Development and Validation of a Quick Sepsis-Related Organ Failure Assessment-Based Machine-Learning Model for Mortality Prediction in Patients with Suspected Infection in the Emergency Department
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection and Definition
2.3. Statistical Analysis and Machine Learning
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Rowan, K.M.; Angus, D.C.; Bailey, M.; Barnato, A.E.; Bellomo, R.; Canter, R.R.; Coats, T.J.; Delaney, A.; Gimbel, E.; Grieve, R.D.; et al. Early, Goal-Directed Therapy for Septic Shock—A Patient-Level Meta-Analysis. N. Engl. J. Med. 2017, 376, 2223–2234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.; Sibbald, W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- April, M.D.; Aguirre, J.; Tannenbaum, L.I.; Moore, T.; Pingree, A.; Thaxton, R.E.; Sessions, D.J.; Lantry, J.H. Sepsis Clinical Criteria in Emergency Department Patients Admitted to an Intensive Care Unit: An External Validation Study of Quick Sequential Organ Failure Assessment. J. Emerg. Med. 2017, 52, 622–631. [Google Scholar] [CrossRef]
- Askim, A.; Moser, F.; Gustad, L.T.; Stene, H.; Gundersen, M.; Asvold, B.O.; Dale, J.; Bjornsen, L.P.; Damas, J.K.; Solligard, E. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality—A prospective study of patients admitted with infection to the emergency department. Scand. J. TraumaResusc. Emerg. Med. 2017, 25, 56. [Google Scholar] [CrossRef]
- Canet, E.; Taylor, D.M.; Khor, R.; Krishnan, V.; Bellomo, R. qSOFA as predictor of mortality and prolonged ICU admission in Emergency Department patients with suspected infection. J. Crit. Care 2018, 48, 118–123. [Google Scholar] [CrossRef]
- Goulden, R.; Hoyle, M.C.; Monis, J.; Railton, D.; Riley, V.; Martin, P.; Martina, R.; Nsutebu, E. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emerg. Med. J. EMJ 2018, 35, 345–349. [Google Scholar] [CrossRef]
- Hwang, S.Y.; Jo, I.J.; Lee, S.U.; Lee, T.R.; Yoon, H.; Cha, W.C.; Sim, M.S.; Shin, T.G. Low Accuracy of Positive qSOFA Criteria for Predicting 28-Day Mortality in Critically Ill Septic Patients During the Early Period After Emergency Department Presentation. Ann. Emerg. Med. 2018, 71, 1–9. [Google Scholar] [CrossRef]
- Moskowitz, A.; Patel, P.V.; Grossestreuer, A.V.; Chase, M.; Shapiro, N.I.; Berg, K.; Cocchi, M.N.; Holmberg, M.J.; Donnino, M.W. Quick Sequential Organ Failure Assessment and Systemic Inflammatory Response Syndrome Criteria as Predictors of Critical Care Intervention Among Patients With Suspected Infection. Crit. Care Med. 2017, 45, 1813–1819. [Google Scholar] [CrossRef]
- Liu, Y.C.; Luo, Y.Y.; Zhang, X.; Shou, S.T.; Gao, Y.L.; Lu, B.; Li, C.; Chai, Y.F. Quick Sequential Organ Failure Assessment as a prognostic factor for infected patients outside the intensive care unit: A systematic review and meta-analysis. Intern. Emerg. Med. 2019, 14, 603–615. [Google Scholar] [CrossRef]
- Song, J.U.; Sin, C.K.; Park, H.K.; Shim, S.R.; Lee, J. Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: A systematic review and meta-analysis. Crit. Care 2018, 22, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maitra, S.; Som, A.; Bhattacharjee, S. Accuracy of quick Sequential Organ Failure Assessment (qSOFA) score and systemic inflammatory response syndrome (SIRS) criteria for predicting mortality in hospitalized patients with suspected infection: A meta-analysis of observational studies. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2018, 24, 1123–1129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, J.; Yang, J.; Mei, J.; Jin, Y.; Lu, Y. Head-to-head comparison of qSOFA and SIRS criteria in predicting the mortality of infected patients in the emergency department: A meta-analysis. Scand. J. TraumaResusc. Emerg. Med. 2018, 26, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, T.L.; Tang, Y.J.; Ching, L.J.; Abdullah, N.; Neoh, H.M. Comparison of Prognostic Accuracy of the quick Sepsis-Related Organ Failure Assessment between Short- & Long-term Mortality in Patients Presenting Outside of the Intensive Care Unit—A Systematic Review & Meta-analysis. Sci. Rep. 2018, 8, 16698. [Google Scholar] [CrossRef] [Green Version]
- Smith, G.B.; Prytherch, D.R.; Meredith, P.; Schmidt, P.E.; Featherstone, P.I. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013, 84, 465–470. [Google Scholar] [CrossRef]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM Mon. J. Assoc. Physicians 2001, 94, 521–526. [Google Scholar] [CrossRef] [Green Version]
- Cildir, E.; Bulut, M.; Akalin, H.; Kocabas, E.; Ocakoglu, G.; Aydin, S.A. Evaluation of the modified MEDS, MEWS score and Charlson comorbidity index in patients with community acquired sepsis in the emergency department. Intern. Emerg. Med. 2013, 8, 255–260. [Google Scholar] [CrossRef]
- Corfield, A.R.; Lees, F.; Zealley, I.; Houston, G.; Dickie, S.; Ward, K.; McGuffie, C. Utility of a single early warning score in patients with sepsis in the emergency department. Emerg. Med. J. EMJ 2014, 31, 482–487. [Google Scholar] [CrossRef]
- Geier, F.; Popp, S.; Greve, Y.; Achterberg, A.; Glockner, E.; Ziegler, R.; Heppner, H.J.; Mang, H.; Christ, M. Severity illness scoring systems for early identification and prediction of in-hospital mortality in patients with suspected sepsis presenting to the emergency department. Wien. Klin. Wochenschr. 2013, 125, 508–515. [Google Scholar] [CrossRef]
- Vorwerk, C.; Loryman, B.; Coats, T.J.; Stephenson, J.A.; Gray, L.D.; Reddy, G.; Florence, L.; Butler, N. Prediction of mortality in adult emergency department patients with sepsis. Emerg. Med. J. EMJ 2009, 26, 254–258. [Google Scholar] [CrossRef]
- Hamilton, F.; Arnold, D.; Baird, A.; Albur, M.; Whiting, P. Early Warning Scores do not accurately predict mortality in sepsis: A meta-analysis and systematic review of the literature. J. Infect. 2018, 76, 241–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, A.; Liu, T.; Shepherd, S.; Paiva, W. Using Statistical and Machine Learning Methods to Evaluate the Prognostic Accuracy of SIRS and qSOFA. Healthc. Inform. Res. 2018, 24, 139–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kia, A.; Timsina, P.; Joshi, H.N.; Klang, E.; Gupta, R.R.; Freeman, R.M.; Reich, D.L.; Tomlinson, M.S.; Dudley, J.T.; Kohli-Seth, R.; et al. MEWS++: Enhancing the Prediction of Clinical Deterioration in Admitted Patients through a Machine Learning Model. J. Clin. Med. 2020, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, M.E.; Lee Ng, C.H.; Goh, K.; Liu, N.; Koh, Z.X.; Shahidah, N.; Zhang, T.T.; Fook-Chong, S.; Lin, Z. Prediction of cardiac arrest in critically ill patients presenting to the emergency department using a machine learning score incorporating heart rate variability compared with the modified early warning score. Crit. Care 2012, 16, R108. [Google Scholar] [CrossRef] [Green Version]
- Vieira, S.M.; Mendonca, L.F.; Farinha, G.J.; Sousa, J.M.C. Modified binary PSO for feature selection using SVM applied to mortality prediction of septic patients. Appl. Soft. Comput. 2013, 13, 3494–3504. [Google Scholar] [CrossRef]
- Kim, J.; Chang, H.; Kim, D.; Jang, D.H.; Park, I.; Kim, K. Machine learning for prediction of septic shock at initial triage in emergency department. J. Crit. Care 2020, 55, 163–170. [Google Scholar] [CrossRef]
- Horng, S.; Sontag, D.A.; Halpern, Y.; Jernite, Y.; Shapiro, N.I.; Nathanson, L.A. Creating an automated trigger for sepsis clinical decision support at emergency department triage using machine learning. PLoS ONE 2017, 12, e0174708. [Google Scholar] [CrossRef] [Green Version]
- Delahanty, R.J.; Alvarez, J.; Flynn, L.M.; Sherwin, R.L.; Jones, S.S. Development and Evaluation of a Machine Learning Model for the Early Identification of Patients at Risk for Sepsis. Ann. Emerg. Med. 2019, 73, 334–344. [Google Scholar] [CrossRef]
- Rodriguez, R.M.; Greenwood, J.C.; Nuckton, T.J.; Darger, B.; Shofer, F.S.; Troeger, D.; Jung, S.Y.; Speich, K.G.; Valencia, J.; Kilgannon, J.H.; et al. Comparison of qSOFA with current emergency department tools for screening of patients with sepsis for critical illness. Emerg. Med. J. EMJ 2018, 35, 350–356. [Google Scholar] [CrossRef]
- Kwon, J.M.; Lee, Y.; Lee, Y.; Lee, S.; Park, J. An Algorithm Based on Deep Learning for Predicting In-Hospital Cardiac Arrest. J. Am. Heart Assoc. 2018, 7. [Google Scholar] [CrossRef] [Green Version]
- Donnelly, J.P.; Safford, M.M.; Shapiro, N.I.; Baddley, J.W.; Wang, H.E. Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) Classification: A retrospective population-based cohort study. Lancet 2017, 17, 661–670. [Google Scholar] [CrossRef]
- Nannan Panday, R.S.; Minderhoud, T.C.; Alam, N.; Nanayakkara, P.W.B. Prognostic value of early warning scores in the emergency department (ED) and acute medical unit (AMU): A narrative review. Eur. J. Intern. Med. 2017, 45, 20–31. [Google Scholar] [CrossRef] [PubMed]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Fernandes, M.; Vieira, S.M.; Leite, F.; Palos, C.; Finkelstein, S.; Sousa, J.M.C. Clinical Decision Support Systems for Triage in the Emergency Department using Intelligent Systems: A Review. Artif. Intell. Med. 2020, 102, 101762. [Google Scholar] [CrossRef] [PubMed]
- Raita, Y.; Goto, T.; Faridi, M.K.; Brown, D.F.M.; Camargo, C.A., Jr.; Hasegawa, K. Emergency department triage prediction of clinical outcomes using machine learning models. Crit. Care 2019, 23, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, S.W.; Ko, T.; Hong, K.J.; Kim, K.H. Machine Learning-Based Prediction of Korean Triage and Acuity Scale Level in Emergency Department Patients. Healthc. Inform. Res. 2019, 25, 305–312. [Google Scholar] [CrossRef]
- Hong, W.S.; Haimovich, A.D.; Taylor, R.A. Predicting hospital admission at emergency department triage using machine learning. PLoS ONE 2018, 13, e0201016. [Google Scholar] [CrossRef] [Green Version]
- Taylor, R.A.; Pare, J.R.; Venkatesh, A.K.; Mowafi, H.; Melnick, E.R.; Fleischman, W.; Hall, M.K. Prediction of In-hospital Mortality in Emergency Department Patients with Sepsis: A Local Big Data-Driven, Machine Learning Approach. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2016, 23, 269–278. [Google Scholar] [CrossRef] [Green Version]
- Perng, J.W.; Kao, I.H.; Kung, C.T.; Hung, S.C.; Lai, Y.H.; Su, C.M. Mortality Prediction of Septic Patients in the Emergency Department Based on Machine Learning. J. Clin. Med. 2019, 8. [Google Scholar] [CrossRef] [Green Version]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef]
- Cho, K.J.; Kwon, O.; Kwon, J.M.; Lee, Y.; Park, H.; Jeon, K.H.; Kim, K.H.; Park, J.; Oh, B.H. Detecting Patient Deterioration Using Artificial Intelligence in a Rapid Response System. Crit. Care Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Cortes-Puch, I.; Hartog, C.S. Opening the Debate on the New Sepsis Definition Change Is Not Necessarily Progress: Revision of the Sepsis Definition Should Be Based on New Scientific Insights. Am. J. Respir. Crit. Care Med. 2016, 194, 16–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dettori, J.R.; Norvell, D.C. The Anatomy of Data. Glob. Spine J. 2018, 8, 311–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo, R.S.L.; Leung, L.Y.; Brabrand, M.; Yeung, C.Y.; Chan, S.Y.; Lam, C.C.Y.; Hung, K.K.C.; Graham, C.A. qSOFA is a Poor Predictor of Short-Term Mortality in All Patients: A Systematic Review of 410,000 Patients. J. Clin. Med. 2019, 8. [Google Scholar] [CrossRef] [Green Version]
- Serafim, R.; Gomes, J.A.; Salluh, J.; Povoa, P. A Comparison of the Quick-SOFA and Systemic Inflammatory Response Syndrome Criteria for the Diagnosis of Sepsis and Prediction of Mortality: A Systematic Review and Meta-Analysis. Chest 2018, 153, 646–655. [Google Scholar] [CrossRef]
- Fleuren, L.M.; Klausch, T.L.T.; Zwager, C.L.; Schoonmade, L.J.; Guo, T.; Roggeveen, L.F.; Swart, E.L.; Girbes, A.R.J.; Thoral, P.; Ercole, A.; et al. Machine learning for the prediction of sepsis: A systematic review and meta-analysis of diagnostic test accuracy. Intensive Care Med. 2020. [Google Scholar] [CrossRef] [Green Version]

| Variable | Total (n = 23,587) | Training-Validation Datasets (n = 19,353) | Test Datasets (n = 4234) | p Value |
|---|---|---|---|---|
| Median age (IQR) | 63 (43–78) | 62 (42–77) | 67 (50–79) | <0.001 |
| Male sex (%) | 10862 (46.1) | 8850 (45.7) | 2012 (47.5) | 0.035 |
| Severity of illness scores (%) | ||||
| qSOFA ≥ 2, | 4698 (19.9) | 1692 (8.7) | 507 (12.0) | <0.001 |
| SIRS ≥ 2 | 12224 (51.8) | 9960 (51.5) | 2264 (53.5) | 0.018 |
| MEWS ≥ 5 | 5857 (24.8) | 4517 (23.3) | 1340 (31.6) | <0.001 |
| Suspected infection source (%) | <0.001 | |||
| Respiratory | 6736 (28.6) | 5437 (28.1) | 1299 (30.7) | |
| Intra-abdominal | 5693 (24.1) | 4622 (23.9) | 1071 (25.3) | |
| Urinary | 3638 (15.4) | 2998 (15.5) | 640 (15.1) | |
| Hepatobiliary | 1871 (7.9) | 1546 (8.0) | 325 (7.7) | |
| Otorhinolaryngological | 1789 (7.6) | 1481 (7.7) | 308 (7.3) | |
| Skin or musculoskeletal | 1132 (4.8) | 944 (4.9) | 188 (4.4) | |
| Gynecological | 430 (1.8) | 393 (2.0) | 37 (0.9) | |
| Central nervous system | 410 (1.8) | 342 (1.8) | 68 (1.6) | |
| Other or unknown | 1888 (8.0) | 1590 (8.2) | 298 (7.0) | |
| Outcomes | ||||
| In-hospital mortality (%) | 941 (4.0) | 795 (4.1) | 146 (3.4) | 0.048 |
| ICU admission (%) | 5173 (21.9) | 4191 (21.7) | 982 (23.2) | 0.029 |
| Hospital length of stay, median (IQR), d | 7 (5–12) | 7 (5–12) | 8 (5–13) | 0.004 |
| Mechanical ventilator use (%) | 1662 (7.0) | 1320 (6.9) | 330 (7.8) | 0.036 |
| Variable | AUROC (95% CI) | |||
|---|---|---|---|---|
| 3-Day Mortality | In-Hospital Mortality | 3-Day ICU Admission | ICU Admission | |
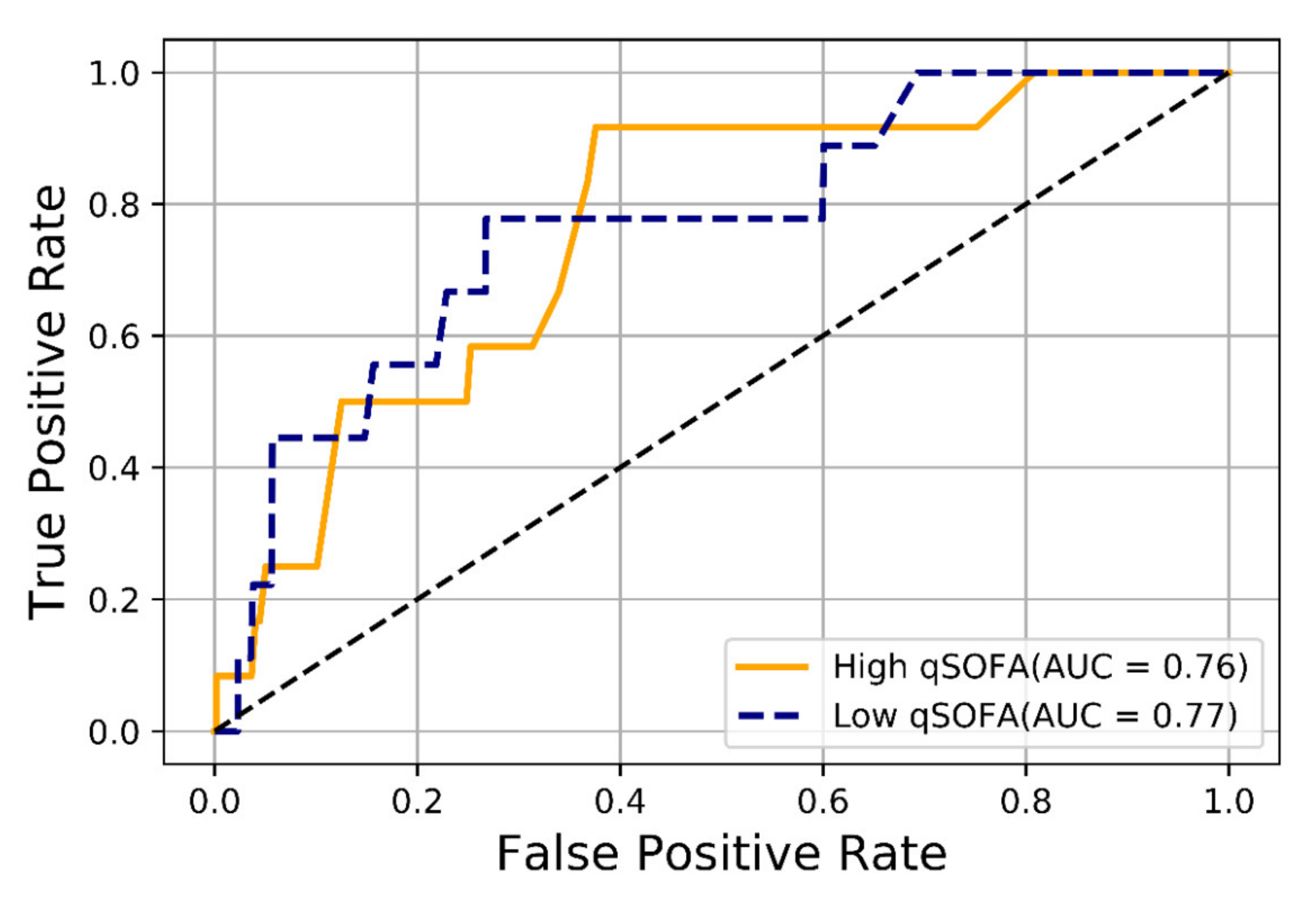
| qSOFA | 0.78 (0.68–0.88) | 0.71 (0.66–0.75) | 0.73 (0.72–0.75) | 0.73 (0.72–0.75) |
| SIRS | 0.68 (0.57–0.79) | 0.66 (0.62–0.70) | 0.63 (0.62–0.65) | 0.63 (0.61–0.65) |
| MEWS | 0.77 (0.67–0.86) | 0.65 (0.61–0.70) | 0.69 (0.67–0.71) | 0.69 (0.67–0.70) |
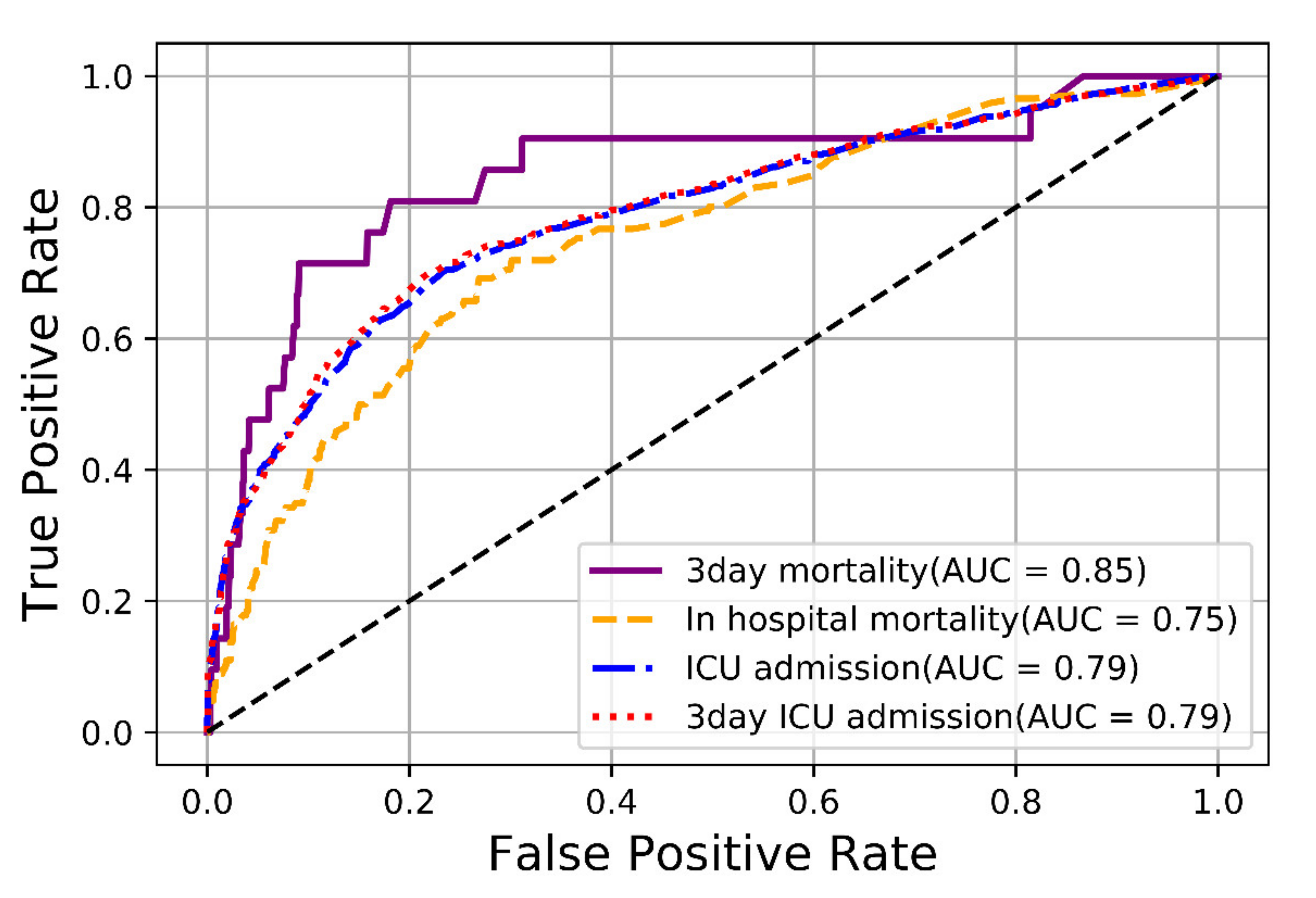
| Models | qSOFA Scores | qSOFA-Based Machine-Learning Models | |
|---|---|---|---|
| Outcomes | AUROC (95% CI) | p Value | |
| 3-day mortality | 0.78 (0.77–0.79) | 0.86 (0.85–0.87) | <0.001 |
| In-hospital mortality | 0.71 (0.69–0.72) | 0.75 (0.74–0.76) | 0.002 |
| 3-day ICU admission | 0.73 (0.72–0.75) | 0.79 (0.78–0.80) | <0.001 |
| ICU admission | 0.73 (0.72–0.75) | 0.79 (0.77–0.80) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, Y.S.; Baek, M.S. Development and Validation of a Quick Sepsis-Related Organ Failure Assessment-Based Machine-Learning Model for Mortality Prediction in Patients with Suspected Infection in the Emergency Department. J. Clin. Med. 2020, 9, 875. https://doi.org/10.3390/jcm9030875
Kwon YS, Baek MS. Development and Validation of a Quick Sepsis-Related Organ Failure Assessment-Based Machine-Learning Model for Mortality Prediction in Patients with Suspected Infection in the Emergency Department. Journal of Clinical Medicine. 2020; 9(3):875. https://doi.org/10.3390/jcm9030875
Chicago/Turabian StyleKwon, Young Suk, and Moon Seong Baek. 2020. "Development and Validation of a Quick Sepsis-Related Organ Failure Assessment-Based Machine-Learning Model for Mortality Prediction in Patients with Suspected Infection in the Emergency Department" Journal of Clinical Medicine 9, no. 3: 875. https://doi.org/10.3390/jcm9030875





