Detecting Anatomical Leg Length Discrepancy Using the Plug-in-Gait Model
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Motion Capture
2.3. Imaging
2.4. Data Analysis
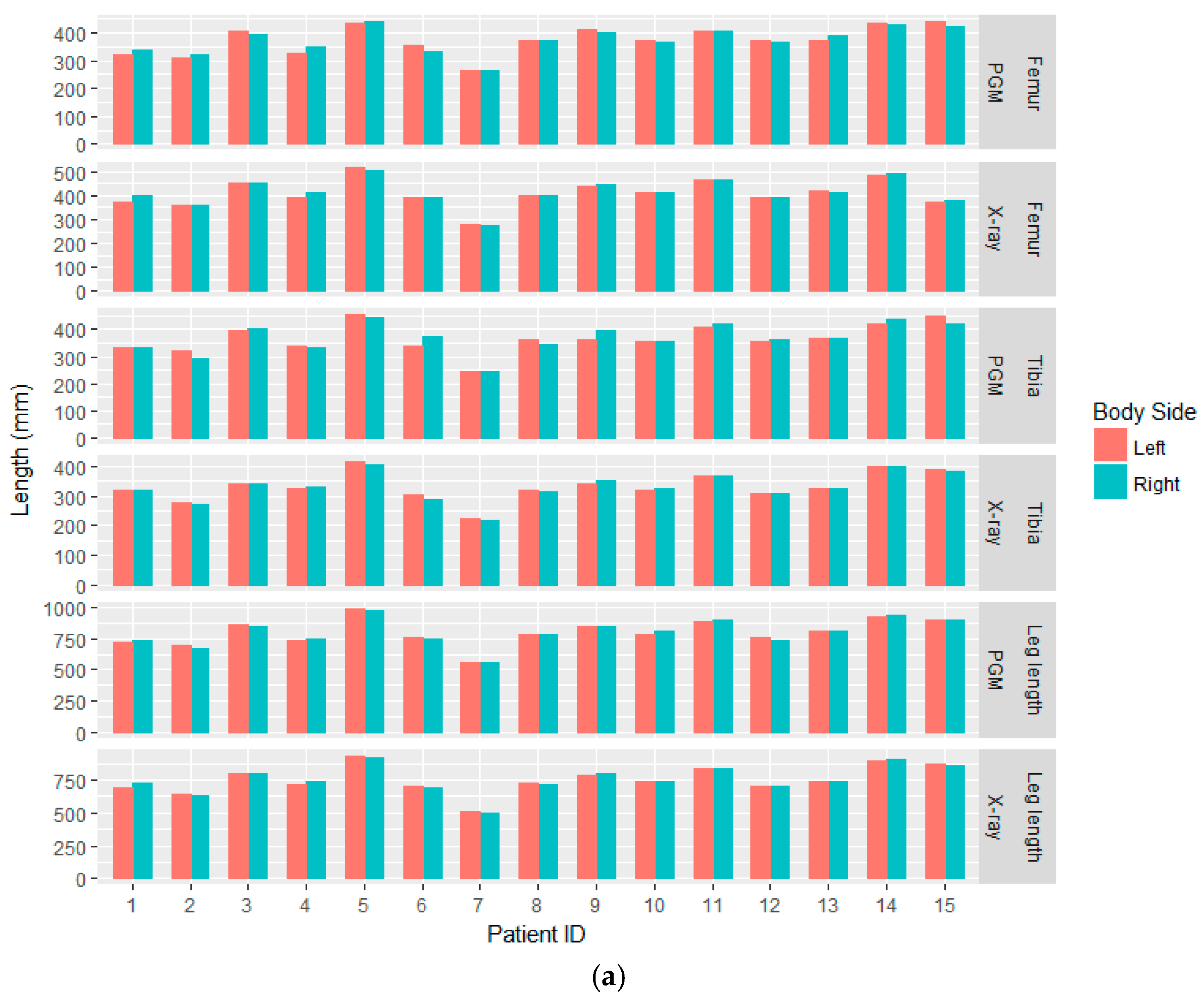
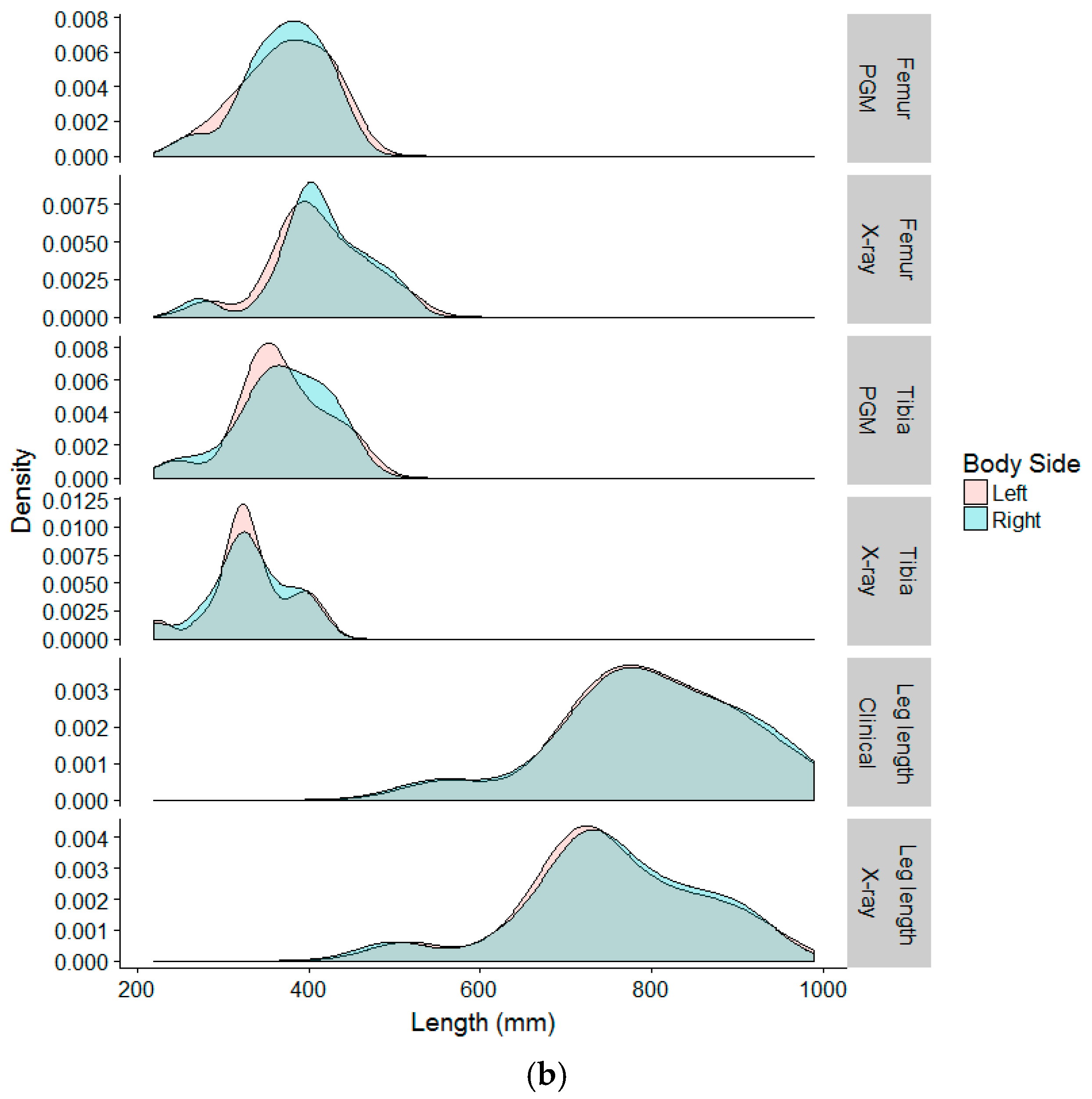
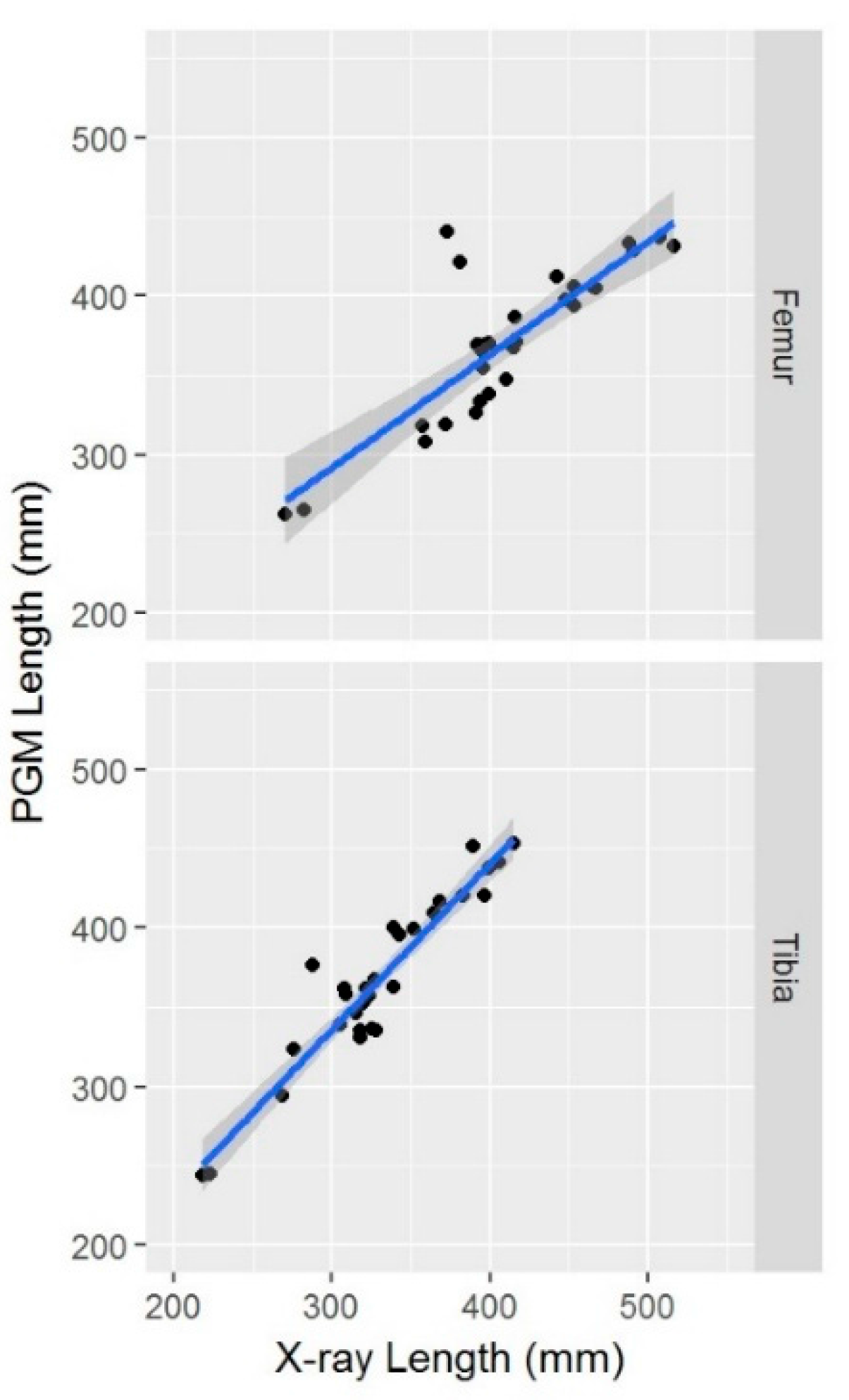
3. Results
4. Discussion
Author Contributions
Conflicts of Interest
References
- Sanhudo, J.A.; Gomes, J.L. Association between leg length discrepancy and posterior tibial tendon dysfunction. Foot Ankle Spec. 2014, 7, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, S.; Huffman, L.K.; Harris, J.G. Limb-length discrepancy as a cause of plantar fasciitis. J. Am. Podiatr. Med. Assoc. 2010, 100, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Vink, P.; Huson, A. Lumbar back muscle activity during walking with a leg inequality. Acta Morphol. Neerlando Scand. 1987, 25, 261–271. [Google Scholar]
- Defrin, R.; Ben Benyamin, S.; Aldubi, R.D.; Pick, C.G. Conservative correction of leg-length discrepancies of 10 mm or less for the relief of chronic low back pain. Arch. Phys. Med. Rehabil. 2005, 86, 2075–2080. [Google Scholar] [CrossRef] [PubMed]
- Raczkowski, J.W.; Daniszewska, B.; Zolynski, K. Functional scoliosis caused by leg length discrepancy. Arch. Med. Sci. 2010, 6, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Harvey, W.F.; Yang, M.; Cooke, T.D.; Segal, N.A.; Lane, N.; Lewis, C.E.; Felson, D.T. Association of leg-length inequality with knee osteoarthritis: A cohort study. Ann. Intern. Med. 2010, 152, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Iversen, M.D.; Chudasama, N.; Losina, E.; Katz, J.N. Influence of self-reported limb length discrepancy on function and satisfaction 6 years after total hip replacement. J. Geriatr. Phys. Ther. 2011, 34, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Fujimaki, H.; Inaba, Y.; Kobayashi, N.; Tezuka, T.; Hirata, Y.; Saito, T. Leg length discrepancy and lower limb alignment after total hip arthroplasty in unilateral hip osteoarthritis patients. J. Orthop. Sci. 2013, 18, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Baylis, W.J.; Rzonca, E.C. Functional and structural limb length discrepancies: Evaluation and treatment. Clin. Podiatr. Med. Surg. 1988, 5, 509–520. [Google Scholar] [PubMed]
- Danbert, R.J. Clinical assessment and treatment of leg length inequalities. J. Manip. Physiol. Ther. 1988, 11, 290–295. [Google Scholar]
- Walsh, M.; Connolly, P.; Jenkinson, A.; O’Brien, T. Leg length discrepancy—An experimental study of compensatory changes in three dimensions using gait analysis. Gait Posture 2000, 12, 156–161. [Google Scholar] [CrossRef]
- Sabharwal, S.; Kumar, A. Methods for assessing leg length discrepancy. Clin. Orthop. Relat. Res. 2008, 466, 2910–2922. [Google Scholar] [CrossRef] [PubMed]
- Baker, R. Gait analysis methods in rehabilitation. J. Neuroeng. Rehabil. 2006, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Tugui, R.D.; Antonescu, D. Cerebral palsy gait, clinical importance. Maedica 2013, 8, 388–393. [Google Scholar] [PubMed]
- Davis, R.B.; Ounpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Sangeux, M.; Peters, A.; Baker, R. Hip joint centre localization: Evaluation on normal subjects in the context of gait analysis. Gait Posture 2011, 34, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Vicon®. Plug-in-Gait Modelling Instructions; Oxford Metrics Ltd.: Oxford, UK, 2015. [Google Scholar]
- Kirtley, C. Sensitivity of the modified Helen Hayes model to marker placement errors. In Proceedings of the Seventh International Symposium on the 3-D Analysis of Human Movement, Newcastle, UK, 10–12 July 2002. [Google Scholar]
- Segev, E.; Hemo, Y.; Wientroub, S.; Ovadia, D.; Fishkin, M.; Steinberg, D.M.; Hayek, S. Intra- and interobserver reliability analysis of digital radiographic measurements for pediatric orthopedic parameters using a novel PACS integrated computer software program. J. Child. Orthop. 2010, 4, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, S.; Zhao, C.; McKeon, J.; Melaghari, T.; Blacksin, M.; Wenekor, C. Reliability analysis for radiographic measurement of limb length discrepancy: Full-length standing anteroposterior radiograph versus scanogram. J. Pediatr. Orthop. 2007, 27, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Leigh, R.J.; Pohl, M.B.; Ferber, R. Does tester experience influence the reliability with which 3D gait kinematics are collected in healthy adults? Phys. Ther. Sport 2014, 15, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, J.; Hebron, J.; Taylor, P.J. The influence of tester experience on the reliability of 3D kinematic information during running. Gait Posture 2014, 40, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Krumm, D.; Cockcroft, J.; Zaumseil, F.; Odenwald, S.; Milani, T.L.; Louw, Q. Analytical evaluation of the effects of inconsistent anthropometric measurements on joint kinematics in motion capturing. Gait Posture 2016, 46, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Dempster, W.T.; Gabel, W.C.; Felts, W.J. The anthropometry of the manual work space for the seated subject. Am. J. Phys. Anthropol. 1959, 17, 289–317. [Google Scholar] [CrossRef] [PubMed]
- Kainz, H.; Carty, C.P.; Modenese, L.; Boyd, R.N.; Lloyd, D.G. Estimation of the hip joint centre in human motion analysis: A systematic review. Clin. Biomech. 2015, 30, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Leardini, A.; Cappozzo, A.; Catani, F.; Toksvig-Larsen, S.; Petitto, A.; Sforza, V.; Cassanelli, G.; Giannini, S. Validation of a functional method for the estimation of hip joint centre location. J. Biomech. 1999, 32, 99–103. [Google Scholar] [CrossRef]
- Assi, A.; Sauret, C.; Massaad, A.; Bakouny, Z.; Pillet, H.; Skalli, W.; Ghanem, I. Validation of hip joint center localization methods during gait analysis using 3D EOS imaging in typically developing and cerebral palsy children. Gait Posture 2016, 48, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Stagni, R.; Leardini, A.; Cappozzo, A.; Grazia Benedetti, M.; Cappello, A. Effects of hip joint centre mislocation on gait analysis results. J. Biomech. 2000, 33, 1479–1487. [Google Scholar] [CrossRef]
- Kiernan, D.; Malone, A.; O’Brien, T.; Simms, C.K. The clinical impact of hip joint centre regression equation error on kinematics and kinetics during paediatric gait. Gait Posture 2015, 41, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Kainz, H.; Carty, C.P.; Maine, S.; Walsh, H.P.J.; Lloyd, D.G.; Modenese, L. Effects of hip joint centre mislocation on gait kinematics of children with cerebral palsy calculated using patient-specific direct and inverse kinematic models. Gait Posture 2017, 57, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Thewlis, D.; Richards, J.; Bower, J. Discrepancies in knee joint moments using common anatomical frames defined by different palpable landmarks. J. Appl. Biomech. 2008, 24, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, J.; Hebron, J.; Taylor, P.J. The test-retest reliability of knee joint center location techniques. J. Appl. Biomech. 2015, 31, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.P.; Gibbs, S.; Arnold, G.; Abboud, R.; Wang, W. A method to calculate the centre of the ankle joint: A comparison with the Vicon Plug-in-Gait model. Clin. Biomech. 2010, 25, 582–587. [Google Scholar] [CrossRef] [PubMed]

| Segment | Left (Mean) | Right (Mean) | Mean Discrepancy (SD) | Significance |
|---|---|---|---|---|
| PGM Femur length | 372 | 371 | 0.66 (13.17) | p = 0.30 |
| X-ray Femur length | 410 | 413 | −2.93 (9.63) | |
| PGM Tibia length | 367 | 368 | −1.60 (19.42) | p = 0.45 |
| X-ray Tibia length | 331 | 329 | 2.06 (7.01) | |
| X-ray total leg length | 753 | 754 | −1.0 (14.71) | p = 0.2 |
| Clinical leg length | 802 | 799 | 2.33 (14.12) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khamis, S.; Danino, B.; Springer, S.; Ovadia, D.; Carmeli, E. Detecting Anatomical Leg Length Discrepancy Using the Plug-in-Gait Model. Appl. Sci. 2017, 7, 926. https://doi.org/10.3390/app7090926
Khamis S, Danino B, Springer S, Ovadia D, Carmeli E. Detecting Anatomical Leg Length Discrepancy Using the Plug-in-Gait Model. Applied Sciences. 2017; 7(9):926. https://doi.org/10.3390/app7090926
Chicago/Turabian StyleKhamis, Sam, Barry Danino, Shmuel Springer, Dror Ovadia, and Eli Carmeli. 2017. "Detecting Anatomical Leg Length Discrepancy Using the Plug-in-Gait Model" Applied Sciences 7, no. 9: 926. https://doi.org/10.3390/app7090926
APA StyleKhamis, S., Danino, B., Springer, S., Ovadia, D., & Carmeli, E. (2017). Detecting Anatomical Leg Length Discrepancy Using the Plug-in-Gait Model. Applied Sciences, 7(9), 926. https://doi.org/10.3390/app7090926





