Clinical Neurophysiological Methods Verify Improvement in the Motor Neural Transmission in Patients with Surgically Treated Idiopathic Scoliosis in Long-Term Follow-up
Abstract
:1. Introduction
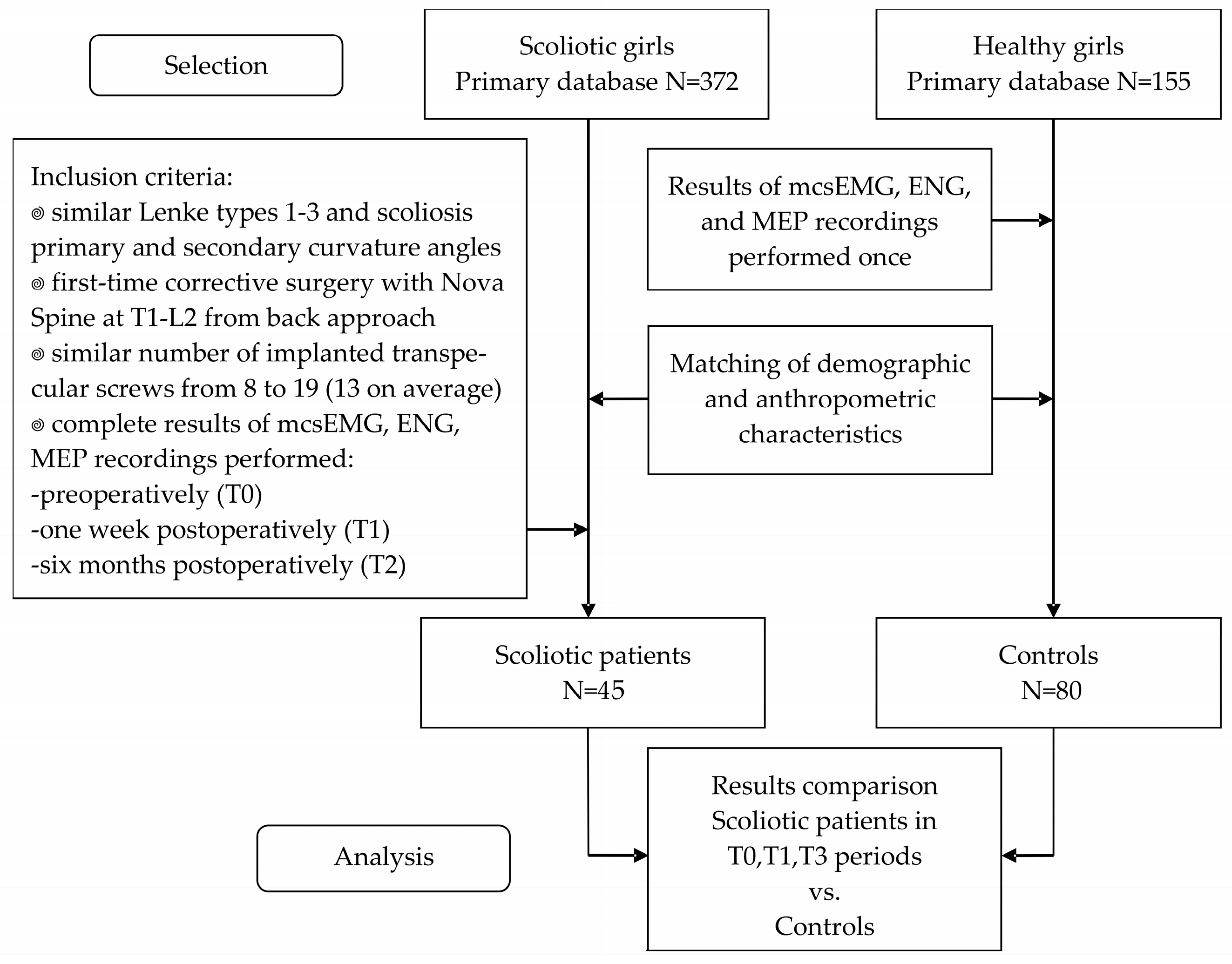
2. Materials and Methods
2.1. Participants and Study Protocol
2.2. Treatment
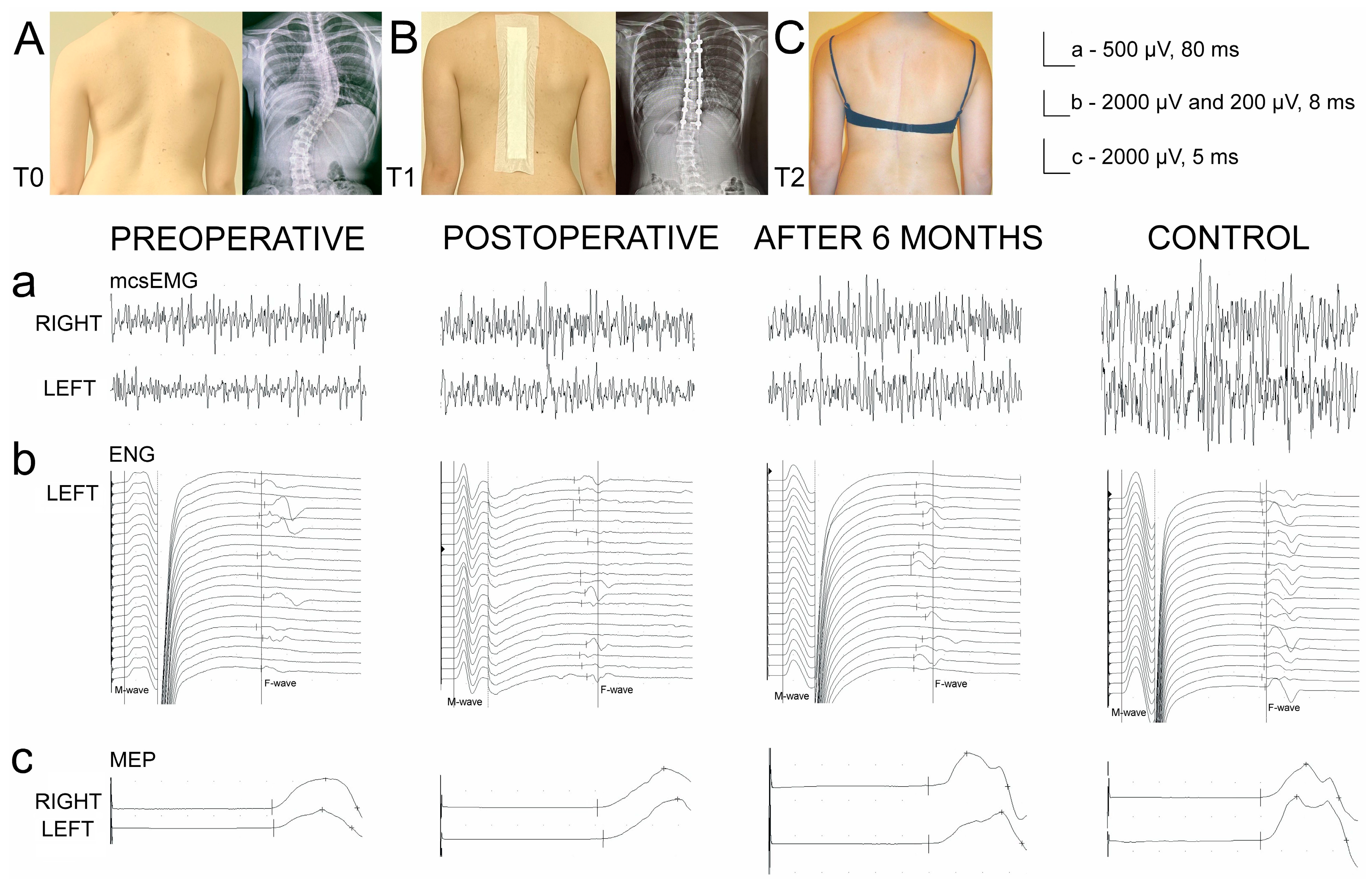
2.3. Neurophysiological Recordings
2.4. Statistical Analysis
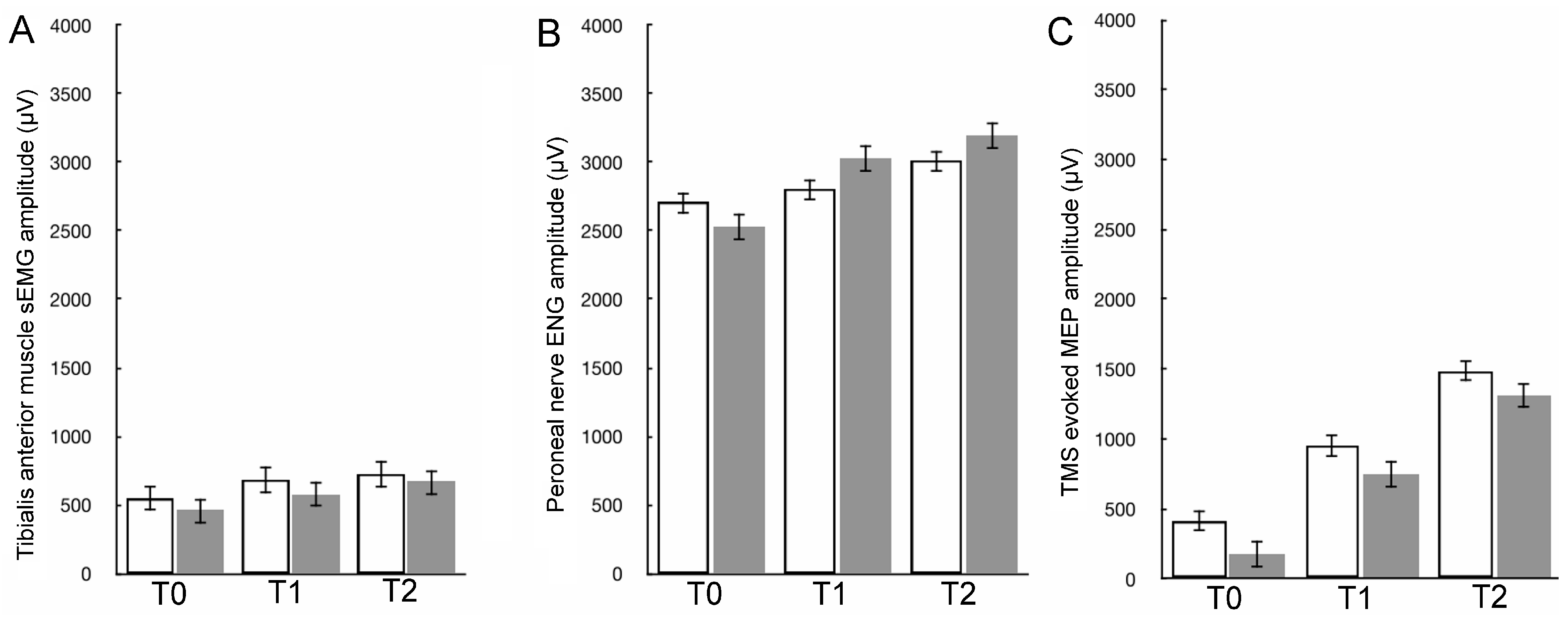
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burwell, R.G.; Dangerfield, P.H.; Lowe, T.G.; Margulies, J.Y. (Eds.) Etiology of Adolescent Idiopathic Scoliosis: Current Trends and Relevance to New Treatment Approaches, State of the Art Reviews; Hanley & Belfus, Incorporated: Philadelphia, PA, USA, 2000; ISBN 1560533331/9781560533337. [Google Scholar]
- Lowe, T.G.; Edgar, M.; Margulies, J.Y.; Miller, N.H.; Raso, V.J.; Reinker, K.A.; Rivard, C.H. Etiology of idiopathic scoliosis: Current trends in research. J. Bone Jt. Surg. 2000, 82, 1157–1168. [Google Scholar] [CrossRef] [PubMed]
- Hawes, M.C.; O’Brien, J.P. The transformation of spinal curvature into spinal deformity: Pathological processes and implications for treatment. Scoliosis 2000, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Huber, J.; Rogala, P. Etiopathogenesis of the adolescent idiopathic scoliosis based on neuroimaging and neurophysiological examinations with the special emphasis on motor evoked potentials (MEP). Stud. Health Technol. Inform. 2012, 176, 446. [Google Scholar]
- Gupta, P.; Lenke, L.G.; Bridwell, K.H. Incidence of neural axis abnormalities in infantile and juvenile patients with spinal deformity. Is a magnetic resonance image screening necessary? Spine 1998, 23, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Winter, R.B.; Lonstein, J.E.; Heithoff, K.B.; Kirkham, J.A. Magnetic resonance imaging evaluation of the adolescent patient with idiopathic scoliosis before spinal instrumentation and fusion. A prospective, double-blinded study of 140 patients. Spine 1997, 22, 855–858. [Google Scholar] [CrossRef] [PubMed]
- Daroszewski, P.; Huber, J.; Kaczmarek, K.; Janusz, P.; Główka, P.; Tomaszewski, M.; Domagalska, M.; Kotwicki, T. Comparison of Motor Evoked Potentials Neuromonitoring Following Pre- and Postoperative Transcranial Magnetic Stimulation and Intraoperative Electrical Stimulation in Patients Undergoing Surgical Correction of Idiopathic Scoliosis. J. Clin. Med. 2023, 12, 6312. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Antonini, G.; Carabalona, R.; Minozzi, S. Physical exercises as a treatment for adolescent idiopathic scoliosis. A systematic review. Pediatr. Rehabil. 2003, 6, 227–235. [Google Scholar] [CrossRef]
- Addai, D.; Zarkos, J.; Bowey, A.J. Current concepts in the diagnosis and management of adolescent idiopathic scoliosis. Child’s Nerv. Syst. 2020, 36, 1111–1119. [Google Scholar] [CrossRef]
- Negrini, S.; Minozzi, S.; Bettany-Saltikov, J.; Zaina, F.; Chockalingam, N.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Romano, M.; Vasiliadis, E.S. Braces for idiopathic scoliosis in adolescents. Spine 2010, 35, 1285–1293. [Google Scholar] [CrossRef]
- Diebo, B.G.; Segreto, F.A.; Solow, M.; Messina, J.C.; Paltoo, K.; Burekhovich, S.A.; Bloom, L.R.; Cautela, F.S.; Shah, N.V. Adolescent idiopathic scoliosis care in an underserved inner-city population: Screening, bracing, and patient- and parent-reported outcomes. Spine Deform. 2019, 17 (Suppl. S10), S213. [Google Scholar] [CrossRef]
- Kelly, J.; Shah, N.; Freetly, T.; Dekis, J.; Hariri, O.; Walker, S.; Borrelli, J.; Post, N.H.; Diebo, B.G.; Urban, W.P.; et al. Treatment of adolescent idiopathic scoliosis and evaluation of the adolescent patient. Curr. Orthop. Pract. 2018, 29, 424–429. [Google Scholar] [CrossRef]
- Pepke, W.; Morani, W.; Schiltenwolf, M.; Bruckner, T.; Renkawitz, T.; Hemmer, S.; Akbar, M. Outcome of Conservative Therapy of Adolescent Idiopathic Scoliosis (AIS) with Chêneau-Brace. J. Clin. Med. 2023, 12, 2507. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Aulisa, L.; Ferraro, C.; Fraschini, P.; Masiero, S.; Simonazzi, P.; Tedeschi, C.; Venturin, A. Italian guidelines on rehabilitation treatment of adolescents with scoliosis or other spinal deformities. Eur. Med. 2005, 41, 183–201. [Google Scholar]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Diebo, B.G.; Segreto, F.A.; Mixa, P.J.; Day, L.M.; Kaur, H.; Burekhovich, S.A.; Lavian, J.D.; Beyer, G.; Challier, V.; Naziri, Q.; et al. P84—Adolescent Idiopathic Scoliosis Care in an Underserved Inner-City Population: Screening, Bracing, Patients’ and Parents’ Reported Outcomes. Spine J. 2017, 17, S213. [Google Scholar] [CrossRef]
- Patel, P.N.; Upasani, V.V.; Bastrom, T.P.; Marks, M.C.; Pawelek, J.B.; Betz, R.R.; Lenke, L.G.; Newton, P.O. Spontaneous lumbar curve correction in selective thoracic fusions of idiopathic scoliosis: A comparison of anterior and posterior approaches. Spine 2008, 33, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- Luk, K.D.K.; Vidyadhara, S.; Lu, D.S.; Wong, Y.W.; Cheung, W.Y.; Cheung, K.M.C. Coupling between sagittal and frontal plane deformity correction in idiopathic thoracic scoliosis and its relationship with postoperative sagittal alignment. Spine 2010, 35, 1158–1164. [Google Scholar] [CrossRef]
- Kwan, M.K.; Loh, K.W.; Chung, W.H.; Hasan, M.S.; Chan, C.Y.W. Perioperative outcome and complications following single-staged posterior spinal fusion using pedicle screw instrumentation in adolescent idiopathic scoliosis(AIS): A review of 1057 cases from a single centre. BMC Musculoskelet. Disord. 2021, 22, 413. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.; Hwang, S.W.; Tataryn, Z.; Samdani, A.F. Neuromonitoring changes in pediatric spinal deformity surgery: A single-institution experience. J. Neurosurg. Pediatr. 2014, 13, 247–254. [Google Scholar] [CrossRef]
- Ozturk, C.; Karadereler, S.; Ornek, I.; Enercan, M.; Ganiyusufoglu, K.; Hamzaoglu, A. The role of routine magnetic resonance imaging in the preoperative evaluation of adolescent idiopathic scoliosis. Int. Orthop. 2010, 34, 543–546. [Google Scholar] [CrossRef]
- Scaramuzzo, L.; Giudici, F.; Archetti, M.; Minoia, L.; Zagra, A.; Bongetta, D. Clinical relevance of preoperative MRI in adolescent idiopathic scoliosis: Is hydromyelia a predictive factor of intraoperative electrophysiological monitoring alterations? Clin. Spine Surg. 2019, 32, E183–E187. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Chen, Y.; Shao, J.; Zhoutian, J.; Wang, F.; Chen, Z.; Li, M. Long-Term Follow-up of Posterior Selective Thoracolumbar/Lumbar Fusion in Patients With Lenke 5C Adolescent Idiopathic Scoliosis: An Analysis of 10-Year Outcomes. Glob. Spine J. 2022, 12, 840–850. [Google Scholar] [CrossRef] [PubMed]
- Ghandhari, H.; Ameri, E.; Nikouei, F.; Mahdavi, S.M.; Chehrassan, M.; Motalebi, M. Selective Thoracolumbar/Lumbar Fusion in Adolescent Idiopathic Scoliosis: A Comprehensive Review of the Literature. Arch. Bone Jt. Surg. 2023, 11, 313–320. [Google Scholar]
- Pastorelli, F.; Di Silvestre, M.; Plasmati, R.; Michelucci, R.; Greggi, T.; Morigi, A.; Bacchin, M.R.; Bonarelli, S.; Cioni, A.; Vommaro, F.; et al. The prevention of neural complications in the surgical treatment of scoliosis: The role of the neurophysiological intraoperative monitoring. Eur. Spine J. 2011, 20, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Daroszewski, P.; Garasz, A.; Huber, J.; Kaczmarek, K.; Janusz, P.; Główka, P.; Tomaszewski, M.; Kotwicki, T. Update on neuromonitoring procedures applied during surgery of the spine—Observational study. Reumatologia 2023, 61, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- MacDonald, D.B. Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. J. Clin. Neurophysiol. 2002, 19, 416–429. [Google Scholar] [CrossRef]
- Kaczmarek, A.M.; Huber, J.; Leszczyńska, K.; Wietrzak, P.; Kaczmarek, K. Relationships between the Clinical Test Results and Neurophysiological Findings in Patients with Thoracic Outlet Syndrome. Bioengineering 2022, 9, 598. [Google Scholar] [CrossRef] [PubMed]
- Wesołek, A.; Daroszewski, P.; Huber, J. Neurophysiological Evaluation of the Functional State of Muscular and Nervous Systems in High-Maneuvering Jet Fighters. Appl. Sci. 2023, 13, 1120. [Google Scholar] [CrossRef]
- Leszczyńska, K.; Huber, J. Unveiling the Correlations between Clinical Assessment of Spasticity and Muscle Strength and Neurophysiological Testing of Muscle Activity in Incomplete Spinal Cord Injury Patients: The Importance of a Comprehensive Evaluation. Appl. Sci. 2023, 13, 7609. [Google Scholar] [CrossRef]
- Huber, J.; Leszczyńska, K.; Wincek, A.; Szymankiewicz-Szukała, A.; Fortuna, W.; Okurowski, S.; Tabakow, P. The Role of Peripheral Nerve Electrotherapy in Functional Recovery of Muscle Motor Units in Patients after Incomplete Spinal Cord Injury. Appl. Sci. 2021, 11, 9764. [Google Scholar] [CrossRef]
- Wiertel-Krawczuk, A.; Huber, J.; Szymankiewicz-Szukała, A.; Wincek, A. Neurophysiological Evaluation of Neural Transmission in Brachial Plexus Motor Fibers with the Use of Magnetic versus Electrical Stimuli. Sensors 2023, 23, 4175. [Google Scholar] [CrossRef] [PubMed]
- Wincek, A.; Huber, J.; Leszczyńska, K.; Fortuna, W.; Okurowski, S.; Chmielak, K.; Tabakow, P. The Long-Term Effect of Treatment Using the Transcranial Magnetic Stimulation rTMS in Patients after Incomplete Cervical or Thoracic Spinal Cord Injury. J. Clin. Med. 2021, 10, 2975. [Google Scholar] [CrossRef] [PubMed]
- Leszczyńska, K.; Huber, J. Comparing Parameters of Motor Potentials Recordings Evoked Transcranially with Neuroimaging Results in Patients with Incomplete Spinal Cord Injury: Assessment and Diagnostic Capabilities. Biomedicines 2023, 11, 2602. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.H.; Park, Y.G.; Kim, D.H.; Yoon, S.Y. Monitoring of Motor and Somatosensory Evoked Potentials During Spine Surgery: Intraoperative Changes and Postoperative Outcomes. Ann. Rehabil. Med. 2016, 40, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Kimiskidis, V.K.; Potoupnis, M.; Papagiannopoulos, S.K.; Dimopoulos, G.; Kazis, D.A.; Markou, K.; Zara, F.; Kapetanos, G.; Kazis, A.D. Idiopathic scoliosis: A transcranial magnetic stimulation study. J. Musculoskelet. Neuronal Interact. 2007, 7, 155–160. [Google Scholar]
- Lo, Y.L.; Dan, Y.F.; Tan, Y.E.; Tan, C.T.; Raman, S. Intra-operative monitoring in scoliosis surgery with multi-pulse cortical stimuli and desflurane anesthesia. Spinal Cord 2004, 42, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, H.L.; Paloheimo, M.P., Jr.; Backman, M.H.; Johnson, J.R.; Holt, R.T.; Shields, C.B. Transcranial magnetic motor evoked potentials (tcMMEP) for functional monitoring of motor pathways during scoliosis surgery. Spine 1989, 14, 683–686. [Google Scholar] [CrossRef] [PubMed]
- Gadella, M.C.; Dulfer, S.E.; Absalom, A.R.; Lange, F.; Scholtens-Henzen, C.H.; Groen, R.J.; Wapstra, F.H.; Faber, C.; Tamási, K.; Sahinovic, M.M.; et al. Comparing Motor-Evoked Potential Characteristics of Needle versus Surface Recording Electrodes during Spinal Cord Monitoring-The NERFACE Study Part I. J. Clin. Med. 2023, 12, 1404. [Google Scholar] [CrossRef]
- Dulfer, S.E.; Gadella, M.C.; Tamási, K.; Absalom, A.R.; Lange, F.; Scholtens-Henzen, C.H.; Faber, C.; Wapstra, F.H.; Groen, R.J.; Sahinovic, M.M.; et al. Use of Needle Versus Surface Recording Electrodes for Detection of Intraoperative Motor Warnings: A Non-Inferiority Trial. The NERFACE Study Part II. J. Clin. Med. 2023, 12, 1753. [Google Scholar] [CrossRef] [PubMed]

| Variable Group of Subjects | Age (years) | Height (cm) | Weight (kg) | BMI | Scoliosis Type | Cobb’s Angle |
|---|---|---|---|---|---|---|
| Patients N = 45 ♀ | 9–17 14.8 ± 1.7 | 135–180 164.1 ± 2.5 | 28–82 52.7 ± 3.7 | 17.1–30.2 22.8 ± 4.3 | Lenke 1 = 12 Lenke 2 = 26 Lenke 3 = 7 | Primary 42–89 58.4 ± 5.8 Secondary 29–48 35.2 ± 3.8 |
| Healthy volunteers Controls N = 80 ♀ | 8–17 13.9 ± 1.9 | 133–182 166.9 ± 2.3 | 28–85 53.1 ± 6.0 | 17.5–29.5 22.4 ± 3.5 | NA | NA |
| p-value | 0.228 NS | 0.293 NS | 0.232 NS | 0.271 NS |
| Test Parameter | Side | Control | Scoliosis Side | Patients Preoperative T0 (1 Day before Surgery) | Control vs. Patients Preoperative T0 | Patients Postoperative T1 (1 Week After Surgery) | Control vs. Patients Postoperative T1 | Patients Postoperative T2 (6 Months After Surgery) | Control vs. Patients Postoperative T2 | Patients Preoperative T0 vs. Postoperative T1 | Patients Preoperative T0 vs. Postoperative T2 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Min.–Max. Mean ± SD | Min.–Max. Mean ± SD | p-Value | Min.–Max. Mean ± SD | p-Value | Min.–Max. Mean ± SD | p-Value | p-Value | p-Value | |||
| Tibialis anterior muscle electromyography during maximal contraction (mcsEMG) | |||||||||||
| Amplitude (µV) | R | 600–2600 890.6 ± 104.2 | Convex | 300–2500 548.2 ± 95.4 | 0.037 | 300–2650 677.3 ± 94.8 | 0.042 | 400–2700 725.5 ± 93.3 | 0.046 | 0.044 | 0.039 |
| L | 600–2550 887.8 ± 91.5 | Concave | 260–2500 453.1 ± 82.1 | 0.031 | 250–2550 572.1 ± 91.9 | 0.041 | 200–1950 663.1 ± 92.0 | 0.043 | 0.046 | 0.040 | |
| p-value | R vs. L | 0.327 | Convex vs. concave | 0.049 | NA | 0.050 | NA | 0.051 | NA | NA | NA |
| FI (3-0) | R | 3.0–3.0 3.0 | Convex | 3.0–1.0 2.3 ± 0.4 | 0.032 | 3.0–1.0 2.4 ± 0.3 | 0.031 | 3.0–2.0 2.8 ± 0.4 | 0.045 | 0.054 | 0.035 |
| L | 3.0–3.0 3.0 | Concave | 3.0–1.0 2.2 ± 0.5 | 0.025 | 3.0–1.0 2.3 ± 0.5 | 0.026 | 3.0–2.0 2.7 ± 0.4 | 0.044 | 0.061 | 0.031 | |
| p-value | R vs. L | NS | Convex vs. concave | 0.046 | NA | 0.045 | NA | 0.045 | NA | NA | NA |
| Peroneal nerve ENG recorded in the extensor digitorum brevis muscle after stimulation at the ankle | |||||||||||
| M-wave Amplitude (µV) | R | 3000–12,500 6760.1 ± 965.1 | Convex | 1500–9800 2702.1 ± 353.1 | 0.007 | 1400–10,500 2804.1 ± 362.7 | 0.008 | 1400–11,000 3011.3 ± 332.0 | 0.009 | 0.041 | 0.036 |
| L | 3000–11,600 6558.4 ± 877.3 | Concave | 1400–9800 2525.3 ± 422.5 | 0.008 | 1500–10,000 3025.4 ± 421.9 | 0.009 | 1400–1050 3191.4 ± 406.7 | 0.011 | 0.036 | 0.033 | |
| p-value | R vs. L | 0.228 | Convex vs. concave | 0.050 | NA | 0.048 | NA | 0.049 | NA | NA | NA |
| M-wave Latency (ms) | R | 3.2–5.4 4.5 ± 1.1 | Convex | 3.2–6.4 5.3 ± 1.4 | 0.042 | 3.5–6.6 5.3 ± 1.3 | 0.041 | 3.2–6.3 4.6 ± 1.3 | 0.068 | 0.167 | 0.039 |
| L | 3.3–5.5 4.6 ± 1.1 | Concave | 3.5–6.5 5.5 ± 1.3 | 0.034 | 3.5–6.6 5.1 ± 1.4 | 0.037 | 3.3–6.2 4.7 ± 1.4 | 0.075 | 0.049 | 0.042 | |
| p-value | R vs. L | 0.328 | Convex vs. concave | 0.048 | NA | 0.046 | NA | 0.061 | NA | NA | NA |
| F-wave Frequency (x/20 M-waves) | R | 14–20 17.5 ± 1.3 | Convex | 10–16 12.1 ± 1.5 | 0.043 | 11–19 14.0 ± 1.4 | 0.048 | 12–18 15.6 ± 1.3 | 0.055 | 0.048 | 0.045 |
| L | 14–20 17.8 ± 1.4 | Concave | 8–15 11.1 ± 1.5 | 0.042 | 11–17 13.9 ± 1.3 | 0.046 | 12–17 14.8 ± 1.4 | 0.052 | 0.048 | 0.045 | |
| p-value | R vs. L | 0.318 | Convex vs. concave | 0.050 | NA | 0.074 | NA | 0.061 | NA | NA | NA |
| M–F waves Inter-latency (ms) | R | 38.6–49.2 44.4 ± 2.2 | Convex | 39.1–57.3 50.4 ± 2.7 | 0.045 | 38.2–57.3 48.9 ± 2.4 | 0.048 | 38.5–49.0 45.1 ± 2.1 | 0.062 | 0.049 | 0.038 |
| L | 38.0–49.4 44.7 ± 2.3 | Concave | 40.1–59.8 53.7 ± 2.2 | 0.031 | 38.1–56.9 48.4 ± 2.7 | 0.047 | 38.3–51.3 47.1 ± 2.8 | 0.047 | 0.047 | 0.046 | |
| p-value | R vs. L | 0.481 | Convex vs. concave | 0.046 | NA | 0.138 | NA | 0.045 | NA | NA | NA |
| TMS-induced MEPs recorded in tibialis anterior muscle | |||||||||||
| Amplitude (µV) | R | 1200–3550 1697.2 ± 96.6 | Convex | 300–1350 412.5 ± 92.1 | 0.010 | 600–2500 953.1 ± 95.2 | 0.027 | 950–2850 1488.3 ± 98.4 | 0.046 | 0.034 | 0.018 |
| L | 1000–2950 1609.1 ± 78.6 | Concave | 250–1150 181.4 ± 66.1 | 0.009 | 400–1800 749.3 ± 88.2 | 0.019 | 800–2700 1312.7 ± 87.2 | 0.041 | 0.032 | 0.019 | |
| p-value | R vs. L | 0.291 | Convex vs. concave | 0.036 | NA | 0.043 | NA | 0.048 | NA | NA | NA |
| Latency (ms) | R | 24.9–31.9 28.7 ± 1.3 | Convex | 27.6–36.1 32.1 ± 2.2 | 0.036 | 28.9–39.1 31.7 ± 2.8 | 0.044 | 25.7–34.2 29.3 ± 2.4 | 0.072 | 0.059 | 0.045 |
| L | 25.3–32.3 29.1 ± 1.4 | Concave | 28.4–37.8 32.8 ± 2.4 | 0.039 | 30.5–41.0 33.6 ± 2.6 | 0.037 | 26.8–35.3 29.9 ± 2.3 | 0.064 | 0.056 | 0.047 | |
| p-value | R vs. L | 0.271 | Convex vs. concave | 0.064 | NA | 0.049 | NA | 0.066 | NA | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daroszewski, P.; Huber, J.; Kaczmarek, K.; Janusz, P.; Główka, P.; Tomaszewski, M.; Kubaszewski, Ł.; Dąbrowski, M.; Kotwicki, T. Clinical Neurophysiological Methods Verify Improvement in the Motor Neural Transmission in Patients with Surgically Treated Idiopathic Scoliosis in Long-Term Follow-up. Appl. Sci. 2024, 14, 4105. https://doi.org/10.3390/app14104105
Daroszewski P, Huber J, Kaczmarek K, Janusz P, Główka P, Tomaszewski M, Kubaszewski Ł, Dąbrowski M, Kotwicki T. Clinical Neurophysiological Methods Verify Improvement in the Motor Neural Transmission in Patients with Surgically Treated Idiopathic Scoliosis in Long-Term Follow-up. Applied Sciences. 2024; 14(10):4105. https://doi.org/10.3390/app14104105
Chicago/Turabian StyleDaroszewski, Przemysław, Juliusz Huber, Katarzyna Kaczmarek, Piotr Janusz, Paweł Główka, Marek Tomaszewski, Łukasz Kubaszewski, Mikołaj Dąbrowski, and Tomasz Kotwicki. 2024. "Clinical Neurophysiological Methods Verify Improvement in the Motor Neural Transmission in Patients with Surgically Treated Idiopathic Scoliosis in Long-Term Follow-up" Applied Sciences 14, no. 10: 4105. https://doi.org/10.3390/app14104105






