Effects of Hyponatremia Normalization on the Short-Term Mortality and Rehospitalizations in Patients with Recent Acute Decompensated Heart Failure: A Retrospective Study
Abstract
:1. Background
2. Methods
Statistical Analysis
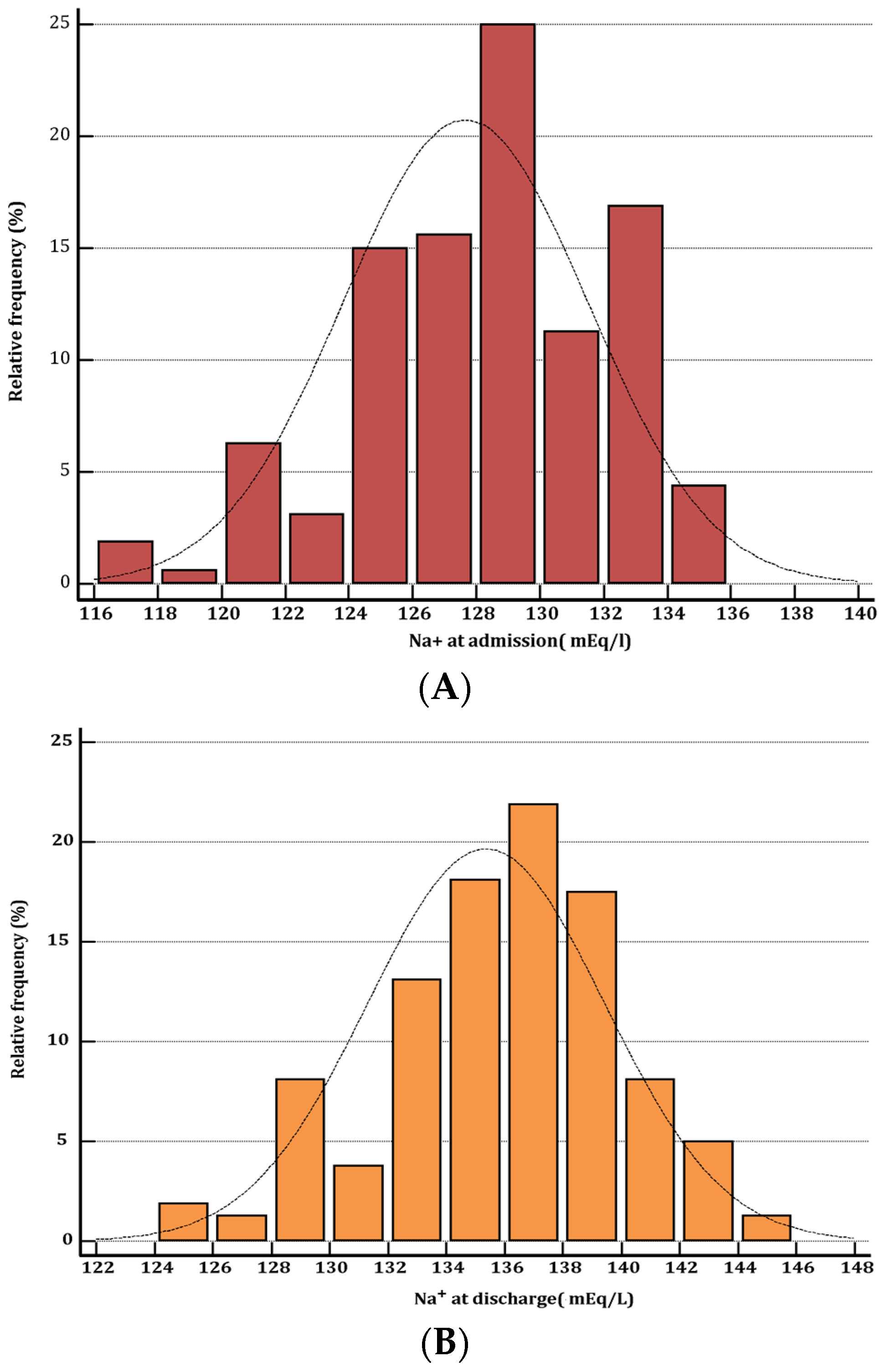
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Lee, W.H.; Packer, M. Prognostic importance of serum sodium concentration and its modification by converting-enzyme inhibition in patients with severe chronic heart failure. Circulation 1986, 73, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; Rossi, J.S.; Cotts, W.; Shin, D.D.; Hellkamp, A.S.; Piña, I.L.; Fonarow, G.C.; DeMarco, T.; Pauly, D.F.; Rogers, J.; et al. Characterization and prognostic value of persistent hyponatremia in patients with severe heart failure in the ESCAPE Trial. Arch. Intern. Med. 2007, 167, 1998–2005. [Google Scholar] [CrossRef]
- Tribouilloy, C.; Buiciuc, O.; Rusinaru, D.; Malaquin, D.; Lévy, F.; Peltier, M. Long-term outcome after a first episode of heart failure. A prospective 7-year study. Int. J. Cardiol. 2010, 140, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Hauptman, P.J.; Burnett, J.; Gheorghiade, M.; Grinfeld, L.; Konstam, M.A.; Kostic, D.; Krasa, H.B.; Maggioni, A.; Ouyang, J.; Swedberg, K.; et al. Clinical course of patients with hyponatremia and decompensated systolic heart failure and the effect of vasopressin receptor antagonism with tolvaptan. J. Card. Fail. 2013, 19, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Hamaguchi, S.; Kinugawa, S.; Tsuchihashi-Makaya, M.; Matsushima, S.; Sakakibara, M.; Ishimori, N.; Goto, D.; Tsutsui, H. Hyponatremia is an independent predictor of adverse clinical outcomes in hospitalized patients due to worsening heart failure. J. Cardiol. 2014, 63, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Rossi, J.; Bayram, M.; Udelson, J.E.; Lloyd-Jones, D.; Adams, K.F.; Oconnor, C.M.; Stough, W.G.; Ouyang, J.; Shin, D.D.; Orlandi, C.; et al. Improvement in hyponatremia during hospitalization for worsening heart failure is associated with improved outcomes: Insights from the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Chronic Heart Failure (ACTIV in CHF) trial. Acute Card. Care 2007, 9, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Klein, L.; O’Connor, C.M.; Leimberger, J.D.; Gattis-Stough, W.; Piña, I.L.; Felker, G.M.; Adams, K.F., Jr.; Califf, R.M.; Gheorghiade, M. OPTIME-CHF Investigators. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: Results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation 2005, 111, 2454–2460. [Google Scholar] [PubMed]
- Lee, S.E.; Choi, D.J.; Yoon, C.H.; Oh, I.Y.; Jeon, E.S.; Kim, J.J.; Cho, M.C.; Chae, S.C.; Ryu, K.H.; Oh, B.H. Improvement of hyponatraemia during hospitalisation for acute heart failure is not associated with improvement of prognosis: An analysis from the Korean Heart Failure (KorHF) registry. Heart 2012, 98, 1798–1804. [Google Scholar] [CrossRef]
- Verbalis, J.G.; Goldsmith, S.R.; Greenberg, A.; Korzelius, C.; Schrier, R.W.; Sterns, R.H.; Thompson, C.J. Diagnosis, evaluation, and treatment of hyponatremia: Expert panel recommendations. Am. J. Med. 2013, 126 (Suppl. S1), S1–S42. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, R.; Grossman, A.B.; Kar, P. Vasopressin receptor antagonist in the treatment of the syndrome of inappropriate antidiuretic hormone in general hospital practice. Endocr. J. 2012, 59, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; Konstam, M.A.; Burnett, J.C., Jr.; Grinfeld, L.; Maggioni, A.P.; Swedberg, K.; Udelson, J.E.; Zannad, F.; Cook, T.; Ouyang, J.; et al. Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST) Investigators. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: The EVEREST Clinical Status Trials. JAMA 2007, 297, 1332–1343. [Google Scholar] [PubMed]
- Konstam, M.A.; Gheorghiade, M.; Burnett, J.C.; Grinfeld, L.; Maggioni, A.P.; Swedberg, K.; Udelson, J.E.; Zannad, F.; Cook, T.; Ouyang, J.; et al. Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST) Investigators. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: The EVEREST Outcome Trial. JAMA 2007, 297, 1319–1331. [Google Scholar] [CrossRef] [PubMed]
- Donzé, J.D.; Beeler, P.E.; Bates, D.W. Impact of Hyponatremia Correction on the Risk for 30-Day Readmission and Death in Patients with Congestive Heart Failure. Am. J. Med. 2016, 129, 836–842. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Vaduganathan, M.; Fonarow, G.C.; Bonow, R.O. Rehospitalization for heart failure: Problems and perspectives. J. Am. Coll. Cardiol. 2013, 61, 391–403. [Google Scholar] [CrossRef] [PubMed]

| Variable | Persistent Hyponatremia at Discharge (No. 56 pts) | Serum Sodium Normalized at Discharge (No. 104 pts) | p-Value |
|---|---|---|---|
| Age, year, mean (SD) | 76 (10.4) | 77 (10.8) | 0.5723 |
| Male gender, No. (%) | 28 (50) | 54 (51.9) | 0.9471 |
| Previous hypertension, No. (%) | 30 (53.5) | 52 (50) | 0.7908 |
| Coronary artery disease, No. (%) | 24 (42.2) | 49 (46.2) | 0.7268 |
| COPD, No. (%) | 10 (17.85) | 19 (18.26) | 0.8803 |
| Diabetes, No. (%) | 16 (28.5) | 35 (33.65) | 0.6311 |
| Chronic kidney disease, (eGFR < 60 mL/min/1.73 m2) No. (%) | 23 (41) | 41 (39.4) | 0.9730 |
| Atrial flutter/ fibrillation, No. (%) | 17 (30.3) | 28 (0.27) | 0.7822 |
| LVEF (%), mean (SD) | 40 (6.6) | 40 (7.5) | 1.00 |
| SBP, mm Hg, mean (SD) | 105 (20) | 112 (21) | 0.043 * |
| Heart rate, bts/ min at admission, mean (SD) | 99 (15) | 95 (15) | 0.1096 |
| HFREF, No. (%) | 29 (51.7) | 51 (49) | 0.8684 |
| HFPEF, No. (%) | 27 (48.3) | 53 (51) | 0.8684 |
| Hb (g/dl), mean (SD) | 11.5 (0.6) | 11.3 (0.8) | 0.1034 |
| serum Na+, mEq/L at admission, mean (SD) | 130.5 (4.4) | 130.7 (5.5) | 0.8148 |
| serum creatinine, mg/dL, mean (SD) | 1.3 (0.2) | 1.25 (0.3) | 0.2646 |
| eGFR, mL/ min (admission), mean (SD) | 60 (12) | 64 (9) | 0.0186 * |
| BNP, pg/mL (admission), mean (SD) | 1100 (120) | 1058 (160) | 0.0874 |
| fluid removal after 48 h, L | 5.5 (1.8) | 5.050 (2.4) | 0.2210 |
| no. of admissions in the last 12 months, median(IQR) | 2.0 (0–3) | 0.5 (0–1) | 0.0182 *,‡ |
| length of stay of index admission, days, median (IQR) | 7.0 (4.75–8) | 5.0 (4–5) | 0.0186 *,‡ |
| I | Death or Rehospitalization during 30-Day Follow-Up | |||
| Yes | No | Total | ||
| Persistent hyponatremia | Yes | 42 | 14 | 56 |
| No | 10 | 94 | 104 | |
| Total | 52 | 108 | 160 | |
| Single table analysis: | ||||
| Odds ratio | 95% Confidence Interval | p-value | ||
| 28.2 | 11.58–68.62 | p < 0.0001 | ||
| IIA | Death within 30 Days after Discharge | |||
| Yes | No | Total | ||
| Persistent hyponatremia | Yes | 4 | 52 | 56 |
| No | 6 | 98 | 104 | |
| Total | 10 | 150 | 160 | |
| Single table analysis: | ||||
| Odds Ratio | 95% Confidence Interval | p (Fisher Exact Test) | ||
| 1.256 | 0.334–4.65 | 0.7410 | ||
| IIB | Readmission within 30 Days after Discharge | |||
| Yes | No | Total | ||
| Persistent hyponatremia | Yes | 36 | 20 | 56 |
| No | 6 | 98 | 104 | |
| Total | 42 | 118 | 160 | |
| Single table analysis: | ||||
| Odds Ratio | 95% Confidence Interval | p (Chi Square Corrected According to Yates) | ||
| 29.4 | 10.93–79.05 | <0.0001 | ||
| Variable | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|
| Persistent hyponatremia | 3.0743 | 1.3981–6.7601 | 0.0054 |
| Age | 1.0018 | 0.9668–1.0380 | 0.9235 |
| Male sex | 0.9982 | 0.5486–1.7223 | 0.5038 |
| Hospital admissions in the last 12 months | 2.0004 | 1.5171–2.6378 | <0.0001 |
| Length of stay of index admission | 1.4951 | 1.1680–1.9138 | 0.0015 |
| Coronary artery disease | 1.2155 | 0.6003–2.4612 | 0.5896 |
| COPD | 1.4590 | 0.7663–2.7779 | 0.2526 |
| Diabetes | 0.8538 | 0.4145–1.7588 | 0.6698 |
| Chronic kidney disease | 0.8053 | 0.4289–1.5122 | 0.5028 |
| Atrial flutter/fibrillation | 1.0400 | 0.4881–2.2160 | 0.9195 |
| NYHA class III at discharge | 3.0125 | 1.4942–6.0736 | 0.0022 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Vecchis, R.; Di Maio, M.; Di Biase, G.; Ariano, C. Effects of Hyponatremia Normalization on the Short-Term Mortality and Rehospitalizations in Patients with Recent Acute Decompensated Heart Failure: A Retrospective Study. J. Clin. Med. 2016, 5, 92. https://doi.org/10.3390/jcm5100092
De Vecchis R, Di Maio M, Di Biase G, Ariano C. Effects of Hyponatremia Normalization on the Short-Term Mortality and Rehospitalizations in Patients with Recent Acute Decompensated Heart Failure: A Retrospective Study. Journal of Clinical Medicine. 2016; 5(10):92. https://doi.org/10.3390/jcm5100092
Chicago/Turabian StyleDe Vecchis, Renato, Marco Di Maio, Giuseppina Di Biase, and Carmelina Ariano. 2016. "Effects of Hyponatremia Normalization on the Short-Term Mortality and Rehospitalizations in Patients with Recent Acute Decompensated Heart Failure: A Retrospective Study" Journal of Clinical Medicine 5, no. 10: 92. https://doi.org/10.3390/jcm5100092






