Development of a Biocontrol Method Applying Bacteriophage-Containing Aerosol against Mycobacterium tuberculosis Using the Bacteriophage BTCU-1 and M. smegmatis as Models
Abstract
:1. Introduction
2. Materials and Methods
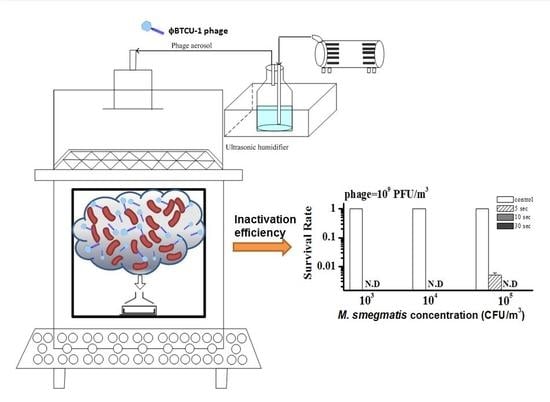
2.1. Phase One: Phage Aerosol against Airborne M. smegmatis
2.1.1. Bacterial Host Strain and Culture
2.1.2. Phage Preparation
2.1.3. Effect of Temperature on ϕBTCU-1 Stability
2.1.4. M. smegmatis Aerosol Preparation and Test System
2.1.5. Test Sampler and Sample Processing
2.1.6. Calculation of the CR Value for Air Sampling of M. smegmatis
2.1.7. Generation of Phage Aerosols against Airborne M. smegmatis
2.2. Phase Two: Phage Aerosol against M. smegmatis Colonies on an Agar Surface
2.3. Statistical Analysis
3. Results
3.1. Effect of Temperature on ϕBTCU-1 Stability
3.2. Collection Efficiency of Tested Bioaerosol Samplers
3.3. Reduction of Airborne M. smegmatis by ϕBTCU-1 Aerosols
3.4. Bactericidal Effect of ϕBTCU-1 Aerosols on M. smegmatis Colonies on an Agar Surface
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Taiwan Centers for Disease Control. Taiwan Tuberculosis Control Report 2016. Available online: https://www.cdc.gov.tw/uploads/files/201712/2bf81c5a-4812-4977-9c02-388aadba77a7.pdf (accessed on 2 August 2019).
- Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report (MMWR). Available online: https://www.cdc.gov/mmwr/volumes/66/wr/mm6611a2.htm (accessed on 2 August 2019).
- Chen, P.S.; Li, C.S. Concentration profiles of airborne Mycobacterium tuberculosis in a hospital. Aerosol Sci. Technol. 2008, 42, 194–200. [Google Scholar] [CrossRef]
- Canada Government. Pathogen Safety Data Sheets: Infectious Substances-Mycobacterium Tuberculosis and Mycobacterium Tuberculosis Complex. Available online: https://www.canada.ca/en/public-health/services/laboratory-biosafety-biosecurity/pathogen-safety-data-sheets-risk-assessment/mycobacterium-tuberculosis-complex.html (accessed on 2 August 2019).
- Xu, P.; Kujundzic, E.; Peccia, J.; Schafer, M.P.; Moss, G.; Hernandez, M.; Miller, S.L. Impact of environmental factors on efficacy of upper-room air ultraviolet germicidal irradiation for inactivating airborne mycobacteria. Environ. Sci. Technol. 2005, 39, 9656–9664. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Peccia, J.; Fabian, P.; Martyny, J.W.; Fennelly, K.P.; Hernandez, M.; Miller, S.L. Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivating airborne bacterial spores and mycobacteria in full-scale studies. Atmos. Environ. 2003, 37, 405–419. [Google Scholar] [CrossRef]
- Schmidt, C. Phage therapy’s latest makeover. Nat. Biotechnol. 2019, 37, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Broxmeyer, L.; Sosnowska, D.; Miltner, E.; Chacón, O.; Wagner, D.; McGarvey, J.; Barletta, R.G.; Bermudez, L.E. Killing of Mycobacterium avium and Mycobacterium tuberculosis by a mycobacteriophage delivered by a nonvirulent mycobacterium: A model for phage therapy of intracellular bacterial pathogens. J. Infect. Dis. 2002, 186, 1155–1160. [Google Scholar] [CrossRef] [PubMed]
- Danelishvili, L.; Young, L.S.; Bermudez, L.E. In vivo efficacy of phage therapy for Mycobacterium avium infection as delivered by a nonvirulent mycobacterium. Microb. Drug Resist. 2006, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Yang, W.; Dong, X.; Cong, L.; Li, N.; Li, Y.; Wen, Z.; Yin, Z.; Lan, Z.; Li, W. Inhalation study of mycobacteriophage D29 aerosol for mice by endotracheal route and nose-only exposure. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 393–405. [Google Scholar] [CrossRef]
- Guenther, S.; Huwyler, D.; Richard, S.; Loessner, M.J. Virulent bacteriophage for efficient biocontrol of Listeria monocytogenes in ready-to-eat foods. Appl. Environ. Microbiol. 2009, 75, 93–100. [Google Scholar] [CrossRef]
- Hudson, J.; Billington, C.; Carey-Smith, G.; Greening, G. Bacteriophages as biocontrol agents in food. J. Food Prot. 2005, 68, 426–437. [Google Scholar] [CrossRef]
- Chen, L.K.; Liu, Y.L.; Hu, A.; Chang, K.C.; Lin, N.T.; Lai, M.J.; Tseng, C.C. Potential of bacteriophage ΦAB2 as an environmental biocontrol agent for the control of multidrug-resistant Acinetobacter baumannii. BMC Microbiol. 2013, 13, 154. [Google Scholar] [CrossRef]
- Ho, Y.H.; Tseng, C.C.; Wang, L.S.; Chen, Y.T.; Ho, G.J.; Lin, T.Y.; Wang, L.Y.; Chen, L.K. Application of bacteriophage-containing aerosol against nosocomial transmission of carbapenem-resistant Acinetobacter baumannii in an intensive care unit. PLoS ONE 2016, 11, e0168380. [Google Scholar] [CrossRef]
- Lai, M.J.; Liu, C.C.; Jiang, S.J.; Soo, P.C.; Tu, M.H.; Lee, J.J.; Chen, Y.H.; Chang, K.C. Antimycobacterial activities of endolysins derived from a mycobacteriophage, BTCU-1. Molecules 2015, 20, 19277–19290. [Google Scholar] [CrossRef]
- Bonilla, N.; Rojas, M.I.; Netto Flores Cruz, G.; Hung, S.-H.; Rohwer, F.; Barr, J.J. Phage on tap-a quick and efficient protocol for the preparation of bacteriophage laboratory stocks. PeerJ 2016, 4, e2261. [Google Scholar] [CrossRef]
- Adams, M. Bacteriophages; Interscience: New York, NY, USA, 1959; pp. 137–159. [Google Scholar]
- Tseng, C.C.; Hsiao, P.K.; Chang, K.C.; Cheng, C.C.; Yiin, L.M.; Hsieh, C.J. Detection of viable antibiotic-resistant/sensitive Acinetobacter baumannii in indoor air by propidium monoazide quantitative polymerase chain reaction. Indoor Air 2015, 25, 475–487. [Google Scholar] [CrossRef]
- Chen, P.S.; Li, C.S. Quantification of airborne Mycobacterium tuberculosis in health care setting using real-time qPCR coupled to an air-sampling filter method. Aerosol Sci. Technol. 2005, 39, 371–376. [Google Scholar] [CrossRef]
- Tseng, C.C.; Chang, L.Y.; Li, C.S. Detection of airborne viruses in a pediatrics department measured using real-time qPCR coupled to an air-sampling filter method. J. Environ. Health 2010, 73, 22–29. [Google Scholar]
- Beggs, C.B.; Kerr, K.G.; Noakes, C.J.; Hathway, E.A.; Sleigh, P.A. The ventilation of multiple-bed hospital wards: Review and analysis. Am. J. Infect. Control 2008, 36, 250–259. [Google Scholar] [CrossRef]
- Hatfull, G.F. Mycobacteriophages: Windows into tuberculosis. PLoS Pathog. 2014, 10, e1003953. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. Method 1602: Male-Specific (F+) and Somatic Coliphage in Water by Single Agar Layer (SAL) Procedure; EPA 821-R-01-029; United States Environmental Protection Agency, Office of Water, Engineering and Analysis Division: Washington, DC, USA, 2001.
- Jończyk, E.; Kłak, M.; Międzybrodzki, R.; Górski, A. The influence of external factors on bacteriophages-review. Folia Microbiol. 2011, 56, 191–200. [Google Scholar] [CrossRef]
- Olson, M.R.; Axler, R.P.; Hicks, R.E. Effects of freezing and storage temperature on MS2 viability. J. Virol. Methods 2004, 122, 147–152. [Google Scholar] [CrossRef]
- Schijven, J.; van Dommelen, J.; Havelaar, A.; Bahar, M.; Mooijman, K. Interlaboratory Study on the Preparation and Use of Standard Samples with F-Specific Rna-Bacteriophages; RIVM Rapport 281008012; National Institute for Public Health and the Environment (RIVM): Bilthoven, The Netherlands, 1995. [Google Scholar]
- Mendez, J.; Jofre, J.; Lucena, F.; Contreras, N.; Mooijman, K.; Araujo, R. Conservation of phage reference materials and water samples containing bacteriophages of enteric bacteria. J. Virol. Methods 2002, 106, 215–224. [Google Scholar] [CrossRef]
- Peccia, J.; Werth, H.M.; Miller, S.; Hernandez, M. Effects of relative humidity on the ultraviolet induced inactivation of airborne bacteria. Aerosol Sci. Technol. 2001, 35, 728–740. [Google Scholar] [CrossRef]
- Lin, W.H.; Li, C.S. The effect of sampling time and flow rates on the bioefficiency of three fungal spore sampling methods. Aerosol Sci. Technol. 1998, 28, 511–522. [Google Scholar] [CrossRef]
- Hsiao, P.K.; Chen, W.T.; Chang, K.C.; Ke, Y.J.; Kuo, C.L.; Tseng, C.C. Performance of CHROMagar Staph aureus and CHROMagar MRSA for detection of airborne methicillin-resistant and methicillin-sensitive Staphylococcus aureus. Aerosol Sci. Technol. 2012, 46, 297–308. [Google Scholar] [CrossRef]
- Chen, P.S.; Li, C.S. Sampling performance for bioaerosols by flow cytometry with fluorochrome. Aerosol Sci. Technol. 2005, 39, 231–237. [Google Scholar] [CrossRef]
- Chang, C.W.; Chou, F.C. Methodologies for quantifying culturable, viable, and total Legionella pneumophila in indoor air. Indoor Air 2011, 21, 291–299. [Google Scholar] [CrossRef]
- Li, C.S.; Hao, M.L.; Lin, W.H.; Chang, C.W.; Wang, C.S. Evaluation of microbial samplers for bacterial microorganisms. Aerosol Sci. Technol. 1999, 30, 100–108. [Google Scholar] [CrossRef]
- Leung, S.S.; Parumasivam, T.; Gao, F.G.; Carrigy, N.B.; Vehring, R.; Finlay, W.H.; Morales, S.; Britton, W.J.; Kutter, E.; Chan, H.K. Production of Inhalation Phage Powders Using Spray Freeze Drying and Spray Drying Techniques for Treatment of Respiratory Infections. Pharm. Res. 2016, 33, 1486–1496. [Google Scholar] [CrossRef]
- Riley, R.; Knight, M.; Middlebrook, G. Ultraviolet susceptibility of BCG and virulent tubercle bacilli. Am. Rev. Respir. Dis. 1976, 113, 413–418. [Google Scholar]
- Brickner, P.W.; Vincent, R.L.; First, M.; Nardell, E.; Murray, M.; Kaufman, W. The application of ultraviolet germicidal irradiation to control transmission of airborne disease: Bioterrorism countermeasure. Public Health Rep. 2003, 118, 99. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Core curriculum on tuberculosis. In What the Clinician Should Know; US Department of Health & Human Services Atlanta: Atlanta, GA, USA, 2000. [Google Scholar]
- Kramer, A.; Schwebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef]
- Kowalski, W. Ultraviolet Germicidal Irradiation Handbook: Uvgi for Air and Surface Disinfection; Springer: New York, UY, USA, 2009. [Google Scholar]
- Collins, F. Relative susceptibility of acid-fast and non-acid-fast bacteria to ultraviolet light. Appl. Microbiol. 1971, 21, 411–413. [Google Scholar]
- Tseng, C.C.; Li, C.-S. Inactivation of viruses on surfaces by ultraviolet germicidal irradiation. J. Occup. Environ. Hyg. 2007, 4, 400–405. [Google Scholar] [CrossRef]
- Lourenco, M.; De Sordi, L.; Debarbieux, L. The Diversity of Bacterial Lifestyles Hampers Bacteriophage Tenacity. Viruses 2018, 10, 327. [Google Scholar] [CrossRef]
- Hatfull, G.F. Molecular Genetics of Mycobacteriophages. Microbiol. Spectr. 2014, 2, 1–36. [Google Scholar] [CrossRef]






© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tseng, C.-C.; Chang, D.C.; Chang, K.-C. Development of a Biocontrol Method Applying Bacteriophage-Containing Aerosol against Mycobacterium tuberculosis Using the Bacteriophage BTCU-1 and M. smegmatis as Models. Microorganisms 2019, 7, 237. https://doi.org/10.3390/microorganisms7080237
Tseng C-C, Chang DC, Chang K-C. Development of a Biocontrol Method Applying Bacteriophage-Containing Aerosol against Mycobacterium tuberculosis Using the Bacteriophage BTCU-1 and M. smegmatis as Models. Microorganisms. 2019; 7(8):237. https://doi.org/10.3390/microorganisms7080237
Chicago/Turabian StyleTseng, Chun-Chieh, Dan Chi Chang, and Kai-Chih Chang. 2019. "Development of a Biocontrol Method Applying Bacteriophage-Containing Aerosol against Mycobacterium tuberculosis Using the Bacteriophage BTCU-1 and M. smegmatis as Models" Microorganisms 7, no. 8: 237. https://doi.org/10.3390/microorganisms7080237