Sick Leave and Factors Influencing Sick Leave in Adult Patients with Atopic Dermatitis: A Cross-Sectional Study
Abstract
:1. Introduction
2. Results
Patient Characteristics
3. Severity of AD, Quality of Life and Socio—Occupational Complaints
| Demographics | Total Group- n = 253 | Outpatient Department- n = 120 | Patients’ Organization- n = 133 | Difference Chi Square-p/t-test-p | |
|---|---|---|---|---|---|
| Sex (n, %) | Man | 87 (34) | 51 (43) | 36 (27) | 0.010 |
| Woman | 166 (66) | 69 (58) | 97 (73) | ||
| Age (mean, sd) | 36.9 (12.4) (n = 252) range 18–70 | 36.3 (13.3) range 18–70 | 37.3 (11.4) (n = 132) range 18–65 | 0.52 | |
| Disease duration (mean in years, sd) | 28.1 (14.0) | 27.5 (14.0) | 28.7 (14.1) | 0.49 | |
| Education (n, %) | low | 29 (12) | 21 (18) | 8 (6) | 0.000 |
| medium | 99 (39) | 54 (45) | 45 (34) | ||
| high | 125 (49) | 45 (38) | 80 (60) | ||
| Work or school (n, %) | school | 15 (6) | 9 (8) | 6 (5) | 0.52 |
| work | 188 (74) | 86 (72) | 102 (77) | ||
| combination of work and school | 50 (20) | 25 (21) | 25 (19) | ||
| Other chronic diseases (n, %) | Yes | 137 (54) | 68 (57) | 69 (52) | 0.45 |
| No | 116 (46) | 52 (43) | 64 (48) | ||
| Other allergic diseases (hay fever, food allergy) (n, %) | Yes | 112 (44) | 55 (46) | 57 (43) | 0.63 |
| No | 141 (56) | 65 (54) | 76 (57) | ||
| Pulmonary diseases | Yes | 90 (36) | 45 (38) | 45 (34) | 0.54 |
| No | 163 (64) | 75 (63) | 88 (66) | ||
| Variable | Total Group (n = 253) | Outpatient Department (n = 120) | Patients’ Organization (n = 133) | Difference Chi square-p/t-test-p | |
|---|---|---|---|---|---|
| Severity of Atopic Dermatitis | |||||
| Severity (mean, sd) (POEM) | 15.1 (7.2) | 14.7 (7.2) | 15.5 (7.2) | 0.37 | |
| Severity (n, %) | Clear/almost clear (score 0–2) | 8 (3.2%) | 5 (4.2%) | 3 (2.3%) | |
| Mild (score 3–7) | 36 (14.2%) | 17 (14.2%) | 19 (14.3%) | ||
| Moderate (score 8–16) | 94 (37.2%) | 47 (39.2%) | 47 (35.3%) | ||
| Severe (score 17–24) | 89 (35.2%) | 41 (34.2%) | 48 (36.1%) | ||
| Very severe (score 25–28) | 26 (10.3%) | 10 (8.3%) | 16 (12.0%) | ||
| Quality of Life (Skindex 29) | |||||
| Symptoms (n, %) | score < 52 | 61 (24) | 34 (28) | 27 (20) | 0.14 |
| score ≥ 52 | 192 (76) | 86 (72) | 106 (80) | ||
| Emotions (n, %) | score < 39 | 138 (55) | 62 (52) | 76 (57) | 0.38 |
| score ≥39 | 115 (46) | 58 (48) | 57 (43) | ||
| Functioning (n, %) | score < 37 | 150 (59) | 79 (66) | 71 (53) | 0.04 |
| Score ≥ 37 | 103 (41) | 41(34) | 62 (47) | ||
| Overall score (n, %) | score < 44 | 143 (57) | 70 (58) | 73 (55) | 0.58 |
| Score ≥ 44 | 110 (44) | 50 (42) | 60 (45) | ||
| Social Occupational Complaints | |||||
| Symptom interference (n, %) | low to mean score | 241 (95) | 116 (97) | 125 (94) | 0.32 |
| above mean or high score (≥31) | 12 (5) | 4 (3) | 8 (6) | ||
| Distress (n, %) | low to mean score | 190 (75) | 93 (78) | 97 (73) | 0.40 |
| above mean or high score (≥29) | 63 (25) | 27 (23) | 36 (27) | ||
| Work pressure (n, %) | low to mean score | 147 (58) | 73 (61) | 74 (56) | 0.40 |
| above mean or high score (≥16) | 106 (42) | 47 (39) | 59 (44) | ||
| Job dissatisfaction (n, %) | low to mean score | 150 (59) | 76 (63) | 74 (56) | 0.21 |
| above mean or high score (≥26) | 103 (41) | 44 (37) | 59 (44) | ||
| Little flexibility (n, %) | low to mean score | 159 (63) | 70 (58) | 89 (67) | 0.16 |
| above mean or high score (≥17) | 94 (37) | 50 (42) | 44 (33) | ||
| Stressful home situation (n, %) | low to mean score | 182 (72) | 88 (73) | 94 (71) | 0.64 |
| above mean or high score (≥15) | 71 (28) | 32 (27) | 39 (29) | ||
| Avoidance/uncertainty (n, %) | low to mean score | 172 (68) | 85 (71) | 87 (65) | 0.36 |
| above mean or high score (≥24) | 81 (32) | 35 (29) | 46 (35) | ||
| Perfectionism/diligence (n, %) | low to mean score | 181 (72) | 85 (71) | 96 (72) | 0.81 |
| above mean or high score (≥37) | 72 (29) | 35 (29) | 37 (28) | ||
3.1. Prevalence of Sick Leave
3.2. Factors Influencing Sick Leave
| Sick Leave | Total Group (n = 253) | Outpatient Department (n = 120) | Patients’ Organization (n = 133) | Difference Chi2-p/t-test-p | |
|---|---|---|---|---|---|
| Sick leave in last two weeks | No n (%) | 196 (78) | 91 (76) | 105 (79) | 0.55 |
| Yes n (%) | 57 (23) | 29 (24) | 28 (21) | ||
| Sick leave in last two weeks due to AD | No n (%) | 222 (88) | 104 (87) | 118 (89) | na |
| Yes n (%) | 29 (12) | 15 (13) | 14 (11) | ||
| Mean (sd) number of sick leave days in last two weeks due to AD | 0.3 (0.9) (n = 251) | 0.3 (0.9) (n = 119) | 0.2 (0.8) (n = 132) | 0.47 | |
| Sick leave in last year | No n (%) | 90 (36) | 44 (37) | 46 (35) | 0.73 |
| Yes n (%) | 163 (64) | 76 (63) | 87 (65) | ||
| Sick leave in last year due to AD | No n (%) | 147 (58) (n = 252) | 67 (56) | 80 (61) | na |
| Yes n (%) | 105 (42) | 53 (44) | 52 (39) | ||
| Mean (sd) number of sick leave days in last year due to AD | 5.7(12.2) (n = 252) | 7.1 (15.0) | 4.4 (8.6) (n = 132) | 0.09 | |
| Influencing factor | Sick Leave Days in Last Two Weeks (n = 251) | ||
|---|---|---|---|
| Parameter | Wald ChiSquare Sig. | Odds Ratio | 95% Wald Confidence Interval for Odds Ratio Lower-Upper |
| Socio demographics | |||
| Age | 0.53 | 0.99 | 0.96–1.02 |
| Sex | 0.22 | 1.63 | 0.74–3.56 |
| Disease duration | 0.89 | 1.00 | 0.98–1.03 |
| Other chronic diseases | 0.74 | 1.14 | 0.53–2.47 |
| Numbers of days of work and school per week | 0.92 | 0.98 | 0.72–1.34 |
| Medium educational level | 0.89 | 0.91 | 0.24–3.47 |
| High educational level | 0.99 | 0.99 | 0.26–3.72 |
| Disease Severity and Quality of Life | |||
| Disease severity | 0.08 | 1.05 | 1.00–1.11 |
| Quality of life (total score) | 0.00 | 1.05 | 1.02–1.07 |
| Quality of life—subscale symptoms | 0.02 | 1.03 | 1.00–1.05 |
| Quality of life—subscale emotions | 0.00 | 1.03 | 1.01–1.05 |
| Quality of life—subscale functioning | 0.00 | 1.04 | 1.02–1.07 |
| Socio Occupational Factors | |||
| Symptom interference | 0.00 | 1.22 | 1.14–1.32 |
| Distress | 0.00 | 1.10 | 1.04–1.15 |
| Work pressure | 0.92 | 1.00 | 0.93–1.09 |
| Job dissatisfaction | 0.00 | 1.08 | 1.02–1.13 |
| Little flexibility | 0.61 | 1.02 | 0.94–1.11 |
| Stressful home situation | 0.00 | 1.14 | 1.05–1.24 |
| Avoidance/uncertainty | 0.00 | 1.09 | 1.03–1.15 |
| Perfectionism/diligence | 0.07 | 0.95 | 0.90–1.00 |
| Parameter (n = 251) | Wald ChiSquare Sig. | Odds Ratio | 95% Wald Confidence Interval for Odds Ratio Lower-Upper |
|---|---|---|---|
| (Intercept) | 0.00 | 0.01 | |
| Disease Severity and Quality of Life | |||
| Disease severity | 0.08 | 0.93 | 0.85–1.01 |
| Quality of life—total score | 0.51 | 1.02 | 0.97–1.06 |
| Socio Occupational Factors | |||
| Symptom interference | 0.00 | 1.26 | 1.13–1.40 |
| Distress | 0.91 | 1.00 | 0.91–1.09 |
| Job dissatisfaction | 0.63 | 1.02 | 0.95–1.08 |
| Stressful home situation | 0.14 | 1.08 | 0.98–1.19 |
| Avoidance/uncertainty | 0.71 | 1.02 | 0.93–1.11 |
| Perfectionism/diligence | 0.00 | 0.90 | 0.83–0.96 |
4. Discussion
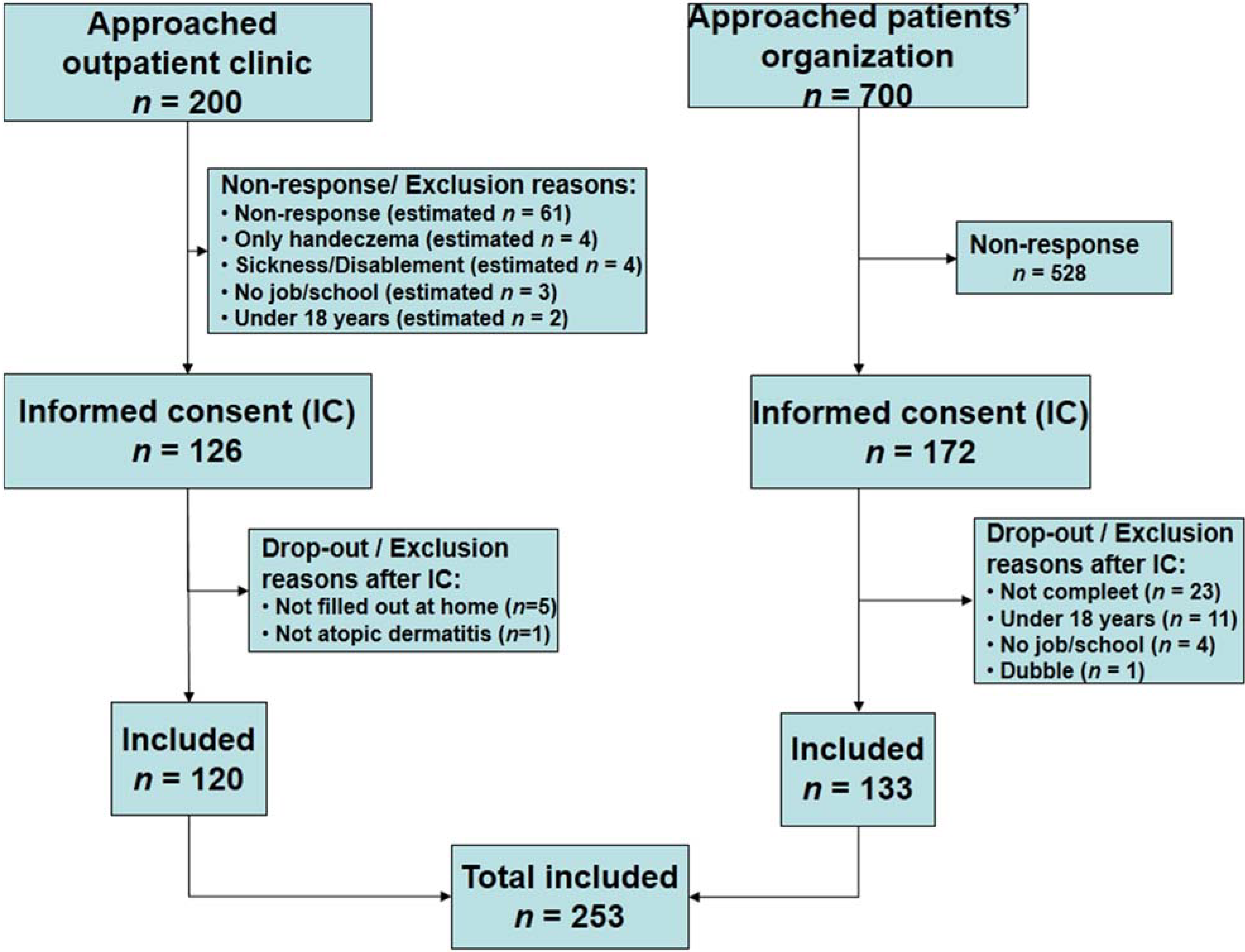
5. Materials and Methods
5.1. Design
5.2. Study Population:
5.3. Outcome Variables and Instruments
5.4. Data Analysis
5.5. Ethical Approval
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Eichenfield, L.F.; Tom, W.L.; Chamlin, S.L.; Feldman, S.R.; Hanifin, J.M.; Simpson, E.L.; Berger, T.G.; Bergman, J.N.; Cohen, D.E.; Cooper, K.D.; et al. Guidelines of care for the management of atopic dermatitis: Section 1. Diagnosis and assessment of atopic dermatitis. J. Am. Acad. Dermatol. 2014, 70, 338–351. [Google Scholar] [CrossRef] [PubMed]
- Verboom, P.; Hakkaart-Van, L.; Sturkenboom, M.; de Zeeuw, R.; Menke, H.; Rutten, F. The cost of atopic dermatitis in the Netherlands: An international comparison. Br. J. Dermatol. 2002, 147, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Holm, E.A.; Esmann, S.; Jemec, G.B. The handicap caused by atopic dermatitis—Sick leave and job avoidance. J. Eur. Acad. Dermatol. Venereol. 2006, 20, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Zuberbier, T.; Orlow, S.J.; Paller, A.S.; Taieb, A.; Allen, R.; Hernanz-Hermosa, J.M.; Ocampo-Candiani, J.; Cox, M.; Langeraar, J.; Simon, J.C. Patient perspectives on the management of atopic dermatitis. J. Allergy Clin. Immunol. 2006, 118, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Torrelo, A.; Ortiz, J.; Alomar, A.; Ros, S.; Prieto, M.; Cuervo, J. Atopic dermatitis: Impact on quality of life and patients’ attitudes toward its management. Eur. J. Dermatol. 2012, 22, 97–105. [Google Scholar] [PubMed]
- Fowler, J.F.; Duh, M.S.; Rovba, L.; Buteau, S.; Pinheiro, L.; Lobo, F.; Sung, J.; Doyle, J.J.; Swensen, A.; Mallett, D.A.; et al. The direct and indirect cost burden of atopic dermatitis: An employer-payer perspective. Manag. Care Interface 2007, 20, 26–32. [Google Scholar] [PubMed]
- Barbeau, M.; Bpharm, H.L. Burden of Atopic dermatitis in Canada. Int. J. Dermatol. 2006, 45, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez Barcala, F.J.; la Fuente-Cid, R.D.; Alvarez-Gil, R.; Tafalla, M.; Nuevo, J.; Caamano-Isorna, F. Factors associated with a higher prevalence of work disability among asthmatic patients. J. Asthma 2011, 48, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Boot, C.R.; van der Gulden, J.W.; Orbon, K.H.; Vercoulen, J.H.; Akkermans, R.; van Weel, C.; Folgering, H.T. Asthma and chronic obstructive pulmonary disease: Differences between workers with and without sick leave. Int. Arch. Occup. Environ. Health 2004, 77, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, J.M.; Ford, D.E. Work limitations and productivity loss are associated with health-related quality of life but not with clinical severity in patients with psoriasis. Dermatology 2006, 213, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Boot, C.R.; Vercoulen, J.H.; van der Gulden, J.W.; van den Borne, B.H.; Orbon, K.H.; van Weel, C.; Folgering, H.T. Sick leave in workers with asthma and COPD: The role of attitudes, perceived social norms and self efficacy. Patient Educ. Couns. 2005, 58, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Accordini, S.; Bugiani, M.; Arossa, W.; Gerzeli, S.; Marinoni, A.; Olivieri, M.; Pirina, P.; Carrozzi, L.; Dallari, R.; de Togni, A.; et al. Poor control increases the economic cost of asthma. A multicentre population-based study. Int. Arch. Allergy Immunol. 2006, 141, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Boot, C.R.; Vercoulen, J.H.; van der Gulden, J.W.; Orbon, K.H.; Rooijackers, J.M.; van Weel, C.; Folgering, H.T. Predictors of changes in sick leave in workers with asthma: A follow-up study. Int. Arch. Occup. Environ. Health 2005, 78, 633–640. [Google Scholar] [CrossRef] [PubMed]
- TNO. Ziekteverzuim in Nederland in 2010. Available online: http://www.rijksoverheid.nl/documenten-en-publicaties/brochures/2012/03/19/ziekteverzuim-in-nederland-in-2010.html (accessed on 1 May 2014).
- Mann, C.J. Observational research methods. Research design II: Cohort, cross sectional, and case-control studies. Emerg. Med. J. 2003, 20, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Roelen, C.A.; Koopmans, P.C.; Groothoff, J.W. Subjective health complaints in relation to sickness absence. Work 2010, 37, 15–21. [Google Scholar] [PubMed]
- Poulsen, O.M.; Persson, R.; Kristiansen, J.; Andersen, L.L.; Villadsen, E.; Orbaek, P. Distribution of subjective health complaints, and their association with register based sickness absence in the Danish working population. Scand. J. Public Health 2013, 41, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Charman, C.R.; Venn, A.J.; Ravenscroft, J.C.; Williams, H.C. Translating Patient-Oriented Eczema Measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br. J. Dermatol. 2013, 169, 1326–1332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vendrig, A. A Vragenlijst Arbeidsreintegratie. Available online: http://vendrig.praktijkinfo.nl/pagina/33/materialen-var/ (accessed on 1 May 2013).
- Vendrig, L. Risico op langdurig verzuim onderzocht met de Vragenlijst ArbeidsReïntegratie (VAR). Tijdschr. Gezondh. 2007, 85, 386–391. [Google Scholar] [CrossRef]
- Vendrig, L. De vragenlijst arbeidsreintegratie. Diagn. Wijzer 2005, 8, 27–39. [Google Scholar]
- Chren, M.M.; Lasek, R.J.; Quinn, L.M.; Mostow, E.N.; Zyzanski, S.J. Skindex, a quality-of-life measure for patients with skin disease: Reliability, validity, and responsiveness. J. Investig. Dermatol. 1996, 107, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, C.A.; Lindeboom, R.; Sprangers, M.A.; Legierse, C.M.; de Korte, J. Health-related quality of life assessment in dermatology: Interpretation of Skindex-29 scores using patient-based anchors. J. Investig. Dermatol. 2010, 130, 1318–1322. [Google Scholar] [CrossRef] [PubMed]
- Stichting Aquamarijn Handleiding Nederlandstalige Skindex-29; Een dermatologiespecifieke kwaliteit-van-leven vragenlijst. Available online: http://www.scribd.com/doc/1186801/skindex-handleiding (accessed on 1 May 2013).
- Chren, M.M.; Lasek, R.J.; Flocke, S.A.; Zyzanski, S.J. Improved discriminative and evaluative capability of a refined version of Skindex, a quality-of-life instrument for patients with skin diseases. Arch. Dermatol. 1997, 133, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Chren, M.M. The Skindex instruments to measure the effects of skin disease on quality of life. Dermatol. Clin. 2012, 30, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Charman, C.R.; Venn, A.J.; Williams, H.C. The patient-oriented eczema measure: Development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch. Dermatol. 2004, 140, 1513–1519. [Google Scholar] [CrossRef] [PubMed]
- Schram, M.E.; Spuls, P.I.; Leeflang, M.M.; Lindeboom, R.; Bos, J.D.; Schmitt, J. EASI, (objective) SCORAD and POEM for atopic eczema: Responsiveness and minimal clinically important difference. Allergy 2012, 67, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Raosoft Sample size calculator. 2004. Available online: http://www.raosoft.com/samplesize.html (accessed on 1 January 2012).
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Os-Medendorp, H.; Appelman-Noordermeer, S.; Bruijnzeel-Koomen, C.; De Bruin-Weller, M. Sick Leave and Factors Influencing Sick Leave in Adult Patients with Atopic Dermatitis: A Cross-Sectional Study. J. Clin. Med. 2015, 4, 535-547. https://doi.org/10.3390/jcm4040535
Van Os-Medendorp H, Appelman-Noordermeer S, Bruijnzeel-Koomen C, De Bruin-Weller M. Sick Leave and Factors Influencing Sick Leave in Adult Patients with Atopic Dermatitis: A Cross-Sectional Study. Journal of Clinical Medicine. 2015; 4(4):535-547. https://doi.org/10.3390/jcm4040535
Chicago/Turabian StyleVan Os-Medendorp, Harmieke, Simone Appelman-Noordermeer, Carla Bruijnzeel-Koomen, and Marjolein De Bruin-Weller. 2015. "Sick Leave and Factors Influencing Sick Leave in Adult Patients with Atopic Dermatitis: A Cross-Sectional Study" Journal of Clinical Medicine 4, no. 4: 535-547. https://doi.org/10.3390/jcm4040535





