The Model of “Informed Refusal” for Vaccination: How to Fight against Anti-Vaccinationist Misinformation without Disregarding the Principle of Self-Determination
Abstract
:1. Introduction
2. Anti-Vaccination Movement: Learning from the Past
3. Internet and Misinformation
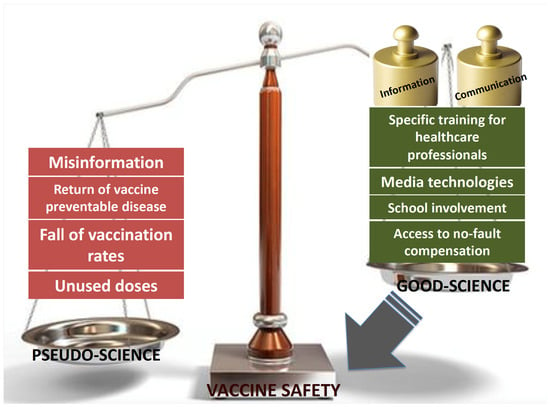
4. Promoting Vaccination through Information
5. Vaccines Safety: Evidence beyond Misperception
6. Vaccine Injury Compensation
7. The Ethical Issue of Mandatory Vaccination
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). Ten great public health achievements—United States. 1900–1999. MMWR Morb. Mortal Wkly. Rep. 1999, 48, 241–243. [Google Scholar]
- Isaacs, D.; Kilham, H.A.; Marshall, H. Should routine childhood immunizations be compulsory? J. Paediatr. Child Health 2004, 40, 392–396. [Google Scholar] [CrossRef]
- Seeman, N.; Ing, A.; Rizo, C. Assessing and responding in real time to online anti-vaccine sentiment during a flu pandemic. Healthc Q 2010, 13, 8–15. [Google Scholar] [CrossRef] [Green Version]
- Available online: http://www.reuters.com/article/us-flu-vaccine-usa-idUSTRE6425HW20100504 (accessed on 28 November 2016).
- Center for Diseases Control and Prevention. Measles United States. Morb. Mortal. Wkly. Rep. 2011, 60, 666–668. [Google Scholar]
- Chan, M.H.; Ma, L.; Sidelinger, D.; Bethel, L.; Yen, J.; Inveiss, A.; Sawyer, M.H.; Waters-Montijo, K.; Johnson, J.M.; Hicks, L.; et al. The California Pertussis Epidemic 2010: A review of 986 pediatric case reports from San Diego County. J. Pediatric Infect. Dis. Soc. 2012, 1, 47–54. [Google Scholar] [CrossRef] [Green Version]
- European Centre for Disease Prevention and Control. Measles and Rubella Monitoring; ECDC: Solna, Sweden, 2014. [Google Scholar]
- Schuster, M.; Eskola, J.; Duclos, P.; SAGE Working Group on Vaccine Hesitancy. Review of vaccine hesitancy: Rationale, remit and methods. Vaccine 2015, 33, 4157–4160. [Google Scholar] [CrossRef] [PubMed]
- Meszaros, J.R.; Asch, D.A.; Baron, J.; Hershey, J.C.; Kunreuther, H.; Schwartz-Buzaglo, J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J. Clin. Epidemiol. 1996, 49, 97–703. [Google Scholar] [CrossRef]
- Blume, S. Anti-vaccination movements and their interpretations. Soc. Sci. Med. 2006, 62, 628–642. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, R.M.; Sharp, L.K. Anti-vaccinationists past and present. BMJ 2002, 325, 430–432. [Google Scholar] [CrossRef] [Green Version]
- Williamson, S. Anti-vaccination leagues. Arch. Dis. Child. 1984, 59, 1195–1196. [Google Scholar] [CrossRef] [Green Version]
- Hennock, E.P. Vaccination policy against smallpox, 1835–1914: A comparison of England with Prussia and Imperial Germany. Soc. Hist. Med. 1998, 11, 49–71. [Google Scholar] [CrossRef] [PubMed]
- Swales, J.D. The Leicester anti-vaccination movement. Lancet 1992, 340, 1019–1021. [Google Scholar] [CrossRef]
- Olpinski, M. Anti-Vaccination Movement and Parental Refusals of Immunization of Children in USA. Pediatr. Pol. 2012, 87, 381–385. [Google Scholar] [CrossRef] [Green Version]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641. [Google Scholar] [CrossRef]
- Institute of Medicine. Immunization Safety Review: Vaccines and Autism; The National Academies Press: Washington, DC, USA, 2004. [Google Scholar] [CrossRef]
- Eggertson, L. Lancet retracts 12-year-old article linking autism to MMR vaccines. CMAJ 2010, 182, E199–E200. [Google Scholar] [CrossRef] [Green Version]
- Taylor, B.; Miller, E.; Farrington, C.P.; Petropoulos, M.C.; Favot-Mayaud, I.; Li, J.; Waight, P.A. Autism and measles, mumps, and rubella vaccine: No epidemiological evidence for a causal association. Lancet 1999, 353, 2026–2029. [Google Scholar] [CrossRef] [Green Version]
- Jama, A.; Lindstrand, A.; Ali, M.; Butler, R.; Kulane, A. Nurses’ Perceptions Of MMR Vaccine Hesitancy In An Area With Low Vaccination Coverage. Pediatr. Health Med. Ther. 2019, 10, 177–182. [Google Scholar] [CrossRef] [Green Version]
- Calvert, N.; Ashton, J.R.; Garnett, E. Mumps outbreak in private schools: Public health lessons for the post-Wakefield era. Lancet 2013, 381, 1625–1626. [Google Scholar] [CrossRef]
- Alvarez-Pasquín, M.J.; Heijbel, H.; Yarwood, J.; Van Damme, P.; VACSATC partners. VACSATC (vaccine safety: Attitudes, training and communication): Why such a project? Euro Surveill. 2009, 14, 19181. [Google Scholar] [CrossRef]
- Mason, B.W.; Donnelly, P.D. Impact of a local newspaper campaign on the uptake of the measles mumps and rubella vaccine. J. Epidemiol. Community Health 2000, 54, 473–474. [Google Scholar] [CrossRef] [Green Version]
- Kata, A. A postmodern Pandora’s box: Anti-vaccination misinformation on the Internet. Vaccine 2010, 28, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Dannetun, E.; Tegnell, A.; Hermansson, G.; Giesecke, J. Parents’ reported reasons for avoiding MMR vaccination. A telephone survey. Scand. J. Prim. Health Care 2005, 23, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Salmon, D.A.; Moulton, L.H.; Omer, S.B.; DeHart, M.P.; Stokley, S.; Halsey, N.A. Factors associated with refusal of childhood vaccines among parents of school-aged children: A case-control study. Arch. Pediatr. Adolesc. Med. 2005, 159, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Poland, G.A.; Jacobson, R.M. Understanding those who do not understand: A brie review of the anti-vaccine movement. Vaccine 2001, 19, 2440–2445. [Google Scholar] [CrossRef]
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm--an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef]
- Davies, P.; Chapman, S.; Leask, J. Antivaccination activists on the world wide web. Arch. Dis. Child. 2002, 87, 22–25. [Google Scholar] [CrossRef] [Green Version]
- Guess, A.M.; Nyhan, B.; O’Keeffe, Z.; Reifler, J. The sources and correlates of exposure to vaccine-related (mis)information online. Vaccine 2020, 38, 7799–7805. [Google Scholar] [CrossRef]
- Panatto, D.; Amicizia, D.; Arata, L.; Laia, P.L.; Gasparini, R. A comprehensive analysis of Italian web pages mentioning squalene-based influenza vaccine adjuvants reveals a high prevalence of misinformation. Hum. Vaccines Immunother. 2018, 14, 969–977. [Google Scholar] [CrossRef] [Green Version]
- Mereu, N.; Mereu, A.; Murgia, A.; Liori, A.; Piga, M.; Argiolas, F.; Salis, G.; Santus, S.; Porcu, C.; Contu, P.; et al. Vaccination Attitude and Communication in Early Settings: An Exploratory Study. Vaccines 2020, 8, 701. [Google Scholar] [CrossRef]
- Danchin, M.H.; Costa-Pinto, J.; Attwell, K.; Willaby, H.; Wiley, K.; Hoq, M.; Leask, J.; Perrett, K.P.; O’Keefe, J.; Giles, M.L.; et al. Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine 2018, 36, 6473–6479. [Google Scholar] [CrossRef]
- Vrdelja, M.; Kraigher, A.; Vercic, D.; Kropivnik, S. The growing vaccine hesitancy: Exploring the influence of the internet. Eur. J. Public Health 2018, 28, 934–939. [Google Scholar] [CrossRef] [PubMed]
- Gust, D.A.; Strine, T.W.; Maurice, E.; Smith, P.; Yusuf, H.; Wilkinson, M.; Battaglia, M.; Wright, R.; Schwartz, B. Underimmunization among children: Effects of vaccine safety concerns on immunization status. Pediatrics 2004, 114, e16–e22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hendrix, K.S.; Finnell, S.M.; Zimet, G.D.; Sturm, L.A.; Lane, K.A.; Downs, S.M. Vaccine message framing and parents’ intent to immunize their infants for MMR. Pediatrics 2014, 34, e675–e683. [Google Scholar] [CrossRef] [Green Version]
- Nyhan, B.; Reifler, J.; Richey, S.; Freed, G.L. Effective messages in vaccine promotion: A randomized trial. Pediatrics 2014, 133, e835–e842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahan, D.M. Social science A risky science communication environment for vaccines. Science 2013, 342, 53–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horne, Z.; Powell, D.; Hummel, J.E.; Holyoak, K.J. Countering antivaccination attitudes. Proc. Natl. Acad. Sci. USA 2015, 112, 10321–10324. [Google Scholar] [CrossRef] [Green Version]
- Parrish-Sprowl, J. Vaccine hesitancy communication: What counts as evidence. Vaccine 2018, 36, 6529–6530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diekema, D.S.; American Academy of Pediatrics Committee on Bioethics. Responding to parental refusals of immunization of children. Pediatrics 2005, 115, 1428–1431. [Google Scholar] [CrossRef] [Green Version]
- Poland, G.A.; Jacobson, R.M. The age-old struggle against the antivaccinationists. N. Engl. J. Med. 2011, 364, 97–99. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, S.; MacDonald, N.E.; Guirguis, S.; SAGE Working Group on Vaccine Hesitancy. Health communication and vaccine hesitancy. Vaccine 2015, 33, 4212–4214. [Google Scholar] [CrossRef] [Green Version]
- Ladner, J.; Besson, M.H.; Rodrigues, M.; Audureau, E.; Saba, J. Performance of 21 HPV vaccination programs implemented in low and middle-income countries, 2009–2013. BMC Public Health 2014, 14, 670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gottvall, M.; Tydén, T.; Larsson, M.; Stenhammar, C.; Höglund, A.T. Informed consent for HPV vaccination: A relational approach. Health Care Anal. 2015, 23, 50–62. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, R.M.; Targonski, P.V.; Poland, G.A. A taxonomy of reasoning flaws in the anti-vaccine movement. Vaccine 2007, 25, 3146–3152. [Google Scholar] [CrossRef] [PubMed]
- Nickerson, R.S. Confirmation Bias: A ubiquitous phenomenon in many guises. Rev. General Psychol. 1998, 2, 175–220. [Google Scholar] [CrossRef]
- Wilson, C.B.; Marcuse, E.K. Vaccine safety--vaccine benefits: Science and the public’s perception. Nat. Rev. Immunol. 2001, 1, 160–165. [Google Scholar] [CrossRef]
- Ball, R.; Horne, D.; Izurieta, H.; Sutherland, A.; Walderhaug, M.; Hsu, H. Statistical, epidemiological, and risk-assessment approaches to evaluating safety of vaccines throughout the life cycle at the Food and Drug Administration. Pediatrics 2011, 127 (Suppl. S1), S31–S38. [Google Scholar] [CrossRef] [Green Version]
- Alavian, S.M.; Tabatabaei, S.V. Effects of oral levamisole as an adjuvant to hepatitis B vaccine in adults with end-stage renal disease: A meta-analysis of controlled clinical trials. Clin. Ther. 2010, 32, 1–10. [Google Scholar] [CrossRef]
- Balicer, R.D.; Grotto, I.; Mimouni, M.; Mimouni, D. Is childhood vaccination associated with asthma? A meta- analysis of observational studies. Pediatrics 2007, 120, e1269–e1277. [Google Scholar] [CrossRef] [Green Version]
- WHO. Global Advisory Committee on Vaccine Safety, 10–11 June 2015. Wkly. Epidemiol. Rec. 2015, 90, 365–372. [Google Scholar]
- Institute of Medicine; Board on Population Health and Public Health Practice; Committee to Review Adverse Effects of Vaccines; Stratton, K.; Ford, A.; Rusch, E.; Clayton, E.W. Adverse Effects of Vaccines: Evidence and Causality; National Academies Press (US): Washington, DC, USA, 2012; pp. 57–102. [Google Scholar]
- Committee on the Assessment of Studies of Health Outcomes Related to the Recommended Childhood Immunization Schedule; Board on Population Health and Public Health Practice; Institute of Medicine. The Childhood Immunization Schedule and Safety: Stakeholder Concerns, Scientific Evidence, and Future Studies; National Academies Press (US): Washington, DC, USA, 2013; pp. 99–126. [Google Scholar]
- Asturias, E.J.; Wharton, M.; Pless, R.; MacDonald, N.E.; Chen, R.T.; Andrews, N.; Salisbury, D.; Dodoo, A.N.; Hartigan-Go, K.; Zuber, P.L.F. Contributions and challenges for worldwide vaccine safety: The Global Advisory Committee on Vaccine Safety at 15 years. Vaccine 2016, 34, 3342–3349. [Google Scholar] [CrossRef] [Green Version]
- Looker, C.; Kelly, H. No-fault compensation following adverse events attributed to vaccination: A review of international programmes. Bull.World Health Organ. 2011, 89, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Mariner, W.K. The National Vaccine Injury Compensation Program. Health Aff. 1992, 11, 255–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, G. Update on vaccine liability in the United States: Presentation at the National Vaccine Program Office Workshop on strengthening the supply of routinely recommended vaccines in the United States, 12 February 2002. Clin. Infect Dis. 2006, 42 (Suppl. S3), S130–S137. [Google Scholar] [CrossRef] [PubMed]
- Mello, M.M. Rationalizing vaccine injury compensation. Bioethics 2008, 22, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, D. Should Australia introduce a vaccine injury compensation scheme? J. Paediatr. Child Health 2004, 40, 247–249. [Google Scholar] [CrossRef] [PubMed]
- Keelan, J.; Wilson, K. Designing a No-Fault Vaccine Injury Compensation Programme for Canada: Lesson Learned from an International Analysis of Programmes; Munk School Briefings, University of Toronto: Toronto, ON, Canada, 2011. [Google Scholar]
- Yang, Y.T.; Silverman, R.D. Legislative prescriptions for controlling nonmedical vaccine exemptions. JAMA 2015, 313, 247–248. [Google Scholar] [CrossRef]
- Gostin, L.O. Law, ethics, and public health in the vaccination debates: Politics of the measles outbreak. JAMA 2015, 313, 1099–1100. [Google Scholar] [CrossRef]
- Constable, C.; Blank, N.R.; Caplan, A.L. Rising rates of vaccine exemptions: Problems with current policy and more promising remedies. Vaccine 2014, 32, 1793–1797. [Google Scholar] [CrossRef]
- Kennedy, A.M.; Brown, C.J.; Gust, D.A. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005, 120, 252–258. [Google Scholar] [CrossRef]
- Offit, P.A. Should childhood vaccination be mandatory? Yes. BMJ 2012, 344, e2434. [Google Scholar] [CrossRef]
- Silverman, R.D.; Hendrix, K.S. Point: Should childhood vaccination against measles be a mandatory requirement for attending school? Yes. Chest 2015, 148, 852–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schröder-Bäck, P.; Martakis, K. Counterpoint: Should childhood vaccination against measles be a mandatory requirement for attending school? No. Chest 2015, 148, 854–856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pelullo, C.P.; Marino, S.; Valdes Abuadili, A.J.; Signoriello, G.; Attena, F. Is it reasonable to abandon obligatory vaccinations in Italy? A 2013 survey. Euro Surveill. 2014, 19, 20889. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, D.M. Should childhood vaccination be mandatory? No. BMJ 2012, 344, e2435. [Google Scholar] [CrossRef]
- Haverkate, M.; D’Ancona, F.; Giambi, C.; Johansen, K.; Lopalco, P.L.; Cozza, V.; Appelgren, E.; VENICE project gatekeepers and contact points. Mandatory and recommended vaccination in the EU, Iceland and Norway: Results of the VENICE 2010 survey on the ways of implementing national vaccination programmes. Euro Surveill. 2012, 17, 20183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wynia, M.K. Mandating vaccination: What counts as a “mandate” in public health and when should they be used? Am. J. Bioeth. 2007, 7, 2–6. [Google Scholar] [CrossRef]
- Salmon, D.A.; Teret, S.P.; MacIntyre, C.R.; Salisbury, D.; Burgess, M.A.; Halsey, N.A. Compulsory vaccination and conscientious or philosophical exemptions: Past, present, and future. Lancet 2006, 367, 436–442. [Google Scholar] [CrossRef]
- Schröder-Bäck, P.; Brand, H.; Escamilla, I.; Davies, J.K.; Hall, C.; Hickey, K.; Jelastopulu, E.; Mechtler, R.; Volf, J. Ethical evaluation of compulsory measles immunisation as a benchmark for good health management in the European Union. Cent. Eur. J. Public Health 2009, 17, 183–186. [Google Scholar]
- Prislin, R.; Dyer, J.A.; Blakely, C.H.; Johnson, C.D. Immunization status and sociodemographic chracteristics: The mediating role of beliefs, attitudes, and perceived control. Am. J. Public Health 1998, 88, 1821–1826. [Google Scholar] [CrossRef] [Green Version]
- Smith, P.J.; Humiston, S.G.; Marcuse, E.K.; Zhao, Z.; Dorell, C.G.; Howes, C.; Hibbs, B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011, 126 (Suppl. S2), 135–146. [Google Scholar] [CrossRef] [Green Version]
- Samad, L.; Butler, N.; Peckham, C.; Bedford, H. Incomplete immunisation uptake in infancy: Maternal reasons. Vaccine 2006, 24, 6823–6829. [Google Scholar] [CrossRef] [PubMed]
- Leask, J. Vaccination and risk communication: Summary of a workshop, Arlington Virginia, USA, 5–6 October 2000. J. Paediatr. Child Health. 2002, 38, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Raithatha, N.; Holland, R.; Gerrard, S.; Harvey, I. A qualitative investigation of vaccine risk perception amongst parents who immunize their children: A matter of public health concern. J. Public Health Med. 2003, 25, 161–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walkinshaw, E. Mandatory vaccinations: The international landscape. CMAJ 2011, 183, E1167–E1168. [Google Scholar] [CrossRef] [Green Version]
- Isaacs, D.; Kilham, H.; Leask, J.; Tobin, B. Ethical issues in immunisation. Vaccine 2009, 27, 615–618. [Google Scholar] [CrossRef]
- Turillazzi, E.; Neri, M.; Riezzo, I.; Frati, P.; Fineschi, V. Informed consent in Italy-traditional versus the law: A gordian knot. Aesthetic Plast. Surg. 2014, 38, 759–764. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Errico, S.; Turillazzi, E.; Zanon, M.; Viola, R.V.; Frati, P.; Fineschi, V. The Model of “Informed Refusal” for Vaccination: How to Fight against Anti-Vaccinationist Misinformation without Disregarding the Principle of Self-Determination. Vaccines 2021, 9, 110. https://doi.org/10.3390/vaccines9020110
D’Errico S, Turillazzi E, Zanon M, Viola RV, Frati P, Fineschi V. The Model of “Informed Refusal” for Vaccination: How to Fight against Anti-Vaccinationist Misinformation without Disregarding the Principle of Self-Determination. Vaccines. 2021; 9(2):110. https://doi.org/10.3390/vaccines9020110
Chicago/Turabian StyleD’Errico, Stefano, Emanuela Turillazzi, Martina Zanon, Rocco Valerio Viola, Paola Frati, and Vittorio Fineschi. 2021. "The Model of “Informed Refusal” for Vaccination: How to Fight against Anti-Vaccinationist Misinformation without Disregarding the Principle of Self-Determination" Vaccines 9, no. 2: 110. https://doi.org/10.3390/vaccines9020110