Vaccine Candidates against Arenavirus Infections
Abstract
:1. Introduction
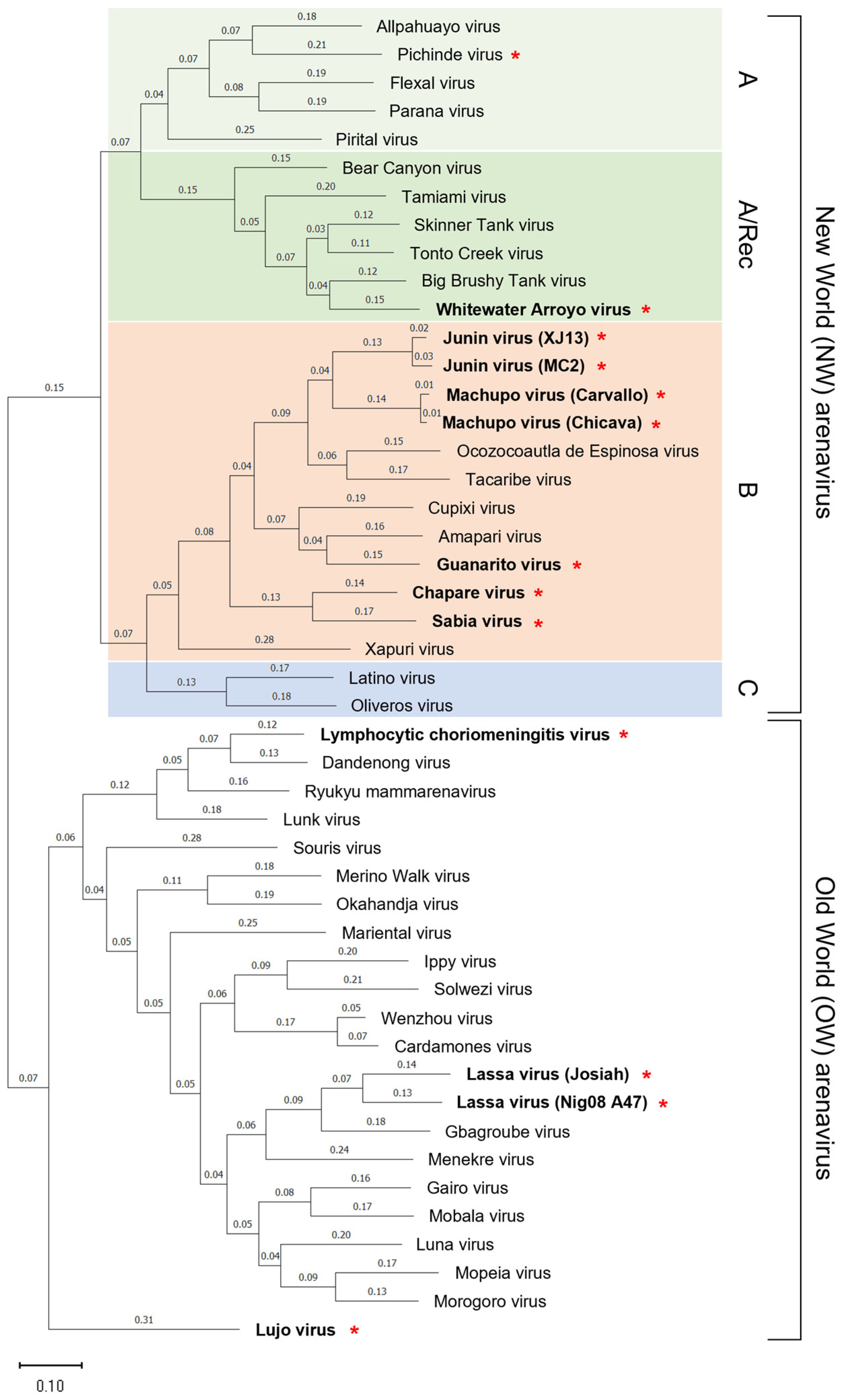
2. Classification and Distribution of Arenaviruses
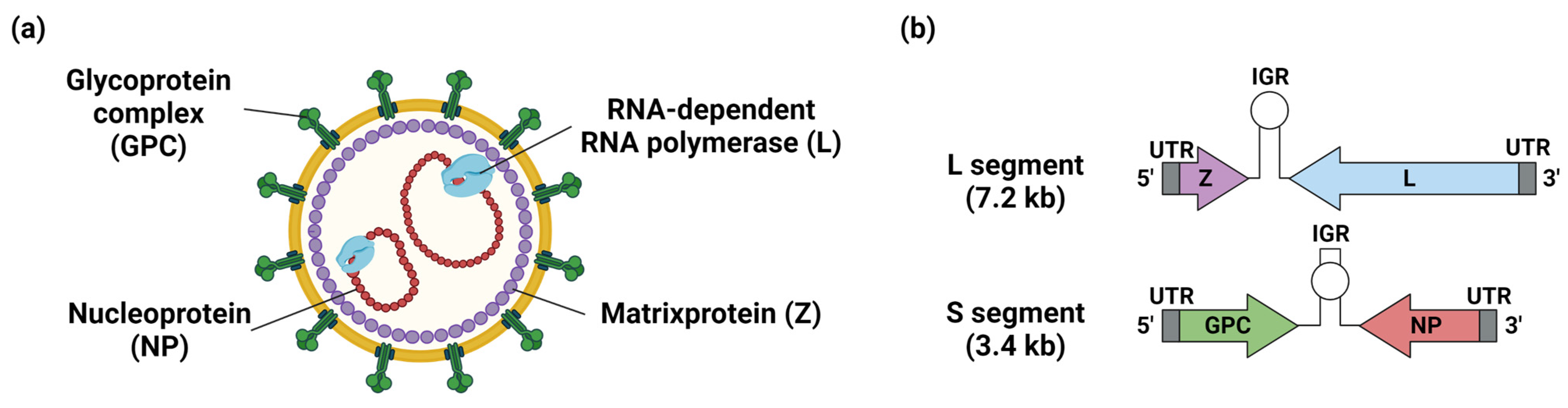
3. Structure of Arenavirus and Its Relevance to Vaccine Development
4. Immune Induction by Arenavirus Infection
5. Arenavirus Vaccine Development
5.1. Vaccine Candidates for LF
5.2. Vaccine Candidates for Other Arenavirus Infections
5.2.1. Vaccine Candidates for AHF
5.2.2. Vaccine Candidates for BHF
5.2.3. Vaccine Candidates for the Other Arenavirus Infections
6. Issues Hindering the Development of Vaccines against Other Arenavirus Infections
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grande-Pérez, A.; Martin, V.; Moreno, H.; De La Torre, J.C.; Grande-Pérez, A.; Martin, Á.V.; Moreno, Á.H.; De La Torre, J.C. Arenavirus Quasispecies and Their Biological Implications. Curr. Top. Microbiol. Immunol. 2016, 392, 231–275. [Google Scholar] [CrossRef] [PubMed]
- Hallam, S.J.; Koma, T.; Maruyama, J.; Paessler, S. Review of Mammarenavirus Biology and Replication. Front. Microbiol. 2018, 9, 1751. [Google Scholar] [CrossRef] [PubMed]
- Garry, R.F. Lassa Fever—the Road Ahead. Nat. Rev. Microbiol. 2023, 21, 87–96. [Google Scholar] [CrossRef]
- Warner, B.M.; Safronetz, D.; Stein, D.R. Current Research for a Vaccine against Lassa Hemorrhagic Fever Virus. Drug Des. Dev. Ther. 2018, 12, 2519–2527. [Google Scholar] [CrossRef] [PubMed]
- Silva-Ramos, C.R.; Faccini-Martínez, Á.A.; Calixto, O.J.; Hidalgo, M. Bolivian Hemorrhagic Fever: A Narrative Review. Travel Med. Infect. Dis. 2021, 40, 102001. [Google Scholar] [CrossRef]
- Clegg, J.C. Influence of Climate Change on the Incidence and Impact of Arenavirus Diseases: A Speculative Assessment. Clin. Microbiol. Infect. 2009, 15, 504–509. [Google Scholar] [CrossRef] [Green Version]
- Barrera Oro, J.G.; McKee, K.T. Toward a Vaccine against Argentine Hemorrhagic Fever. Bull. Pan Am. Health Organ. 1991, 25, 118–126. [Google Scholar]
- Ambrosio, A.; Saavedra, M.C.; Mariani, M.A.; Gamboa, G.S.; Maiza, A.S. Argentine Hemorrhagic Fever Vaccines. Hum. Vaccines 2011, 7, 694–700. [Google Scholar] [CrossRef]
- Droniou-Bonzom, M.E.; Reignier, T.; Oldenburg, J.E.; Cox, A.U.; Exline, C.M.; Rathbun, J.Y.; Cannon, P.M. Substitutions in the Glycoprotein (GP) of the Candid#1 Vaccine Strain of Junin Virus Increase Dependence on Human Transferrin Receptor 1 for Entry and Destabilize the Metastable Conformation of GP. J. Virol. 2011, 85, 13457–13462. [Google Scholar] [CrossRef] [Green Version]
- Nunberg, J.H.; York, J. The Curious Case of Arenavirus Entry, and Its Inhibition. Viruses 2012, 4, 83–101. [Google Scholar] [CrossRef] [Green Version]
- Sarute, N.; Ross, S.R. New World Arenavirus Biology. Annu. Rev. Virol. 2017, 4, 141–158. [Google Scholar] [CrossRef] [PubMed]
- Mapaco, L.; Crespin, L.; Rodrigues, D.; Gouy de Bellocq, J.; Bryja, J.; Bourgarel, M.; Missé, D.; Caron, A.; Fafetine, J.; Cappelle, J.; et al. Detection and Genetic Diversity of Mopeia Virus in Mastomys Natalensis from Different Habitats in the Limpopo National Park, Mozambique. Infect. Genet. Evol. 2022, 98, 105204. [Google Scholar] [CrossRef]
- Grobbelaar, A.A.; Jardine, J.; Burt, F.J.; Shepherd, A.J.; Shepherd, S.P.; Leman, P.A.; Kemp, A.; Braack, L.E.O.; Weyer, J.; Paweska, J.T.; et al. Mammarenaviruses of Rodents, South Africa and Zimbabwe. Emerg. Infect. Dis. 2021, 27, 3092–3102. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, J.; Reynard, S.; Carnec, X.; Pietrosemoli, N.; Dillies, M.A.; Baize, S. Non-Pathogenic Mopeia Virus Induces More Robust Activation of Plasmacytoid Dendritic Cells than Lassa Virus. Viruses 2019, 11, 287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishii, A.; Thomas, Y.; Moonga, L.; Nakamura, I.; Ohnuma, A.; Hang’ombe, B.; Takada, A.; Mweene, A.; Sawa, H. Novel Arenavirus, Zambia. Emerg. Infect. Dis. 2011, 17, 1921–1924. [Google Scholar] [CrossRef] [PubMed]
- Simulundu, E.; Mweene, A.S.; Changula, K.; Monze, M.; Chizema, E.; Mwaba, P.; Takada, A.; Ippolito, G.; Kasolo, F.; Zumla, A.; et al. Lujo Viral Hemorrhagic Fever: Considering Diagnostic Capacity and Preparedness in the Wake of Recent Ebola and Zika Virus Outbreaks. Rev. Med. Virol. 2016, 26, 446–454. [Google Scholar] [CrossRef] [Green Version]
- Saito, T.; Hattori, T.; Okuya, K.; Manzoor, R.; Miyamoto, H.; Kajihara, M.; Takada, A. Molecular Mechanisms Underlying the Cellular Entry and Host Range Restriction of Lujo Virus. MBio 2022, 13, e03060-21. [Google Scholar] [CrossRef]
- Downs, W.G.; Anderson, C.R.; Spence, L.; Aitken, T.H.; Greenhall, A.H. Tacaribe Virus, a New Agent Isolated from Artibeus Bats and Mosquitoes in Trinidad, West Indies. Am. J. Trop. Med. Hyg. 1963, 12, 640–646. [Google Scholar] [CrossRef]
- Price, J.L. Serological Evidence of Infection of Tacaribe Virus and Arboviruses in Trinidadian Bats. Am. J. Trop. Med. Hyg. 1978, 27, 162–167. [Google Scholar] [CrossRef]
- Escalera-Antezana, J.P.; Rodriguez-Villena, O.J.; Arancibia-Alba, A.W.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Rodríguez-Morales, A.J. Clinical Features of Fatal Cases of Chapare Virus Hemorrhagic Fever Originating from Rural La Paz, Bolivia, 2019: A Cluster Analysis. Travel Med. Infect. Dis. 2020, 36, 101589. [Google Scholar] [CrossRef]
- Nastri, A.C.; Duarte-Neto, A.N.; Casadio, L.V.B.; de Souza, W.M.; Claro, I.M.; Manuli, E.R.; Selegatto, G.; Salomão, M.C.; Fialkovitz, G.; Taborda, M.; et al. Understanding Sabiá Virus Infections (Brazilian Mammarenavirus). Travel Med. Infect. Dis. 2022, 48, 102351. [Google Scholar] [CrossRef]
- Rodríguez-Morales, A.J.; Bonilla-Aldana, D.K.; Risquez, A.; Paniz-Mondolfi, A.; Suárez, J.A. Should We Be Concerned about Venezuelan Hemorrhagic Fever?–A Reflection on Its Current Situation in Venezuela and Potential Impact in Latin America amid the Migration Crisis. New Microbes New Infect. 2021, 44, 100945. [Google Scholar] [CrossRef]
- Li, K.; Lin, X.D.; Wang, W.; Shi, M.; Guo, W.P.; Zhang, X.H.; Xing, J.G.; He, J.R.; Wang, K.; Li, M.H.; et al. Isolation and Characterization of a Novel Arenavirus Harbored by Rodents and Shrews in Zhejiang Province, China. Virology 2015, 476, 37–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamura, K.; Stecher, G.; Kumar, S. MEGA11: Molecular Evolutionary Genetics Analysis Version 11. Mol. Biol. Evol. 2021, 38, 3022–3027. [Google Scholar] [CrossRef]
- Fedeli, C.; Moreno, H.; Kunz, S. Novel Insights into Cell Entry of Emerging Human Pathogenic Arenaviruses. J. Mol. Biol. 2018, 430, 1839–1852. [Google Scholar] [CrossRef]
- Kang, H.; Cong, J.; Wang, C.; Ji, W.; Xin, Y.; Qian, Y.; Li, X.; Chen, Y.; Rao, Z. Structural Basis for Recognition and Regulation of Arenavirus Polymerase L by Z Protein. Nat. Commun. 2021, 12, 4134. [Google Scholar] [CrossRef]
- Kranzusch, P.J.; Whelan, S.P.J. Arenavirus Z Protein Controls Viral RNA Synthesis by Locking a Polymerase-Promoter Complex. Proc. Natl. Acad. Sci. USA 2011, 108, 19743–19748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cornu, T.I.; de la Torre, J.C. RING Finger Z Protein of Lymphocytic Choriomeningitis Virus (LCMV) Inhibits Transcription and RNA Replication of an LCMV S-Segment Minigenome. J. Virol. 2001, 75, 9415–9426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fehling, S.K.; Lennartz, F.; Strecker, T. Multifunctional Nature of the Arenavirus RING Finger Protein Z. Viruses 2012, 4, 2973. [Google Scholar] [CrossRef] [Green Version]
- Stott, R.J.; Strecker, T.; Foster, T.L. Distinct Molecular Mechanisms of Host Immune Response Modulation by Arenavirus NP and Z Proteins. Viruses 2020, 12, 784. [Google Scholar] [CrossRef]
- Papageorgiou, N.; Spiliopoulou, M.; Van Nguyen, T.H.; Vaitsopoulou, A.; Laban, E.Y.; Alvarez, K.; Margiolaki, I.; Canard, B.; Ferron, F. Brothers in Arms: Structure, Assembly and Function of Arenaviridae Nucleoprotein. Viruses 2020, 12, 772. [Google Scholar] [CrossRef]
- Carnec, X.; Mateo, M.; Page, A.; Reynard, S.; Hortion, J.; Picard, C.; Yekwa, E.; Barrot, L.; Barron, S.; Vallve, A.; et al. A Vaccine Platform against Arenaviruses Based on a Recombinant Hyperattenuated Mopeia Virus Expressing Heterologous Glycoproteins. J. Virol. 2018, 92, e02230-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mateo, M.; Reynard, S.; Carnec, X.; Journeaux, A.; Baillet, N.; Schaeffer, J.; Picard, C.; Legras-Lachuer, C.; Allan, R.; Perthame, E.; et al. Vaccines Inducing Immunity to Lassa Virus Glycoprotein and Nucleoprotein Protect Macaques after a Single Shot. Sci. Transl. Med. 2019, 11, eaaw3163. [Google Scholar] [CrossRef] [PubMed]
- Reynard, S.; Carnec, X.; Picard, C.; Borges-Cardoso, V.; Journeaux, A.; Mateo, M.; Germain, C.; Hortion, J.; Albrecht, L.; Perthame, E.; et al. A MOPEVAC Multivalent Vaccine Induces Sterile Protection against New World Arenaviruses in Non-Human Primates. Nat. Microbiol. 2023, 8, 64–76. [Google Scholar] [CrossRef]
- Ölschläger, S.; Flatz, L. Vaccination Strategies against Highly Pathogenic Arenaviruses: The Next Steps toward Clinical Trials. PLoS Pathog. 2013, 9, e1003212. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, B.M.; Sakabe, S.; Hartnett, J.N.; Ngo, N.; Goba, A.; Momoh, M.; Sandi, J.D.; Kanneh, L.; Cubitt, B.; Garcia, S.D.; et al. High Crossreactivity of Human T Cell Responses between Lassa Virus Lineages. PLoS Pathog. 2020, 16, 13. [Google Scholar] [CrossRef] [PubMed]
- Abreu-Mota, T.; Hagen, K.R.; Cooper, K.; Jahrling, P.B.; Tan, G.; Wirblich, C.; Johnson, R.F.; Schnell, M.J. Non-Neutralizing Antibodies Elicited by Recombinant Lassa–Rabies Vaccine Are Critical for Protection against Lassa Fever. Nat. Commun. 2018, 9, 4223. [Google Scholar] [CrossRef] [Green Version]
- Azim, K.F.; Lasker, T.; Akter, R.; Hia, M.M.; Bhuiyan, O.F.; Hasan, M.; Hossain, M.N. Combination of Highly Antigenic Nucleoproteins to Inaugurate a Cross-Reactive next Generation Vaccine Candidate against Arenaviridae Family. Heliyon 2021, 7, e07022. [Google Scholar] [CrossRef]
- Mantlo, E.; Paessler, S.; Huang, C. Differential Immune Responses to Hemorrhagic Fever-Causing Arenaviruses. Vaccines 2019, 7, 138. [Google Scholar] [CrossRef] [Green Version]
- Baize, S.; Marianneau, P.; Loth, P.; Reynard, S.; Journeaux, A.; Chevallier, M.; Tordo, N.; Deubel, V.; Contamin, H. Early and Strong Immune Responses Are Associated with Control of Viral Replication and Recovery in Lassa Virus-Infected Cynomolgus Monkeys. J. Virol. 2009, 83, 5890–5903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ibekwe, T.S.; Okokhere, P.O.; Asogun, D.; Blackie, F.F.; Nwegbu, M.M.; Wahab, K.W.; Omilabu, S.A.; Akpede, G.O. Early-Onset Sensorineural Hearing Loss in Lassa Fever. Eur. Arch. Oto-Rhino-Laryngol. 2011, 268, 197–201. [Google Scholar] [CrossRef]
- Mateer, E.J.; Huang, C.; Shehu, N.Y.; Paessler, S. Lassa Fever–Induced Sensorineural Hearing Loss: A Neglected Public Health and Social Burden. PLoS Negl. Trop. Dis. 2018, 12, e0006187. [Google Scholar] [CrossRef]
- Maruyama, J.; Reyna, R.A.; Kishimoto-Urata, M.; Urata, S.; Manning, J.T.; Harsell, N.; Cook, R.; Huang, C.; Nikolich-Zugich, J.; Makishima, T.; et al. CD4 T-Cell Depletion Prevents Lassa Fever Associated Hearing Loss in the Mouse Model. PLoS Pathog. 2022, 18, e1010557. [Google Scholar] [CrossRef] [PubMed]
- Sattler, R.A.; Maruyama, J.; Shehu, N.Y.; Makishima, T.; Paessler, S. Current Small Animal Models for LASV Hearing Loss. Curr. Opin. Virol. 2019, 37, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Yun, N.E.; Ronca, S.; Tamura, A.; Koma, T.; Seregin, A.V.; Dineley, K.T.; Miller, M.; Cook, R.; Shimizu, N.; Walker, A.G.; et al. Animal Model of Sensorineural Hearing Loss Associated with Lassa Virus Infection. J. Virol. 2016, 90, 2920–2927. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Isaac, A.B.; Karolina, W.; Temitope, A.A.; Anuska, R.; Joanne, E.; Deborah, A.; Bianca, O.C.; Filip, T.; Zofia, P.; Oluwasegun, O.I.; et al. Prospects Of Lassa Fever Candidate Vaccines. Afr. J. Infect. Dis. 2022, 16, 46. [Google Scholar] [CrossRef]
- Silva-Ramos, C.R.; Montoya-Ruíz, C.; Faccini-Martínez, Á.A.; Rodas, J.D. An Updated Review and Current Challenges of Guanarito Virus Infection, Venezuelan Hemorrhagic Fever. Arch. Virol. 2022, 167, 1727–1738. [Google Scholar] [CrossRef]
- de Mello Malta, F.; Amgarten, D.; de Seixas Santos Nastri, A.C.; Ho, Y.L.; Casadio, L.V.B.; Basqueira, M.; Selegatto, G.; Cervato, M.C.; Duarte-Neto, A.N.; Higashino, H.R.; et al. Sabiá Virus-like Mammarenavirus in Patient with Fatal Hemorrhagic Fever, Brazil, 2020. Emerg. Infect. Dis. 2020, 26, 1332–1334. [Google Scholar] [CrossRef]
- Stein, D.R.; Warner, B.M.; Soule, G.; Tierney, K.; Frost, K.L.; Booth, S.; Safronetz, D. A Recombinant Vesicular Stomatitis-Based Lassa Fever Vaccine Elicits Rapid and Long-Term Protection from Lethal Lassa Virus Infection in Guinea Pigs. npj Vaccines 2019, 4, 8. [Google Scholar] [CrossRef] [Green Version]
- Marzi, A.; Feldmann, F.; Geisbert, T.W.; Feldmann, H.; Safronetz, D. Vesicular Stomatitis Virus–Based Vaccines against Lassa and Ebola Viruses. Emerg. Infect. Dis. 2015, 21, 305–307. [Google Scholar] [CrossRef]
- Safronetz, D.; Mire, C.; Rosenke, K.; Feldmann, F.; Haddock, E.; Geisbert, T.; Feldmann, H. A Recombinant Vesicular Stomatitis Virus-Based Lassa Fever Vaccine Protects Guinea Pigs and Macaques against Challenge with Geographically and Genetically Distinct Lassa Viruses. PLoS Negl. Trop. Dis. 2015, 9, e0003736. [Google Scholar] [CrossRef] [PubMed]
- Mateo, M.; Reynard, S.; Journeaux, A.; Germain, C.; Hortion, J.; Carnec, X.; Picard, C.; Baillet, N.; Borges-Cardoso, V.; Merabet, O.; et al. A Single-Shot Lassa Vaccine Induces Long-Term Immunity and Protects Cynomolgus Monkeys against Heterologous Strains. Sci. Transl. Med. 2021, 13, 6348. [Google Scholar] [CrossRef] [PubMed]
- Cashman, K.A.; Wilkinson, E.R.; Shaia, C.I.; Facemire, P.R.; Bell, T.M.; Bearss, J.J.; Shamblin, J.D.; Wollen, S.E.; Broderick, K.E.; Sardesai, N.Y.; et al. A DNA Vaccine Delivered by Dermal Electroporation Fully Protects Cynomolgus Macaques against Lassa Fever. Hum. Vaccines Immunother. 2017, 13, 2902–2911. [Google Scholar] [CrossRef]
- Grant, A.; Seregin, A.; Huang, C.; Kolokoltsova, O.; Brasier, A.; Peters, C.; Paessler, S. Junín Virus Pathogenesis and Virus Replication. Viruses 2012, 4, 2317–2339. [Google Scholar] [CrossRef] [Green Version]
- Gowen, B.B.; Hickerson, B.T.; York, J.; Westover, J.B.; Sefing, E.J.; Bailey, K.W.; Wandersee, L.; Nunberg, J.H. Second-Generation Live-Attenuated Candid#1 Vaccine Virus Resists Reversion and Protects against Lethal Junín Virus Infection in Guinea Pigs. J. Virol. 2021, 95, e0039721. [Google Scholar] [CrossRef] [PubMed]
- Koma, T.; Patterson, M.; Huang, C.; Seregin, A.V.; Maharaj, P.D.; Miller, M.; Smith, J.N.; Walker, A.G.; Hallam, S.; Paessler, S. Machupo Virus Expressing GPC of the Candid # 1 Vaccine Strain of Junin Virus Is Highly Attenuated and Immunogenic. J. Virol. 2016, 90, 1290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salami, K.; Gouglas, D.; Schmaljohn, C.; Saville, M.; Tornieporth, N. A Review of Lassa Fever Vaccine Candidates. Curr. Opin. Virol. 2019, 37, 105–111. [Google Scholar] [CrossRef]
- Liu, G.; Cao, W.; Salawudeen, A.; Zhu, W.; Emeterio, K.; Safronetz, D.; Banadyga, L. Vesicular Stomatitis Virus: From Agricultural Pathogen to Vaccine Vector. Pathogens 2021, 10, 1092. [Google Scholar] [CrossRef]
- Ollmann Saphire, E. A Vaccine against Ebola Virus. Cell 2020, 181, 6. [Google Scholar] [CrossRef]
- Cross, R.W.; Woolsey, C.; Prasad, A.N.; Borisevich, V.; Agans, K.N.; Deer, D.J.; Geisbert, J.B.; Dobias, N.S.; Fenton, K.A.; Geisbert, T.W. A Recombinant VSV-Vectored Vaccine Rapidly Protects Nonhuman Primates against Heterologous Lethal Lassa Fever. Cell Rep. 2022, 40, 111094. [Google Scholar] [CrossRef]
- Fischer, R.J.; Purushotham, J.N.; van Doremalen, N.; Sebastian, S.; Meade-White, K.; Cordova, K.; Letko, M.; Jeremiah Matson, M.; Feldmann, F.; Haddock, E.; et al. ChAdOx1-Vectored Lassa Fever Vaccine Elicits a Robust Cellular and Humoral Immune Response and Protects Guinea Pigs against Lethal Lassa Virus Challenge. npj Vaccines 2021, 6, 32. [Google Scholar] [CrossRef]
- Collins, N.D.; Barrett, A.D.T. Live Attenuated Yellow Fever 17D Vaccine: A Legacy Vaccine Still Controlling Outbreaks In Modern Day. Curr. Infect. Dis. Rep. 2017, 19, 14. [Google Scholar] [CrossRef] [PubMed]
- Bredenbeek, P.J.; Molenkamp, R.; Spaan, W.J.M.; Deubel, V.; Marianneau, P.; Salvato, M.S.; Moshkoff, D.; Zapata, J.; Tikhonov, I.; Patterson, J.; et al. A Recombinant Yellow Fever 17D Vaccine Expressing Lassa Virus Glycoproteins. Virology 2006, 345, 299–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, X.; Dalebout, T.J.; Bredenbeek, P.J.; Carrion, R.; Brasky, K.; Patterson, J.; Goicochea, M.; Bryant, J.; Salvato, M.S.; Lukashevich, I.S. Yellow Fever 17D-Vectored Vaccines Expressing Lassa Virus GP1 and GP2 Glycoproteins Provide Protection against Fatal Disease in Guinea Pigs. Vaccine 2011, 29, 1248–1257. [Google Scholar] [CrossRef] [Green Version]
- Lukashevich, I.S. Advanced Vaccine Candidates for Lassa Fever. Viruses 2012, 4, 2514–2557. [Google Scholar] [CrossRef] [Green Version]
- Maruyama, J.; Mateer, E.J.; Manning, J.T.; Sattler, R.; Seregin, A.V.; Bukreyeva, N.; Jones, F.R.; Balint, J.P.; Gabitzsch, E.S.; Huang, C.; et al. Adenoviral Vector-Based Vaccine Is Fully Protective against Lethal Lassa Fever Challenge in Hartley Guinea Pigs. Vaccine 2019, 37, 6824–6831. [Google Scholar] [CrossRef]
- Osada, T.; Yang, X.Y.; Hartman, Z.C.; Glass, O.; Hodges, B.L.; Niedzwiecki, D.; Morse, M.A.; Lyerly, H.K.; Amalfitano, A.; Clay, T.M. Optimization of Vaccine Responses with an E1, E2b and E3-Deleted Ad5 Vector Circumvents Pre-Existing Anti-Vector Immunity. Cancer Gene Ther. 2009, 16, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Ramos, S.J.; Bangalore, P.; Elwood, D.; Cashman, K.A.; Kudchodkar, S.B.; Schultheis, K.; Pugh, H.; Walters, J.; Tur, J.; et al. Multivalent Dna Vaccines as a Strategy to Combat Multiple Concurrent Epidemics: Mosquito-Borne and Hemorrhagic Fever Viruses. Viruses 2021, 13, 382. [Google Scholar] [CrossRef]
- INO 4500; A DNA Based LASV Vaccine, Induces Robust T Cell Responses and Long-Term Memory Antigen-Specific T Cells|Vaccines Conferences|Vaccines Conferences 2021|International Vaccines Congress|Vaccines 2021. Available online: https://vaccinescongress.com/program/scientific-program/2021/ino-4500-a-dna-based-lasv-vaccine-induces-robust-t-cell-responses-and-long-term-memory-antigen-specific-t-cells (accessed on 7 December 2022).
- Zapata, J.C.; Poonia, B.; Bryant, J.; Davis, H.; Ateh, E.; George, L.; Crasta, O.; Zhang, Y.; Slezak, T.; Jaing, C.; et al. An Attenuated Lassa Vaccine in SIV-Infected Rhesus Macaques Does Not Persist or Cause Arenavirus Disease but Does Elicit Lassa Virus-Specific Immunity. Virol. J. 2013, 10, 52. [Google Scholar] [CrossRef] [Green Version]
- Lukashevich, I.S.; Patterson, J.; Carrion, R.; Moshkoff, D.; Ticer, A.; Zapata, J.; Brasky, K.; Geiger, R.; Hubbard, G.B.; Bryant, J.; et al. A Live Attenuated Vaccine for Lassa Fever Made by Reassortment of Lassa and Mopeia Viruses. J. Virol. 2005, 79, 13934–13942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lukashevich, I.S.; Carrion, R.; Salvato, M.S.; Mansfield, K.; Brasky, K.; Zapata, J.; Cairo, C.; Goicochea, M.; Hoosien, G.E.; Ticer, A.; et al. Safety, Immunogenicity, and Efficacy of the ML29 Reassortant Vaccine for Lassa Fever in Small Non-Human Primates. Vaccine 2008, 26, 5246–5254. [Google Scholar] [CrossRef] [Green Version]
- Salvato, M.S.; Lukashevich, I.S. Vaccines Against Lassa Fever. In New Gener Vaccines; CRC: Boca Raton, FL, USA, 2016; pp. 923–932. [Google Scholar] [CrossRef]
- Johnson, D.M.; Jokinen, J.D.; Lukashevich, I.S. Attenuated Replication of Lassa Virus Vaccine Candidate ML29 in STAT-1−/− Mice. Pathogens 2019, 8, 9. [Google Scholar] [CrossRef] [Green Version]
- Carrion, R.; Patterson, J.L.; Johnson, C.; Gonzales, M.; Moreira, C.R.; Ticer, A.; Brasky, K.; Hubbard, G.B.; Moshkoff, D.; Zapata, J.; et al. A ML29 Reassortant Virus Protects Guinea Pigs against a Distantly Related Nigerian Strain of Lassa Virus and Can Provide Sterilizing Immunity. Vaccine 2007, 25, 4093–4102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goicochea, M.A.; Zapata, J.C.; Bryant, J.; Davis, H.; Salvato, M.S.; Lukashevich, I.S. Evaluation of Lassa Virus Vaccine Immunogenicity in a CBA/J-ML29 Mouse Model. Vaccine 2012, 30, 1445–1452. [Google Scholar] [CrossRef] [Green Version]
- Reyna, R.A.; Maruyama, J.; Mantlo, E.K.; Manning, J.T.; Taniguchi, S.; Makishima, T.; Lukashevich, I.S.; Paessler, S. Depletion of CD4 and CD8 T Cells Reduces Acute Disease and Is Not Associated with Hearing Loss in ML29-Infected STAT1−/− Mice. Biomedicines 2022, 10, 2433. [Google Scholar] [CrossRef]
- Roman-Sosa, G.; Leske, A.; Ficht, X.; Dau, T.H.; Holzerland, J.; Hoenen, T.; Beer, M.; Kammerer, R.; Schirmbeck, R.; Rey, F.A.; et al. Immunization with GP1 but Not Core-like Particles Displaying Isolated Receptor-Binding Epitopes Elicits Virus-Neutralizing Antibodies against Junín Virus. Vaccines 2022, 10, 173. [Google Scholar] [CrossRef] [PubMed]
- Pushko, P.; Geisbert, J.; Parker, M.; Jahrling, P.; Smith, J. Individual and Bivalent Vaccines Based on Alphavirus Replicons Protect Guinea Pigs against Infection with Lassa and Ebola Viruses. J. Virol. 2001, 75, 11677–11685. [Google Scholar] [CrossRef] [Green Version]
- Lukashevich, I.S.; Pushko, P. Vaccine Platforms to Control Lassa Fever. Expert Rev. Vaccines 2016, 15, 1135–1150. [Google Scholar] [CrossRef]
- Müller, H.; Fehling, S.K.; Dorna, J.; Urbanowicz, R.A.; Oestereich, L.; Krebs, Y.; Kolesnikova, L.; Schauflinger, M.; Krähling, V.; Magassouba, N.F.; et al. Adjuvant Formulated Virus-like Particles Expressing Native-like Forms of the Lassa Virus Envelope Surface Glycoprotein Are Immunogenic and Induce Antibodies with Broadly Neutralizing Activity. npj Vaccines 2020, 5, 71. [Google Scholar] [CrossRef]
- Branco, L.M.; Grove, J.N.; Geske, F.J.; Boisen, M.L.; Muncy, I.J.; Magliato, S.A.; Henderson, L.A.; Schoepp, R.J.; Cashman, K.A.; Hensley, L.E.; et al. Lassa Virus-like Particles Displaying All Major Immunological Determinants as a Vaccine Candidate for Lassa Hemorrhagic Fever. Virol. J. 2010, 7, 279. [Google Scholar] [CrossRef] [Green Version]
- Cai, Y.; Iwasaki, M.; Motooka, D.; Liu, D.X.; Yu, S.; Cooper, K.; Hart, R.; Adams, R.; Burdette, T.; Postnikova, E.N.; et al. A Lassa Virus Live-Attenuated Vaccine Candidate Based on Rearrangement of the Intergenic Region. MBio 2020, 11, e00186-20. [Google Scholar] [CrossRef] [Green Version]
- Cai, Y.; Ye, C.; Cheng, B.; Nogales, A.; Iwasaki, M.; Yu, S.; Cooper, K.; Liu, D.X.; Hart, R.; Adams, R.; et al. A Lassa Fever Live-Attenuated Vaccine Based on Codon Deoptimization of the Viral Glycoprotein Gene. MBio 2020, 11, e00039-20. [Google Scholar] [CrossRef] [Green Version]
- Whitmer, S.L.M.; Strecker, T.; Cadar, D.; Dienes, H.P.; Faber, K.; Patel, K.; Brown, S.M.; Davis, W.G.; Klena, J.D.; Rollin, P.E.; et al. New Lineage of Lassa Virus, Togo, 2016. Emerg. Infect. Dis. 2018, 24, 599–602. [Google Scholar] [CrossRef] [PubMed]
- Siddle, K.J.; Eromon, P.; Barnes, K.G.; Mehta, S.; Oguzie, J.U.; Odia, I.; Schaffner, S.F.; Winnicki, S.M.; Shah, R.R.; Qu, J.; et al. Genomic Analysis of Lassa Virus during an Increase in Cases in Nigeria in 2018. N. Engl. J. Med. 2018, 379, 1745–1753. [Google Scholar] [CrossRef] [PubMed]
- Ehichioya, D.U.; Dellicour, S.; Pahlmann, M.; Rieger, T.; Oestereich, L.; Becker-Ziaja, B.; Cadar, D.; Ighodalo, Y.; Olokor, T.; Omomoh, E.; et al. Phylogeography of Lassa Virus in Nigeria. J. Virol. 2019, 93, e00929-19. [Google Scholar] [CrossRef] [Green Version]
- Bowen, M.D.; Rollin, P.E.; Ksiazek, T.G.; Hustad, H.L.; Bausch, D.G.; Demby, A.H.; Bajani, M.D.; Peters, C.J.; Nichol, S.T. Genetic Diversity among Lassa Virus Strains. J. Virol. 2000, 74, 6992–7004. [Google Scholar] [CrossRef] [Green Version]
- Manning, J.T.; Forrester, N.; Paessler, S. Lassa Virus Isolates from Mali and the Ivory Coast Represent an Emerging Fifth Lineage. Front. Microbiol. 2015, 6, 1037. [Google Scholar] [CrossRef] [Green Version]
- Ambrosio, A.M.; Riera, L.M.; Del Carmen Saavedra, M.; Sabattini, M.S.; Maiztegui, J.I. Immune Response to Vaccination against Argentine Hemorrhagic Fever in an Area Where Different Arenaviruses Coexist. Viral Immunol. 2006, 19, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Koma, T.; Huangid, C.; Cosciaid, A.; Hallamid, S.; Manningid, J.T.; Maruyamaid, J.; Walkerid, A.G.; Miller, M.; Smith, J.N.; Pattersonid, M.; et al. Glycoprotein N-Linked Glycans Play a Critical Role in Arenavirus Pathogenicity. PLoS Pathog. 2021, 17, e1009356. [Google Scholar] [CrossRef]
- Hallam, S.J.; Manning, J.T.; Maruyama, J.; Seregin, A.; Huang, C.; Walker, D.H.; de la Torre, J.C.; Paessler, S. A Single Mutation (V64G) within the Ring Domain of Z Attenuates Junin Virus. PLoS Negl. Trop. Dis. 2020, 14, e0008555. [Google Scholar] [CrossRef] [PubMed]
- York, J.; Nunberg, J.H. Epistastic Interactions within the Junín Virus Envelope Glycoprotein Complex Provide an Evolutionary Barrier to Reversion in the Live-Attenuated Candid#1 Vaccine. J. Virol. 2018, 92, e01682-17. [Google Scholar] [CrossRef] [Green Version]
- Gómez, R.M.; Jaquenod de Giusti, C.; Sanchez Vallduvi, M.M.; Frik, J.; Ferrer, M.F.; Schattner, M. Junín Virus. A XXI Century Update. Microbes Infect. 2011, 13, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Zaza, A.D.; Herbreteau, C.H.; Peyrefitte, C.N. Description and Characterization of a Novel Live-Attenuated Tri-Segmented Machupo Virus in Guinea Pigs. Virol. J. 2018, 15, 99. [Google Scholar] [CrossRef] [Green Version]
- Koma, T.; Huang, C.; Aronson, J.F.; Walker, A.G.; Miller, M.; Smith, J.N.; Patterson, M.; Paessler, S. The Ectodomain of Glycoprotein from the Candid#1 Vaccine Strain of Junin Virus Rendered Machupo Virus Partially Attenuated in Mice Lacking IFN-Aβ/γ Receptor. PLoS Negl. Trop. Dis. 2016, 10, e0004969. [Google Scholar] [CrossRef] [Green Version]
- Mantlo, E.K.; Maruyama, J.; Manning, J.T.; Wanninger, T.G.; Huang, C.; Smith, J.N.; Patterson, M.; Paessler, S.; Koma, T. Machupo Virus with Mutations in the Transmembrane Domain and Glycosylation Sites of the Glycoprotein Is Attenuated and Immunogenic in Animal Models of Bolivian Hemorrhagic Fever. J. Virol. 2022, 96, e00209-22. [Google Scholar] [CrossRef]
- Golden, J.W.; Beitzel, B.; Ladner, J.T.; Mucker, E.M.; Kwilas, S.A.; Palacios, G.; Hooper, J.W. An Attenuated Machupo Virus with a Disrupted L-Segment Intergenic Region Protects Guinea Pigs against Lethal Guanarito Virus Infection. Sci. Rep. 2017, 7, 4679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golden, J.W.; Maes, P.; Kwilas, S.A.; Ballantyne, J.; Hooper, J.W. Glycoprotein-Specific Antibodies Produced by DNA Vaccination Protect Guinea Pigs from Lethal Argentine and Venezuelan Hemorrhagic Fever. J. Virol. 2016, 90, 3515–3529. [Google Scholar] [CrossRef] [Green Version]
- Johnson, D.M.; Jokinen, J.D.; Wang, M.; Pfeffer, T.; Tretyakova, I.; Carrion, R.; Griffiths, A.; Pushko, P.; Lukashevich, I.S. Bivalent Junin & Machupo Experimental Vaccine Based on Alphavirus RNA Replicon Vector. Vaccine 2020, 38, 2949–2959. [Google Scholar] [CrossRef]
- Iwasaki, M.; Cubitt, B.; Sullivan, B.M.; de la Torre, J.C. The High Degree of Sequence Plasticity of the Arenavirus Noncoding Intergenic Region (IGR) Enables the Use of a Nonviral Universal Synthetic IGR To Attenuate Arenaviruses. J. Virol. 2016, 90, 3187–3197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, C.; de la Torre, J.C.; Martínez-Sobrido, L. Development of Reverse Genetics for the Prototype New World Mammarenavirus Tacaribe Virus. J. Virol. 2020, 94, e01014-20. [Google Scholar] [CrossRef] [PubMed]
- Dhanwani, R.; Zhou, Y.; Huang, Q.; Verma, V.; Dileepan, M.; Ly, H.; Liang, Y. A Novel Live Pichinde Virus-Based Vaccine Vector Induces Enhanced Humoral and Cellular Immunity after a Booster Dose. J. Virol. 2016, 90, 2551–2560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shieh, W.J.; Lan, S.; Zaki, S.R.; Ly, H.; Liang, Y. Pichinde Virus Infection of Outbred Hartley Guinea Pigs as a Surrogate Animal Model for Human Lassa Fever: Histopathological and Immunohistochemical Analyses. Pathogens 2020, 9, 579. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, A.L.; Tchitchek, N.; Safronetz, D.; Carter, V.S.; Williams, C.M.; Haddock, E.; Korth, M.J.; Feldmann, H.; Katze, M.G. Delayed Inflammatory and Cell Death Responses Are Associated with Reduced Pathogenicity in Lujo Virus-Infected Cynomolgus Macaques. J. Virol. 2015, 89, 2543–2552. [Google Scholar] [CrossRef] [Green Version]
- Lingas, G.; Rosenke, K.; Safronetz, D.; Guedj, J. Lassa Viral Dynamics in Non-Human Primates Treated with Favipiravir or Ribavirin. PLoS Comput. Biol. 2021, 17, e1008535. [Google Scholar] [CrossRef]
- Bell, T.M.; Shaia, C.I.; Bunton, T.E.; Robinson, C.G.; Wilkinson, E.R.; Hensley, L.E.; Cashman, K.A. Pathology of Experimental Machupo Virus Infection, Chicava Strain, in Cynomolgus Macaques (Macaca Fascicularis) by Intramuscular and Aerosol Exposure. Vet. Pathol. 2015, 52, 26–37. [Google Scholar] [CrossRef]
- Golden, J.W.; Hammerbeck, C.D.; Mucker, E.M.; Brocato, R.L. Corrigendum to “Animal Models for the Study of Rodent-Borne Hemorrhagic Fever Viruses: Arenaviruses and Hantaviruses”. Biomed. Res. Int. 2015, 2015, 313190. [Google Scholar] [CrossRef] [PubMed]
- Bradfute, S.B.; Stuthman, K.S.; Shurtleff, A.C.; Bavari, S. A STAT-1 Knockout Mouse Model for Machupo Virus Pathogenesis. Virol. J. 2011, 8, 300. [Google Scholar] [CrossRef] [Green Version]
- Maruyama, J.; Manning, J.T.; Mateer, E.J.; Sattler, R.; Bukreyeva, N.; Huang, C.; Paessler, S. Lethal Infection of Lassa Virus Isolated from a Human Clinical Sample in Outbred Guinea Pigs without Adaptation. mSphere 2019, 4, e00428-19. [Google Scholar] [CrossRef] [Green Version]
- Tang-Huau, T.L.; Feldmann, H.; Rosenke, K. Animal Models for Lassa Virus Infection. Curr. Opin. Virol. 2019, 37, 112–117. [Google Scholar] [CrossRef]
- Sattler, R.A.; Paessler, S.; Ly, H.; Huang, C. Animal Models of Lassa Fever. Pathogens 2020, 9, 197. [Google Scholar] [CrossRef] [Green Version]
- Falzaran, D.; Bente, D.A. Animal Models for Viral Haemorrhagic Fever. Clin. Microbiol. Infect. 2019, 21S, e17–e27. [Google Scholar] [CrossRef] [Green Version]
- Smith, D.R.; Holbrook, M.R.; Gowen, B.B. Animal Models of Viral Hemorrhagic Fever. Antivir. Res. 2014, 112, 59–79. [Google Scholar] [CrossRef]
- Bell, T.M.; Bunton, T.E.; Shaia, C.I.; Raymond, J.W.; Honnold, S.P.; Donnelly, G.C.; Shamblin, J.D.; Wilkinson, E.R.; Cashman, K.A. Pathogenesis of Bolivian Hemorrhagic Fever in Guinea Pigs. Vet. Pathol. 2016, 53, 190–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, W.C.; Geisbert, T.W.; Huggins, J.W.; Jahrling, P.B. Experimental Infection of Guinea Pigs with Venezuelan Hemorrhagic Fever Virus (Guanarito): A Model of Human Disease. Am. J. Trop. Med. Hyg. 1996, 55, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Tesh, R.B.; Jahrling, P.B.; Salas, R.; Shope, R.E. Description of Guanarito Virus (Arenaviridae: Arenavirus), the Etiologic Agent of Venezuelan Hemorrhagic Fever. Am. J. Trop. Med. Hyg. 1994, 50, 452–459. [Google Scholar] [CrossRef]
- Bird, B.H.; Dodd, K.A.; Erickson, B.R.; Albariño, C.G.; Chakrabarti, A.K.; McMullan, L.K.; Bergeron, E.; Ströeher, U.; Cannon, D.; Martin, B.; et al. Severe Hemorrhagic Fever in Strain 13/N Guinea Pigs Infected with Lujo Virus. PLoS Negl. Trop. Dis. 2012, 6, e1801. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Viruses | Diseases | Vaccine Platforms | Name of Vaccine Candidates | Antigen | Animal Experiment | Clinical Trial | Immumne Induction | Advantage | Disadvantage |
|---|---|---|---|---|---|---|---|---|---|
| LASV | LF | Inactivated viruses | |||||||
| Inactivated recombinant Lassa-Rabies virus | LASSARAB | GPC | Guinea pigs (80% protection) | Preclinical | Protective non-neutralizing antibodies | Partial protection in guinea pigs | |||
| Replication-incompetent virus vectors | |||||||||
| Recombinant serotype 5 adenovirus (Ad5) | Ad5 (E1-, E2b-) LASV-NP,-GPC | GPC and NP | Guinea pigs (100% protection) | Preclinical | Neutralizing antibodies | High stability, low risk of adverse event, unaffected by prior immunity to adenovirus | |||
| DNA vaccines candidate | |||||||||
| Plasmid DNA vaccine encoding LASV GPC | INO-4500 | GPC | Guinea pigs (100% protection), NHPs (100% protection) | Phase I | T cell response (Induction of GPC-reactive CD4 ant CD8 Tcell) | Long shelf life, Long term immunity | Special equipment requirements | ||
| Replication-competent virus vectors | |||||||||
| Vesicular stomatitis virus vector | rVSVΔG-LASV-GPC | GPC | Guinea pigs (100% protection), NHPs (100% protection) | Phase I | Neutralizing antibodies T cell response | Long term immunity, Cross protection among LASV lineages | Possible effects of preimmunity to VSV, Mild side effects | ||
| Vaccinia virus vector | V-LSG | GPC | Cynomolgus macaques (67% protection), Rhesus macaques (100% protection) | Preclinical | T cell response (Cell-mediated immunity) | Good safety, stable antigen expression and convenient storage | Partial protection in the animal models | ||
| Chimpanzee adenovirus vector | ChAdOx1-Lassa-GPC | GPC | Guinea pigs (100% protection) | Preclinical | T cell response (Cell-mediated immunity) | Unaffected by prior immunity to human adenovirus | |||
| Measles Schwarz virus vector | MV-LASV (MeV-NP) | GPC and NPEXON | NHPs (100% protection) | Phase I | T cell response (Cell-mediated immunity) | Long term immunity, Cross protection among LASV lineages | |||
| Yellow fever virus 17D vector | YF17D/LASV-GPC | GPC | Guinea pigs (80% protection), Common marmosets (0% protection) | Preclinical | T cell response (Cell-mediated immunity) | Potential as a bivalent vaccine to YF and LF | Partial protection in the animal models Possible effects of preimmunity to YF | ||
| Recombinant live-attenuated virus | |||||||||
| Recombinant LASV with the replacement of L segment IGR with that of S segment | rLASV(IGR/S-S) | Whole virus | Guinea pigs (100% protection) | Preclinical | T cell response (Cell-mediated immunity) | Genetically stable in vitro | |||
| Recombinant LASV with codon deoptimized GPC genes | rLASV-GPC/CD | Whole virus | Guinea pigs (100% protection) | Preclinical | T cell response (Cell-mediated immunity) | Genetically stable in vitro | |||
| Recombinant MOPV with NPExoN and LASV GPC | MOPEVACLASV | Whole virus | Cynomolgus macaques (100% protection) | Preclinical | T cell response (Cell-mediated immunity) | Genetically stable in vitro | |||
| Reasortant of LASV and MOPV | |||||||||
| Reasortant of LASV and MOPV | ML29 | Whole virus | Guinea pigs (100% protection), NHPs (100% protection) | Preclinical | T cell response (Cell-mediated immunity) | Lethal infection in Stat1−/− mouse | |||
| LUJV | LHF | Not available | |||||||
| Viruses | Diseases | Vaccine Platforms | Name of Vaccine Candidates | Antigen | Animal Experiment | Clinical Trial | Advantage | Disadvantage |
|---|---|---|---|---|---|---|---|---|
| JUNV | AHF | Live-attenuate virus | ||||||
| Candid#1 | Whole virus | Guinea pigs (100% protection), Rhesus macaques (100% protection) | Avaiable in Argentina | Long term immunity | Risk of revertant to high pathogenicity | |||
| Recombinant live-attenuated virus | ||||||||
| Recombinant JUNV Candid#1 with K33S mutaion in GPC | K33S rCan | Whole virus | Guinea pigs (100% protection) | Preclinical | Reduced risk of revertant to high pathogenicity | |||
| Tri-segmented recombinant virus | r3MACV | Whole virus | Guinea pigs (50% protection) | Preclinical | Potential as multivalent vaccine | |||
| Recombinant MOPV with NPExoN and NW arenavirus GPCs | MOPEVACNEW | Whole virus | No data | Preclinical | Potential as multivalent vaccine | |||
| DNA vaccine candidate | ||||||||
| DNA vaccine | DNA vaccine | GPC | No data | Preclinical | Long shelf life | Special equipment requirements | ||
| MACV | BHF | Recombinant live-attenuated virus | ||||||
| Tri-segmented recombinant virus | r3MACV | Whole virus | No data | Preclinical | Potential as multivalent vaccine | Risk of revertant to high pathogenicity | ||
| Recombinant live-attenuated virus | rMACV/Cd#1-GPC | Whole virus | Guinea pigs (100% protection) | Preclinical | Risk of revertant to high pathogenicity | |||
| Recombinant live-attenuated virus | rMACVΔN83/ΔN166/F438I | Whole virus | Guinea pigs (100% protection) | Preclinical | Risk of revertant to high pathogenicity | |||
| Recombinant live-attenuated virus | Car91 | Whole virus | No data (Partially protection in Guinea pigs from GTOV) | Preclinical | Risk of revertant to high pathogenicity | |||
| Recombinant MOPV with NPExoN and MACV GPC | MOPEVACMACV | Whole virus | Cynomolgus macaques (100% protection) | Preclinical | ||||
| Recombinant MOPV with NPExoN and NW arenavirus GPCs | MOPEVACNEW | Whole virus | Cynomolgus macaques (100% protection) | Preclinical | Potential as multivalent vaccine | |||
| DNA vaccine candidate | ||||||||
| Plasmid DNA vaccine encoding MACV GPC | DNA vaccine encoding the MACV GPC | GPC | No data | Preclinical | Long shelf life | Special equipment requirements | ||
| GTOV | VHF | DNA vaccine candidate | ||||||
| Plasmid DNA vaccine encoding GTOV GPC | DNA vaccine encoding the GTOV GPC | GPC | No data | Preclinical | Long shelf life | Special equipment requirements | ||
| Recombinant live-attenuated virus | ||||||||
| Recombinant MOPV with NPExoN and NW arenavirus GPCs | MOPEVACNEW | Whole virus | Cynomolgus macaques (100% protection) | Preclinical | Potential as multivalent vaccine | |||
| SABV | BzHF | Recombinant live-attenuated virus | ||||||
| Recombinant MOPV with NPExoN and NW arenavirus GPCs | MOPEVACNEW | Whole virus | No data | Preclinical | Potential as multivalent vaccine | Need to be verified in animal experiments | ||
| CHAPV | CHF | Recombinant live-attenuated virus | ||||||
| Recombinant MOPV with NPExoN and NW arenavirus GPCs | MOPEVACNEW | Whole virus | No data | Preclinical | Potential as multivalent vaccine | Need to be verified in animal experiments |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, T.; Reyna, R.A.; Taniguchi, S.; Littlefield, K.; Paessler, S.; Maruyama, J. Vaccine Candidates against Arenavirus Infections. Vaccines 2023, 11, 635. https://doi.org/10.3390/vaccines11030635
Saito T, Reyna RA, Taniguchi S, Littlefield K, Paessler S, Maruyama J. Vaccine Candidates against Arenavirus Infections. Vaccines. 2023; 11(3):635. https://doi.org/10.3390/vaccines11030635
Chicago/Turabian StyleSaito, Takeshi, Rachel A. Reyna, Satoshi Taniguchi, Kirsten Littlefield, Slobodan Paessler, and Junki Maruyama. 2023. "Vaccine Candidates against Arenavirus Infections" Vaccines 11, no. 3: 635. https://doi.org/10.3390/vaccines11030635






