show synergy in drug combinations with the three sulfa drugs at their clinically relevant serum concentrations against B. burgdorferi. We found that sulfa drugs combined with other antibiotics were more active than their respective single drugs and that four-drug combinations were more active than three-drug combinations. Four-drug combinations dapsone + minocycline + cefuroxime + azithromycin and dapsone + minocycline + cefuroxime + rifampin showed the best activity against stationary phase B. burgdorferi in these sulfa drug combinations. However, these four-sulfa-drug–containing combinations still had considerably less activity against B. burgdorferi stationary phase cells than the Daptomycin + cefuroxime + doxycycline used as a positive control which completely eradicated B. burgdorferi stationary phase cells. Future studies are needed to evaluate and optimize the sulfa drug combinations in vitro and also in animal models.
1. Introduction
Lyme disease, which is caused by Borrelia burgdorferi sensu lato complex species, is the most common vector-borne disease in the United States with an estimated 300,000 cases a year [1]. The infection is transmitted to humans by tick vectors that feed upon rodents, reptiles, birds, deer, etc. [2]. In the early stage of Lyme disease, patients often have a localized erythema migrans rash that expands as the bacteria disseminate from the cutaneous infection site via the blood stream to other parts of the body. Late-stage Lyme disease is a multi-system disorder which can cause arthritis and neurologic manifestations [1]. While the majority of Lyme disease patients can be cured if treated promptly with the standard two- four-week doxycycline, amoxicillin, or cefuroxime therapy [3], at least 10%–20% of Lyme patients have lingering symptoms such as fatigue, muscular and joint pain, and neurologic impairment even six months after the antibiotic treatment—a set of symptoms called post-treatment Lyme disease syndrome (PTLDS) [4]. While the cause of PTLDS is unknown, several possibilities are likely to be involved, including autoimmune response [5], immune response to continued presence of antigenic debris [6], tissue damage as a result of Borrelia infection and inflammation, co-infections [7], as well as persistent infection due to B. burgdorferi persisters that are not killed by the current antibiotics used to treat Lyme disease [8,9,10]. Various studies have found evidence of B. burgdorferi persistence in dogs [11], mice [8,9], monkeys [10], as well as humans [12] after antibiotic treatment; however, viable organisms are very difficult to culture from the host after antibiotic treatment.
B. burgdorferi develops various forms of dormant persisters in stationary phase cultures which are tolerant to the antibiotics used to treat Lyme disease [13,14,15,16]. These persister bacteria have an altered gene expression profile, which may underlie their drug-tolerant phenotype [17]. In log phase cultures (three to five days old), B. burgdorferi is primarily in motile spirochetal form which is highly susceptible to current Lyme antibiotics doxycycline and amoxicillin; however, in stationary phase cultures (seven to 15 days old), increased numbers of atypical forms such as round bodies and aggregated biofilm-like microcolonies develop [13,14]. These atypical forms have been shown to have increased tolerance to doxycycline and amoxicillin when compared to the growing spirochetal forms [13,14,15,16]. In addition, that the active hits from the round body persister screens [18] overlap with those from the screens on stationary phase cells [13] indicates the stationary phase culture or cells can be used as a relevant persister model. Therefore, stationary phase cultures (seven to 15 days old) enriched in persisters have been used as a model for high-throughput drug screens against persisters [13,14,19].
We have recently identified a range of drugs with high activity against stationary phase cells enriched in persisters through screens of the FDA-approved drug library and NCI compound libraries [13,19]. Besides daptomycin, clofazimine and cephalosporin antibiotics, we also found sulfa drugs as having good activity against B. burgdorferi stationary phase cells as well as round body forms [19]. In addition, a recent study found that the sulfa drug dapsone had clinical benefit in the treatment of Lyme disease patients with persistent symptoms [20]. However, the relative activity of different sulfa drugs against B. burgdorferi stationary phase cells has not been evaluated in the same study under the same conditions. In this study, we compared the relative activity of three commonly used sulfa drugs, sulfamethoxazole (Smx), dapsone (Dps), sulfachlorpyridazine (Scp), and trimethoprim (Tmp) (a drug that also inhibits the folate pathway but is not considered a sulfa drug), and assessed their combinations with the commonly prescribed Lyme antibiotics and other antibiotics with activities against B. burgdorferi stationary phase cells as a persister model.
2. Results and Discussion
2.1. Comparison of the Relative Anti-Persister Activity of Commonly Used Sulfa Drugs Sulfamethoxazole, Dapsone, Sulfachlorpyridazine, and Trimethoprim for Their Activity against Stationary Phase B. burgdorferi Culture
To compare the activity of sulfamethoxazole, dapsone, sulfachlorpyridazine, and trimethoprim against B. burgdorferi stationary phase cells, we tested them on the same seven-day-old B. burgdorferi stationary phase culture with the same molarity concentrations (10, 20, and 40 µM), using doxycycline and persister drug daptomycin as controls. Compared to the drug-free control (residual viability 91%), the three sulfa drugs and trimethoprim (residual viability 88%–92%, Figure 1) showed little or no activity against stationary phase B. burgdorferi cultures at the low concentration (10 µM). Meanwhile, the doxycycline control also showed no activity (residual viability 91%, Figure 1) against the stationary phase B. burgdorferi. At the 10 µM concentration, we only found persister drug daptomycin showed good activity (residual viability 48%, Figure 1) against the stationary phase B. burgdorferi culture. To confirm results of the plate reader SYBR Green I/PI assay, we performed a microscope counting SYBR Green I/PI assay on the antibiotic-treated samples. The microscope counting results were in agreement with the plate reader results (Figure 1).
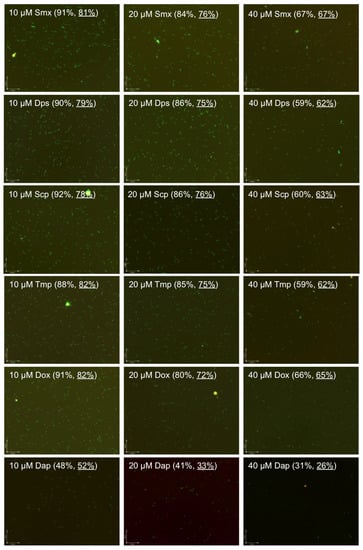
Figure 1.
Comparison of anti-persister activity of sulfamethoxazole, dapsone, sulfachlorpyridazine and trimethoprim with doxycycline and daptomycin as controls. A seven-day-old B. burgdorferi stationary phase culture containing aggregated microcolonies was incubated for seven days with sulfamethoxazole (Smx), dapsone (Dps), sulfachlorpyridazine (Scp), trimethoprim (Tmp), doxycycline (Dox) and daptomycin (Dap) at the same drug concentrations of 10, 20 or 40 µM, respectively, followed by viability assessment using the SYBR Green I/PI assay. Representative images were taken using epifluorescence microscopy at 100× magnification. The calculated percentage and direct counting percentage (underlined) of residual viable cells are shown in brackets. The green cells stained by SYBR Green I dye indicate live cells while the red cells stained by PI dye indicate dead cells.
At the higher concentration (20 µM), the three sulfa drugs and trimethoprim had some activity (residual viability 86%–84%, Figure 1) against the B. burgdorferi stationary phase culture. We did not observe a statistically significant difference in the activity of these four drugs. The three sulfa drugs and trimethoprim (residual viability 86%–84%) showed slightly less activity than doxycycline (residual viability 80%) but considerably less activity than daptomycin (residual viability 41%) at the 20 µM concentration (Figure 1).
We found a dose-dependent increase in the killing activity of the three sulfa drugs and trimethoprim against the stationary phase B. burgdorferi, resulting in 59%–67% residual viability (Figure 1) at the highest concentration (40 µM). Dapsone, sulfachlorpyridazine and trimethoprim showed very similar activity against stationary phase B. burgdorferi with the 59%, 60% and 59% residual viability, respectively, at 40 µM; however, sulfamethoxazole was the less active drug among the three sulfa drug and trimethoprim as shown by 67% residual viability after the drug treatment for seven days (Figure 1). Meanwhile, we observed that dapsone, sulfachlorpyridazine and trimethoprim showed better activity than the doxycycline control (residual viability 66%) at the high concentration (40 µM). However, the three sulfa drugs and trimethoprim still could not eradicate stationary phase B. burgdorferi even at 40 µM. After the seven-day drug treatment of sulfamethoxazole, dapsone, sulfachlorpyridazine and trimethoprim, we could still find many green (live) B. burgdorferi cells in aggregated microcolony form, round body form and spirochetal form under the microscope revealed by the SYBR Green I/PI viability assay (Figure 1). As shown in our previous studies [13,14,18], daptomycin showed impressive activity (residual viability 31%) against stationary phase B. burgdorferi at 40 µM, as shown by mostly red (dead) cells and red microcolonies (Figure 1). Although dapsone, sulfachlorpyridazine, and trimethoprim showed better activity than doxycycline at 40 µM, their activity is relatively weak compared to daptomycin. We also noticed that sulfamethoxazole showed the weakest activity (residual viability 67%) among the sulfa drugs evaluated and is close to the activity of doxycycline (residual viability 66%) at the high concentration (40 µM).
2.2. Comparison of the Relative Anti-Persister Activity of Sulfamethoxazole, Dapsone, Sulfachlorpyridazine, and Trimethoprim in Drug Combinations at Respective Serum Drug Concentrations
Comparison with the same molar concentration of sulfamethoxazole, dapsone, sulfachlorpyridazine, and trimethoprim could reflect the relative activity of these drugs, while testing the activity of these drugs and their drug combination at their respective serum concentration would provide clinically relevant information. To evaluate effective drug combinations that kill B. burgdorferi stationary phase culture at their serum concentrations, we tested sulfamethoxazole (15 µg/mL), dapsone (3 µg/mL), sulfachlorpyridazine (3 µg/mL), and trimethoprim (3 µg/mL) alone and their combinations with doxycycline (4 µg/mL), cefuroxime (5 µg/mL) and ciprofloxacin (3 µg/mL) on a seven-day-old B. burgdorferi stationary phase culture. Using these clinically relevant concentrations, except sulfamethoxazole (residual viability 84%), sulfachlorpyridazine (residual viability 84%) and sulfamethoxazole + trimethoprim (residual viability 86%), all the other drugs or drug combinations showed some killing activity compared to the drug-free control (residual viability 95%) (p < 0.01, Table 1). Sulfamethoxazole (residual viability 84%), dapsone (residual viability 83%), sulfachlorpyridazine (residual viability 84%), and trimethoprim (residual viability 84%) showed some killing activity compared to the drug-free control (residual viability 95%) (Table 1), but the differences between their activities were statistically insignificant (p > 0.05).

Table 1.
Relative activity of drugs at blood drug combinations on a seven-day-old B. burgdorferi stationary phase culture a.
Interestingly, trimethoprim (residual viability 84%) did not show synergy in the drug combinations with sulfamethoxazole (combination residual viability 86%), dapsone (combination residual viability 85%) and sulfachlorpyridazine (combination residual viability 86%). The results showed that the three sulfa drugs and trimethoprim combined with doxycycline (residual viability 85%), cefuroxime (residual viability 83%) and ciprofloxacin (residual viability 82%) were indeed more active (combination residual viability 74%–78%) than the single drugs (Table 1). However, we did not find significant differences in the activity among these drug combinations. As shown in our previous studies [14,18], cefuroxime combined with doxycycline showed better activity (residual viability 78%) than either one alone (Table 1). However, cefuroxime/doxycycline and cefuroxime/ciprofloxacin combined with sulfamethoxazole, dapsone, sulfachlorpyridazine or trimethoprim did not show higher activity (residual viability 74%–77%).
Our genomic analysis did not identify dihydropteroate synthase and dihydrofolate reductase in B. burgdorferi B31, which respectively are the known targets of sulfa drugs and trimethoprim in other bacteria. Therefore, sulfa drugs and trimethoprim may work on B. burgdorferi B31 through some different and unknown pathways. This may explain why the sulfa drugs and trimethoprim combination did not show a synergistic effect against B. burgdorferi as would be expected with other bacteria, but instead showed more activity when combined with doxycycline, cefuroxime and ciprofloxacin (Table 1).
2.3. Effect of Dapsone Drug Combinations with Clinically Used Drugs on Stationary Phase B. burgdorferi Culture
Dapsone improved chronic Lyme disease/PTLDS patients’ clinical symptoms in a recent study [20]. To identify more effective dapsone drug combinations that kill B. burgdorferi stationary phase cells, we tested some dapsone drug combinations with clinically used antibiotics (cefuroxime, azithromycin, rifampin and minocycline). The plate reader results were also confirmed with the microscope counting after SYBR Green I/PI viability staining (Figure 2). The results showed that some drug combinations (Figure 2h–n) were indeed much more effective than single drugs (Figure 2c–g). Dapsone (residual viability 84%, Figure 2d) showed slightly better activity against the seven-day-old stationary phase culture (residual viability 93%, Figure 2a) than the other three clinically used antibiotics azithromycin (residual viability 88%, Figure 2e), rifampin (residual viability 87%, Figure 2f) and minocycline (residual viability 86%, Figure 2g). Both two-drug combinations dapsone/minocycline and dapsone/rifampin showed better activity, with 78% and 81% residual viable (green) cells (Figure 2h,k) remaining, respectively, in comparison to the single drugs (residual viability 84%–87%, Figure 2d,f,g). Interestingly, when cefuroxime was added to the drug combination dapsone/rifampin, the anti-persister activity of these compounds was markedly increased as shown by the 65% residual viable cells remaining (Figure 2l), compared to the dapsone/rifampin combination (residual viability 81%, Figure 2k). We also noted that rifampin/dapsone/minocycline showed better cooperative activity (residual viability 66%, Figure 2m) than the azithromycin/dapsone/minocycline combination (residual viability 72%, Figure 2i), indicating rifampin is more important than azithromycin in combination with dapsone and minocycline. Not surprisingly, the four-drug combinations were more active (residual viability 58% and 60%, Figure 2j,n) than the three-drug combinations (residual viability 65%–72%, Figure 2i,l,m). However, in contrast to the three-drug combination, azithromycin combined with dapsone/minocycline/cefuroxime was slightly more active (residual viability 58%, Figure 2j) than the rifampin four-drug combination (rifampin/dapsone/minocycline/cefuroxime, residual viability 60%, Figure 2n).
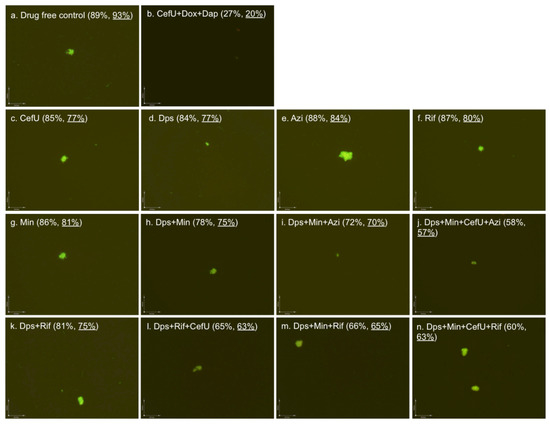
Figure 2.
Effect of antibiotics alone or in combinations on stationary phase B. burgdorferi culture. A seven-day-old B. burgdorferi stationary phase culture was incubated with the indicated drugs or drug combinations at a final concentration of 5 µg/mL for each antibiotic for seven days, followed by SYBR Green I/PI staining and epifluorescence microscopy (100× magnification). The calculated percentage and direct counting percentage (underlined) of residual viable cells are shown in brackets. Abbreviations: CefU, cefuroxime; Dps, dapsone; Azi, azithromycin; Rif, rifampin; Min, minocycline; Dox, doxycycline; Dap: daptomycin.
Sulfa drugs have recently been shown to have activity against B. burgdorferi persisters [13,14], and more recently, dapsone has been shown to improve the symptoms of patients with persistent Lyme disease [20]. Nevertheless, the relative activity of commonly used sulfa drugs such as sulfamethoxazole, dapsone and drug trimethoprim has not been compared under the same conditions. In this study, we found that the different sulfa drugs dapsone, sulfachlorpyridazine, sulfamethoxazole and trimethoprim, when used alone at their respective blood concentrations, had similar but limited activity against B. burgdorferi stationary phase cells. However, at the same molar concentrations, trimethoprim had comparable activity to dapsone, both of which seem to be slightly more active than sulfachlorpyridazine and sulfamethoxazole (Figure 1).
Although the sulfa drugs had some activity against B. burgdorferi stationary phase cells, their activities were enhanced when the sulfa drugs were combined with doxycycline, cefuroxime, ciprofloxacin, rifampin, or azithromycin, and the combination effects were more active than those of the respective single drugs. Among them, the oral four-drug combinations dapsone + minocycline + cefuroxime + azithromycin and dapsone + minocycline + cefuroxime + rifampin showed the best activity (residual viable cells at 58% and 60%, respectively, Figure 2j,n) against stationary phase B. burgdorferi. However, the sulfa drug combinations containing even up to four drugs still had considerably less activity against B. burgdorferi stationary phase cells than the best drug combination of daptomycin + cefuroxime + doxycycline (residual viable cells at 27%), used as a positive control (Figure 2b). As in our previous study [21], the daptomycin + cefuroxime + doxycycline drug combination could eradicate all B. burgdorferi cells as shown by all red (dead) cells or lack of aggregated biofilm-like microcolony structures under the microscope (Figure 2b).
In our previous studies [14,18,21], we used subculture to compare the samples with less than 30% viability after drug treatment to confirm whether the drugs eradicated the bacteria completely. However, in this study, most borrelia were still viable after sulfa drug or drug combination treatment with viable cells above 60%. In this case, the recovery subculture would not find any difference between these samples, and therefore we did not perform subculture tests in this study.
It is worth noting the present study was conducted in vitro and as such the findings may have limitations. The levels of antibiotics in in vitro systems and the degree of protein binding in BSK medium are quite different from human serum, and it remains to be seen if the differences in the relative activity of sulfa drugs and their combinations in vitro can be validated in vivo in animal models or in patients.
2.4. Effect of Sulfamethoxazole, Dapsone, Sulfachlorpyridazine, and Trimethoprim on Growing B. burgdorferi
We also determined the minimum inhibitory concentration (MIC) of sulfamethoxazole, dapsone, sulfachlorpyridazine and trimethoprim on growing B. burgdorferi using the standard microdilution method. Our results showed that the three sulfa drugs and trimethoprim could only partly inhibit the growth of B. burgdorferi, but failed to completely inhibit the growth, even at 200 µg/mL (Figure 3c–l). Sulfamethoxazole and trimethoprim showed an obvious inhibition effect at the lowest concentration (Figure 3c,g), and their combination nearly completely inhibited the growth of B. burgdorferi at 200 µg/mL (Figure 3l). However, even the 200 µg/mL of these drugs still could not completely inhibit the growth of B. burgdorferi compared to the start culture (Figure 3d,f,h,l). This result is in disagreement with our previous test in which sulfamethoxazole showed a low MIC (less than 0.25 µg/mL) [13]. There are several possible reasons for the discrepant results. First, in this study we used an animal-passaged B. burgdorferi strain instead of the previous unpassaged ATCC strain. Second, we could only selectively check some wells in the 96-well plate by counting chamber in the previous study, but in this study we checked every well directly in the 96-well plate with the BZ-X710 fluorescence microscopy. This greatly improved the experimental accuracy. In this study, we also found an obvious growth-inhibiting effect of sulfamethoxazole even at very low concentrations (0.4 µg/mL) (Figure 3c) compared to the drug-free control (Figure 3a). This inhibiting effect led to incorrect MIC determination because of the lack of a day 0 start culture control in the previous study. Besides the comparison to the drug-free control (Figure 3b), the sulfamethoxazole-treated B. burgdorferi culture grew mainly in microcolony form instead of spirochetal form (Figure 3c,d), which could also have led to difficulties and inaccuracy of the counting chamber method used in the previous study. Meanwhile, consistent with our previous experiment [13], doxycycline and amoxicillin, included as controls, did not show growth of B. burgdorferi, even at the lowest concentration of 0.2 µg/mL (Figure 3m–p).
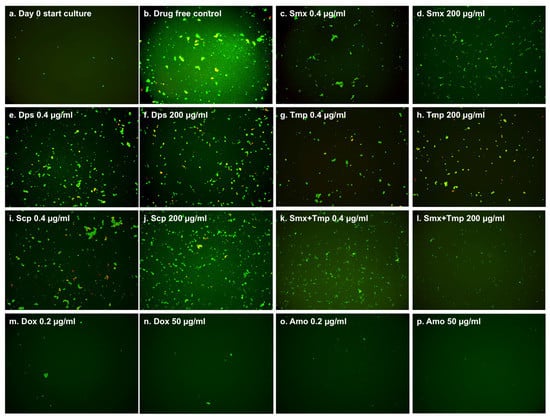
Figure 3.
Effect of antibiotics on growing B. burgdorferi culture (five days old). The 104 spirochetes in 90 µL fresh BSK-H medium as start culture (a) were incubated in 96-well microplate at 33 °C and 5% CO2. The 10 µL two-fold diluted antibiotics (200 µg/mL to 0.4 µg/mL) (c–l) and 10 µl DMSO as the drug-free control (b) were added to the start culture. After a five-day incubation, the cell proliferation of every well was assessed using the SYBR Green I/PI assay and BZ-X710 All-in-One fluorescence microscope (KEYENCE, Inc., Itasca, IL, USA).
3. Experimental Section
3.1. Strain, Media and Culture Techniques
Low passaged Borrelia burgdorferi strain B31 5A19 was kindly provided by Monica Embers [16,22]. The B. burgdorferi B31 strain was grown in BSK-H medium (HiMedia Laboratories Pvt. Ltd., Mumbai, India) and supplemented with 6% rabbit serum (Sigma-Aldrich, St. Louis, MO, USA). All culture medium was filter-sterilized by 0.2 μm filter. Cultures were incubated in sterile 15 mL conical tubes (BD Biosciences, CA, USA) in microaerophilic incubator (33 °C, 5% CO2) without antibiotics. After incubation for seven to 10 days, stationary-phase B. burgdorferi culture (about 107 spirochetes/mL) was transferred into a 96-well plate for evaluation with the drugs or their combinations.
3.2. Drugs
The following drugs were obtained from Sigma-Aldrich, St. Louis, MO, USA and dissolved in suitable solvents as suggested by the Clinical and Laboratory Standards Institute to make a 5 mg/mL stock solution: doxycycline (Dox), cefuroxime (CefU), ciprofloxacin (Cip), sulfamethoxazole (Smx), dapsone (Dps), sulfachlorpyridazine (Scp), trimethoprim (Tmp), azithromycin (Azi), rifampin (Rif), minocycline (Min) and daptomycin (Dap). The drug stock solutions were filter-sterilized using a 0.2 µm filter and stored at −20 °C.
3.3. Microscopy
The B. burgdorferi cultures were examined using a Zeiss AxioImager M2 microscope with epifluorescence illumination. Pictures were taken using a SPOT slider camera. The SYBR Green I/PI viability assay was performed to assess cell viability using the ratio of green/red fluorescence to determine the live:dead cell ratio, respectively, as described previously [14]. This residual cell viability reading was confirmed by analyzing three representative images of the bacterial culture using epifluorescence microscopy. Image Pro-Plus software was used to quantitatively determine the fluorescence intensity.
3.4. Evaluation of Drugs and Drug Combinations for Their Activities against B. burgdorferi Stationary Phase Cultures
For assessing the activity of drugs and drug combinations against stationary phase B. burgdorferi, 5 µL aliquots of the drugs were added to 96-well plate containing 100 µL of the seven-day-old stationary phase B. burgdorferi culture to obtain the desired drug concentration. Different drugs and drug combinations were evaluated at concentrations close to their Cmax values (maximum serum concentration). The plate was then sealed and was incubated at 33 °C and 5% CO2 without shaking for seven days when the residual viable cells remaining were calculated according to the regression equation and ratios of Green/Red fluorescence obtained by the SYBR Green I/PI viability assay, and then confirmed using epifluorescence microscopy as described [23]. Untreated groups were used as controls.
3.5. Minimum Inhibitory Concentration (MIC) Determination
The standard microdilution method was used to determine the MIC based on inhibition of visible growth of B. burgdorferi by microscopy. B. burgdorferi cells (1 × 104) were inoculated into each well of a 96-well microplate containing 90 mL fresh BSK-H medium per well. Antibiotics were two-fold diluted from 200 µg/mL to 0.4 µg/mL. Each diluted compound (10 µL) was added to the culture. All experiments were run in triplicate. The 96-well plate was sealed and placed in an incubator at 33 °C for five days. Cell proliferation was assessed using the SYBR Green I/PI assay and BZ-X710 All-in-One fluorescence microscope (KEYENCE, Inc.) after the incubation.
3.6. Statistical Analysis
All experiments were run in triplicate. Statistical analyses were performed using Student’s t-test.
4. Conclusions
In summary, dapsone, sulfachlorpyridazine and trimethoprim showed very similar activity against stationary phase B. burgdorferi at the same molarity concentration, and sulfamethoxazole was the least active drug among them. However, at blood concentrations, all four drugs had similar activity. It is worth noting that trimethoprim did not show synergy in the drug combinations with the three sulfa drugs at their serum concentrations. However, sulfa drugs and trimethoprim, when combined with other antibiotics such as doxycycline, ciprofloxacin and cefuroxime, were more active than the respective single drugs. However, none of the sulfa drug combinations were as effective as the daptomycin drug combination control since they were unable to completely eradicate B. burgdorferi stationary phase cells. Future studies are needed to optimize the drug combinations in vitro and to evaluate the sulfa drugs and their drug combinations in vivo.
Acknowledgments
We acknowledge the support of our work by the Steven & Alexandra Cohen Foundation, the Global Lyme Alliance, the Lyme Disease Association, and NatCapLyme. We thank Richard Horowitz for suggesting some drug combinations tested in this study. Ying Zhang was supported in part by NIH grants AI099512 and AI108535.
Author Contributions
Ying Zhang conceived the experiments; Jie Feng, Wanliang Shi, Shuo Zhang, performed the experiments; Jie Feng and Ying Zhang analyzed the data; Jie Feng and Ying Zhang wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- CDC. Lyme Disease. Available online: http://www.cdc.gov/lyme/ (accessed on 13 September 2015).
- Radolf, J.D.; Caimano, M.J.; Stevenson, B.; Hu, L.T. Of ticks, mice and men: Understanding the dual-host lifestyle of lyme disease spirochaetes. Nat. Rev. Microbiol. 2012, 10, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Wormser, G.P.; Dattwyler, R.J.; Shapiro, E.D.; Halperin, J.J.; Steere, A.C.; Klempner, M.S.; Krause, P.J.; Bakken, J.S.; Strle, F.; Stanek, G.; et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: Clinical practice guidelines by the infectious diseases society of america. Clin. Infect. Dis. 2006, 43, 1089–1134. [Google Scholar] [CrossRef] [PubMed]
- CDC. Post-Treatment Lyme Disease Syndrome. Available online: http://www.cdc.gov/lyme/postLDS/index.html (accessed on 18 September 2016).
- Steere, A.C.; Gross, D.; Meyer, A.L.; Huber, B.T. Autoimmune mechanisms in antibiotic treatment-resistant lyme arthritis. J. Autoimmun. 2001, 16, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Bockenstedt, L.K.; Gonzalez, D.G.; Haberman, A.M.; Belperron, A.A. Spirochete antigens persist near cartilage after murine lyme borreliosis therapy. J. Clin. Investig. 2012, 122, 2652–2660. [Google Scholar] [CrossRef] [PubMed]
- Swanson, S.J.; Neitzel, D.; Reed, K.D.; Belongia, E.A. Coinfections acquired from ixodes ticks. Clin. Microbiol. Rev. 2006, 19, 708–727. [Google Scholar] [CrossRef] [PubMed]
- Hodzic, E.; Feng, S.; Holden, K.; Freet, K.J.; Barthold, S.W. Persistence of Borrelia burgdorferi following antibiotic treatment in mice. Antimicrob. Agents Chemother. 2008, 52, 1728–1736. [Google Scholar] [CrossRef] [PubMed]
- Hodzic, E.; Imai, D.; Feng, S.; Barthold, S.W. Resurgence of persisting non-cultivable Borrelia burgdorferi following antibiotic treatment in mice. PLoS ONE 2014, 9, e86907. [Google Scholar] [CrossRef] [PubMed]
- Embers, M.E.; Barthold, S.W.; Borda, J.T.; Bowers, L.; Doyle, L.; Hodzic, E.; Jacobs, M.B.; Hasenkampf, N.R.; Martin, D.S.; Narasimhan, S.; et al. Persistence of Borrelia burgdorferi in rhesus macaques following antibiotic treatment of disseminated infection. PLoS ONE 2012, 7, e29914. [Google Scholar] [CrossRef]
- Straubinger, R.K.; Summers, B.A.; Chang, Y.F.; Appel, M.J. Persistence of Borrelia burgdorferi in experimentally infected dogs after antibiotic treatment. J. Clin. Microbiol. 1997, 35, 111–116. [Google Scholar] [PubMed]
- Marques, A.; Telford, S.R., 3rd; Turk, S.P.; Chung, E.; Williams, C.; Dardick, K.; Krause, P.J.; Brandeburg, C.; Crowder, C.D.; Carolan, H.E.; et al. Xenodiagnosis to detect Borrelia burgdorferi infection: A first-in-human study. Clin. Infect. Dis. 2014, 58, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Wang, T.; Shi, W.; Zhang, S.; Sullivan, D.; Auwaerter, P.G.; Zhang, Y. Identification of novel activity against Borrelia burgdorferi persisters using an FDA approved drug library. Emerg. Microb. Infect. 2014. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Auwaerter, P.G.; Zhang, Y. Drug combinations against Borrelia burgdorferi persisters in vitro: Eradication achieved by using daptomycin, cefoperazone and doxycycline. PLoS ONE 2015, 10, e0117207. [Google Scholar] [CrossRef] [PubMed]
- Sharma, B.; Brown, A.V.; Matluck, N.E.; Hu, L.T.; Lewis, K. Borrelia burgdorferi, the causative agent of lyme disease, forms drug-tolerant persister cells. Antimicrob. Agents Chemother. 2015, 59, 4616–4624. [Google Scholar] [CrossRef] [PubMed]
- Caskey, J.R.; Embers, M.E. Persister development by Borrelia burgdorferi populations in vitro. Antimicrob. Agents Chemother. 2015, 59, 6288–6295. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Shi, W.; Zhang, S.; Zhang, Y. Persister mechanisms in borrelia burgdorferi: Implications for improved intervention. Emerg. Microbes Infect. 2015. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Shi, W.; Zhang, S.; Sullivan, D.; Auwaerter, P.G.; Zhang, Y. A drug combination screen identifies drugs active against amoxicillin-induced round bodies of in vitro Borrelia burgdorferi persisters from an FDA drug library. Front. Microbiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Weitner, M.; Shi, W.; Zhang, S.; Sullivan, D.; Zhang, Y. Identification of additional anti-persister activity against Borrelia burgdorferi from an FDA drug library. Antibiotics 2015. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, R.; Freeman, P. The use of dapsone as a novel “persister” drug in the treatment of chronic lyme disease/post treatment lyme disease syndrome. J. Clin. Exp. Dermatol. Res. 2016. [Google Scholar] [CrossRef]
- Feng, J.; Weitner, M.; Shi, W.; Zhang, S.; Zhang, Y. Eradication of biofilm-like microcolony structures of Borrelia burgdorferi by daunomycin and daptomycin but not mitomycin C in combination with doxycycline and cefuroxime. Front. Microbiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Purser, J.E.; Norris, S.J. Correlation between plasmid content and infectivity in Borrelia burgdorferi. Proc. Natl. Acad. Sci. USA 2000, 97, 13865–13870. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Wang, T.; Zhang, S.; Shi, W.; Zhang, Y. An optimized SYBR Green I/PI assay for rapid viability assessment and antibiotic susceptibility testing for Borrelia burgdorferi. PLoS ONE 2014, 9, e111809. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).